Dr. Abdulla Al-Farttoosi
Lec. 1
Toxoplasmosis -
Amoebiais
Wed
18 / 3 / 2015
2014 – 2015
ﻣﻜﺘﺐ ﺍﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
1
toxoplasmosis
(Toxoplasma gondii)
Objectives
To define toxoplasmosis.
To determine methods of its transmission.
To describe its epidemiology.
To recognize clinical features of toxoplasmosis.
To asses and investigate a case of toxoplasmosis.
To evaluate lines of management of toxoplasmosis.
Introduction
Toxoplasmosis is considered to be a leading cause of death attributed to
foodborne illness in the United States. More than 60 million men, women, and
children in the U.S. carry the Toxoplasma parasite, but very few have
symptoms because the immune system usually keeps the parasite from causing
illness.
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
2
Toxoplasmosis is caused by infection with the obligate intracellular parasite
Toxoplasma gondii. Acute infection acquired after birth may be asymptomatic
but frequently results in the chronic persistence of cysts in the host's tissues. In
both acute and chronic toxoplasmosis, the parasite is responsible for clinically
evident disease, including lymphadenopathy, encephalitis, myocarditis, and
pneumonitis.
Congenital toxoplasmosis is an infection of newborns that results from the
trans-placental passage of parasites from an infected mother to the fetus.
These infants usually are asymptomatic at birth but later manifest a wide range
of signs and symptoms, including chorioretinitis, strabismus, epilepsy, and
psychomotor retardation.
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
3
Epidemiology
T. gondii infects a wide range of mammals and birds. Its seroprevalence*
depends on the locale and the age of the population. Generally, hot, arid climatic
conditions are associated with a low prevalence of infection. In the United States and
most European countries, the seroprevalence increases with age and exposure. For
example, in the United States, 5–30% of individuals 10–19 years old and 10–67% of
those >50 years old have serologic evidence of exposure.
* seroprevalence:
the level of a pathogen in a population, as measured in blood
serum.
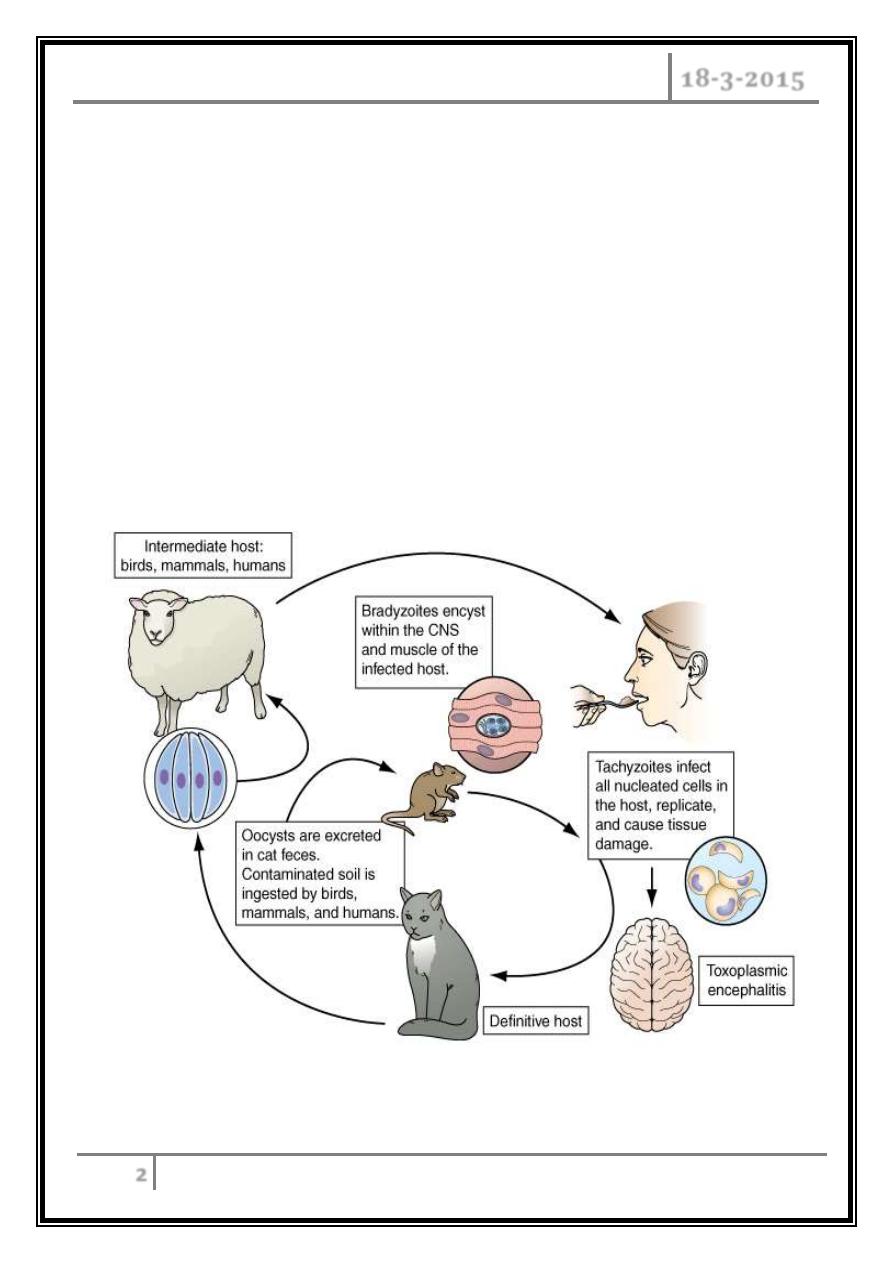
Transmission
Oral transmission.
