Laparoscopy & Hysteroscopy
The single most important change in gynecological surgical practice over
the last 20–30 years is the endoscopic surgery.
(
للدرس
و
للفهم
)
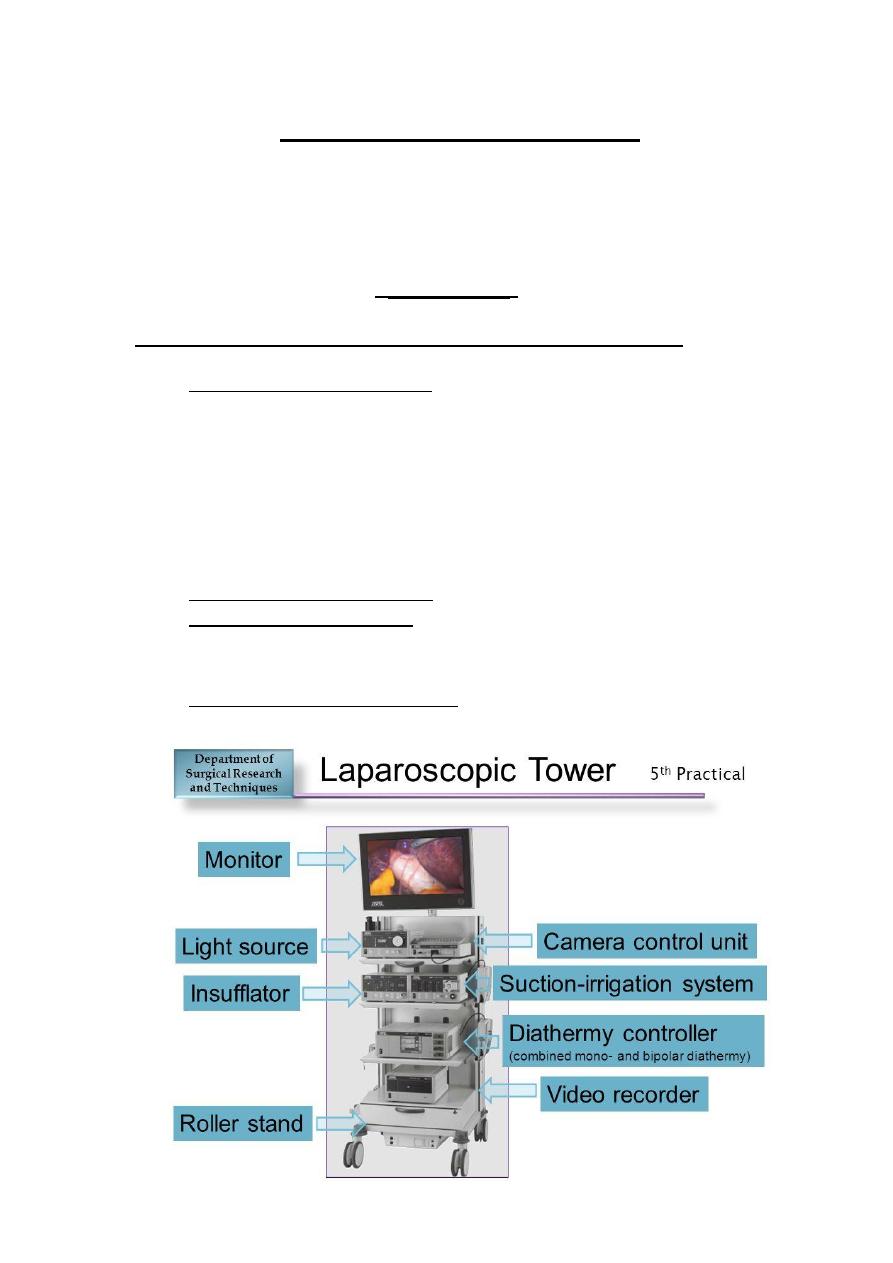
Equipments common to hysteroscopy and laparoscopy:
o
Light Source and Light Head: Laparoscopy requires a brighter light
to sufficiently illuminate a larger cavity at a greater distance
compared with hysteroscopy, and the same is true in the presence
of bleeding as blood absorbs light. Light leads are of two types:
fiber optic or liquid. The former are more common because they
are cheaper, but the fibers are prone to breaking with gradual
deterioration in light transmission.
o Camera and Moniter System
o
Electrosurgical generator: used for haemostasis or cutting, and
has be bipolar, monopolar cutting and monopolar coagulation.
