Congenital heart diseases
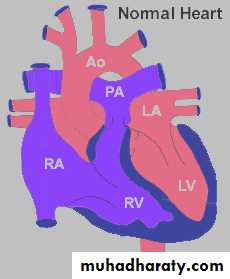
These are abnormalities in the cardiocirculatory structures or function that are present at birth , even if it is discovered later.
Incidence
0.8% in normal population.2-6% in 2nd pregnancy after birth of 1st child with CHD.
20-30% if 2 other siblings have CHD.
Etiology
Multifactorial : genetic , enviromentalGenetic :
• Chromosomal anomalies ( Turner, Trisomies 18,21).• Supracristal VSD in Asian.
• Increase incidence if 1st degree relative affected.
• Chromosomal deletion ( chr. 22q11….. DiGeorge syndrome ).
• Cardiomyopathy.
• Heritable arrhythmias
Enviromental :
Maternal DM
Phenylketonuria
Congenital rubella
SLE
Drugs (Lithium, ethanol, warferin, thalidomide, antimetabolites, anticonvulsants)
classification
Acyanotic CHD:a .Ventricular septal defects (VSD) 25%
b .Atrial septal defects (ASD) 10% volvme
c. Patent ductus arteriosus (PDA) 10% load Lf
d. Pulmonary stenosis 10%
e. Coarctation of the aorta 8% pressuref.Aortal stenosis 6% load
Cyanotic heart disease
With pulmonary blood flow• TOF
• P. ATRESIA +/- VSD
• TRICUSPID ATRESIA
• DORV+ PS
• EBSTEIN ANOMALY OF TV
With pulmonary blood flow
• TGA
• Total anomalous pulmonary venous return
• Truncus arteriosus
• Single ventricle
• Hypoplastic Lt. heart syndrome
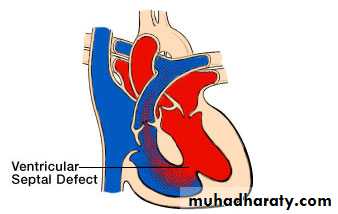
VENTRICULAR SEPTAL DEFECT (VSD)
The most common CHDAnatomically classified into:
1-membranous VSD 80%
2-Muscular VSD 5%
3-Inlet VSD 5%
Hemodynamically (functionally): classified into:
1- Small VSD (small Lt.-Rt. Shunt)
2-Moderate VSD
3-Large VSD
Ventriculoseptal Defect
pathophysiology
Lt to Rt shunt depend on :• 1-Size ( restrictive & large non restrictive )
• 2-qp : qs ratio :(pulmonary to systmic blood flow)
Small < 1.75:1
Large > 2:1
'When a small communication is present (usually <0.5 cm2), the VSD is called restrictive and right ventricular pressure is normal.
In large nonrestrictive VSDs (usually >1.0 cm2), right and left ventricular pressure is equalized.
The functional disturbance caused by VSD magnitude of the L-R shunt depends on: size of VSD & degree of pulmonary vascular resistance not on the site of VSD.
In large VSD
there is no resistance to the flow, so there is large shunt and there will be progressive increase in right ventricular (RV) & pulmonary artery pressure, as a result of increase of the pulmonary vascular resistance which causes reverse shunt Rt-Lt. (Eisenmenger syndrome) which is irreversibleIn small VSD
there is high resistance to the flow through the VSD so there is small Lt.-Rt Shunt and the pressure is normal in RV and pulmonary artery (PA).
Clincal features
Small VSD• 1-Most common.
• 2-Asymptomatic .
• 3-Dx during routine examination .
• 4-Harsh , blowing holosystolic murmur .
• 5-Immediately in neonatal period Lt to Rt shunt minimal lead to that the murmur may not be heard .
• 6-In premature the murmur heard earlier .
Large VSD
Dyspnea ,feeding difficulty , poor growth , profuse sweeting recurrent pulmonary infection .
Cyanosis usually absent , but duskiness specially during infection.
