1
Genus Streptococci
Objectives, Upon completion of this lecture, the student will:
Outline the medically important streptococci species.
Classification of genus streptococci.
Describing the morphology & physiology for streptococci.
Determine the virulence factors for streptococci.
Analyze the diseases & pathogenicity for streptococci.
Demonstrate the epidemiology/transmission for streptococci.
Outline the laboratory diagnosis for streptococci.
State the drug of choice and prophylaxis where regularly
used.
Lec.2
Dr.Sarmad M.H. Zeiny
2014-2015
College of Medicine-
University of Baghdad
2
Genus Streptococcus
General Characteristic:
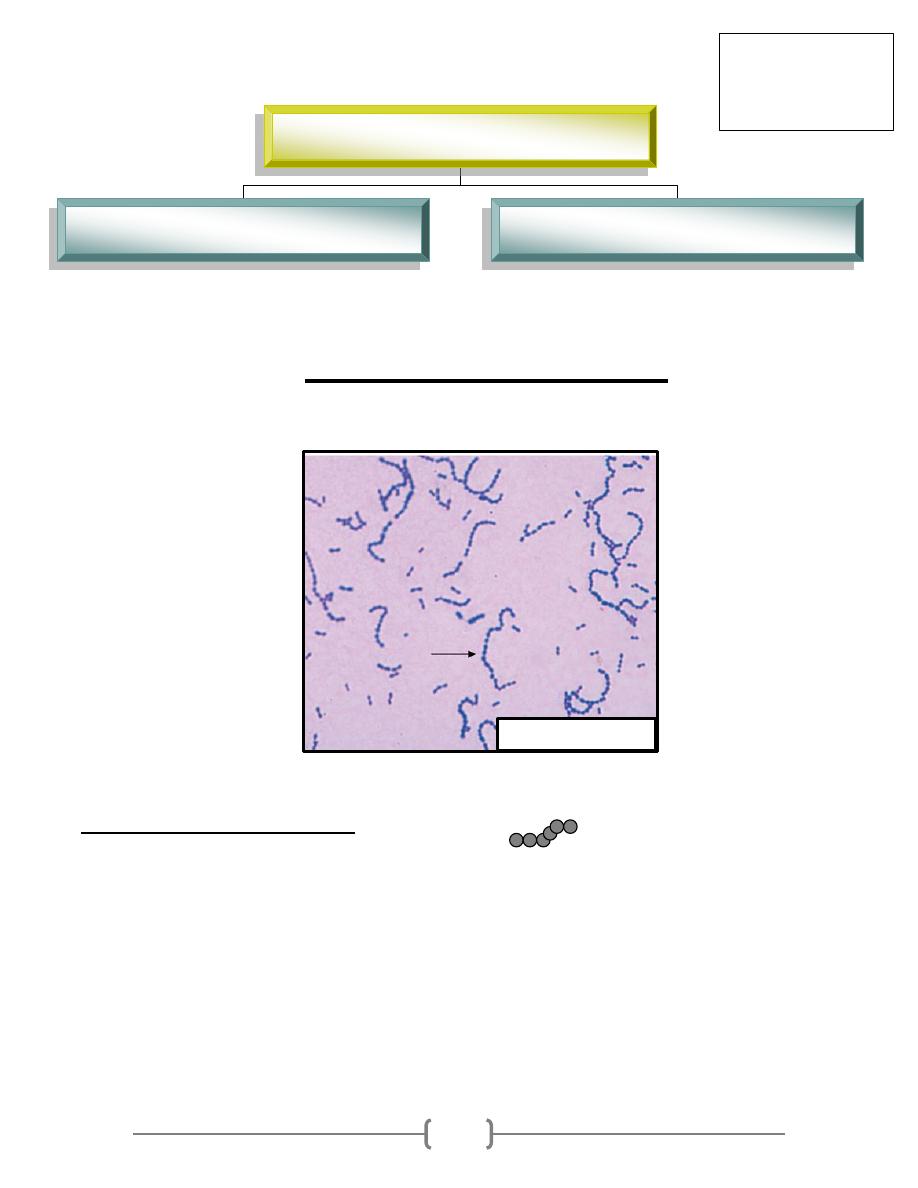
G+ve cocci, arrange in chains or pairs. (Fig.1)
Some strains are capsulated, which are important in pathogenicity.
