
Nutritional Requirements
in
Different
Age Groups
Objectives:
q
Nice to know the related definitions,
physiological changes in old age,
q
Have to know the food guide pyramids for
pregnant, lactating, adolescents, RDA in old age &
specific nutritional requirements in different age
groups, common nutritional problems during
childhood & adolescent period.
The fetus is most vulnerable to nutritional deficiencies
in 1
st
trimester of pregnancy.
Poor maternal nutrition before pregnancy has both:
§Immediate effect(LBW) &may continue with retarded
growth during childhood.
§long term consequences (CVD &type II D.M.)
Dietary changes can the mother made to giving birth to
a healthy infant;
o
Take folic acids supplements to protect against
neural tube defects.
o
Choose foods rich in folic acid; >100µg eg. Kale
& spinach.
Pre& periconceptional
nutrition in women
o
Maintain ideal wt. at preconception (3m. Before
conception);
** obesity (BMI 30) can inhibit ovulation
** underwt. (BMI<18.5) at preconception can
increase the risk of pre term delivery.
o
Avoid excessive intake of retinol (β-carotene is not
toxic), avoid vit.A supplements (drugs or
oint.), liver, sausage (8000-10000µg).
o
Giving up smoking& drinking alcohol.
Nutritional Requirements During
Pregnancy :
v The RDA suggest increase of all nutrients
except Vit. A, D, Ph, florid.
v Separate dietary recommendations for adolescent pregnant.
v Adolescent pregnant more prevalent to an iron deficiency.
v Malnutrition during 1
st
trimester can cause irreversible
damage to brain and spinal cord, heart, liver, kidneys, etc.
v A woman who enters pregnancy weighing >20% of her
ideal body weight for her height is at a higher risk for
gestational diabetes & hypertensive disorders.
v Pregnancy is NOT the time to reduce extra wt.
v Sweet should consume in moderation to avoid excessive
weight gain.
