Fever without a focus(Pediatric Mystery)
University Of Baghdad
College of MedicineDept. Of Pediatrics
5th Year
Infectious Diseases Module
LEARNING OBJECTIVES
1- Define fever and FUO.2- Put a differential diagnosis.
3- Master a panel of investigations.
4- Decide when to start empirical therapy?
MCQ
The commonest cause of PUO is:
A- A common disease presenting in an atypical way.B- A rare disease presenting in atypical way.
C- A common disease presenting typically.
D- A rare disease presenting typically.
• A 10 - year old female, presented to the outpatient clinic with a 4 - week history of fever (38.3 C – 39.5 C) and easy fatigability. She underwent a good primary work up by the family physician prior to referral with failure to reach a diagnosis. She is sitting now with her worried parents in the desk next to you and ready to receive your questions and actions.
1- How you define this complaint in view of duration?
2- Put a differential diagnosis inside a general frame?
3- What shall you ask in the context of history?
4- What are the general and special sites you look for in physical examination?
5- Set a panel of investigations you are planning to perform?
6- Start a treatment plan?
• A 10 - year old female, presented to the outpatient clinic with a 4 - week history of fever (38.3 C – 39.5 C) and easy fatigability. She underwent a good primary work up by the family physician prior to referral with failure to reach a diagnosis. She is sitting now with her worried parents in the desk next to you and ready to receive your questions and actions.
1- How you define this complaint in view of duration?
DEFINITIONS
Fever: A rectal temperature of ≥38 C. It fluctuates in degree and timing.FWLS (Fever without localising sign): Fever of acute onset, with duration of <1 wk and without localizing signs.
FUO (Fever of unknown origin): Fever documented by a health care provider and for which the cause could not be identified after 3 wk of evaluation as an outpatient or after 1 wk of evaluation in the hospital.
• Axillary 36 - 37.4 C
• Oral 36.7 - 37.7 C• Rectal 36.9 - 37.9 C
Range of normal temperature
PATHOGENESIS
• Regulators:
• 1- Thermo sensitive neurons in pre-optic and anterior hypothalamus
• 2- Blood temperature
• 3- Receptors in skin and muscles
• Mechanisms:
• 1- Pyrogens (endogenous and exogenous)
• 2- Heat production exceeding loss
• 3- Defective Heat loss
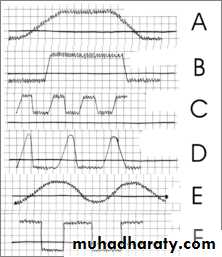
Continuous: Temperature remains above normal throughout the day and does not fluctuate more than 1 °C in 24 hrs
Typhoid, lobar pneumonia,
Remittent: Temperature remains above normal throughout the day and fluctuates more than 1 °C in 24 hours
SBE
Intermittent: The temperature elevation is present only for a certain period, later cycling back to normal
Kala Azar
Undulant: fever is typically undulant, rising and falling like a wave Brucellosis
Relapsing: multiple episodes of fever occur and each may last up to 3 days. Individuals may be free of fever for up to 2 weeks before it returns. Tick borne
Remember the sequelae
SIR
• A 10 - year old female, presented to the outpatient clinic with a 4 - week history of fever (38.3 C – 39.5 C) and easy fatigability. She underwent a good primary work up by the family physician prior to referral with failure to reach a diagnosis. She is sitting now with her worried parents in the desk next to you and ready to receive your questions and actions.
2- Put a differential diagnosis inside a general frame?
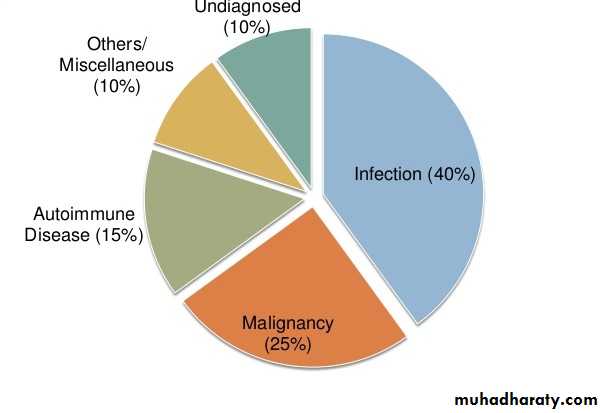
between 5 and 15% of FUO cases defy diagnosis, despite exhaustive studies.
CAUSES• 1- Infections:
• Bacterial
• Systemic: Brucellosis, Salmonella, Tuberculosis
• Localized infections: Osteomyelitis, Pneumonia and Sinusitis
• Viruses: CMV, Hepatitis viruses ,HIV, IM (Epstein-Barr virus)
• Parasitic Diseases: Malaria ,Toxoplasmosis
Fungal diseases
CAUSES
• 2- Rheumatologic diseases
• JRA, Rheumatic fever, SLE and drug fever.