O/E:
1-Palpable parasternal lift .2-Lateral displaced impulse .
3-Systolic thrill .
4-Holosystolic murmur less harsh.
5-Pulmonary component of 2nd heart sounds increased .
6-Mid diastolic rumbling murmur increased at apex =qp;qs ratio 2:1.
DIAGNOSIS:
1. ECG:a.small VSD -> normal ECG
b.large VSD -> biventricular hypertrophy
• 2.CxR.:
a.small VSD -> normal
b.large VSD -> cardiomegaly, dilated pulmonary vessels (plethoric lung)
• Echo:
• two-dimensional and doppler echo must be done in all patients to determine the following:
a. Size
b. Anatomical location
c. Size & direction of intracardiac shunt
d. The degree of pulmonary hypertension
e. Present of associated lesion (as TOF)
• 4-Catheterization & angiography:
• a small number of patients with VSD requires cath. (because echo is more sensitive & more specific).• a Provide a clear anatomical picture of the location and no. of VSD in patients when surgery is required
b.Estimation of magnitude of the shunt & pulmonary vascular resistance (to know if the patient is still operable or not).
c .Close some muscular VSDs with catheter derived devices.
Prognosis and natural historyCourse depends on the size :
Small VSD ( 30-50%) close spontaneously frequently during 1st 2 years of life
Muscular 80%.Membranous 35%
Small asymptomatic if unoperated long term sequalies (arrythmia , subaortic stenosis , exercise intolerance ).
Large vsd less likely to close spontaneously . 8% may close completely . repeated infection , repeated HF,FTT.
Large VSD: most patients need surgical repair, in the 1st year of life,
Without surgical repair, most patients will develop pulmonary hypertensionand some reach to Eisenmenger syndrome (10%), but 5% wall develop infundibular & pulmonary stenosis.
Those with supracristal VSD at risk for aortic regurgitation.
Small % acquired infandibular pulmonary stenosis protect pulmonary circulation from over circulaion .There is risk of infective endocarditis irrespective of defect size.
TreatmentSmall VSD
1-Reassured the parents .
2-Encouraged patient to have normal life , no restriction of physical activity.
3-Surgical repair not encouraged .
4-Protect against IE with AB.
5-Can monitor the patient with
• Clinical examination
• ECG for evidence of PH• Echo
Large VSD
• Medical Rx:To control HF and prevent development of PH and tx of resp. infection nutritional support prophylaxis SBE
• Surgical repair: either pulmonary arty banding or total surgical repaire
• Indications• 1-Any age with large defects in whom clinical features and failure to thrive can’t be controlled medically
• 2-Infants between 6-12 months with large defects associated with PH even if symptoms controlled by medical Rx.
• 3- more thane 24 months old age and qp:qs > 2:1.
• 4-Patient with supracristal VSD of any size because of risk of development of aortic regurgitation.• Catheterization based tx;most muscular VSD and some membranous can closed by devices place during cath.
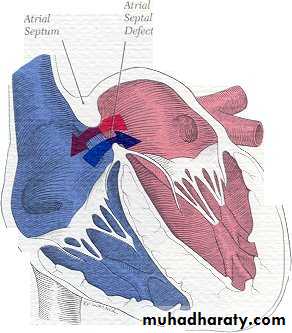
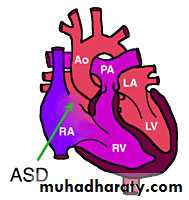
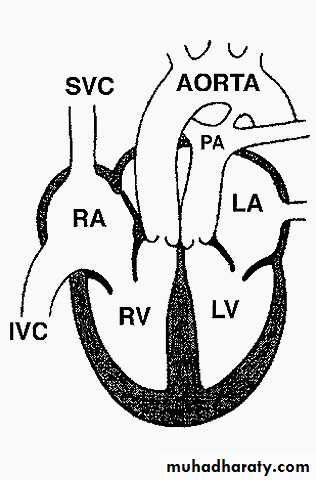
ATRIAL SEPTAL DEFECT (ASD)
• an opening in the intra-atrial septum other than patent foramen ovale more
• common in females; F:M ratio is 3:1.