ü CHO requirements:
not less than 200 gm / day, to prevent ketosis &excessive
protein breakdown.
ü Fats & Essential fatty acids requirements:
*
4.5% of caloric intake in form of EFA
is recommended.
ü Caffeine:
It can rapidly crosses the human placenta & enters the fetal
circulation.
The fetus & neonate appear to lack the enzymes that
necessary to demethylate the caffeine.
It is present in high concentration in:
o
coffee (45-155mg/cup)
o
tea(9-50mg/cup)
o
cola(30-65mg/cup)
Soft beverages not more than 300mg/day or 2 cups.
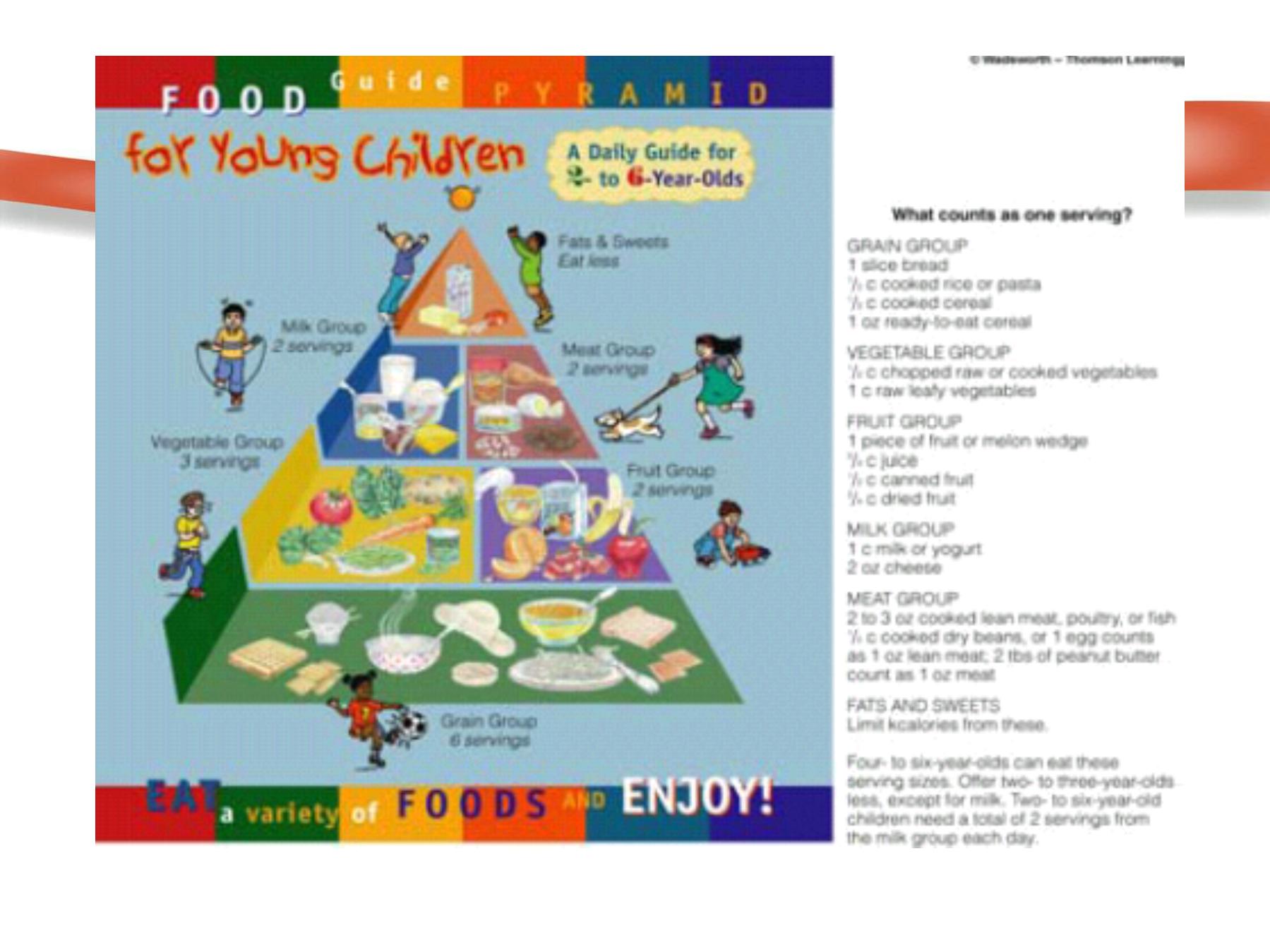
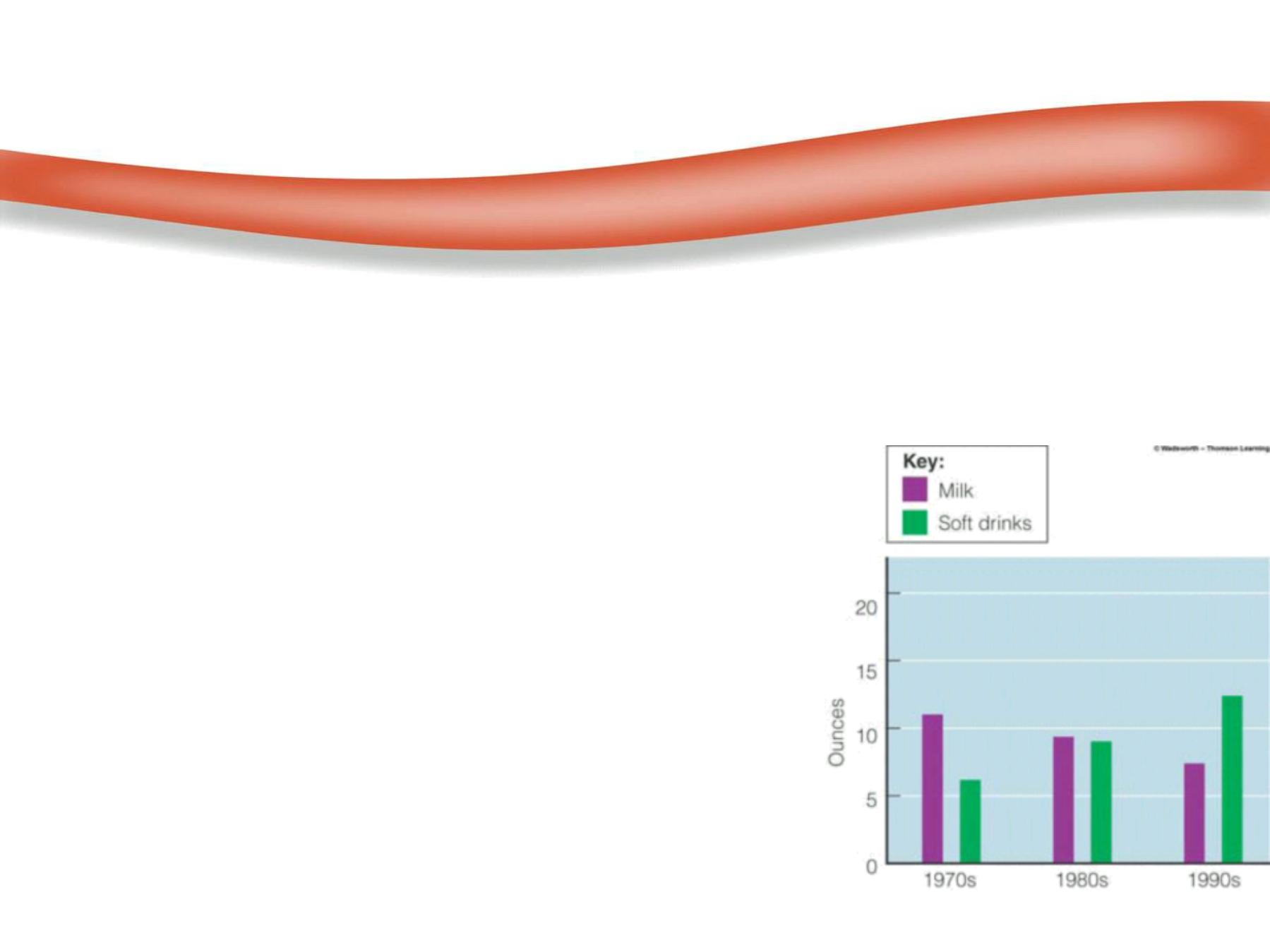
Changes in the daily Food Guide pyramid
during pregnancy & lactation:
Non pregnant
pregnant or
adolescent preg.
lactating
& lactating
*Milk group
2-3servings
3-4servings
5servings
*
Meat group
2-3servings
3-4servings
4
=
*Fruits
2-4servings
3-4servings(1-2 citrus)
*vegetables
3-5servings
4-5servings
(1-2 green leafy veg.)
