
Vitamin A (retinol)
Metabolites
: are retinaldehyde and retinoic acid
Function
retinaldehyde
is important of vision
retinoic acid
for the cell growth and
differentiation
retinoid
synthetic molecule
Vitamin A (retinol)
plays a role in
iron utilization
humeral immunity
T cell–mediated immunity
natural killer cell activity
phagocytosis
Vitamin A (retinol)
Metabolism
The
liver
contains 90% of the vitamin A is bound
to retinol-binding protein
transthyretin
trimolecular complex
specific cell-
surface receptors
bound to a series of
cellular retinol-binding proteins, function as
transporting agents as well as co-
ligands
for
certain nuclear receptors that act as transcription
factors.( retinoid-mediated gene transcription)
receptors for cell proliferation and differentiation

• * The trimolecular complex [retinol (vit.A) + retinol-binding protein
(RBP) + transthyretin(TTR)] prevents the glomerular filtration of the
low molecular weight RBP (and so vit.A).
* Transthyretin (TTR) is a carrier for retinol-binding protein, and also
thyroxine (T4). [This is how transthyretin gained its name,
trans
ports
thy
roxine and
retin
ol]
* RBP plays an important role in transporting retinol in circulation,
and delivering it to the cells by binding to specific cell-surface
receptors, releasing retinol to the cell after binding with the receptor,
then recirculate as the apo-form of BPR. Thus
• RBP is involved in multiple molecular interactions: it binds
• retinol and interacts with TTR and the cell-surface receptor

Vitamin A (retinol)
Dietary source
animal source
: liver and fish (excellent source)
plant source
: dark-green vegetable and fruits
by the splitting of carotenes.

Vitamin A (retinol)
Deficiency
1. chronic dietary deficit
(developing countries)
Southern Asia, Sub-Saharan Africa, some areas
of Latin America
More than
125 million
preschool-age children
with vitamin A deficiency, ~
4 million
have an
ocular manifestation of deficiency .
A
quarter
of a million children each year
developed blindness.

Vitamin A (retinol)
2. Malabsorption:
celiac disease, short bowel syn.
3. Zinc deficiency:
interfere with vitA mobilization
from the liver
4. Alcohol :
interfere with conversion of
retinol
to retinaldehyde in the
retina
(dehydrogenase)
5. Drugs :
interfere with the absorption of vitA
neomycin, cholestyramine (bile acid
sequestrant, so it can also bind fat-
soluble vitamins interference with absorbtion.
Vitamin A (retinol)
Clinical features
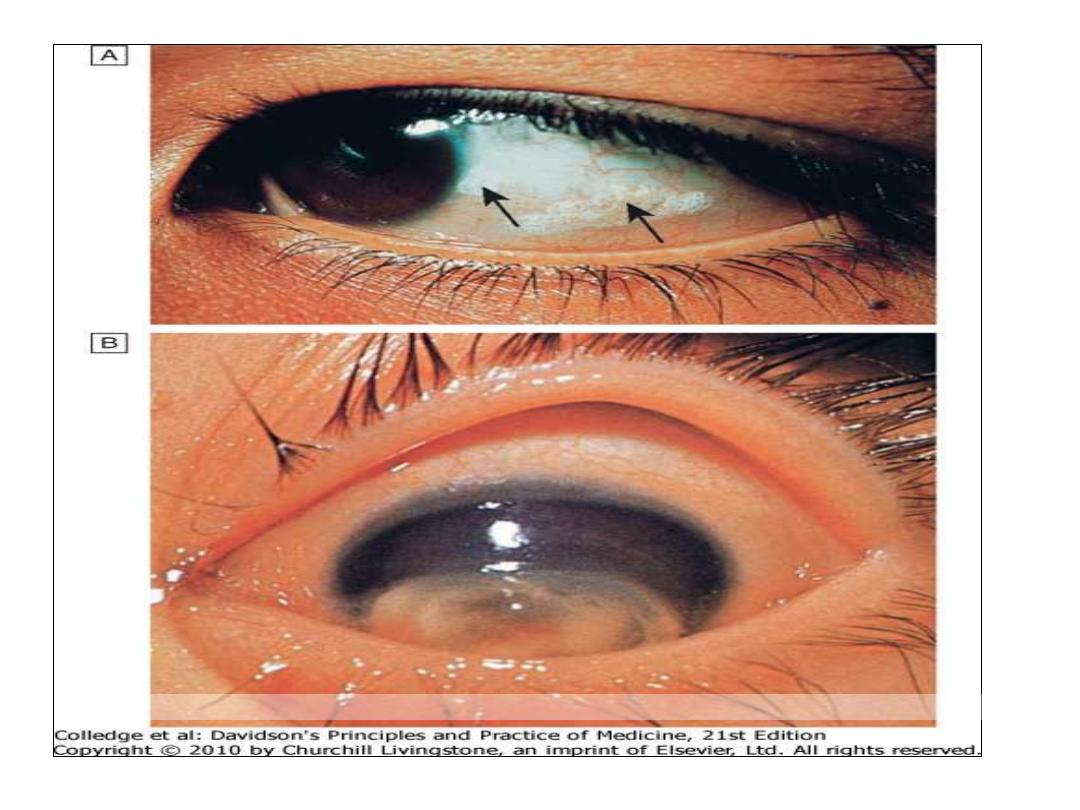
• night blindness
(loss of dark adaptation)
and may develop to complete blindness (endemic
blindness).
• conjunctival xerosis
(dryness)
(xerophalmia)
(because of loss of mucus secreting cells)
• Bitot's spots
(white patches of keratinized
epithelium on the sclera)
• Keratomalacia
(softening of the cornea) leads
corneal ulceration and
necrosis
result in corneal scarring
• increased risk of infection
dysentery
respiratory disease.
Downloaded from: StudentConsult (on 29 October 2011 12:19 AM)
© 2005 Elsevier

