1
Immune Deficiency
Learning Objectives
To define: primary and secondary ID
Describe clinical presentations of ID
List the Causes of ID
List the Sequelae of ID
Give some practical examples
Summary
Quiz
4

5
1)
Recurrent infections
:
Frequent, severe, by unusual organisms
& at unusual sites
2)
Autoimmunity
3) Susceptibility to
malignancy
Clinical features of immune defificency:
6
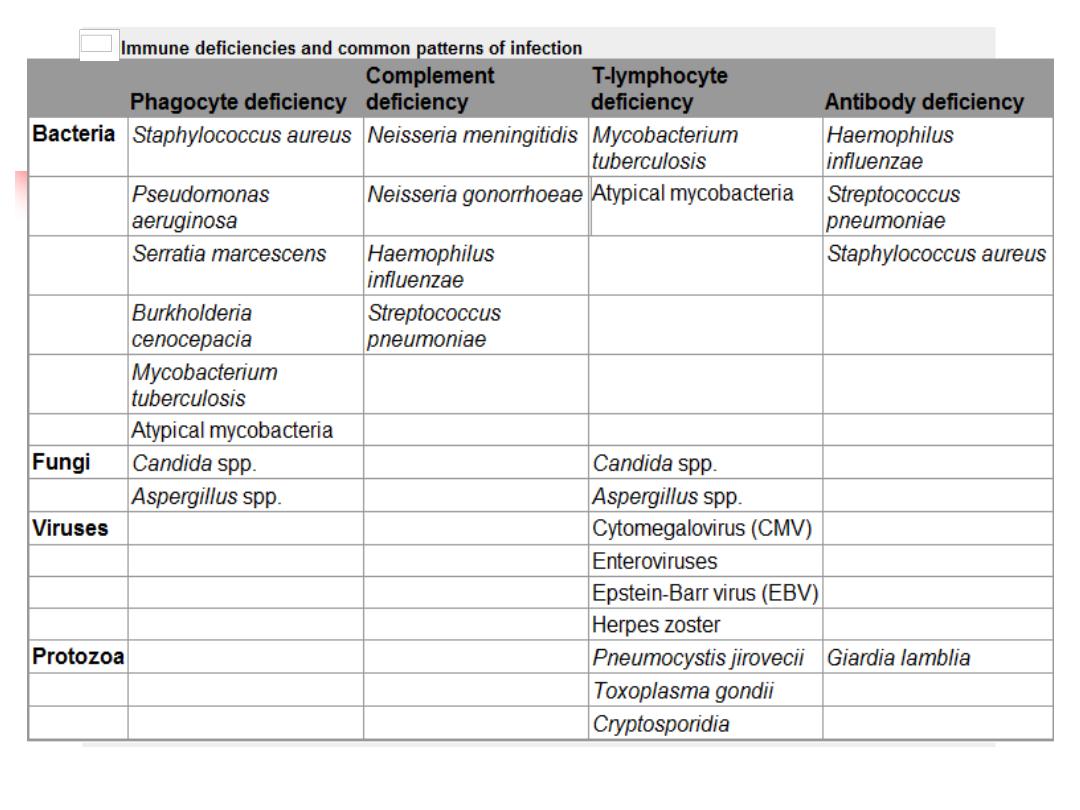
Causes of immune deficiency
:
Primary :
Phagocyte ↓
Complement Pathway ↓
Adaptive IS ↓
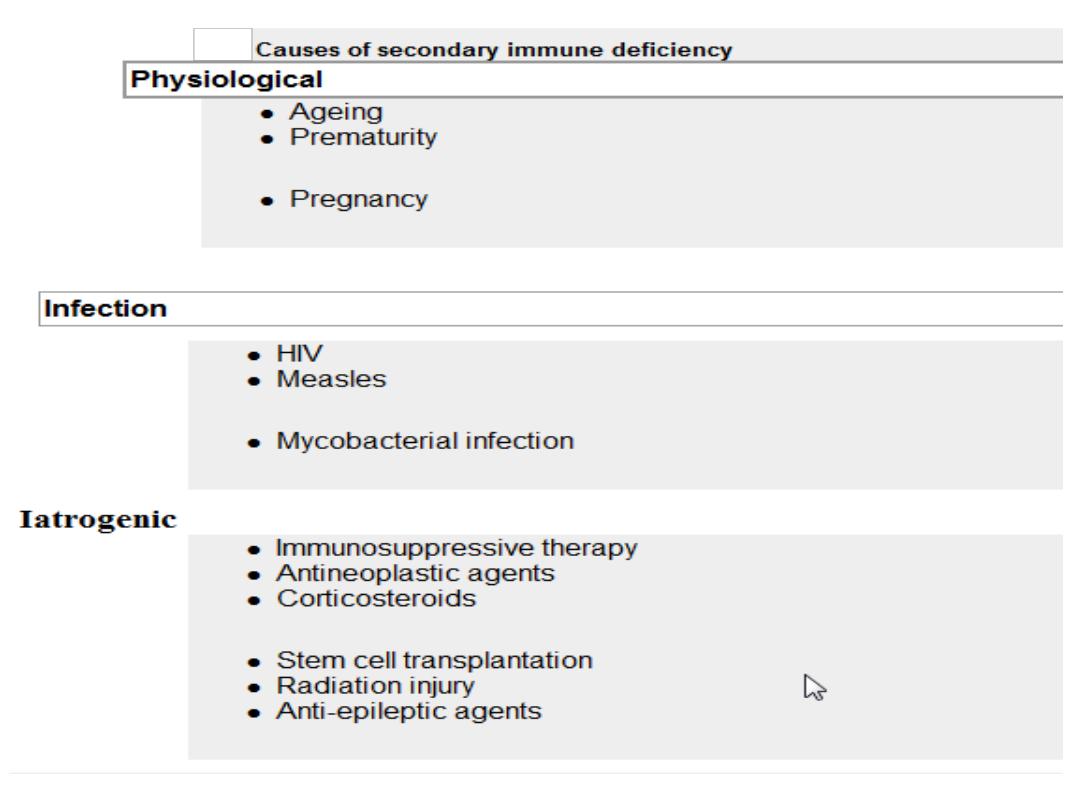
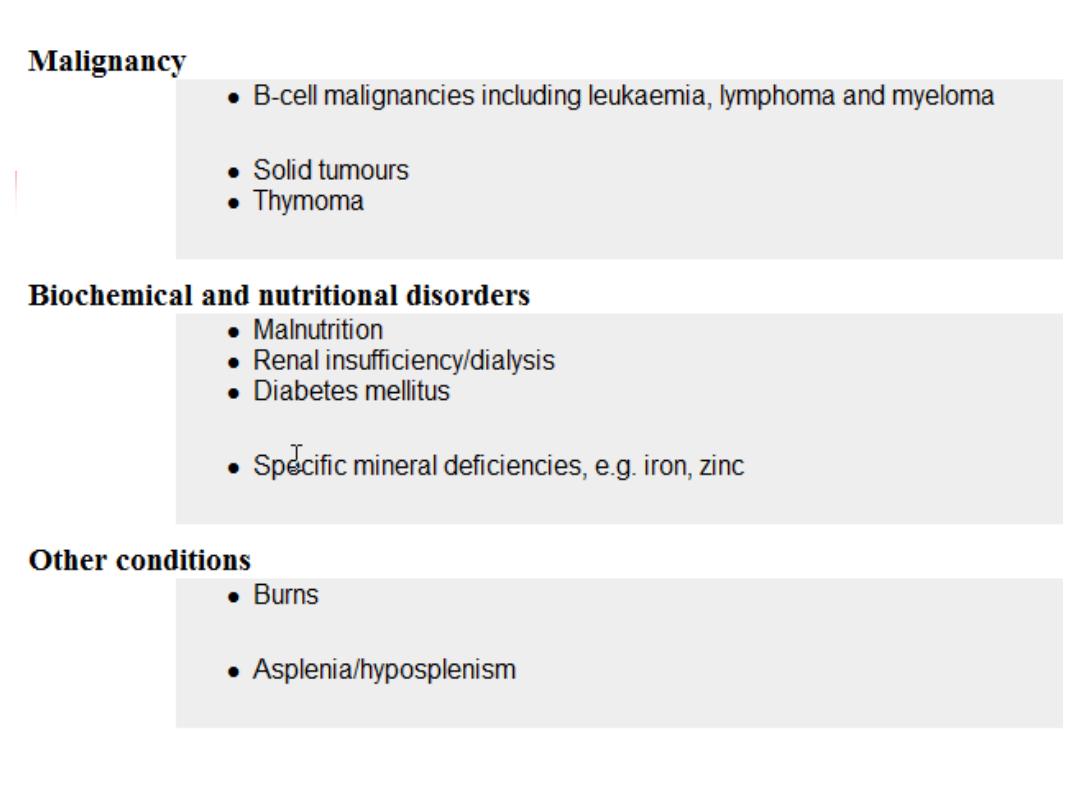
Secondary:
Physiological
Infection
Iatrogenic
Malignancy
Biochemical & Nutritional
Others
7
8
A. Phagocyte ↓
↓WBC Adhesion Chronic Granul Dis ↓ Cytokine & Cytokine
receptors
Staphyl.aureaus
Aspegillus
Bacterial Infection
TB
TB
9
A.Phagocyte ↓ sequlae
:-
1)↓WBC Adhesion
------- infection
2
) Chronic granulomatous disease
Catalase-positive organisms like
Staphyl. aureus
&
aspergillus.
Intracellular killing of mycobacteria in macrophages is also
impaired.
Infections most commonly involve the lungs, lymph nodes,
soft tissues, bone, skin and urinary tract
3) Defects in cytokines and cytokine receptors
------failure of intracellular killing -----mycobacterial
infections
10
11
Management:
1)
Drugs:
IV AB, Longterm prophylaxis with antifungal
agents, and trimethoprim-sulfamethoxazole.
2)
Surgical
drainage of abscesses
3)
Specific
treatment depends upon the nature of the
defect.
