Medical Nutritional Therapy
For
Renal Diseases & Gout

Objectives
•
Nice to know the relative definitions, kidney
function, pathophysiology, hidden sources of
sodium, high sod. Foods, high oxalate foods,
high purine foods.
•
Must know the medical nutritional therapy
goals, MNT of; nephrotic syndrome, chronic
renal failure, gout,

Kidney Function:
•
Filters & reabsorbs essential blood constituents.
•
Maintain fluid, electrolytes, acid-base balance.
•
Eliminate waste products, &many drugs.
•
Manufacturing hormones to maintain BP (renin).
•
Stimulate RBC production.
•
Regulate Ca &P metabolism.
Nep hriti c Sy n d ro m e
:
Damage of capillary walls of glomerulus leads to
ü
proteinuria
ü
hypoalbuminemia
ü
hyperlipidemia
ü
edema

•
It is caused by secondary diseases;
glomerulonephritis, nephropathy secondary to
amyloidosis, DM, SLE, or infectious diseases.
•
Treated with steroids &immunosuppressant, but
s.t. not respond & pass to chronic renal failure
MNT goals:
ü
Control hypertension
ü
Minimize edema
ü
Decr. urinary alb. losses
ü
Prevent protein malnutrition& muscle catabolism
ü
Supply adequate energy
ü
Slow the progress of renal disease.

MNT:
•
Adequate protein 0.8-1gm/kg/d to avoid
catabolism.
•
Energy 35Kcal/kg/d, to avoid malnutrition.
•
CHO 50-60%of total caloric intake.
•
Fat up to 30% of total caloric intake, mainly
monounsaturated &PUFA to decrease the
risk of hyperlipidemia.

•
Limited dietary sodium to control HT & edema,
avoid canned& processed foods,
hidden sources of sodium; water,
baking powder, toothpaste & mouth
wash, medication( antacid, antibiotics, cough
medicine, laxatives, pain killers, sedatives).
High sod. Foods; olives, salted nuts, salad
dressings, ketchup, sauce, potato chips,
popcorn, processed meat, tuna, all cheese
(except low sod.), canned veg., tomato juice.

Chronic Renal Failure
Result from progressive, irreversible loss of
kidney function, &pass to end stage renal
disease ESRD. It can be caused by;
glomerulonephritis, nephrosclerosis, obstructive
diseases ( R.S., tumors, congenital birth
defects), DM, SLE, abuse of analgesics.
CRF cause retention of nitrogenous waste
products, fluid & electrolytes imbalance which
affect all the systems.
Management goals
: focus on slowing the
progression of CRF to ESRD by; reducing
uremia by either conservative management,
hemodialysis, peritoneal dialysis, or renal
transplantation.

It is important not only to design food combinations that
include the necessary nutrients, but it should be
acceptable &the patient enjoy it, it depends on the
method of treatment in addition to medical & nutritional
status of the patient.
ü
Dietary modification should be initiated as early as
possible to minimize uremic toxicity,
ü
Delay the progression of renal disease (limit food toxic
byproducts)
ü
Prevent wasting & malnutrition (adequate calories to
prevent tissues catabolism),
ü
Motivation & encouragement to the patient if he feel
that’
s difficult to follow
.