• * Vit.A deficiency in children is dangerous, and
increases mortality, because vit.A is essential
to maintain intact epithelia tissue as a physical
barrier to infection; it is also involved in
maintaining a number of immune cell types
from both the innate and acquired immune
systems.
• Prevention of deficiency :
1- A pregnant woman is advised to eat dark-green leafy vegetables,
and yellow fruits retinol in baby’s liver. (she shouldn’t take
vit.A supplements (high doses), because they have serious side
effects< and are teratogenic to the baby).
2- 60 mg retinol as palmitate is given to pre-school children leads to
a decrease in mortality by gastroetnteritis, respiratory infections,
and also measles.

• Toxicity :
1- Repeated moderate of high doses liver damage,
hyperostosis (excessive growth of bone), and
teratogenecity.
• 2- Acute overdose nausea, headache, elevated
intracranial pressure, skin desquamation.
3- Excessive intake of carotenes causes benign condition
(hypercarotenaemia), in which skin pigmentation
occurs and gradually fates when intake is stopped

Vitamin A (retinol)
Diagnosis
1.Serum retinol level
2.Test of dark adaptation
3.Impression cytology of the conjunctiva
4.Store assessment by liver BX

Vitamin A (retinol)
Treatment
30mg IM
or 60mg orally
Vitamin A
supplementation can markedly
reduce risk of child mortality where
deficiency is widely prevalent.
NB.
Used in patient with M3 leukemia (acute
promyelocytic leukaemia) and cystic acne
(cream).