*Bread group
6-11 servings
7-11 servings
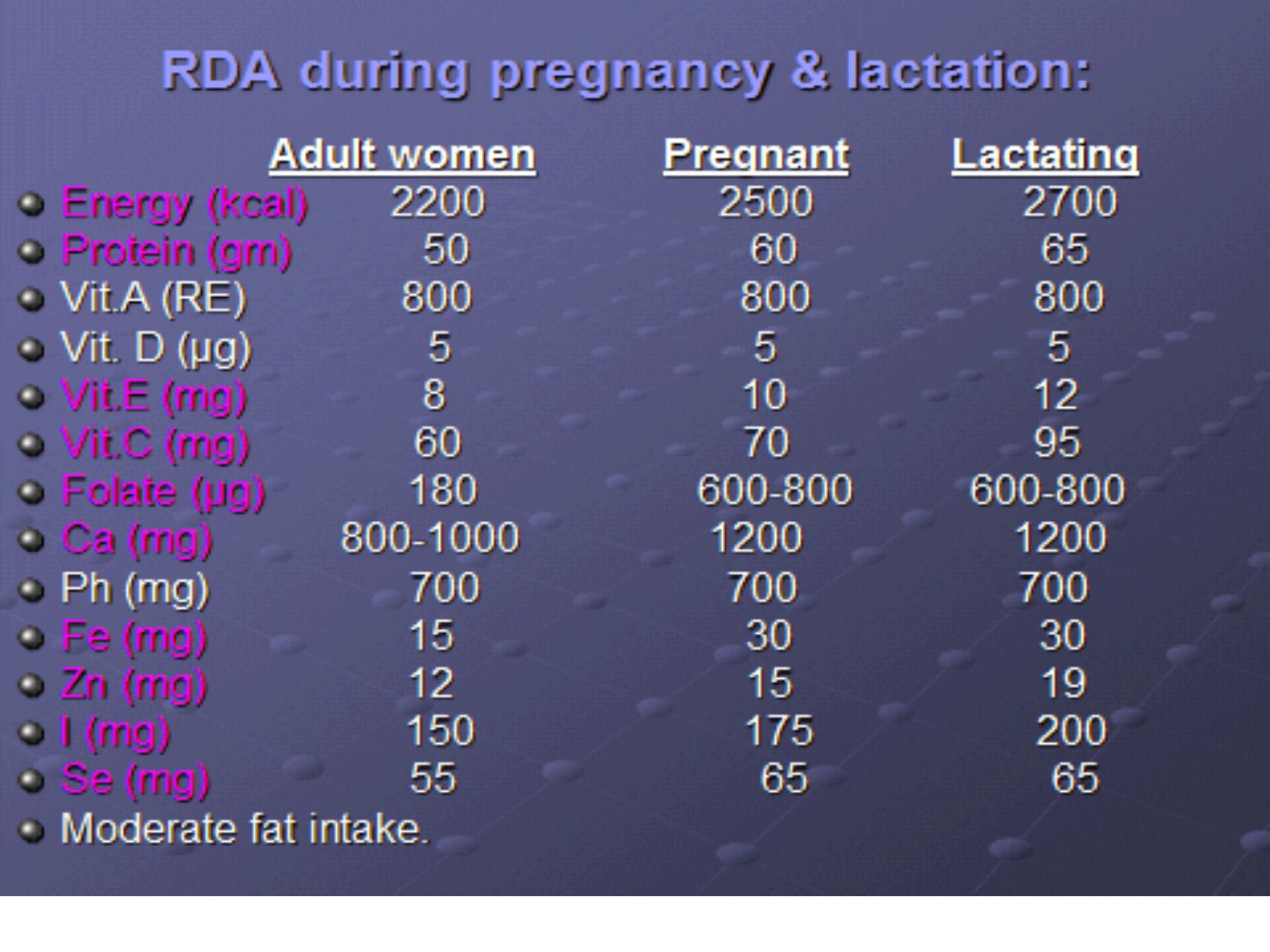
Nutrition during lactation:
To produce sufficient milk the mother has to
§Eat a well balanced diet with special emphasis on
critical nutrients, (Severe malnutrition in mother reduces
quantity of milk but not quality of milk).
§Ca, Fe, water sol. vit., with a very little alteration in the
normal diet.
§The iron supplementation to replace the depleted
stores from pregnancy& delivery.
§More water& fluids intake 8-10cups/d
(additional 700ml).
§3-5gm/day of EFA required for lactation.
§It may be a good time for over weight mother
to lose weight, by moderate dietary restriction.
For the 1st 6ms of life;
üExclusive breast feeding
, as often as
the child wants, day &night, at least 8x/d.
üGrowth monitoring
is important monthly during 1
st
y.