o
Photo and Video Documetation
Equipment for hysteroscopy:
o HYSTEROSCOPES: Both rigid and flexible hysteroscopes are
available, the majority of gynecologists preferring the former
because the image tends to be superior. Rigid hysteroscope have
a rod-lens optical system, and it is of different sizes (4 and 2.9 mm
being popular sizes), and angles of view at 0, 12, 15, or 30 degree
angles of view.
o UTERINE DISTENSION: The uterine cavity is a potential space and
has to be distended at relatively high pressure to afford a view. To
achieve this, gas (CO2), low-viscosity fluids (e.g. N/saline, 5%
dextrose, 1.5% glycine, 3% sorbitol, 5% mannitol) or high-viscosity
fluid (e.g. Hyskon, which is 32% dextran 70 in dextrose) can be
used. Diagnostic hysteroscopy is typically done using CO2 or
N/saline, operative hysteroscopy with mechanical instruments or
laser with N/saline, and resectoscopic surgery with electrolyte
free solutions such as glycine, sorbitol or mannitol. The pressure
required to provide an adequate view of the uterine cavity
depends on a number of factors, but tends to be around 100
mmHg.
o MECHANICAL INSTRUMENTS: scissors, grasping and biopsy forceps
and monopolar electrodes can be used with operating sheaths for
minor procedures such as target biopsy or polypectomy
o RESECTOSCOPE: The modern resectoscope consists of five
components the optic, handle mechanism, inflow and outflow
sheath and an electrode for polypectomy, myomectomy,
endometrial resection, endometrial ablation, and metroplasty.

Equipment for laparoscopy:
o LAPAROSCOPES: As with rigid hysteroscopes, most laparoscopes
are built around a rod-lens system and come in a number of
diameters (3–12 mm) and angles of view [0–30 degree], with 10
mm degree scopes being the most widely used.
o VERESS NEEDLE: Traditionally, gynecologists use a Veress needle
to insufflate the abdomen with gas at the start of laparoscopy.
The usual insertion point for the Veress needle is the inferior
border of the umbilicus, A well-recognized alternative to
subumbilical insufflations is the use of Palmer’s point, which is
situated in the left mid-clavicularline approximately 3 cm below
the costal margin. The left upper quadrant of the abdomen is the
area least likely to be affected by adhesions, so Palmer’s point is
useful when there is a concern about possible lower abdominal or
peri-umbilical adhesions (e.g. midline laparotomy incision,
appendicitis). Palmer’s point is also useful when dealing with a
large pelvic mass.
o TROCARS AND CANNULAE: Trocars and cannulae act as a conduit
for the laparoscope and other instruments. They come in a variety
of sizes depending on the diameter of the instrumentation to be
accommodated, with 5 mm and 10–12 mm ports being the most
commonly required.
o LAPAROSCOPIC INSUFFLATOR: These pumps control intra-
abdominal pressure rather than flow of CO2, and this should be
set at 12–15 mmHg; a higher pressure of up to 25mmHg is
acceptable during the set-up phase as this has the effect of
increasing the distance between any trocar being inserted and
bowel or large blood vessels, thereby in theory at least, reducing
the risk of injury.
o SUCTION/IRRIGATION PUMP: can be used to aspirate blood and
clean the pelvis, ovarian cysts can be quickly deflated, ectopic
pregnancies sucked out.
o ANCILLARY INSTRUMENTS: If the laparoscope is the eye of the
surgeon, grasping forceps are the surgeon’s hands. Bipolar
forceps should always be available for haemostasis. Pre-tied loop
sutures, suture carriers and needle holders should be available for
major procedures both for haemostasis and repair. One or two
ancillary ports are inserted in the lower abdomen. Injury by the
ancillary ports can be minimized by inserting them under direct
vision having identified the deep and superficial epigastric vessels
and the bladder. A useful concept here is that of the ‘safe
triangle’ which is bounded by the umbilical ligaments (remnants
of the umbilical vessels) laterally with the symphysis pubis as its
base and the umbilicus as its apex; although the position of the
inferior epigastric vessels can be variable, their course is always
lateral to the safe triangle. Ports should therefore be placed either
inside the safe triangle or lateral to the inferior epigastric vessels.a
(
من
هنا
للفهم
والحفظ
)
(DIAGNOSTIC HYSTEROSCOPY)
Diagnostic hysteroscopy has become a basic investigation in modern
gynecology and has essentially replaced the time honored D & C
(dilation and curettage). It can be done as an outpatient procedure, and
is an integral component of a One-Stop approach to the management of
menstrual symptoms.