• It has 3 types:
• 1-Primum ASD (in lower part) 10%
• 2-Secondum ASD (in the middle) 80%
• 3-Sinus venosus (in the upper part) 10%
• HEMODYNAMIC EFFECT: There will be chronic Lt-Rt. Shunt which causes volume overload on the Rt. Sided cardiac structures & result in their dilatation & increase of pulmonary blood flow.
ATRIAL SEPTAL DEFECT
Clinical features
Most often asymptomatic.In younger children may cause subtle FTT.
In older children lead to exercise intolerance .
O/E:
Mild Lt precordial bulge.Loud 1st heart sound.
2nd heart sound split widely and fixedly.
Systolic ejection murmur.
Short rumbling mid – diastolic murmur with the bell of the stethoscope =qp:qs at least 2:1.
DX:
A.CXR
Cardiomegaly of RV configuration
Round apex peak
Increase pulmonary marking
B. ECG:
Right axis deviation (RAD)
Incomplete RBBB
Peaked P-wave (RA enlargement)
C- Echo: Trans-thoracic & trans-esophageal echocardiography is essential for Dx.
D. Cardiac Catheterization: Not essential for Dx, indicated in: Therapeutic aim & 'Exclude associated cardiac anomaly .Natural history
ASD is a benign lesion Rarely causes heart failure or pulmonary hypertension in the 1st decade of life
Rarely complicated by infective endocarditis
Rarely closed spontaneously after infancy
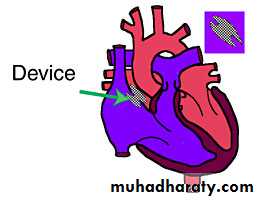
Treatment
If patient Symptomatic or has qp :qs ratio at least 2:1Then the treatment is
The surgery done after 1 yr. of age and before enterance to school.
• Surgery• Transcatheter device closure
Atrial septal defect
Prognosis
May close spontaneously during infant .Mau be tolerated during childhood .
Symptoms not appear until 3rd decade or later and late menifestation is
• PH
• Atria dysarrhythmias
• Mitral or tricuspid insufficiency
• HF
Infective endocarditis rare and need no prophylaxis with AB.
Atriovantricular septal defect(endocardial cushion defect)
It is agroup of anomalies sharing adefect at the siteatrioventricular septum And abnormality in the atrioventricular valve.
Common in downs syndrom,so all patients with downs syndromshould Have cardiac evaluation if symptomatic or before 6 months of age
Equal no. of male and females are affected
CLASSIFICATION:
1-Partial: ASD primum, clefted mitral valve .intact VSD2-Complete: ASD primum, large inlet VSD, common single atrioventricular valve.
C/F:1- Partial: either asymptomatic (mainly) or mild symptoms. O/E: ASD murmur of mitral regurgitation.
2. Complete: as the above with heart failure and/or pulmonary vascular disease.
pathophysiology
OP: Lt Rt. Shunt .
Mitral insufficiency.
PA pressure normal .
C/F of ASD.
AVSD : Lt Rt shunt at atrial + ventricular level.
Valvular insuffiency volume load on one or both ventricles.pulmonary vascular resistance Rt Lt shunt cyanosis.
Diagnosis
• CXR : marked cardiac enlargement , pulmonary vascularity , PA enlargement.• ECG: Rt axis deviation of QRS,RBBB,RVH.
• ECHO : RV enlargement , septal deficiency .
• CATHE.
• Selective LV ventriculography.
Treatment
OP : surgical correction .Complete AVSD : risk of PHPT during 1st 6-12 mo. surgery in early infancy
Some time do pulmonary banding if too small baby or associated with deformity that make surgery risky.