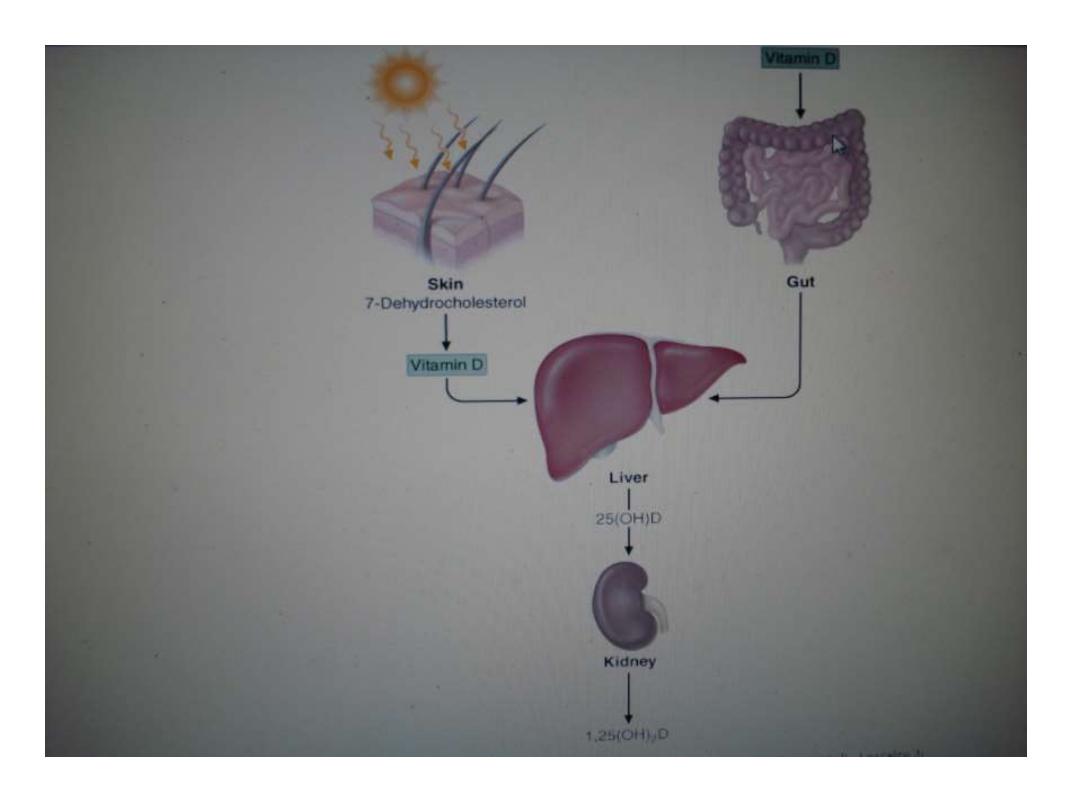
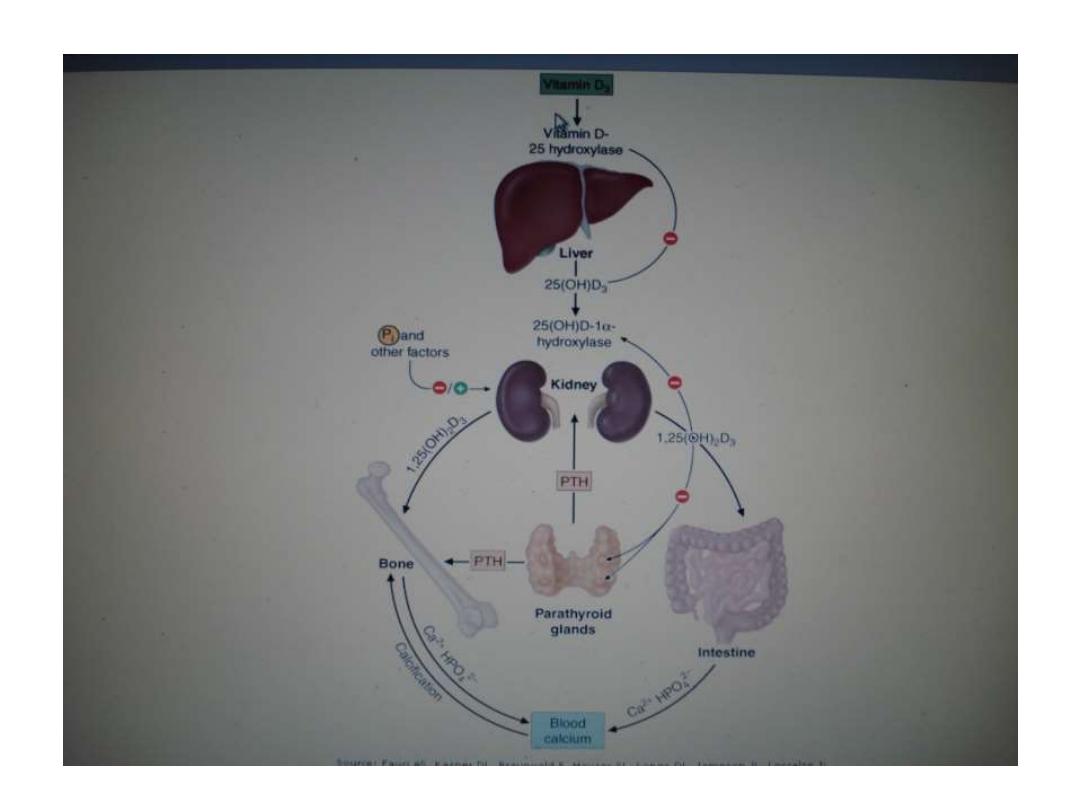
Vitamin D
Synthesis and Metabolism
• steroid
hormone
involved in mineral ion
homeostasis (calcium and phosphate)
• can be synthesized In response to ultraviolet
radiation of the skin (a photochemical cleavage
from 7-dehydrocholesterol).
source
animal sources(vitD3):
dairy products, fish
oils
egg yolks
plant sources (vitamin D
2
):
cereals

Vitamin D
Causes of the deficiency
Vitamin D deficiency
Impaired cutaneous production
decrease dietary
Malabsorption
Accelerated loss of vitamin D
Increased metabolism (barbiturates, phenytoin, rifampin)
Impaired enterohepatic circulation
* Anti-epileptic drugs (AEDs)
can also cause a deficiency in 25(OH)D,
even at sub-therapeutic serum levels of the drug, so theoretically it
can be worthwhile to supplement calcium and vitamin D even
before initiation of antiepileptic therapy.