Transmission via blood or organs.
Trans-placental transmission.
Clinical features
In most immunocompetent individuals, including children and pregnant
women, the infection goes unnoticed.
In 10% of patients, it causes a self-limiting illness, most common in adults aged
25-35 years. The most common presenting feature is painless
lymphadenopathy, local or generalized.
Most patients have no systemic symptoms, but some complain of malaise,
fever, fatigue, muscle pain, sore throat and headache.
Complete resolution usually occurs within a few months, although some
patients do not recover completely for a year or more.
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
4
Very infrequently, patients may develop encephalitis, myocarditis,
polymyositis, pneumonitis or hepatitis. Retinochoroiditis is nearly always the
result of congenital infection but has also been reported in acquired disease.
Congenital toxoplasmosis
Acute toxoplasmosis, mostly subclinical, affects 0.3-1% of pregnant women,
with an approximately 60% transmission rate to the fetus which increases with
increasing gestation.
Seropositive females infected 6 months before conception have no risk of fetal
transmission.
Congenital disease affects approximately 40% of infected fetuses, and is more
likely and more severe with infection early in gestation.
Many fetal infections are subclinical at birth, but long-term sequelae include
retinochoroiditis, microcephaly, and hydrocephalus.
Investigations
In immunocompromised patients: direct detection of parasites.
Immunocompetent individuals: serology; The Sabin-Feldman dye test (indirect
fluorescent antibody test), which detects IgG antibody.
Recent infection is indicated by a fourfold or greater increase in titre when
paired sera are tested in parallel. Peak titres of 1/1000 or more are reached
within 1-2 months of the onset of infection, and the dye test then becomes an
unreliable indicator of recent infection.
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
5
The detection of significant levels of Toxoplasma-specific IgM antibody may be
useful in confirming acute infection. False positives or persistence of IgM
antibodies for years after infection make interpretation difficult; however,
negative IgM antibodies virtually rule out acute infection.
During pregnancy it is critical to differentiate between recent and past
infection; the presence of high-avidity IgG antibodies excludes infection
acquired in the preceding 3-4 months.
If necessary, the presence of Toxoplasma organisms in a lymph node biopsy can
be sought by staining sections histochemically with T. gondii antiserum, or by
the use of PCR to detect Toxoplasma-specific DNA.
Management
In immunocompetent subjects, uncomplicated toxoplasmosis is self-limiting,
and responds poorly to antimicrobial therapy. Treatment with pyrimethamine,
sulfadiazine and folinic acid is therefore usually reserved for rare cases of
severe or progressive disease, and for infection in immunocompromised
patients
In a pregnant woman with an established recent infection, spiramycin (3 g daily
in divided doses) should be given until term. Once fetal infection is established,
treatment with sulfadiazine and pyrimethamine plus calcium folinate is
recommended (spiramycin does not cross the placental barrier).
Treatment during pregnancy decreases the severity of infection. Many women
who are infected in the first trimester elect termination of pregnancy. Those
who do not terminate pregnancy are offered prenatal.
Antibiotic therapy to reduce the frequency and severity of Toxoplasma
infection in the infant.
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
6
Congenitally infected neonates are treated with daily oral pyrimethamine (1
mg/kg) and sulfadiazine (100 mg/kg) with folinic acid for 1 year. Depending on
the signs and symptoms, prednisone (1 mg/kg per day) may be used for
congenital infection.
Amoebiasis
(Entamoeba histolytica)
objectves
To recognize the characteristics and transmission of amoebiasis.
To judge the types and clinical features of amoebiasis.
To assess the clinical and laboratory methods to diagnose a case of amoebiasis.
To illustrate drugs and methods of treatment of amoebiasis.
Introduciton
Amoebiasis is an infection with the intestinal protozoan Entamoeba histolytica.
About 90% of infections are asymptomatic, and the remaining 10% produce a
spectrum of clinical syndromes ranging from dysentery to abscesses of the liver or
other organs. It is spread between humans by its cysts. It is one of the leading
parasitic causes of morbidity and mortality in the tropics.
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
7
Life Cycle and Transmission
• E. histolytica is acquired by ingestion of viable cysts from fecally contaminated
water, food, or hands. Food-borne exposure is most prevalent and is
particularly likely when food handlers are shedding cysts, or food is being
grown with feces-contaminated soil, fertilizer, or water.