Majority are facultative anaerobic, few are obligatory anaerobic.
Catalase –ve
Non motile.
Non spore forming
Fastidious microorganism (require rich media for its growth with additional growth
supplement). Such as Blood Agar and Chocolate Agar (enrich media).
Lec.2
Dr.Sarmad Zeiny
2013-2014
BCM
Fig.1: Streptococci
Gram positive cocci
Streptococci (catalase –ve)
Staphylococci (catalase +ve)
3
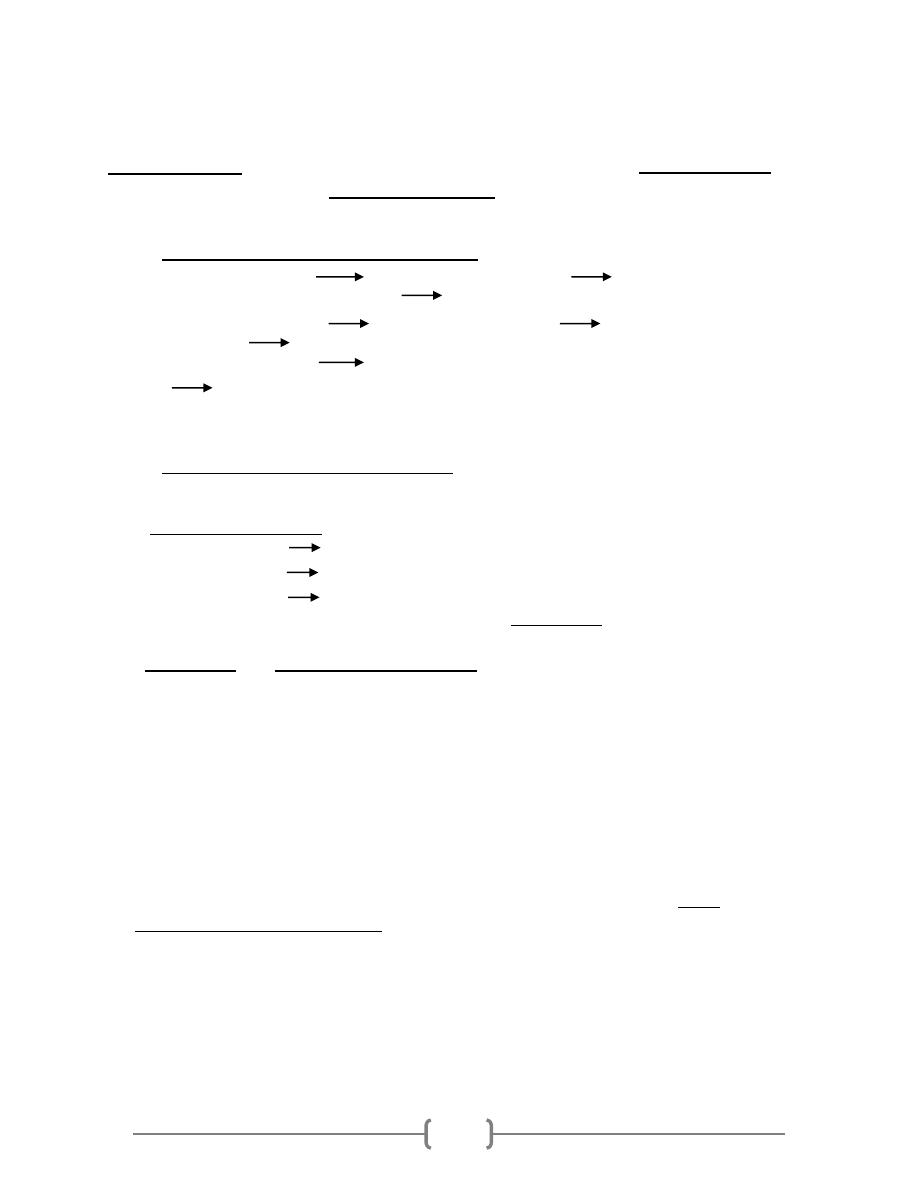
Classification:
Streptococci can be classified mainly according to the type of hemolysis on
blood agar or according to the antigenic components, both classification are used and integrated
to describe member of genus Streptococci:
1. HEMOLYSIS: (tested on blood agar plate)
β- hemolysis complete RBCs destruction Clear zone around the
colony(called target sign) S. pyogenes, S. agalactiae
α- hemolysis partial RBCs destruction Greenish discoloration of
agar S.pneumoniae, Viridans streptococci
γ- hemolysis No obvious changes around the colony (No hemolysis).