4)
and
stem cell transplantation
12
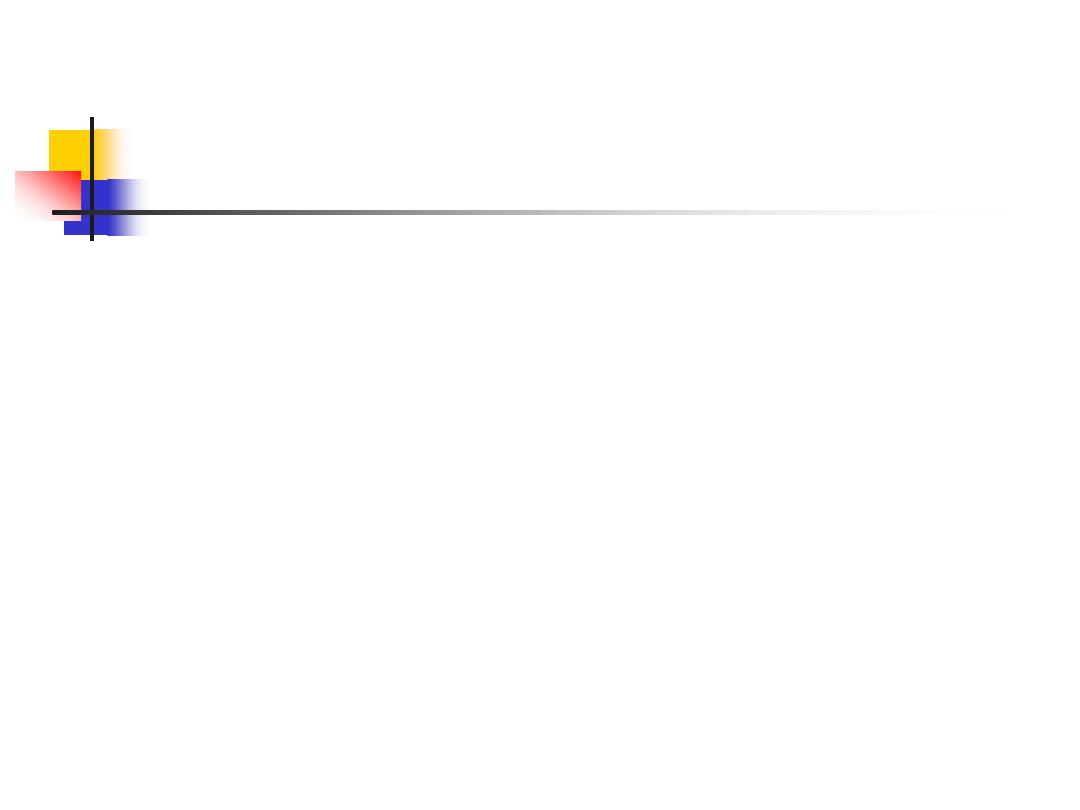
B. Complement Pathway ↓
Genetic deficiencies.
Deficiency of the
regulatory protein C1 inhibitor
--
recurrent angioedema.
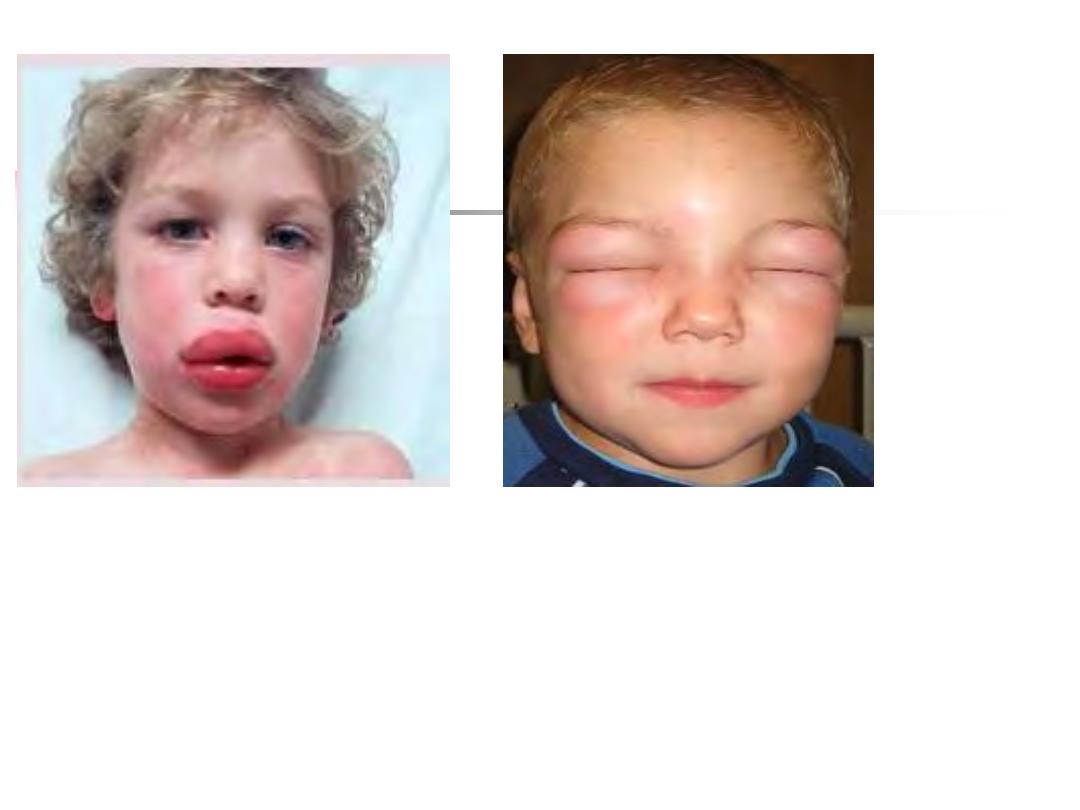
C1, C2 and C4
------
autoimmune disease
(severe SLE)
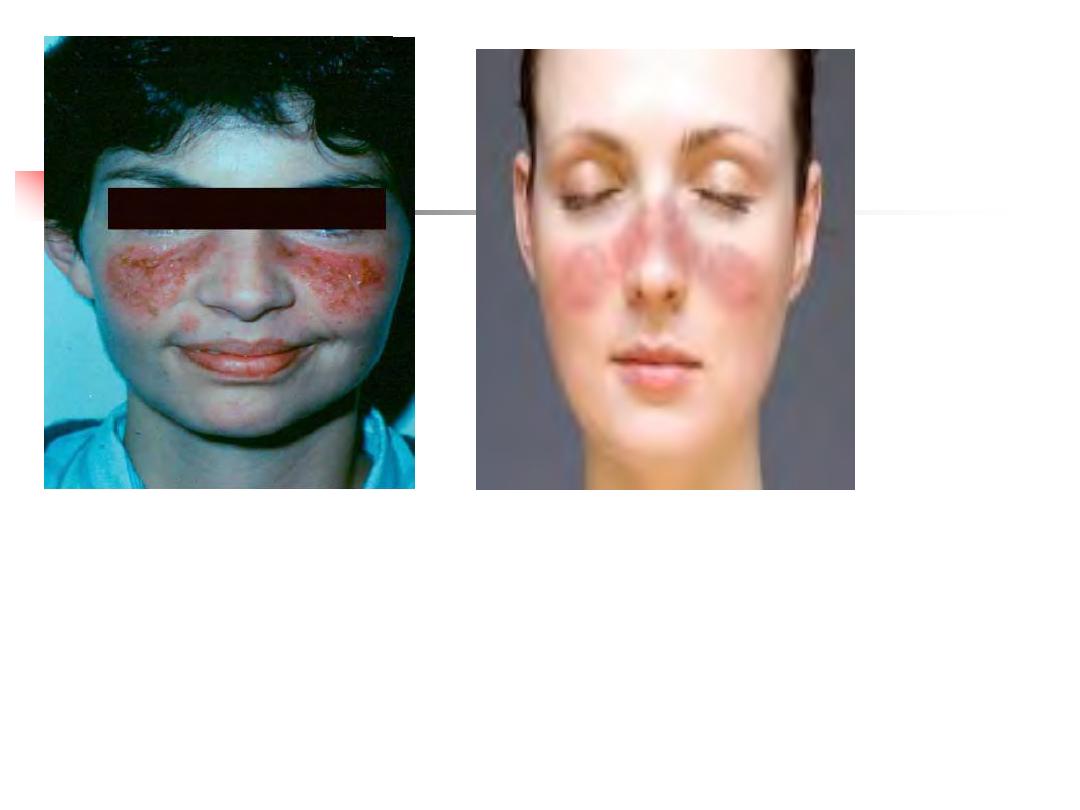
Classical and alternative pathway components
: recurrent
infection with
encapsulated bacteria
