Dr. Mushtak Gherbawe
Lec. 3
METABOLIC
DISORDERS
Mon
22 / 12 / 2014
Published by : Ali Kareem
2014 – 2015
مكتب اشور لالستنساخ
HYPERURICEMIA
Definition serum uric acid level of at least 2 SD above the normal
according to gender. I.e. serum uric acid level greater than
� 7.0 mg/dL in adult men i.e. after puberty and
� 6.0 mg/dL in premenopausal women.
In females it stays lower until menopause because estrogen promote
renal excretion of uric acid (female hormones are protective).
Male predominance (> 10:1).
CAUSES of HYPERURICEMIA:
� Increased uric acid production
� Diminished uric acid excretion by the kidney,
� Combination of above,
� Mechanism incompletely defined
A. Increased uric acid production
1. Primary hyperuricemia
a- Idiopathic
b- HGPRT deficiency AR
c- PRPP synthetase superactivity AR
2. Secondary hyperuricemia
a- Excessive dietary purine intake
b- Increased cell turnover e.g.(myeloproliferative and lymphoproliferative
disorders, hemolytic diseases, psoriasis, and …etc)
c- Accelerated ATP degradation to adenosine monophosphate (AMP), a
UA precursor e.g.
� Ethanol abuse
� Glycogen storage diseases (types I, III, V, VII)
� Fructose ingestion, hereditary fructose intolerance
� Hypoxemia and tissue underperfusion
� Severe muscle exertion
� Hypertriglyceridaemia (via metabolism of excess acetate)
B. Diminished uric acid excretion by the kidney,
1. Primary hyperuricemia
a- Idiopathic
b- Familial juvenile hyperuricemic nephropathy (AD)
2. Secondary hyperuricemia
a- Diminished glomerular filtration
b- Enhanced tubular urate reabsorption e.g.
• Dehydration
• Diuretics
• Insulin resistance (metabolic synd)
c- Inhibition of tubular urate secretion
d- Competitive anions (e.g. keto and lactic acidosis)
C- Mechanism incompletely defined
a- Hypertension
b- Hyperparathyroidism
c- Hypothyroidism
d- Certain drugs (e.g., cyclosporine, Pyrazinamide, ethambutol, and low-
dose salicylates)
e- Lead toxicity with nephropathy
GOUT
Disorders resulting from tissue deposition of monosodium urate
crystals or crystallization of uric acid in the urinary tract, due to great
increase in total body uric acid stores.
It is a common disorder (1%) of population.
Classification
� Primary gout is almost exclusively a male disease and the most
common cause of inflammatory arthritis in men over the age of 40
� Secondary gout, mainly affects people over the age of 65 and is the
form usually seen in women.
Gout rarely occurs in men before puberty or in women before
menopause.
The prevalence of Gout is increasing due to
1- Improving standard of living, dietary and lifestyle risk factors for the
development of gout in men include a relatively high intake of meat,
seafood, and barley water(Beer), and plants (peas, beans, and
mushrooms).
2- Increased longevity (age),
3- Increase use of thiazide diuretics,
4- In association with chronic renal insufficiency.
Clinical features
� Primary gout
1. Asymptomatic
Hyperuricemia can be found in at least 5% of asymptomatic persons on at
least one occasion during adulthood. Only a minority of individuals with
sustained hyperuricemia will develop clinical gout later.
Therefore, asymptomatic hyperuricemia is not Gout. In most it occurs
transiently in response to dietary and pharmacologic changes.
2.Acute gout
� The first attack involve a single distal joint.
First metatarsophalangeal joint is affected in over 50% of cases called
(podagra).
� Other common sites according to frequency are the ankle, knee, small
joints of hands, wrist and elbow.
� The axial skeleton and large proximal joints are rarely involved and if,
it is never as the first site.
Typical attacks usually present as:
� Very severe pain of a rapid onset, occur at night and awakes the
patient from sleep.

� Extreme tenderness-the patient is unable to wear socks or to let
bedding rest on the joint.
� Marked swelling with overlying red, shiny skin.
� Self-limiting over 5-14 days, with complete return to normal.
� Other manifestation are fever, malaise, bursitis, tenosynovitis or
cellulites.
� Polyarticular attacks are rare in first attack.
Differential diagnosis is septic arthritis, infective cellulites etc.
3. Intercritical or interval periods:
These are asymptomatic periods between attacks, then
� A second attack usually occurs within 1 year.
� The frequency of attacks gradually increases with time.
� Later attacks are more likely to involve several joints and to be more
severe.
� With time continued deposition causes joint damage and chronic pain.
� The interval between the first attack and the development of chronic
symptoms averages around 10 years.