Enterococci and non-enterococcal streptococci (S.bovis).
2. SEROLOGY (antigenic components):
(Lancefield Grouping): there are differences in the polysaccharide antigens of the cell wall
(C carbohydrate). Depending to these specific polysaccharide antigens, Streptococci named
as groups (group specific) from A to U (more than 20 serogroups). Important are:
Group A S. pyogenes
Group B S. agalactiae
Group D Enterococci & non-enterococcal streptococcus.
Group A (S. pyogenes) have M-protein which is a type specific Ag, classify (group A) into
more than (80 serotypes).
M protein is a major virulence factor for the group A streptococcus. It
inhibits the activation of complement and protects the organism from
phagocytosis. However, it is also the weakest point in the organism's defense,
because plasma cells generate antibodies against the M protein. These
antibodies bind to the M protein (opsonization), aiding in the destruction of the
organism by macrophages and neutrophils.
So when you want to describe S. pyogenes you should say: Group A beta-
hemolytic Streptococci =GABH Streptococci.
Although there are more than 30 species of streptococci, only 5 are
significant human pathogens. Three of these pathogens have Lancefield
antigens: Lancefield group A, B and D. The other two pathogenic species of
the streptococcal genus do not have Lancefield antigens, and are therefore just
called by their species names: One is Streptococcus pneumoniae and the other
is actually a big group of streptococci collectively called the Viridans group
streptococci.
4
GROUP A β-HEMOLYTIC STREPTOCOCCI
(Streptococcus pyogenes)
o These organisms are so-named because they possess the Lancefield group A
antigen and are beta-hemolytic on blood agar. They are also called
Streptococcus pyogenes (which means pus-producing).
o The components of the streptococcal cell wall that are antigenic include: C
carbohydrate & M protein (~80 types).
o Reservoir: • Human throat • Skin
o Transmission: • Direct contact • Respiratory droplets
Virulent factors & Pathogenesis:
1) M protein is a major virulence factor for the group A streptococcus.
2) Capsule:
composed of hyaluronic acid. They impede phagocytosis.
3) Streptolysin O: The O stands for oxygen labile as it is inactivated by oxygen.
This enzyme destroys red and white blood cells and is the reason for the
beta-hemolytic group A streptococci's beta-hemolytic ability. This enzyme
is also antigenic. Following pharyngeal or systemic beta hemolytic group A
streptococcal infection, anti-streptolysin O (ASO) antibodies develop. On
the wards you may order ASO titers on a patient's blood to confirm recent
infection.
4) Streptolysin S: The S stands for oxygen stabile. This is also responsible for
beta-hemolysis but is not antigenic.
5) Pyrogenic exotoxins (also called erythrogenic toxin): This is found in only a
few strains of beta hemolytic group A streptococci, but when these strains
invade they can cause scarlet fever. Some strains produce pyrogenic
exotoxins that are superantigens. The exotoxins directly super stimulate T
cells to pour out inflammatory cytokines, this is called streptococcal toxic
shock syndrome
6) Streptokinase (activates the proteolytic enzyme plasmin, which breaks up
fibrin blood clots). spreading factor
7) Hyaluronidase spreading factor
8) Streptodornases (DNAases) spreading factor
9) (Anti-C5a) peptidase. anti-inflammatory
5
Diseases:
I. Local infections(invasion):
1) Sore throat (acute pharyngitis, pharyngotonsillitis). Leading Cause.
2) Wound infection, cellulitis, Necrotizing fasciitis and myonecrosis.
3) Impetigo.
4) Erysipelas (erythema on face).
II. Systemic infection: (invasion &/or toxin)
1) Sepsis.
2) Meningitis.
3) Puerperal sepsis.
4) Streptococcus toxic shock syndrome, Scarlet fever (sunburn rash)
both caused by pyrogenic exotoxins.
III.
Post streptococcal infection sequel ( delayed antibody mediated
diseases): it is a non-suppurative complications
1) Rheumatic fever (after sore throat): type II hypersensitivity
2) Acute glomerulonephritis (after skin or pharynx infection), mainly
by M-12 serotype: type III hypersensitivity
Notes on post streptococcal infection sequel:
Rheumatic fever:
It usually strikes children 5-15 years of age. When it occurs, it has been shown to
follow untreated beta-hemolytic group A streptococcal pharyngitis (but NOT after
a skin infection).