Vitamin D
Clinical features
1.
Asymptomatic
(Mild to moderate deficiency)
2.
Osteomalacia
(defective bone mineralization)
Muscle and bone pain
Malaise
Fragility fracture (pseudofractures or Looser’s zone)
Proximal myopathy (waddling gait)
Bone tenderness
3.
Rickets
( growth retardation, bone deformities)

Looser zone

Looser zone

Vitamin D
Diagnosis
1. Biochemical tests
decrease serum 25(OH)D
low or normal s. Ca. , ph.
increasing PTH levels
increase alkaline phosphatase
2. Radiological tests of oteomalacia
decrease in cortical thickness
osteopenia of the skeleton
pseudofractures, or Looser's zones in the ribs
and pelvis and long bones and vertebra
3. Bone biopsy

Vitamin D
Treatment
VitD 50,000 IU
weekly for 3–12 Weeks
followed by maintenance therapy (800 IU
daily).
Calcium supplementation include 1.5–2.0 g
/d
800 IU of vitamin D, with calcium
supplementation, decreases the risk of hip
fractures in elderly women.

Vitamin E ( tocopherols)
Function
• acts as
antioxidant
and radical
scavenger
which protects low-
density lipoprotein and polyunsaturated fats in membranes from
oxidation, and especially effective for protecting nerve cells, red
blood cells, and immune system function; aiding in the
prevention of and healing of neurological disorders, chronic viral
illness and anemia. Several studies have been performed in
relation to fertility health, revealing its importance for
reproductive function and health.
Absorption and Metabolism
• After absorption, vitamin E is taken up from
chylomicrons
by the
liver, and a hepatic tocopherol transport protein mediates
intracellular vitamin E transport and incorporation into very low-
density lipoprotein
(VLDL)
.

Vitamin E ( tocopherol)
Dietary source
widely distributed in the food supply
High
: sunflower, soybean and corn oils
meats, nuts, and cereal grains
small amounts
: fruits and vegetables.

Vitamin E ( tocopherol)
Causes of the deficiency:
1.
Dietary deficiency
( does not exist).
2.
prolonged
malabsorptive diseases
.
3.
prolonged
cholestasis
4.
abetalipoproteinemia
cannot absorb or
transport vitamin E.
5.
A
familial form
of isolated vitamin E
deficiency (defect in the tocopherol
transport protein).

Vitamin E ( tocopherols)
Clinical features
axonal degeneration of the large myelinated
axons and results in
posterior column
Peripheral neuropathy
Sensory ataxic gait
Ophthalmoplegia
skeletal myopathy
pigmented retinopathy

Vitamin E ( tocopherols)
Diagnosis
low blood levels of tocopherol
Treatment
• 800–1200
mg of tocopherol per day.

Vitamin k
Function
• vitamin K
1
,
phylloquinone, from vegetable and
animal sources
• vitamin K
2
, menaquinone, synthesized by
bacterial flora and found in hepatic tissue
• Vitamin K3
, menadion, synthetic
• required for the
carboxylation
of glutamic
acid, which is necessary for calcium binding to
-carboxylated proteins such as prothrombin
(factor II); factors VII, IX, and X; protein C;
protein S).

Vitamin k
Dietary Sources
green leafy vegetables
(spinach)
liver
vegetable oils
: olive, soybean oils.
* It’s also synthesized by bacteria in the
colon ( intestinal flora), so intestinal
disorders and broad spectrum antibiotics
will affect the flora decrease vit.K supply
by the flora.
Vitamin k
Causes of the deficiency
1.
small-intestinal disease
(e.g., celiac disease)
2.
cholestatic
liver disease (obstructive jaundice).
3. Broad-spectrum
antibiotic
treatment (especially with
anticoagulant drugs as warfarin) killing intestinal flora
decreased normal vit.K supplement by the flora G.I.T bleeding
(because of the drugs and low vit.K level which is needed for
coagulation).
3.
drug
therapy, the antiobesity drug orlistat (Absorption of fat-
soluble vitamins and other fat-soluble nutrients is inhibited,
because orlistat acts by inhibiting the gastric and pancreatic
lipase).

• In new born, primary deficiency results from :
1- Inefficient placental vit.K transferring.
2- Neonatal bowel has not yet acquired the
flora.
3- Breast milk contains little amounts of vit.K.
So, vit.K supplements are given to the new born
babies routinely to prevent haemorrhigic
diseases of the new born .

Vitamin k
The diagnosis
• elevated
prothrombin time
or reduced
clotting factors
• vitamin K may also be measured directly.
Treatment
• Vitamin K deficiency is treated using a
parenteral dose of
10
mg.

Thanks