NATURAL HISTORY:
It depends on the size of various atrial and ventricular defects and the amount of mitral regurgitation.
The ostium primum ASD with no mitral regurgitation has the same benign natural history of simple secondum ASD, but with complete AV-canal defect, heart failure and/or pulmonary vascular disease may occur.
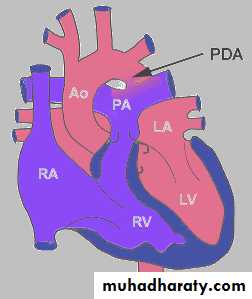
PATENT DUCTUS ARTERIOSUS (PDA)
It is a channel that connect the pulmonary artery with the descending aorta (isthumus part). It results from the persistence of patency of the fetal ductus arteriosus after birth.
It is the most common lesion in infant of mothers with congenital rubella, PDA more common in females.
Patent ductus arteriosus
Normally functional closure of ductus arteriosus occurs at 10-15 hr after birth . If it persist opened after pulmonary vascular resistance falls leads to aortic blood shunts to pulmonary artery.More common in female
Aortic side ( distal to the origin of lt subclavian art.)Pulmonary side ( at the bifurication )
Why it is not closed ?
Premature ( normal structure ) due to hypoxia and immaturity .In term baby have structural abnormality.
In term baby if persist beyond 1st few weeks means not closed spontaneously.
Most of cases in premature closed spontaneously.
10% associated with other CHD.
PathophysiologyLt Rt shunt depends
Size of defect
Ratio of pulmonary : systemic vascular resistanceClinical features
SmallAsymptomatic .
Heart size may be abnormal
Large
Hf , growth retardation
Bounding peripheral pulse
Wide pulse pressure
Large heart
Apical impulse prominent
Thrill
Machinery murmur
Mid-diastolic murmur at apex
DIAGNOSIS:
ECG: In small PDA, it is normal, but large PDA, there is normal axis deviation, left ventricular hypertrophy (LVH) or biventricular hypertrophy.
Chest X-ray: Cardiomegaly, plethoric lung, and prominent pulmonary conus.
treatment
Closure irrespective of age .Endomethacin is often effective in closing the PDA in the premature neonate by decreasing PGE1 levels.
Closure by :
• Thoracoscopic ( postoperative discomfort and scarring ) .
• Transcatheter :
• Small coil.
• Large sac in which several coils released or umberella –like device .
Thank you
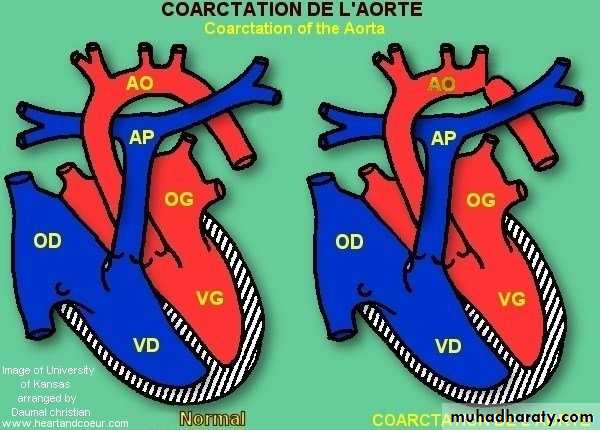
Coarctation of aortaConstriction that occur at any portion of aorta from transverse arch to the iliac bifurication.more in male afeatures of turner
Pathophysiology :
2 typesJuxtaductal ( if mild adult type) 98% just below origin of lt subclavian art.
Tubular hypoplastic ( infantile type ) .
If more severe juxtaductal or tubularhypoplastic blood pass through ductus arteriosus decsending aorta if closed diffrential cyanosis ( lower blue extremities and upper pink extremities ).
In COA:
blood pressure in area proximal to coarctation( mechanical and hormonal )
blood pressure distal to the coarctation.
Development of collaterals from subcalvian , internal mamery , superior intercostal .