Rheumatic fever is antibody-mediated. There are antigens in the heart that
are similar to the antigens of the beta-hemolytic group A streptococci. Therefore,
the antibodies that forms to eradicate this particular streptococcus also cross-
react with antigens in the heart. This immunologic attack on the heart tissue
causes heart inflammation, called myocarditis. Patients may complain of chest
pain and may develop arrhythmias or heart failure.
ASO test:
Measure Ab against Streptolysin O,
ASO test used in suspected case of rheumatic fever.
6
This test used to determine significance of current streptococcal infection
by measuring the ASOT: ASOT (Ab Titer):
Normal < 200 > significance result
Acute post-streptococcal glomerulonephritis:
This is an antibody-mediated inflammatory disease of the glomeruli of the
kidney. It occurs about one week after infection of either the pharynx OR skin by
nephritogenic (having the ability to cause glomerulonephritis) strains of beta-
hemolytic group A streptococci. Certain antigens from these nephritogenic
streptococci induce an antibody response. The resulting antigen-antibody
complexes travel to and are deposited in the glomerular basement membrane,
where they activate the complement cascade. This leads to local glomerular
destruction in the kidney.
Lab Dx for S.pyogenes:
Specimens: depend on the nature of infection, e.g. sputum, throat swab,
nasopharyngeal swab, blood, CSF…etc.
Gram stain: G+ve cocci, arrange in chains.
Culture: on blood agar under 5-10%CO
2
pinpointed, Grayish white,
translucent, matte or glossy colonies with large zone of β- hemolysis.
Sensitive to Bacitracin disc (0.04 U) causes zone of growth inhibition more
than 15mm.
PYR +ve: rapid test, pink is positive.
Serology: 1)The rapid strep test (ELISA-based), 2) Lancefield grouping, 3) M-
protein serotyping and 4) ASO test:
Ab Titer: Normal < 200 > significance result
GROUP B STREPTOCOCCI
S. agalactiae (β- hemolytic, Group B)
Normal flora of female genital tract (15-25% of woman), male urethra.
Leading Cause for neonatal sepsis, pneumonia & meningitis (acquire these
bacteria during delivery).
Pathogenesis: Capsule, hemolysin and cAMP factor
These streptococci are also beta-hemolytic. When thinking of group B
streptococci, think of group B for BABY.
Bacitracin resistant.