üEnergy requirement:
up to 120Kcal/kg/d.
üProtein requirement:
2-2.5gm/kg/day
(
35%
of total caloric intake).
üCHO :
50% of total calories.
•Starchy foods should be avoided (amylase enzy.
which digest starch is low during1
st
4-6m of life).
•Major CHO source is lactose which incr. absorption
of dietary Ca &Mg.
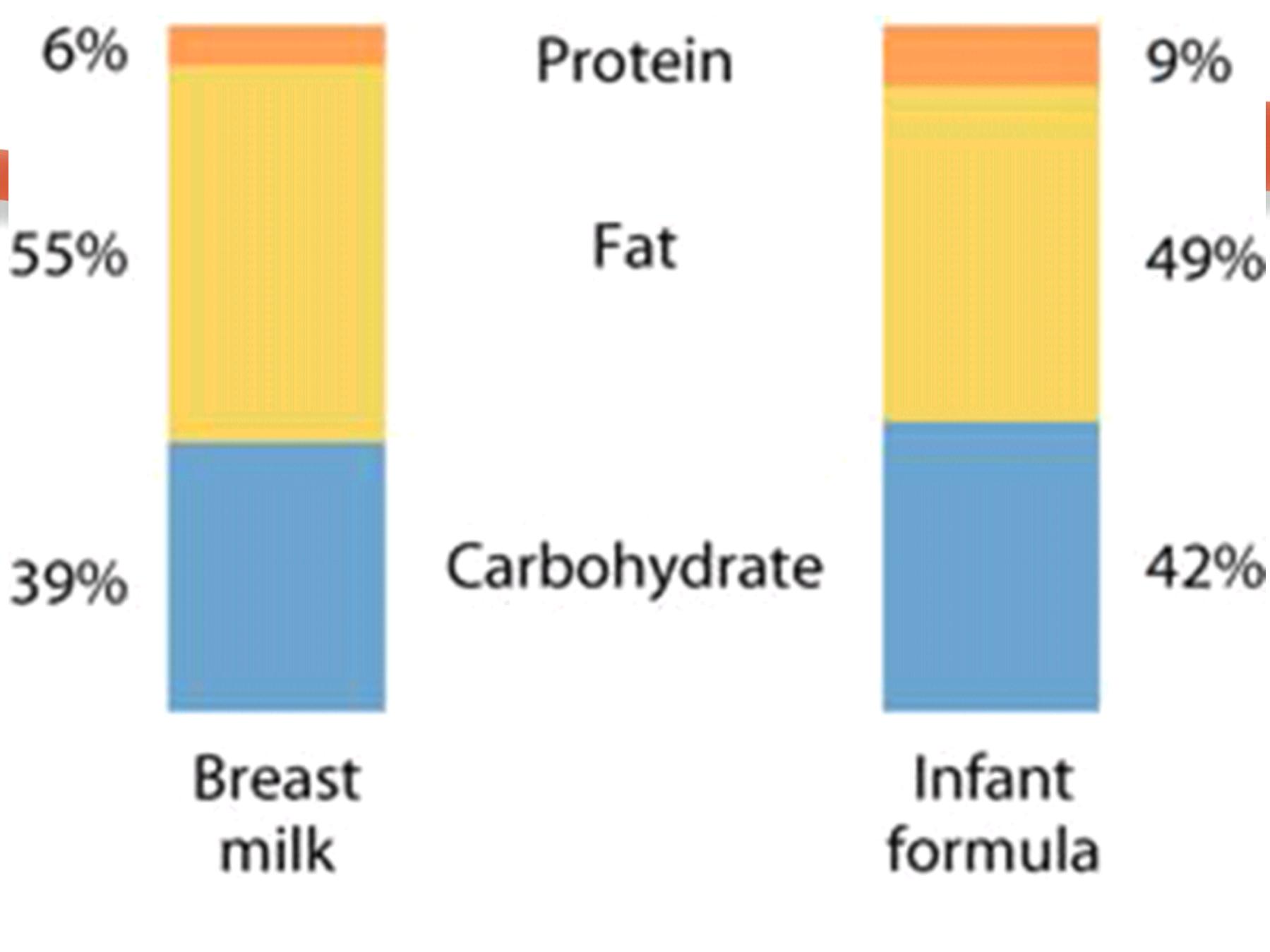
Nutritional Requirements During infancy:

ü
Lipids:
play a role in absorption of
fat sol. vit.& as a source of E.F.A.,
The milk provides E.F.A. & PUFA.