Clincal features
If mild and Dx after infancy rarely significant symptoms and most diagnosed by blood pressure with routine physical examination.Signs :
Pulses of UL and LL.
Radio-femoral delay.
Blood pressure in both UL and LL.
Blood pressure in each arm.
Ejection systolic click + thrill.
Systolic murmur in 3rd , 4th Lt sternal border .
Mid-diastolic murmur.
Systolic murmur of aortic stenosis
In neonatal period
Lt body hypoperfusion, acidosis, HF .
Before ductal closure differential cynosis.
Diagnosis
• CXR• ECG
• ECHO
• COLOR DOPPLER
• CONTINOUS AND PULSED WAVE DOPPLER
• CATHETRAIZATION + LT VENTRICULOGRAPHY
• MRI used in dx due to difficulty in infancy
Complications
• Untreated succumb at 20-40 yr.• Complications secondary to
• IE, Endarteritis
• Aneuryzms of the descending aorta or collaterals.
• Neonates : hypoperfusion + HF
• Premature coronary arterey disease
• HF
• ICH
• Hypertensive encephalopathy
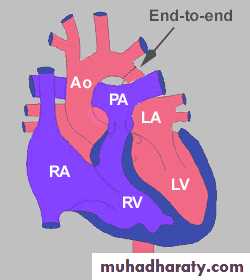
Treatment
• In neonate PGE1 reopen ductus and relieve obstruction stabilize him surgery.
• Older children HF antifailure surgery
• Surgery:
Excision and primary re-anastamosis
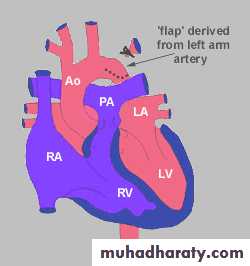
Subclavian flap.
Patch aortoplasty.
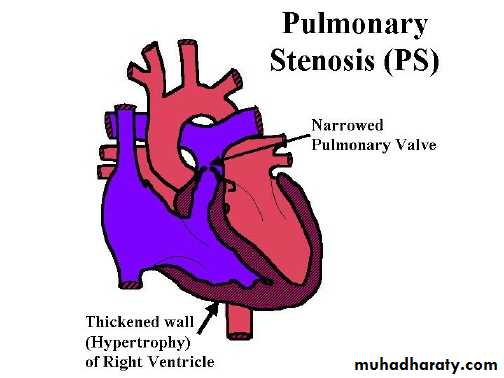
Pulmonary stenosis
Pulmonary stenosis divided anatomically into :• Vulvular ( most common ) .90%
• Supravalvular .
• Subvalvular.
Pathophysiology
Obstruction Rt. Ventricular pressure during systole wall stress severe cases RVH.Pulmonary art. Pressure normal or .
Arterial O2 normal unless VSD or ASD.
Critical pulmonic stenosis in neonate shunt at the foramen ovale
Clinical features
According to severity• Mild : asymptomatic , normal venous pressure , ejection click after 1st heart sound , 2nd heart sounds split , short ejection systolic murmur in pulmornary area .
ECG: normal or mild RVH.
CXR: poststenotic pulmonary arterial dilatation.
ECHO: pr.gradient usually 10-30mmHg
• Moderate : slightly elevated venous pr. , prominent a – wave in jugular pulse, 2nd heart sound split , ejection click, ejection systolic murmur
• CXR: normal or pulm.vascularity .
• ECG: RVH, spiked p-wave.
• ECHO: thickened valve , pr.gradient 30-60 mmHg.
• .
• Severe: Rt.sided failure, hepatic enlargment, periphral edema , venous pr. a-wave , heart enlarged , inaudible pulmonary component of 2nd heart sound , ejection systolic murmur and thrill , no click.
CXR: enlarged heart + pulmonary vascularity.
ECG: RVH, spiked p-wave.