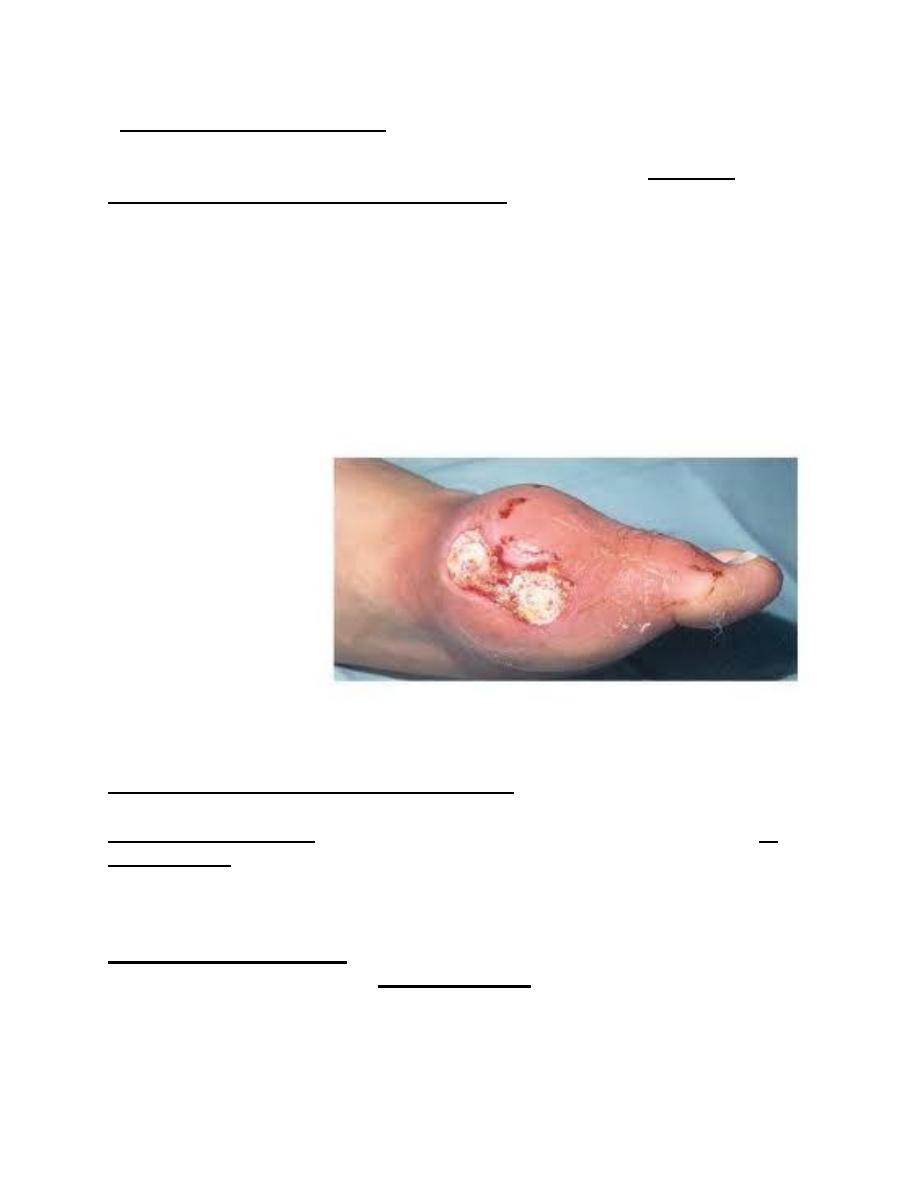
4. Chronic tophaceous gout:
� Large MSUM (monosodium urate monohydrate) crystal deposits
produce irregular firm nodules (tophi) at:
• Extensor surfaces of fingers, hands, forearm, elbows,
• Achilles tendons
• Helix of the ear.
� These may ulcerate, discharging whitish chalky material and association
with local inflammation (erythema, pus), even in the absence of secondary
infection.
1
.
5. Renal and urinary tract manifestations
Uric acid urolithiasis is a common manifestation of gout, particularly in
acidic urine.
Also excessive excretion of uric acid in the urinary tract also promotes
calcium oxalate urolithiasis.
Interstitial nephropathy, characterized by the deposition of monosodium
urate in the renal medulla, is currently a rare manifestation of gout, largely
because of advances in recognition and treatment of gout.
Secondary gout
� Presentation in older people,
� Often presents as painful tophi rather than as acute attacks.
� Hands, not feet, are the target site.
Diagnosis of Gout
Definitive diagnosis requires identification of Monosodium urate
monohydrate (MSUM) crystals in the aspirate from a joint, bursa or
tophus.
Acute gout synovial fluid shows increased turbidity due to the greatly
elevated cell count (> 90% neutrophils).
Chronic gouty fluid is more variable but occasionally appears white due
to the high crystal load.
Hyperuricemia does not confirm gout.
Also normal uric acid level, especially during an attack, does not exclude
gout (uric acid falls as part of the acute phase reaction).
Treatment
1- Acute attack
� Oral NSAID (e.g. diclofenac, indometacin) is the standard treatment.
� Oral colchicine can be very effective, but often causes vomiting and
severe diarrhoea at the doses needed for rapid relief (1 mg loading dose,
then 0.5 mg 6- hourly until symptoms abate).
� Aspiration of the joint will give instant relief and, when combined with
an intraarticular corticosteroid injection to prevent fluid re accumulation,
often effectively aborts the attack.
2- Long-term management
a- Correction of any predisposing factors
b- Hypouricaemic drugs
Indications for hypouricaemic drugs
� Recurrent attacks of acute gout
� Tophi
� Evidence of bone or joint damage
� Associated renal disease
� Gout with greatly elevated serum uric acid
Allopurinol
� Is the drug of choice It inhibits xanthine oxidase and reduces
conversion of hypoxanthine and xanthine to uric acid.
� The usual starting dose is 100-300 mg daily
� The sharp reduction in tissue uric acid levels that follows initiation of
treatmentcan partially dissolve MSUM crystals and may trigger acute
attacks, this can be minimised by
A- Using a lower starting dose (100 mg) or
B- Concurrent administration of oral colchicine (0.5 mg 12-hourly) or
NSAID for the first few weeks.
� Initiation of Allopurinol treatment during an attack can exacerbate and
prolong the episode so it is best to wait until the attack settles.
c- Uricosuric drugs (for under excreters)
� Probenecid or Sulfinpyrazone can achieve equivalent reductions in
serum uric acid to allopurinol but require several doses each day and
maintenance of a high urine flow (to avoid uric acid crystallisation in
renal tubules).
� Uricosurics are contraindicated in over-producers , renal
impairment (ineffective), and in patients with urolithiasis (increased stone
formation).
� Salicylates antagonise the uricosuric action of these drugs and should
be avoided.