• 3- Neoplasms
• Leukemia, Lymphoma, other malignancies.
• 4- Miscellaneous
• Familial Mediterranean fever, Kawasaki disease.
• 5- Undiagnosed
Always look for
• Abscesses: Abdominal, brain, dental, hepatic, pelvic, perinephric, rectal, subphrenic, psoasCAUSES
APPROACH• The Best Approach
• “there is no substitute for observing the patient, talking to him and thinking about him”
• A 10 - year old female, presented to the outpatient clinic with a 4 - week history of fever (38.3 C – 39.5 C) and easy fatigability. She underwent a good primary work up by the family physician prior to referral with failure to reach a diagnosis. She is sitting now with her worried parents in the desk next to you and ready to receive your questions and actions.
3- What shall you ask in the context of history?
HISTORY
Fever specifications, sweating, antipyretics use and response, appearance, other complaints (CNS, urinary,,,,), pain (severity, site), rash and distribution, arthralgia / arthritis, travel, contact, animals, medications, hospitalization, immunizations, ethnicity, exposure to contaminated food or water.
• A 10 - year old female, presented to the outpatient clinic with a 4 - week history of fever (38.3 C – 39.5 C) and easy fatigability. She underwent a good primary work up by the family physician prior to referral with failure to reach a diagnosis. She is sitting now with her worried parents in the desk next to you and ready to receive your questions and actions.
4- What are the general and special sites you look for in physical examination?
CAREFUL PHYSICAL EXAMINATION
General appearance and vital signs (heart rate, pressure, respiratory, temperature), pallor, jaundice, clubbing, skin and scalp, eyes, sinuses, oropharynx, LN, abdomen, musculoskeletal, genitourinary.• A 10 - year old female, presented to the outpatient clinic with a 4 - week history of fever (38.3 C – 39.5 C) and easy fatigability. She underwent a good primary work up by the family physician prior to referral with failure to reach a diagnosis. She is sitting now with her worried parents in the desk next to you and ready to receive your questions and actions.
5- Set a panel of investigations you are planning to perform?
INVESTIGATIONS
Level 1:
CBC differentials, ESR, CRP, metabolic panel (RFT, LFT, elects), GUE, stool, C/S, LP, CXR, US, TB, EBV, CMV, cultures.INVESTIGATIONS
Level 2:
Echo, CT, Bone scan, Serology, Autoimmune, Bone marrow
INVESTIGATIONS
Level 3:
Tissue biopsy, EndoscopyINVESTIGATIONS
• avoid indiscriminately ordering a large battery of tests.• A 10 - year old female, presented to the outpatient clinic with a 4 - week history of fever (38.3 C – 39.5 C) and easy fatigability. She underwent a good primary work up by the family physician prior to referral with failure to reach a diagnosis. She is sitting now with her worried parents in the desk next to you and ready to receive your questions and actions.
6- Start a treatment plan?
Treatment
• in general,• NONE
• Until diagnosis
Treatment
• You should know that
• 1. most children will get better
• 2. most children have common illnesses
• 3. it hasn’t killed them yet! So do not rush to antibiotic treatment.
Treatment
• Admit• 1- Reliability
• 2- Toxicity
• 3- Invasive investigations
Treatment
• Empirical therapy (little or no role in cases of classic fever of unknown origin) is indicated only in:• 1- Nonsteroidal agents in presumed JIA
• 2- Antituberculosis drugs in critically ill children with possible disseminated TB
• 3- Clinically deteriorating with suspicion of bacteremia or sepsis.
• 4- Immunocompromised
• Antibiotics if used should be at targeted disease rather than blanket therapy with 4-5 antibiotics.
FUO is more likely to be an unusual presentation of a common disorder than a common presentation of a rare disorder.
Giving antibiotics to a child with FUO is like shooting a gun into dark room
Take home message
SUMMARY OF DEFINITIONS
FEATURECLASSIC FUO
Definition
>38.0°C, >3 wk, >2 visits or 1 wk in hospital
Patient location
Community, clinic, or hospital
Leading causes
infections, inflammatory conditions, Cancer, undiagnosed, habitual hyperthermia
History emphasis
Travel, contacts, animal and insect exposure, medications, immunizations, family history, cardiac valve disorder
Examination emphasis
Fundi, oropharynx, temporal artery, abdomen, lymph nodes, spleen, joints, skin, nails, genitalia, rectum or prostate, lower limb deep veins
Investigation emphasis
Imaging, biopsies, sedimentation rate, skin tests
Management
Observation, outpatient temperature chart, investigations, avoidance of empirical drug treatments
Time course of disease
Months
Tempo of investigation
Weeks
Infections
Oncology
Rheumatology