ECHO: valve deformity, RVH.,pr.gradient ≥ 60 mmHg
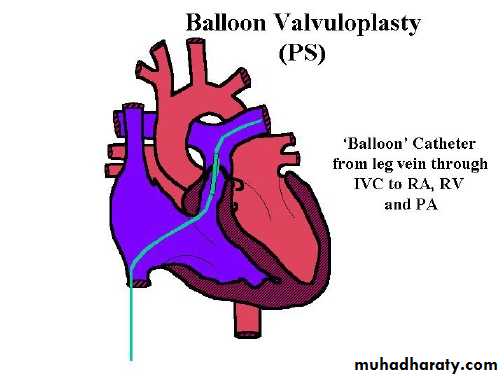
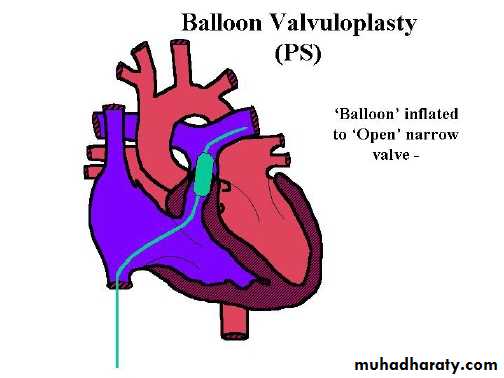
Treatment
• Mild reassurance .
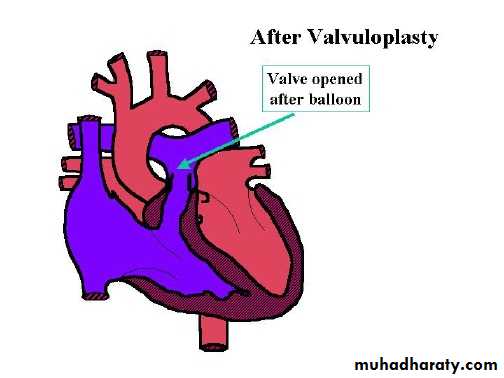
• Moderate or severe balloon valvuloplasty .
• Critical pulmonic stenosis valvuloplasy or surgery.valvutomy
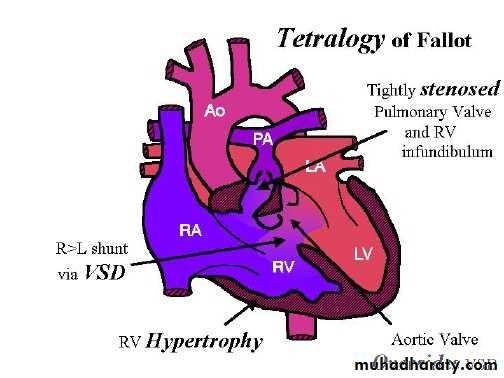
Tetralogy of Fallot
It is the commonest cyanotic heart disease in children , it’s a combination of :-
Right ventricular outflow obstruction(pulmonary stenosis)
VSD
Dextroposition of aorta with override of ventricular septum.
Right ventricular hypertrophy.
RV outflow obstruction : various sites , but most common is infandibular site .
VSD large , non obstructive .Overriding of aorta ( right sided in 20% ).
Clinical featuresTime of onset of symptoms
Severity of cyanosisRV hypertrophy
Depend of the degree of right ventricular outflow obstruction
If mild initially heart failure with age , patient grows infandibular hypertrophy cyanosis develops in 1st year of life .
If severe obstruction cyanosis develops immediately after birth .
In older children , long standing dusky blue skin, grey sclera, engorged blood vessels, clubing of fingers & extracardiac manifestation.Dyspnea on exertion so they stop to take rest or have squatting position.
Growth retardation ( if severe and untreated ) .
Delayed puberty .
O/E
Pulse normalVenous and arterial pressure normal .
Heart size normal .
Lt. hemithorax bulged because of RVH.
Murmur , ejection systolic because of RV outflow obstruction .
Murmur can be holosystolic due to VSD.
The intensity of murmur during spells .