Infant formula containing only 2% of total EFA.
ü
Vitamins& minerals:
**Vitamin K
is routinely administered 0.5-1mg i.m. or oral
to protect them against hemorrhagic diseases .
**
Vit. D
:
o
In exclusive B.F. infant & adequate exposure to
sunlight there is no need for vit D supplementation
during 1
st
6m.
o
If no sunlight exposure 400IU/day vit.D
supplementation.
**V.A:
100 000IU with measles vaccine.
**Iron:
store can last up to 6m of age (start the
complementary feeding).
Oral dose of 1mg/kg/d as prophylactic.
**Fluoride:
for teeth growth
(from diet or fortified water
=fluoridated).
üWater:
1.5ml/ Kcal,
(under ordinary circumstances)
breast milk supply sufficient water & no
need for extra water.
vCan only give other foods if:
-The infant not gaining wt.
-Appear hungry after breast feeding.
Given 1-2x/d after B.F
.( one or more of food listed under
6-12m.)
Breast milk
;
-Contains all the vitamins and minerals that an infant
needs (but is low in vit D, so may need to supplements
after 6m.).
–carbohydrates, proteins, fats are already predigested
for absorption.
–very high in omega-3 fats.
–the iron, zinc, and magnesium in breast milk is highly
absorbable.
–low in sodium.
–Calcium to phosphorus ratio is 2:1, which enhance
calcium absorption.
If breastfeeding is not possible, an iron fortified infant
formula should be used to prevent iron deficiency
anemia.
Cow’
s milk is not recommended because:
–Protein is poorly digested in newborns& can cause
GI upset.
–Too high in sodium.
–Very low in iron and vit C.
–Can cause failure to thrive because of the
overall lack of nutrients in cow’
s milk.
Complementary feeding:
Addition of semisolid foods is desirable, which provide
iron & other nutrients esp. vit. C.
For the past few decades there has been a trend
towards earlier introduction of solid foods, often after
4-6wks of life. While the current recommendation is to
delay until 6ms of age.
§Each type should be given separately for about week
to avoid allergy or intolerance.
§Start with iron fortified cereals. Rice is the best to
begin with (less likely cause allergy).
§Fruits & vegetables are added next.
§No need to add sugar or salt at the beginning.
Feeding during 6-12m.:
§Breastfeed as the child wants.
§Give adequate servings of:
*Thick porridge made of rice, potato, milk with starch
*Can add sugar & oil or sesame oil after 8th month.
*Mixture of mashed foods; rice or potato with green
vegetables, beans, chicken, red meat, & finally fish.
•Give 3 meals /d if breastfed.
•Give 5 meals/d if not breastfed.
•Give nutritious snacks between meals like
egg yolk, banana or bread after 8
th
m.
•Allergy Foods: peanuts, seafood, cows milk, egg white.
Regular monitoring of wt. &ht./1 m. during 1
st
y. of life,
& /2m. during 2
nd
y. of life.
The growth during 1st year of life is very rapid( 3x BW &
50% incr. B.Ht.), but after 12m the growth speed is decr.