• Besides the drinking of contaminated water, less common means of
transmission include oral and anal sexual practices and—in rare instances—
direct rectal inoculation through colonic irrigation devices.
• Motile trophozoites are released from cysts in the small intestine, and, in most
patients, remain as harmless commensals in the large bowel. After encystation,
infectious cysts are shed in the stool and can survive for several weeks in a
moist environment.
• In some patients, the trophozoites invade either the bowel mucosa, causing
symptomatic colitis, or the bloodstream, causing distant abscesses of the liver,
lungs, or brain.
• The trophozoites may not encyst in patients with active dysentery, and motile
hematophagous trophozoites are frequently present in fresh stools.
• Trophozoites are rapidly killed by exposure to air or stomach acid, however,
and therefore cannot transmit infection.
• The parasite may invade the mucous membrane of the large bowel, producing
lesions that are maximal in the caecum but found as far down as the anal canal.
These are flask-shaped ulcers, varying greatly in size and surrounded by healthy
mucosa.
• A localized granuloma (amoeboma), presenting as a palpable mass in the
rectum or a filling defect in the colon on radiography, is a rare complication
which should be differentiated from colonic carcinoma.
• Amoebic ulcers may cause severe haemorrhage but rarely perforate the bowel
wall.
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
8
• Amoebic trophozoites can emerge from the vegetative cyst from the bowel and
be carried to the liver in a portal venule. They can multiply rapidly and destroy
the liver parenchyma, causing an abscess The liquid contents at first have a
characteristic pinkish colour which may later change to chocolate brown (like
anchovy sauce).
• Cutaneous amoebiasis, though rare, causes progressive genital, perianal or
peri-abdominal surgical wound ulceration.
Clinical features
Intestinal amoebiasis-amoebic dysentery.
Most amoebic infections are asymptomatic.
The incubation period of amoebiasis ranges from 2 weeks to many years,
followed by a chronic course with abdominal pains and two or more unformed
stools a day.
Offensive diarrhoea alternating with constipation, and blood or mucus in the
stool are common.
There may be abdominal pain, especially right lower quadrant (which may
simulate acute appendicitis).
A dysenteric presentation with passage of blood, simulating bacillary dysentery
or ulcerative colitis, occurs particularly in older people, in the puerperium* and
with superadded pyogenic infection of the ulcers.
*
Puerperium is defined as the time from the delivery of the placenta through the first
few weeks after the delivery. This period is usually considered to be 6 weeks in duration
(or
the period between childbirth and the return of the uterus to its normal size).
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
9
Amoebic liver abscess
The abscess is usually found in the right hepatic lobe. There may not be
associated diarrhoea. Early symptoms may be local discomfort only and
malaise; later, a swinging temperature and sweating may develop, usually
without marked systemic symptoms or associated cardiovascular signs.
An enlarged, tender liver, cough, and pain in the right shoulder (referred pain
from the irritation of diaphragm which is innervated by the phrenic n.) are
characteristic, but symptoms may remain vague and signs minimal.
A large abscess may penetrate the diaphragm and rupture into the lung, from
where its contents may be coughed up. Rupture into the pleural cavity, the
peritoneal cavity or pericardial sac is less common but more serious.
Investigations
The stool and any exudate should be examined at once under the microscope
for motile trophozoites containing red blood cells. Movements cease rapidly as
the stool preparation cools. Several stools may need to be examined in chronic
amoebiasis before cysts are found. Sigmoidoscopy may reveal typical flask-
shaped ulcers, which should be scraped and examined immediately for E.
histolytica.
In endemic areas one-third of the population are symptomless passers of
amoebic cysts.
An amoebic abscess of the liver is suspected on clinical grounds; there is often
a neutrophil leucocytosis and a raised right hemi-diaphragm on chest X-ray.
Confirmation is by ultrasonic scanning.
Aspirated pus from an amoebic abscess has the characteristic anchovy sauce
or chocolate brown appearance but only rarely contains free amoebae.
Toxoplasmosis - Amoebiasis Dr. Abdulla Al-Farttoosi
18-3-2015
10
Serum antibodies are detectable by immunofluorescence in over 95% of
patients with hepatic amoebiasis and intestinal amoeboma, but in only about
60% of dysenteric amoebiasis.
DNA detection by PCR has been shown to be useful in diagnosis of E. histolytica
infections but is not generally available.
Management
o Intestinal and early hepatic amoebiasis responds quickly to oral metronidazole
(800 mg 8-hourly for 5-10 days) or other long-acting nitroimidazoles like
tinidazole or ornidazole (both in doses of 2 g daily for 3 days). Either diloxanide
furoate or paromomycin, in doses of 500 mg orally 8-hourly for 10 days after
treatment, should be given to eliminate luminal cysts.
o If a liver abscess is large or threatens to burst, or if the response to
chemotherapy is not prompt, aspiration is required and is repeated if
necessary.
o Rupture of an abscess into the pleural cavity, pericardial sac or peritoneal
cavity necessitates immediate aspiration or surgical drainage. Small serous
effusions resolve without drainage.