Medical Nutritional Therapy:
v
Reduce protein &phosphorous to minimum
requirements to slow the progression of renal
insufficiency,(Protein should be of high
biological value).
v
Sodium 2000mg/d
v
Potassium 2000mg/d.
v
Phosphorous 1000mg/d.
v
Fluid 1000ml/d.
•
Add spices like garlic or onion to enhance the
flavor for the allowed foods.
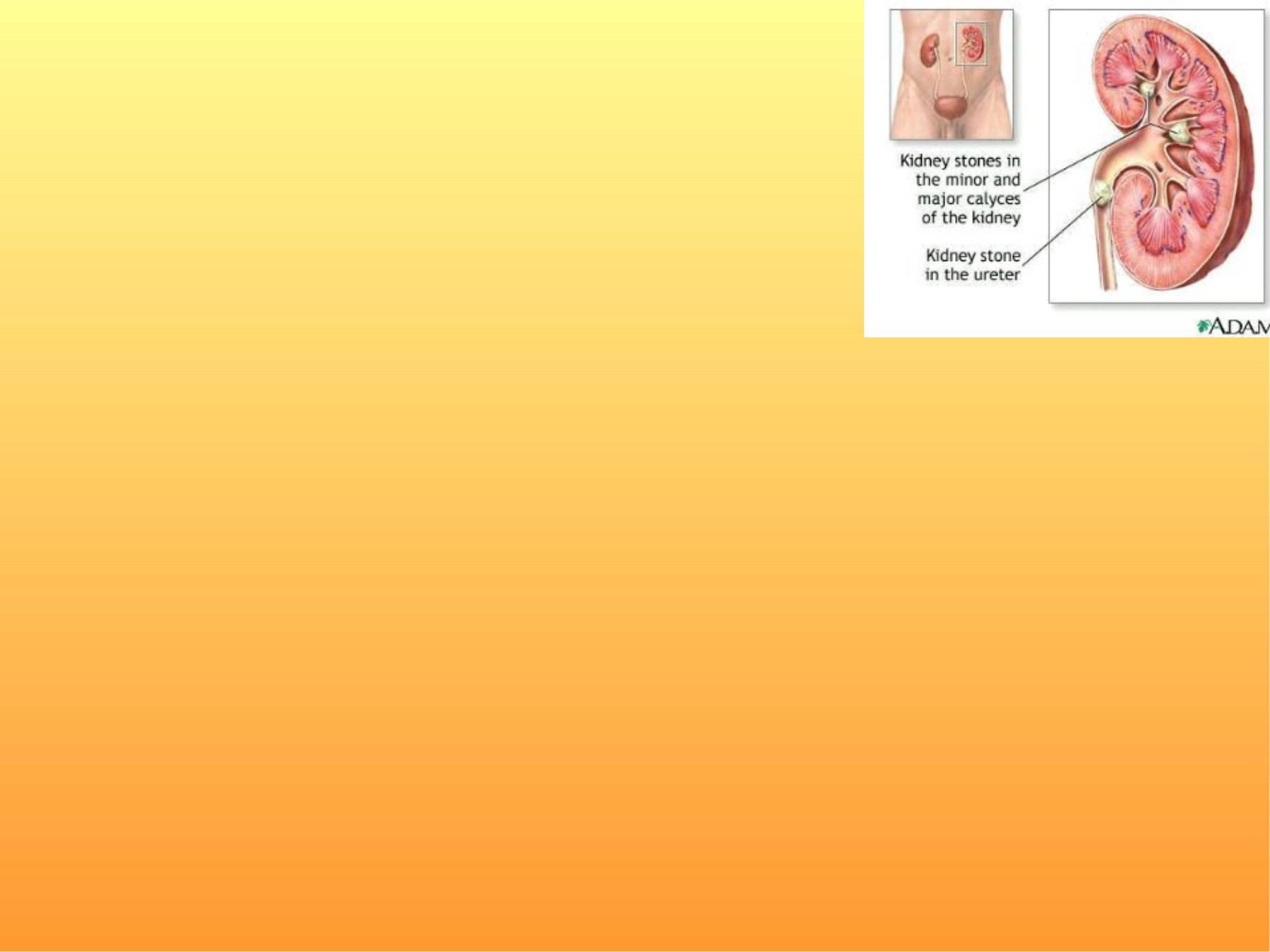
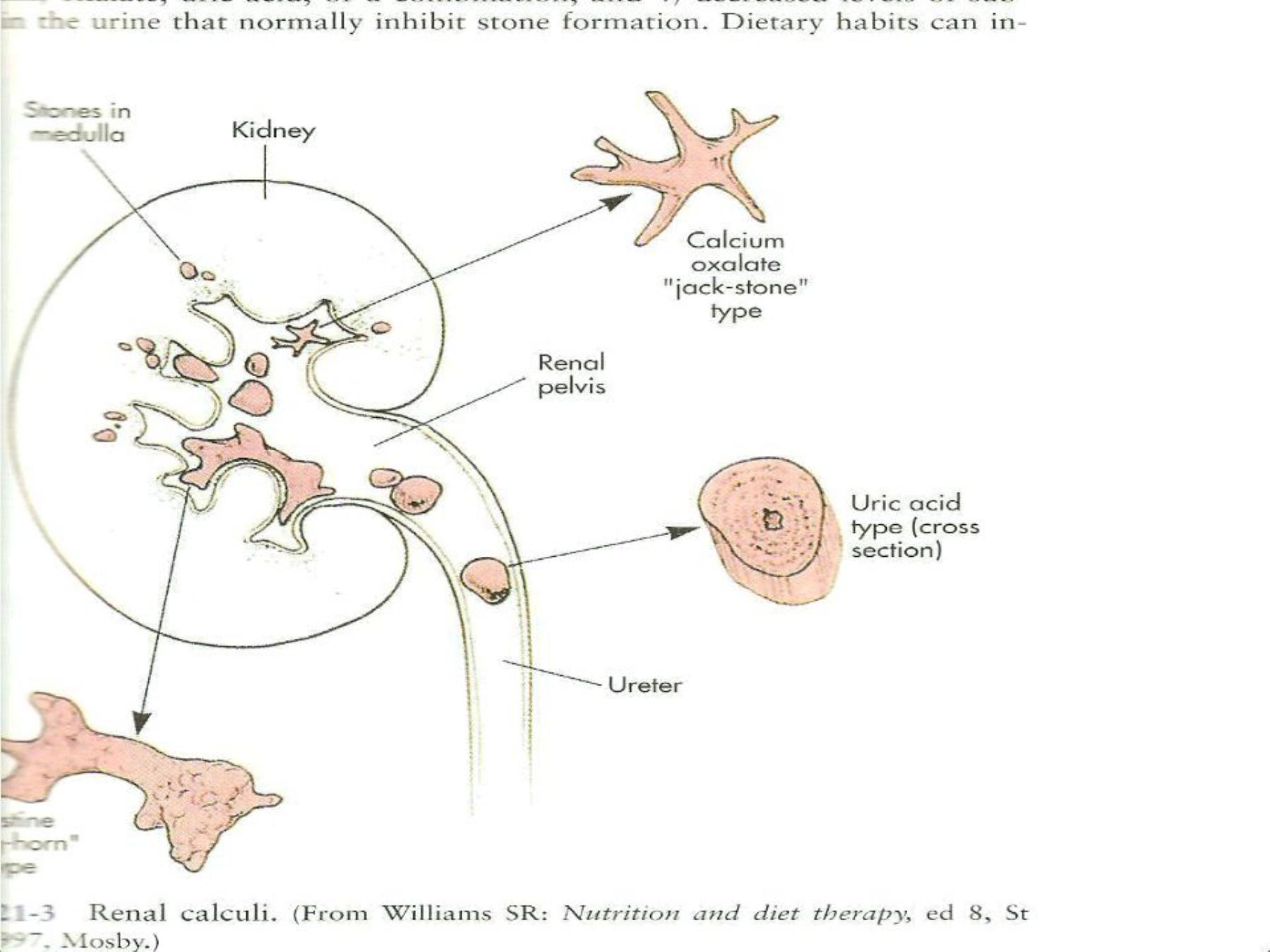
Renal Calculi
q
Common & recurrent condition.
q
Most calculi are composed of Ca
oxalate (75-80%), struvite (Mg, Am,
phosphate)15%, uric acid 7%, cystine <1%.
•
Factors that stimulate stones formation
;
v
Low urine volume (inadequate fluid intake).
v
High urine pH.
v
Excessive urinary excretion of calcium, oxalate, uric
acid, or combination.
v
Decrease urinary level of substances that inhibit
stone formation.
v
Dietary habits in susceptible person.
Advices to prevent renal stones formation:
ü
Increase fluid intake
incr. urine output, &
dilution of minerals in urine ( maintain output
to 2L/d & 2-3L of fluid intake).
ü
Moderate protein intake is recommended
(protein intake should not exceed 100gm/d)
ü
Uric acid stones: metabolic products of
purines (nitogen-containing comp.; lean meats,
organ meats, legumes & whole grains)