Adverse reactions to foods:
vMilk allergy: incidence of cow’
s milk protein allergy
1-3% in bottle-fed babies. Breast milk is ideal, also soy
protein milk appear to be tolerated by most of infants.
vWheat allergy = celiac disease: sensitivity to gluten (in
wheat, barley& oats) asymptomatic until 6m. of age.
vLactose intolerance=Lactase enz. def.
lactose hydrolyzed to glucose& galactose by lactase
enz., either;
**Genetic (inborn error)
**Acquired condition( following diarrhea of
any cause).
It is temporary state & reversible, treated by temporary
elimination of all lactose containing foods
.
CF during 1-2y.:
o
Breastfeed as often as the child wants.
o
Give adequate servings of; family foods + mixture of
mashed foods of rice, potato, cereals,
with meat----, beans, +green vegetables,
carrots+ add sugar &oil mixed with milk.
o
Give 3 meals/d +2 snacks.
o
Encourage to eat.
2y. & older:
*Family foods 3 meals/d +2 nutritious snacks.
*Encourage to eat.
Nutrition during childhood:
Prior to adolescence there is little
difference in yearly height increment betw.
both sexes, but boys wt. more than girls until about
11-13y when girls wt. is more.
üEnergy & protein
:
The needs vary according to the age, body size
(Ht.& wt.) & physiological activities.
Age
total Cal.
Cal/kg
total protein
protein/kg
1-3y
1300
102
16gm
1.2gm
4-6y
1800
90
24gm
1.1gm
7-10y 2000
70
28gm
1gm
ü Minerals & vitamins:
o
Preschool children are at risk for development of
IDA. (attention to good sources of iron foods).
o
Calcium should be adequate for bone mineralization
& growth maintenance (adequate milk & dairy
products intake).
o
Child should learn good food pattern during this
period.
o
Careful assessment of growth is important for early
diagnosis of malnutrition, 4x/y during 3rdy. & 2x/y.
during 4
th
& 5
th
y.
Common Nutritional Related
Problems Among Children:
qObesity; 1 in 4 children are now classified as obese.
Prevalence has increased 50% in children in last 10y.
qDental caries.
qIron deficiency anemia.
qHyperactivity due to lack of regular meals &
caffeinated beverages.
• Adolescent is a period between the
onset of puberty & adulthood(10-20y).
• Puberty is anabolic period with incr. in Ht.&wt.
• Rapid growth for girls betw.10-13y & for boys 12-15y
(last for 3y.).
• Nutrients need are greatest during the pubescent
growth spurt & gradually decrease as individual
achieve physical maturity.
• The nutritional needs of males and females of the
same age differ little in childhood but diverge after
the onset of the pubertal growth spurt.
• After puberty, the differences in nutrient needs
persist.
Nutrition During Adolescence:
ü Energy & protein:
Age
total Cal
Cal/kg
total protein
Boys 11-14y
2500
55
45gm
15-18y
3000
45
59gm
19-24y
2900
40
56gm
Girls
11-14y
2200
47
46gm
15-18y
2200
40
44gm
19-24y
2200
38
46gm
ü Vitamins & minerals:
All are needed in increased amount in proportion to
energy requirements.
Calcium, iron, zinc, are needed during growth spurt ;
§
Ca RDA 1200mg/d (from dairy foods =4 cups/d ).
§
Fe RDA 12mg/d for male &15mg/d for female.
§
Zn RDA 15mg/d for male &12mg/d for female, it is
necessary for growth & sexual maturity (from meat,
sea foods, eggs,& milk).
• Energy requirements more in due to increased
muscle mass.
• Body composition of females differ from males higher
body fat composition at onset of menstruation.
• Kcal needs are based on body composition (height
and weight), age, and physical activity.
Follow the
Adult Food Guide Pyramid:
v Snacks should be nutrients-dense to prevent wt. gain.
v Balance fast foods with fruits &vegetables high in
fibers.
v Do not skip breakfast
v Consume plenty of lean meats to increase iron and
protein consumption
v Consume at least 4 cups of low-fat milk to meet
calcium requirements
v Encourage healthy eating habits& lifestyle to prevent
adult onset of diseases related to nutrition e.g. CVD.,
DM, osteoporosis & cancer.