particularly
Neisseria
species
Mannose-binding lectin deficiency is
very common
13

14
15
16
Encapsulated Neisseria Species.

17
Investigations:
Blood for complement : C3 and C4 (routinely), CH50
Treatment:
1.
No definitive
2.
Vaccination: with meningococcal, pneumococcal and
H.
influenzae
B vaccines to boost their adaptive immune
responses
3.
Life-long prophylactic penicillin
4.
Screening family members at-risk.
18
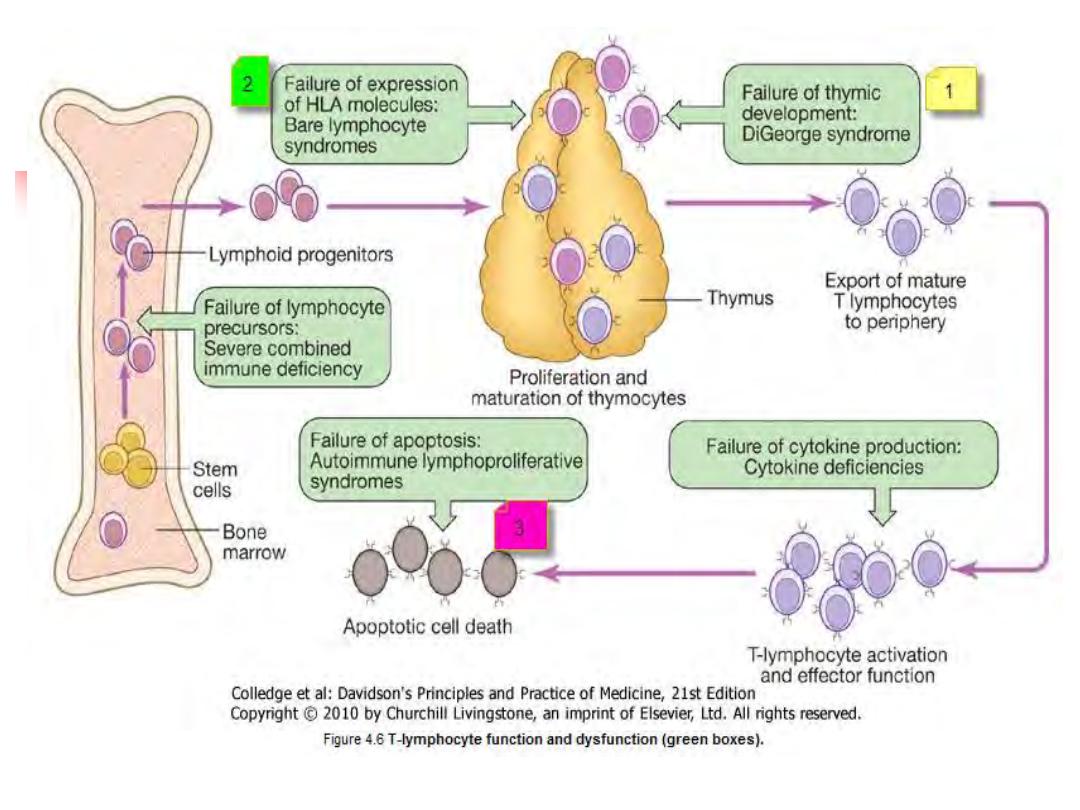
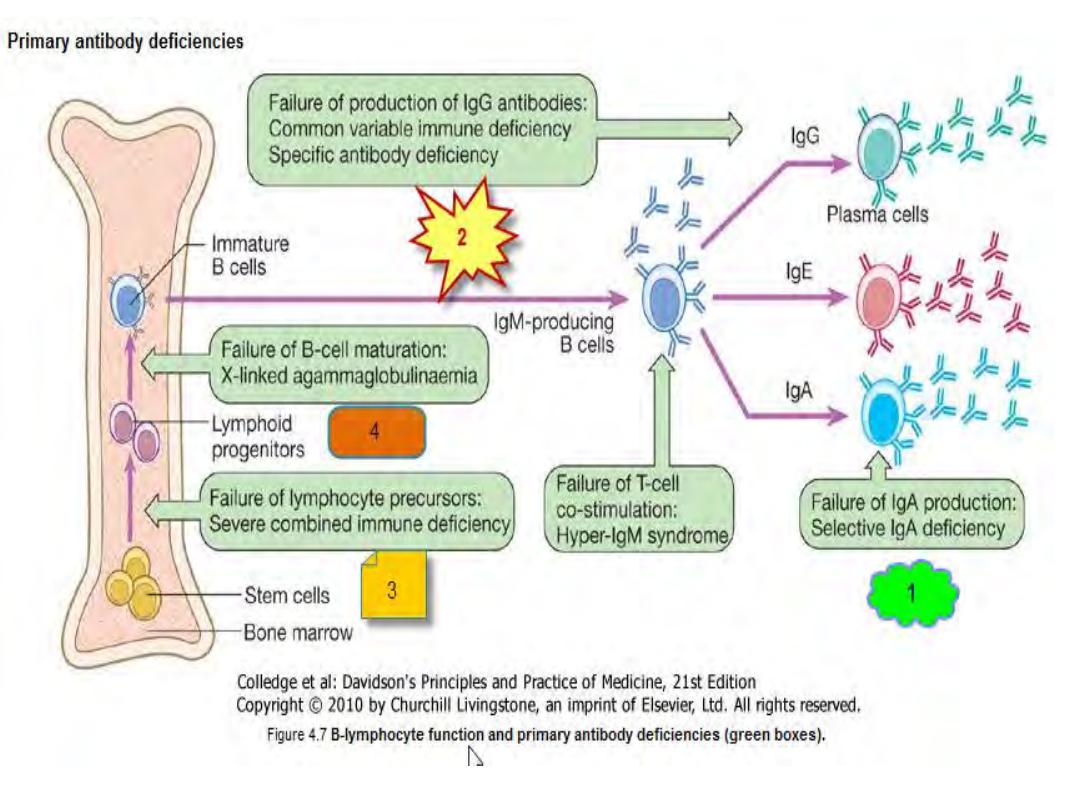
C.1⁰↓Adaptive immune system
Combined ↓
B & T lymphocytes
T lymph ↓
-
DiGeorge syndrome
- Bare lymphocyte syndromes
-Autoimmune
lymphoprolif. Syndrome
↓ B lymph
- Selective
IgA
-
CVID
- IgG
- overlap
- global
19
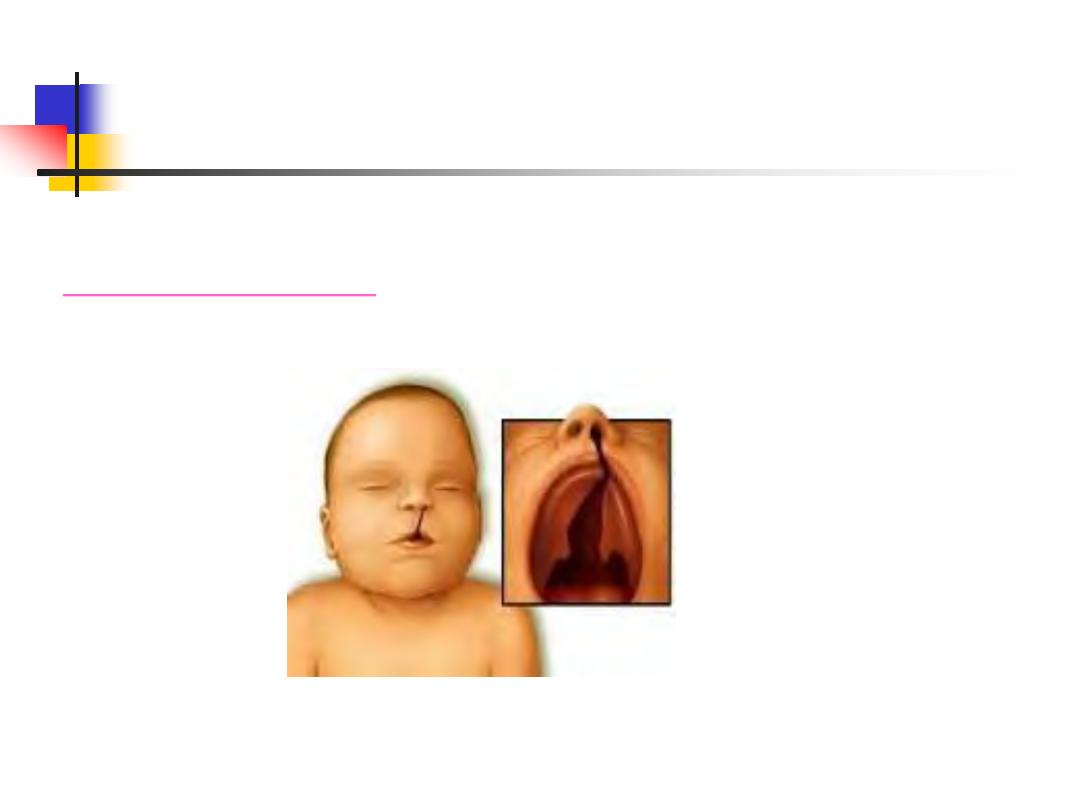
Primary T-lymphocyte Deficiencies
Sequelae:
1)DiGeorge syndrome:

20
2)Bare lymphocyte syndromes:
21