Indications to diagnostic hysteroscopy:
Abnormal menstruation (age >40 years)
Abnormal menstruation not responsive to medical treatment (age
<40 years)
Intermenstrual bleeding (IMB) despite normal cervical smear
Post coital bleeding (PCB) despite normal cervical smear
Post menopausal bleeding (PMB) (persistent or endometrial
thickness ≥4 mm)
Abnormal pelvic ultrasound findings (e.g. endometrial polyps,
submucous fibroids)
Subfertility
Recurrent miscarriage
Asherman’s syndrome
Congenital uterine anomaly
Lost intrauterine contraceptive device (IUCD)
Complications of diagnostic hysteroscopy:
Diagnostic hysteroscopy is a safe procedure, and complications are
uncommon. Perhaps the most frequently seen problem is:
pain when negotiating the cervix or distending the uterine cavity,
and a vaso-vagal reaction to cervical dilatation (can be solved by
giving local anaesthesia)
Uterine perforation in extreme cervical stenosis can occur; in this
situation, insertion of the hysteroscope under ultrasound
guidance is a useful ploy, as may be prior priming with a
prostaglandin.
Infection and excessive bleeding are rarely seen.
Contraindications to diagnostic hysteroscopy:
Pelvic infection
Pregnancy
Cervical cancer
(OPEARATIVE HYSTEROSCOPY)
Hysteroscopic surgery has a number of well-defined indications and is
the treatment of choice for polypectomy, myomectomy for intracavitary
or submucous fibroids, adhesiolysis and metroplasty.
Indications of operative hysteroscopy:
Polypectomy
Endometrial sampling
Removal of intrauterine contraceptive device
Proximal fallopian tube cannulation
Asherman’s syndrome treatment
myomectomy
Division/resection of uterine septum
Endometrial resection or ablation
Complications of operative hysteroscopy
Early
Uterine perforation
Fluid overload
Haemorrhage
Gas embolism
Infection
Cervical trauma
Late
Intrauterine adhesions
Haematometra (after endometrial ablation)
Post ablation sterilization syndrome (after endometrial ablation)
Pregnancy (after endometrial ablation).
Cancer (after endometrial ablation)
(DIAGNOSTIC LAPAROSCOPY)
It is usually done as an inpatient procedure under general anesthesia.
Indications for diagnostic laparoscopy;
Acute or chronic pelvic pain
Ectopic pregnancy
Pelvic inflammatory disease (including TB)
Endometriosis
Adnexal torsion
Subfertility
Congenital pelvic abnormality
Abnormal pelvic scan
Unexplained pelvic mass
Staging for ovarian malignancy
Contraindications for diagnostic laparoscopy
Mechanical or paralytic bowel obstruction
Generalized peritonitis
Diaphragmatic hernia
Major intra-peritoneal hemorrhage (e.g. shock)
Severe cardio-respiratory disease
Massive obesity
Inflammatory bowel disease
Large abdominal mass
Advanced pregnancy
Multiple abdominal incisions
Irreducible external hernia
Complications of diagnostic laparoscopy:
Diagnostic laparoscopy is a safe procedure with published
complication rates of 2–4 per 1000. Most complications occur during
the set-up phase of the procedure when the abdomen is being
instrumented (e.g. injury to the inferior epigastric vessels or major
retroperitoneal vessels, bowel injury). Injury to retroperitoneal vessels
usually requires immediate laparotomy, whereas bowel injury can be
managed laparoscopically provided the perforation is small and there is
minimal fecal soilin
(OPERATIVE LAPAROSCOPY)
Indications for operative laparoscopy:
Sterilization
Aspiration of ovarian cyst
Ovarian biopsy
Division of adhesions
Linear salpingotomy or salpingectomy for ectopic pregnancy
Ovarian cystectomy
Treatment of endometrioma
Salpingo-oophorectomy
Ovarian drilling with laser or diathermy for polycystic ovaries
Treatment of endometriosis
Myomectomy for pedunculated subserous fibroid
Laparoscopic utero-sacral nerve ablation (LUNA)
Laparoscopically assisted vaginal hysterectomy (LAVH)
Total laparoscopic hysterectomy
Myomectomy for intramural fibroids
Pelvic and aortic lymphadenectomy
Pelvic side wall and ureteric dissection
Presacral neurectomy
Incontinence procedures
Prolapse of genital organs procedures
Complications of laparoscopic surgery:
Intra operative:
Bowel injury
Vascular injury
Bladder injury
Ureteric injury
Surgical emphysema
Anaesthetic complications
Post operative:
Unrecognized visceral or vascular injury
Venous thromboembolism
Infection
Port site hernia