Nutrition Related Problems During Adolescence:
o
Obesity: 1 in 5.
o
Eating disorders: anorexia nervosa & bulimia.
o
Dental caries.
o
Iron deficiency anemia seen in
adolescent girls.
o
Calcium deficiency decrease in
bone size.
ü
Aging is a complex biological process, normal,
progressive& irreversible phenomenon
throughout adult life & is associated with incr.
prevalence of chronic diseases or degenerative
conditions eg. CVD, H.T., D.M., cancer, obesity, &
osteoporosis.
ü The process begins with the cessation of growth &
development & the changes that occur in body
composition, organ function & physical performance.
ü There is a general variability from person to person&
even within individuals when various organs may
age at different rates.
ü Elderly form 10-12% of population.
Nutrition & Aging:
Physiologic changes:
§Decline in total body K & N as age advances which is
indicative of a decr. In total body cell mass & skeletal
muscle.
§Decline in lean body mass with concomitant incr. in
total body fat with same body wt.,& centralized shift of
s.c. fat from the limbs to the trunk.
§Total body water is decr. which is significant for
detoxified metabolites &thermal regulation.
§Reduction of organs function& wt.; kidneys, lungs,
liver, bones 12% in males & 25% in females.
Factors affecting nutritional status
:
§Mal absorption &GI disorders:
The efficiency of digestion &absorption of nutrients is
affected due to reduced level of some enzymes.
§Metabolism:
**Decr. In BMR about 20% between 30-90y.
**Decr. of vit. D precursor with decr. Ca. absorption.
**Progressive impairment of CHO intolerance.
§Diseases: CVD, DM, HT& Cancer all may
modify nutrients requirements.
§Other factors: disability, inadequate or
improperly fitted dentures, poverty, social
& personal problems all affect nutritional status.
Ø Energy:
Depressed physical activity & decr. In lean body mass,
causes a reduction of energy needs.
For ages 51-75y, energy allowances decrease10%
( reduction of 300Cal/d for men & 200Cal/d for women).
For person over 75y, energy allowances decrease
another 10% of energy consumed by young adult.
Ø Protein:
It is necessary to maintain nitrogen balance in
elderly because of possible decrease in the
efficiency of digestion, absorption, & utilization of
dietary protein,
12-14% of total energy intake.
Nutrients Requirements:
Ø Other macronutrients:
ü Daily consumption of 15-25gm fat ( to ensure a
sources of EFA & carrier of fat sol. vit.).
ü
There is no RDA for CHO but not < 50-100gm /d of
total caloric intake (more complex CHO &less refined
sugars).
ü
Dietary fibers serve an important function in by
promoting the elimination of waste products,
moderate intake of dietary fibers (20-35g/d) from
fruits, veg.,& whole grains,& not rely on laxatives
.
Ø Micronutrients:
o
Most of nutrients needs for elderly are the same
except for thiamine& riboflavin which are
expressed in term of total caloric intake.
o
The needs for vit. D higher because of the reduction
capacity of their skin to produce 7-dehydro
cholesterol (precursor to convert inactive form to
active one)+ their limited exposure to sunlight.
o
Efficiency of calcium absorption is decr. with age
(osteoporosis) advisable to take 1200mg cal./d
o
Daily use of multivitamin-mineral supplements.
Advices:
o
Encourage to eat several (5–6) small non-fatty
meals (greater food varieties and lower body fat &
lower blood glucose and lipid levels)
o
Be physically active on a regular basis and include
exercises that strengthen muscles and improve
balance.
o
Avoid dehydration by regularly consuming
(especially in warm climates) fluids and foods with a
high water content.
30ml/kg of water/d (at least 1500 ml of fluid per day).