3) Autoimmune lymphoproliferative syndrome:
22
23
Investigations
Blood Ix
Total lymphocyte count
Serum immunoglobulins
Functional tests of T-cell and/or an HIV test
Treatment:
Anti-
Pneumocystis
and antifungal
prophylaxis
Aggressive management of
specific
infections
Immunoglobulin replacement may be indicated if disease is
associated with defective antibody production
Stem cell transplantation ---in bare lymphocyte
syndromes
Thymic transplantation - in DiGeorge syndrome
24
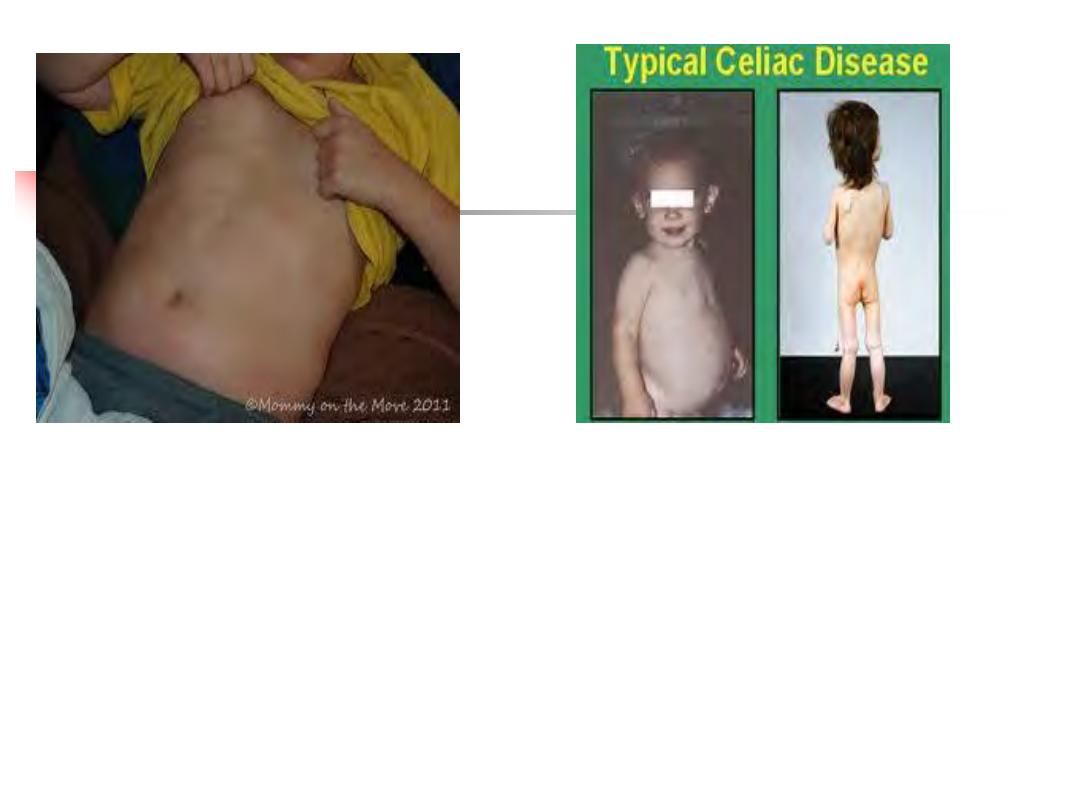
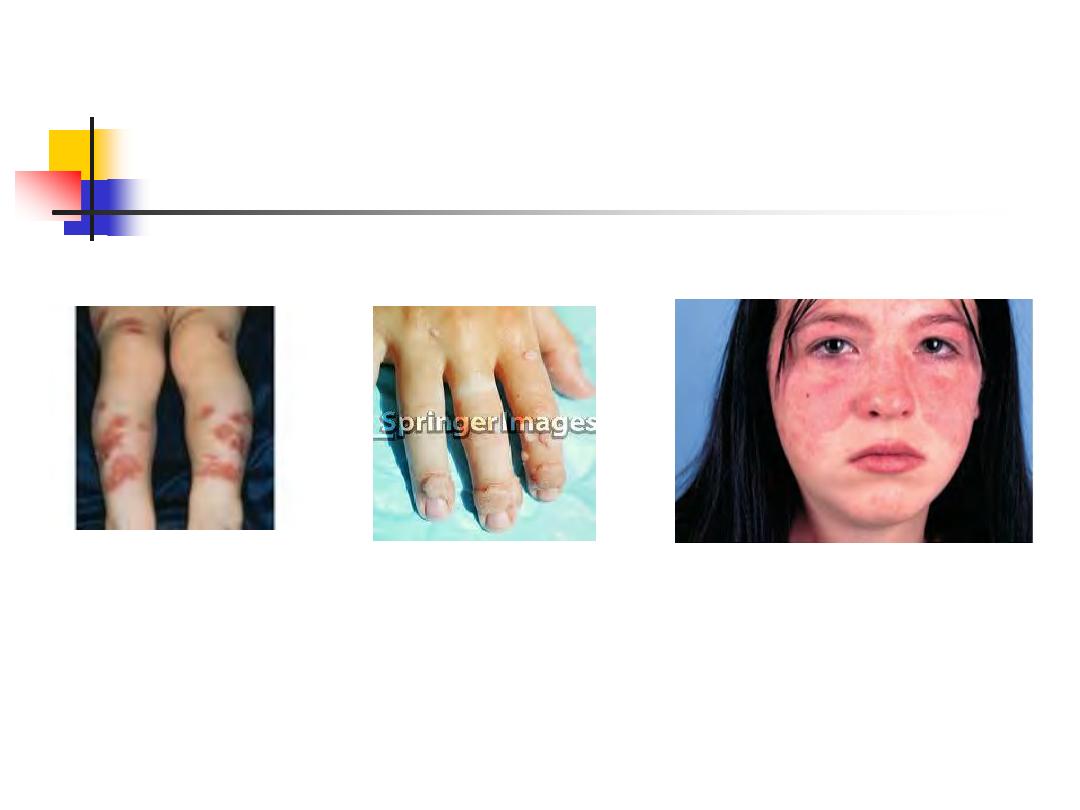
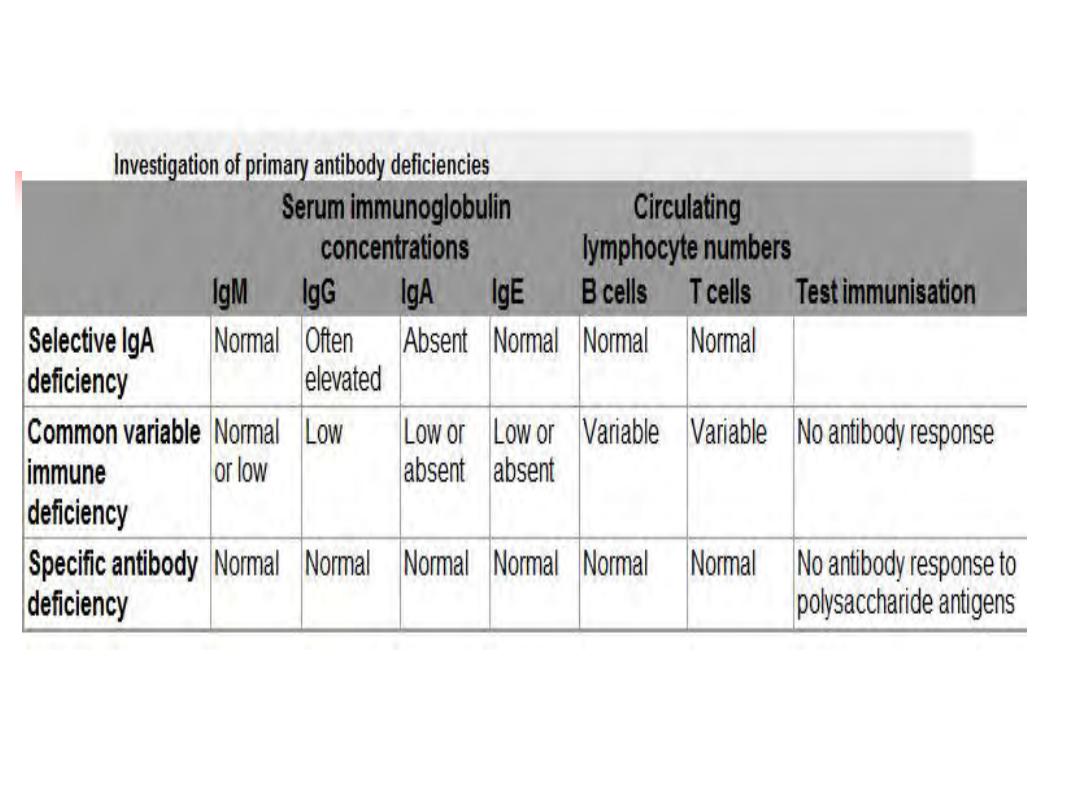
3) Primary B lymphocyte deficiency(Ab ↓):
1)Selective IgA deficiency:
is the
most common
primary immune deficiency
Mostly,
an incidental finding with no clinical
sequelae
30%
of individuals experience recurrent mild
respiratory and gastrointestinal infections
.