ü
Calcium stones: foods high in Ca (milk, cheese,
yogurt, green leafy veg.) & Na 2000-3000mg/d.
But research indicate that there is no need to
restrict dietary Ca (protective, because more
oxalate will be absorbed when decrease Ca
intake).
Renal stones formation is more influenced by;
Ø
high protein diet
Ø
high Sodium
Ø
high oxalate
Ø
low calcium,
v
While K & fluid intake found to be protective.

Oxalate (plant origin; spinach, beets, nuts,
chocolate, tea, wheat bran, strawberries) is
the end products of ascorbic acid
metabolism. Restriction of oxalate foods
reduce the risk of recurrence of Ca-oxalate
RS.
Avoid v.c. supplements 1000mg/d.
Increase complex CHO (whole grains, fresh
fruits, veg. which are a rich sources of K).

Foods high in oxalate
(> 10mg/servin g)
•
Vegetables:
Beans (green & dried), cucumber, okra, parsley, green
peppers, sweet potatoes, spinach---.
•
Fruits& juices:
Black berries, black & red grapes, strawberries, citrus peel
(lemon, orange), fruit cocktail.
•
Cereals:
Bread, pasta, fruit cake, bran
•
Fat:
Peanuts, almonds, cashews, walnut, nut butter, sesame
seeds& tahini.
•
Beverages:
Beer, tea, chocolate milk, cocoa, coffee, cola.
•
Others:
Chocolate, cocoa powder, vegetable soup, tomato soup,
tomato sauce.

Gout
Hereditary abnormal metabolism of purines,
cause a form of acute arthritis, with inflamed
joints (usually knees& feet).
Hyperuricemia results with deposition
of urate& s.t. sodium.
Objectives of MNT:
-Weight loss for obese patient.
-Increase urates excretion.
-Force fluid intake to prevent uric acid
stones.
-Correct any existing hyperlipidemia.

Dietary recommendations (MNT):
1-High CHO diet& low fat intake
increase excretion of urates.
2- In acute case; avoid excessive intake of
purines( shellfish, smoked meat, sardines &
meat extracts).
3-Calorie controlled diet for obese.
4-Ensure high fluid intake.
5-Exclude alcohol beverages.

Foods high in purines
•
High: content 150-825mg/100g
*Shellfish, seafood, sardines.
*Meat, brain, kidney, liver.
•
Moderate: content 50-150mg/g
*Vegetables; cauliflower, green peas,
mushrooms, spinach
*Grains& legumes; peas, lentils, beans,
*Oatmeal, wheat bran, whole grain
breads & cereals.
*Fish; all kind, lobsters, oysters.

*Meat; beef, lamb
*Poultry; chicken, duck, turkey.
•
Low: content 0-50mg/100g
*Beverages; carbonated beverages, coffee, tea.
*Grains; braid& cereals (refined white flour)
*Dairy; cheese, milk (all fat levels)
*Miscellaneous; eggs, fat, fruits& juices,
gelatin, nuts, sugars& sweets,
vegetables.