Hydrolyzes hippurate. Positive (purple color)
7
cAMP test-positive: cAMP factor is a polypeptide that "compliments" a Staph
aureus to make an area of new complete beta-hemolysis. Organism produces
definitive arrow when close to Staphylococcus aureus.
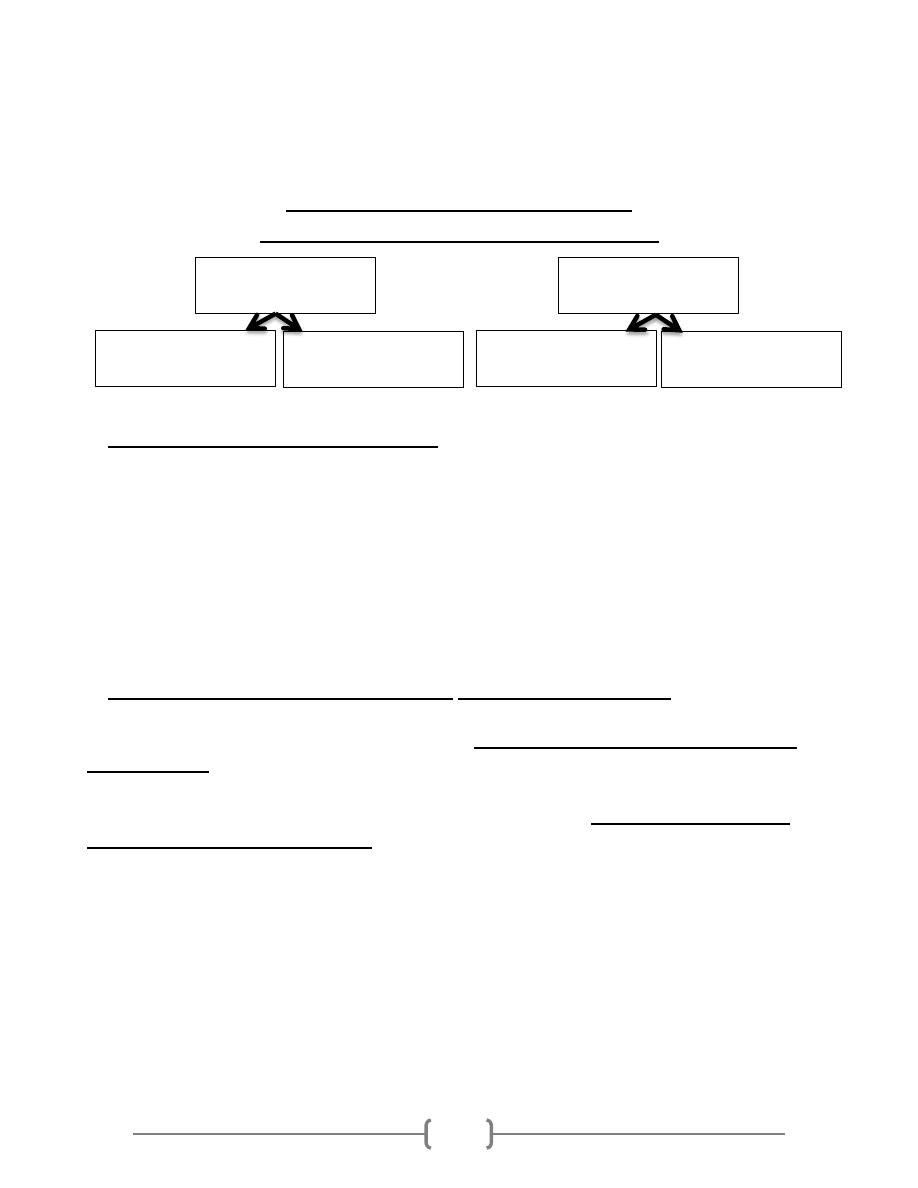
GROUP D STREPTOCOCCI
(Enterococci and Non-enterococci)
Enterococcus (E.faecalis, E.faecium):
Normal flora of GIT, oral mucosa.
Grow well in 40% bile and on 6.5% NaCl.
Causes UTI, biliary tract infection, and endocarditis.
Varies Hemolysis
PYR +ve
Hydrolyzes esculin in 40% bile and 6.5% NaCl (bile esculin agar turns black).
Multi-drug resistant, e.g. Vancomycin resistant enterococci (VRE) have developed
and have been spreading. Treatment as with VRSA.
Non-enterococcus (Streptococcus bovis,
Streptococcus equinus ):
Like the enterococci, Streptococcus bovis is hardy growing in 40% bile (but not
in 6.5% NaCl).
It lives in the G.I. tract, and it causes similar diseases.
An important unique property is that there is a remarkable association between S.
bovis infection and colon cancer!!! In some series 50% of people with S. bovis
bacteremia have a colonic malignancy. We do not know if S. bovis is a cause of colon
cancer or just a marker of the disease.
(BOVIS in the BLOOD:
Better Beware, CANCER in the BOWEL)
Enterococci
Enterococcus
faecalis
Enterococcus
faecium
Non-Enterococci
Streptococcus bovis
Streptococcus
equinus
8
Summary:
Streptococci classified according to the type of hemolysis &
antigenic components.
S.pyogenes is the most pathogenic species because of their virulent
factors.
S.pyogenes can cause post-infection severe complications.
ASO test used in suspected case of rheumatic fever.
Streptococci easily diagnosed in the lab. By using Gram’s staining,
culture and biochemical tests.
S.agalactia is the leading Cause for neonatal sepsis, pneumonia &
meningitis.
Enterococcus Causes UTI, biliary tract infection, wound infection,
bed sore, endocarditis.
streptococci infections can be prevented by regular hygiene
precautions and by antibiotics, no vaccine.
References:
-
Review of Medical Microbiology and Immunology11th edition 2010.
-
Clinical Microbiology Made Ridiculously Simple, 6
th
ed, 2014.
-
Baily & Scott diagnostic microbiology, 12
th
ed.
-
Lippincotts Illustrated microbiology 3
ed
ed., 2013
END