Sometimes continuous murmur due to collaterals.
Diagnosis
• CXR : boat shaped heart , clear lung field , 20 % right sided aorta .
• ECG : RVH , right axis deviation .
• ECHO
• Cardiac cathetarization .
• Selective right ventriculography : important for child as surgical candidate .
• Lt. ventriculography .
• Coronary angiography .
Complications
• Cyanotic spells• Cerebral thrombosis
• Brain abcess
• Infective endocarditis
• Heart failure
Cyanotic spell
Usually at 4-6 mo.Patient restless , cyanosed , gasping , syncop follows .
Mainly after awakening or vigorous exercise .
intensity of the murmur.
Continued for few min.-few hrs .
Followed by generalized weakness , sleep.
Treatment of spell
• Put him on abdomen , knee-chest position.
• O2 .
• Morphine ( 0.2mg/kg s.c ) relaxe pulmonary infandibulum and sedate child .
• Premature attempts to get blood sample agitation.
• If severe NaHCO3 to correct acidosis .
• If still resistant phenylephrine or methoxantheme to systemic vascular resistance and Rt. Lt shunt .
Treatment
Medical :• If severe obstruction medical Rx until surgical intervention.
• Include
• Provide O2 , maintain body temperature .
• Treat and prevent hypoglycemia .
• Start PGE1 infusion
• If less severe obstruction and while await for the surgery observe for the following:
Rx dehydration.
Rx iron deficiency anemia .Inderal 0.5-1 mg/kg 6hr.
Phlebotomy if symptomatic patient and hematocrite > 65%.
Surgical Rx.
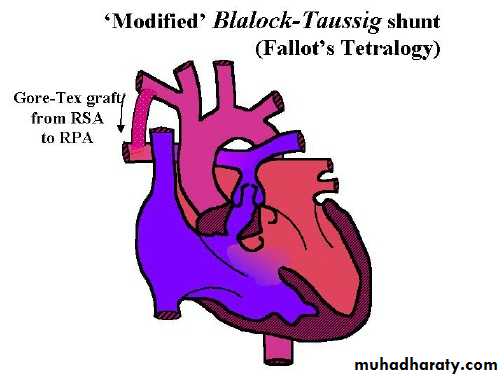
2 options : palliative
corrective
Time : 4-12 mo.
Palliative surgeryModified Blalock – Taussing shunt , which a conduit from subclavian artery to homolateral branch of pulmonary art. or directly from ascending art. To main pulmonary artery .
Response cyanosis , continuous murmur heard from functioning anastomosis .
With increasing age need for more pulmonary blood flow do corrective surgery or reanastomose on the opposite site
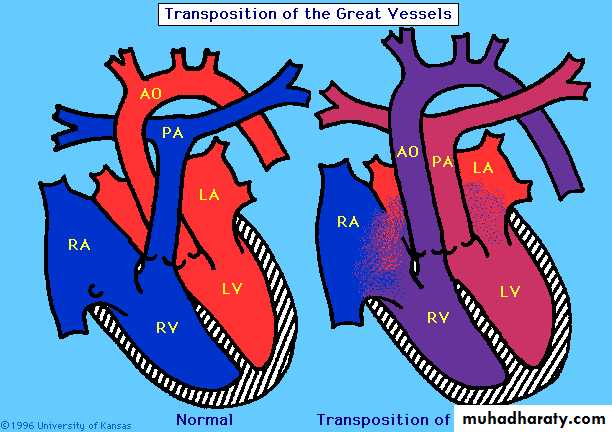
Transposition of great vessels
CCHD with pulmonary blood flow .Either d-TGA or l-TGA.
Either with intact VS or VSD.
Male > female .
50% with VSD .
For d- TGA aorta arises from RV and pulmonary art. From LV .
Aorta anterior and to the right of pulmonary art.
C/F: cyanosis & tachycardia .HF less common
if untreated not survive neonatal period .
Dx
ECG Rt. Sided dominance pattern.