25
26
Selective IgA deficiency
27
2)Common variable immune deficiency (CVID):
Unknown cause
Characterized by
low serum IgG levels
and
failure to
make antibody responses
to exogenous pathogens
Complications:
Antibody-mediated autoimmune
diseases & increased risk of malignancy.
28
29
3)Specific antibody deficiency [functional IgG antibody
deficiency]
4)
There is
overlap
between
specific
antibody deficiency
,
IgA deficiency and CVID
,
and some patients may progress to a more
global
antibody deficiency over time
30
31
Investigations:
Serum immunoglobulins & protein and urine electrophoresis
Specific antibody :measuring IgG antibodies against
tetanus,
H. influenzae
and
S. pneumonia
32
Management:
1. The mainstay of treatment is IVIG & life-long
.
2. AB:
Aggressive treatment of infections, and prophylactic
antibiotics
3. Immunization
is in selective IgA deficiency [generally not
effective (because of the defect in IgG antibody
production)].
4. live vaccines should be avoided
33
34
35
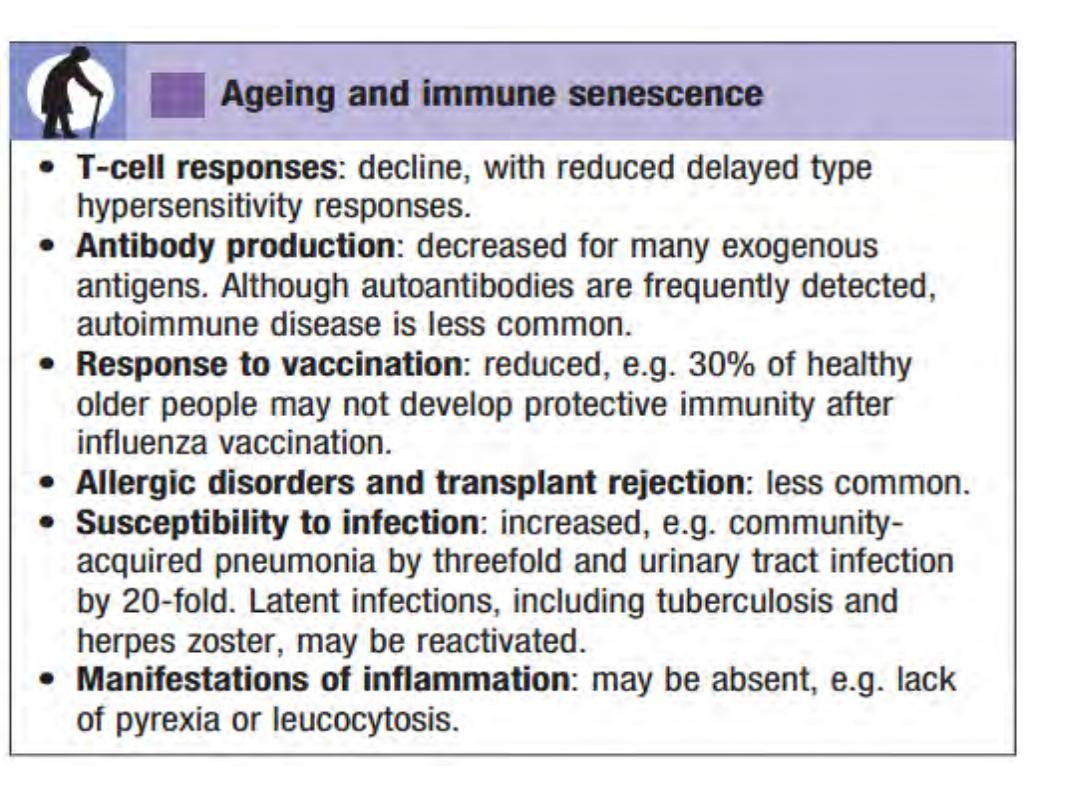
2 ⁰ >> 1⁰ immune deficiencies
Infection is a common cause of secondary immune
deficiency, particularly HIV infection, measles and other viral
illnesses
Immune deficiency is also an expected side-effect of some
drugs (immune suppressive)
May be an idiosyncratic effect of other agents, particularly
anti-epileptic medication
Physiological immune deficiency occurs at the extremes of
life
36
Summary
ID presented with infection, autoimmune, malignancy.
Causes are 1⁰ ( phagocyte↓, cmm ↓, Ad ↓), 2 ⁰ ( Phys, inf,
iatrog, malig, biochem--).
Phagocyte ↓---W ↓, CGd, ↓CCR
cmm ↓-angioedema, autoimmune, inf
Ad ↓----- both B & T ↓- inf
T ↓---Digeorge, Bare, & Autoimm Lymph
B ↓-- ↓ IgA, CVD, IgG, Overlap & global
37
Quiz?
38
Q1/ In complement pathway deficiency
, which
one
of the following is
a common
pattern of
infection?
A.
Atypical mycobacteria
B.
Neisseria meningitides.
C.
Herpes zoster
D.
Staphylococcus aureus
E.
All of the above
39
Q2/ Regarding T lymphocyte deficiency
,
which
one
of the following is
correct?
A.
Selective IgA deficiency
B.
Common variable immune deficiency
C.
DiGeorge syndrome.
D.
IgG deficiency
E.
None of the above
40
Q3/ In primary immune deficiency, which
one
of the following is
likely cause
?
A.
Physiological
B.
Infection
C.
Iatrogenic
D.
Malignancy
E.
Phagocyte deficiency
41
Next lecture
Autoimmune diseases and allergy
42