CXR mild cardiomegaly.
Hyperoxia test.
ECHO.
CATHETRIZATION.
Treatment
Infusion of PGE1Protect against hypothermia , Rx acidosis & hypoglycemia .
If no response Rashkind Balloon septostomy then arterial switch operation ( Jantene operation ) within 2 wks.
If TGA&VSD do Rashkind operation.
Extracardiac manifestation of CCHD.
• Polycythemia .• Relative anemia .
• CNS abcess.
• CNS thromboembolic stroke.
• Low grade DIC , thrombocytopenia.
• Hemoptysis .
• Gum disease .
• Gout .
• Arthropathy , COF.
• Infection .
• Pregnancy complications .
• FTT.
• Psychosicial problems .
Thank you
TETRALOGY OF FALLOT(TOF)
It is the commonest cyanotic congenital heart disease in children and adults
It is a combination of:
1-VSD
2-Pulmonary stenosis (PS).
3-Overriding of aorta.
4-Right ventricular hypertrophy (RVH).
HEMODYNAMICS: The degree of right ventricular outflow obstruction (i.e. P.S.) determines the degree of pulmonary blood flow and the severity of cyanosis.
C/F:
1-Cyanosis: most patients develop cyanosis in the first 6 month - 1 year of life.2-Dyspnoea: occurs in exertion, so they have a limited exercise tolerance.
3-Squatting: it is the characteristic posture of children with TOF after any physical effort.
Q/E:
1-Cyanosis (central and peripheral).
2-Clubbing (usually after 3 months of age).
3-Single S2 & ejection systolic murmur at the left sternal border.
4-Normal pulse & quiet procardium.
INVESTIGATION:
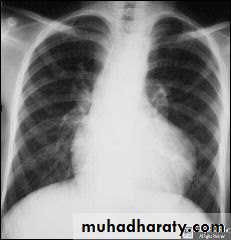
ECG: Right axis deviation (RAD) & right ventricular hypertrophyCXR:
1-Normal heart size.
2-Rounded apex situated above the diaphragm (hypertrophied RV).
3-Concavity at the main pulmonary artery area.
4-Reduced pulmonary vascularity (oligemic lung).
The classical radiological picture of TOF is called (boot shape).
Echo: It is essential for Dx.
Catheterization: Gives the definitive Dx and as a preoperative step.
COMPLICATIONS:
1-Hypercyanotic spells.
2-Cerebrovascular accidents (CVA).
3-Cerebral abscess.
4-Infective endocarditis.
5-Haematological complications include bleeding and thrombosis. All complications are essentially due to cyanosis & polycythemia.
6- Polycythemia is due to hypoxia which results from right to left shunt (as the right pressure grows higher than the left one).
RX:
1. Medical:
a. Rx of anemia by iron, sometimes considered as relative anemia if wefind normal Hb level; also nutritional support.
b. Phlebotomy: in symptomatic patients with hematocrit more than 65%(as there is a risk for CVA).
2. Surgical:
a. Palliative to pulmonary blood flow e.g.: Blalock-Taussig shunt (BT shunt).
b. Total surgical repair.
Indications for surgery:
1-Cyanosis2-Hypecyanotic spells
3-Polycythemia
4-↓ exercise tolerance
5-Appropriate age and weight (usually between 2-3 years, if there is cyanosis).
HYPER.CYANOTIC SPELLS:
Attacks of increasing cyanosis associated with abnormal respiration and altered level of consciousness and it is an important cause of death in TOF patients (especially in mild cyanosis)
.
Spells are particular problems during the 1st 2 years of life and is more common in the morning and can be precipitated by any activity. Most spells are self-limited, but should be considered as an indication for surgery.
The cause is infundibular spasm.
RX:
1-Knee-chest position.
2-O2.
3-Sodium bicarbonate to correct metabolic acidosis.
4-Morphine: 0.2 mg/Kg subcutaneously (s.c.) or i.v. can be repated 4 hourly.