Dr. Abdulla Al-Farttoosi
Lec. 2
Malaria
Wed 25 / 3 / 2015
2014 – 2015
ﻣﻜﺘﺐ ﺍﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
1
Malaria
Malaria is defined as a mosquito-borne infectious disease of humans and
other animals caused by parasitic protozoans of the genus Plasmodium
transmitted via a bite from an infected female Anopheles mosquito.
The name "malaria" comes from the Italian mal (bad) and aria (air) – it was
originally thought the disease was spread by the damp air from swamps.
It is the most important of the parasitic diseases of humans, with transmission
in 107 countries. Malaria is a major public health problem in warm climates
especially in developing countries.
WHO: 2012 estimated 627 000 deaths (with an range of 473 000 to 789 000),
mostly among African children. Mortality rates ↓ 45% globally since 2000, by
49% in the African Region.
Epidemiology
Malaria occurs throughout most of the tropical regions of the world.
P. falciparum predominates in Africa, New Guinea, and Haiti; P. vivax is more
common in Central America. The prevalence of these two species is
approximately equal in South America, the Indian subcontinent, eastern Asia,
and Oceania.
P. malariae is found in most endemic areas, especially throughout sub-Saharan
Africa, but is much less common. P. ovale is relatively unusual outside of Africa
and, where it is found, comprises <1% of isolates.
Endemicity traditionally has been defined in terms of parasitemia rates or
palpable-spleen rates in children 2–9 years of age as hypoendemic (<10%),
mesoendemic (11–50%), hyperendemic (51–75%), and holoendemic (>75%).
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
2
The principal determinants of the epidemiology of malaria are the number
(density), the human-biting habits, and the longevity of the anopheline
mosquito vectors.
It is a leading cause of disease and death among children under five years,
pregnant women, and non-immune travellers/immigrants.
Five species of Plasmodium can infect and be transmitted by humans.
The vast majority of deaths are caused by P. falciparum, its prevalence is 75%.
P. vivax prevalence is 20%, most common outside Africa.
P. ovale, and P. malariae cause a milder form of malaria, rarely fatal.
The zoonotic species P. knowlesi, prevalent in Southeast Asia, causes malaria
in macaques but can also cause severe infections in humans.
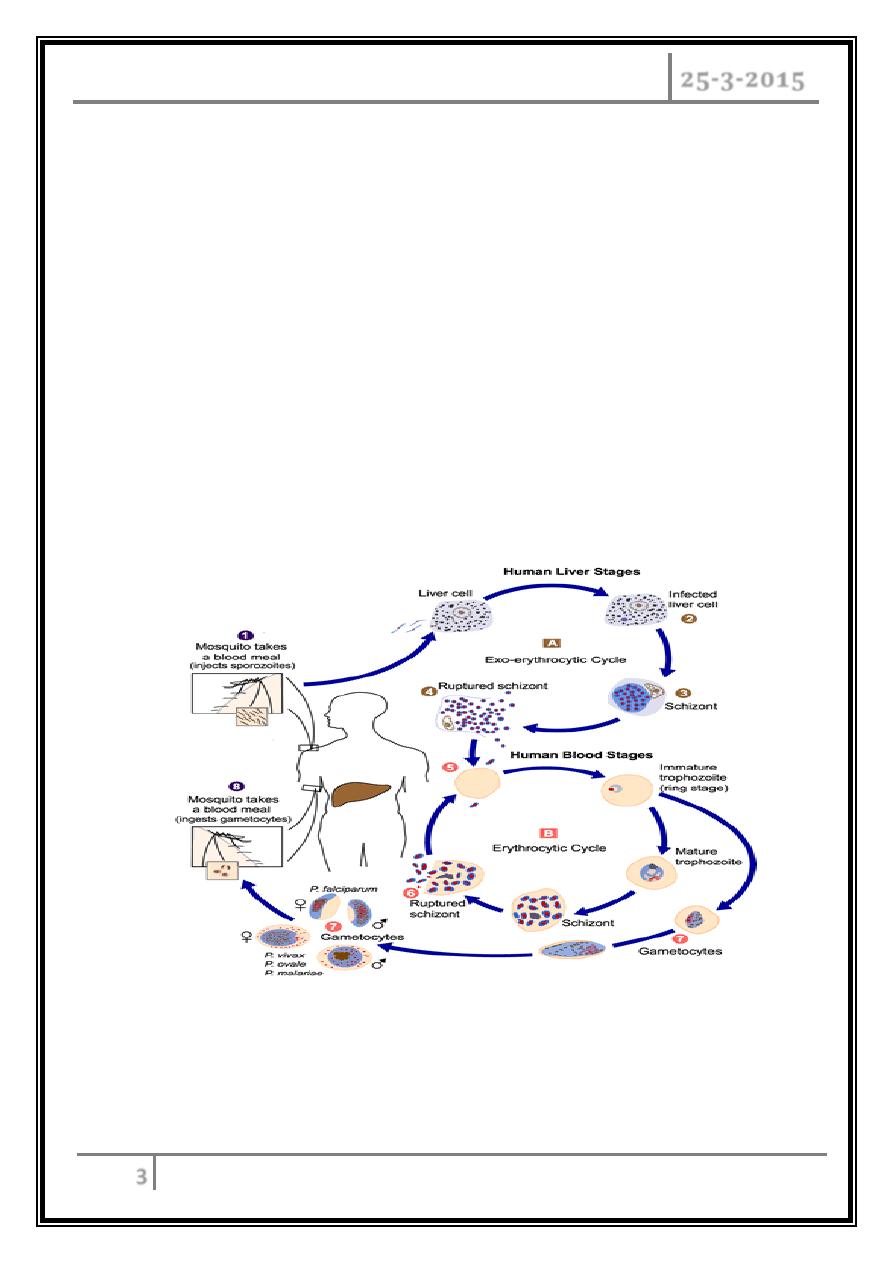
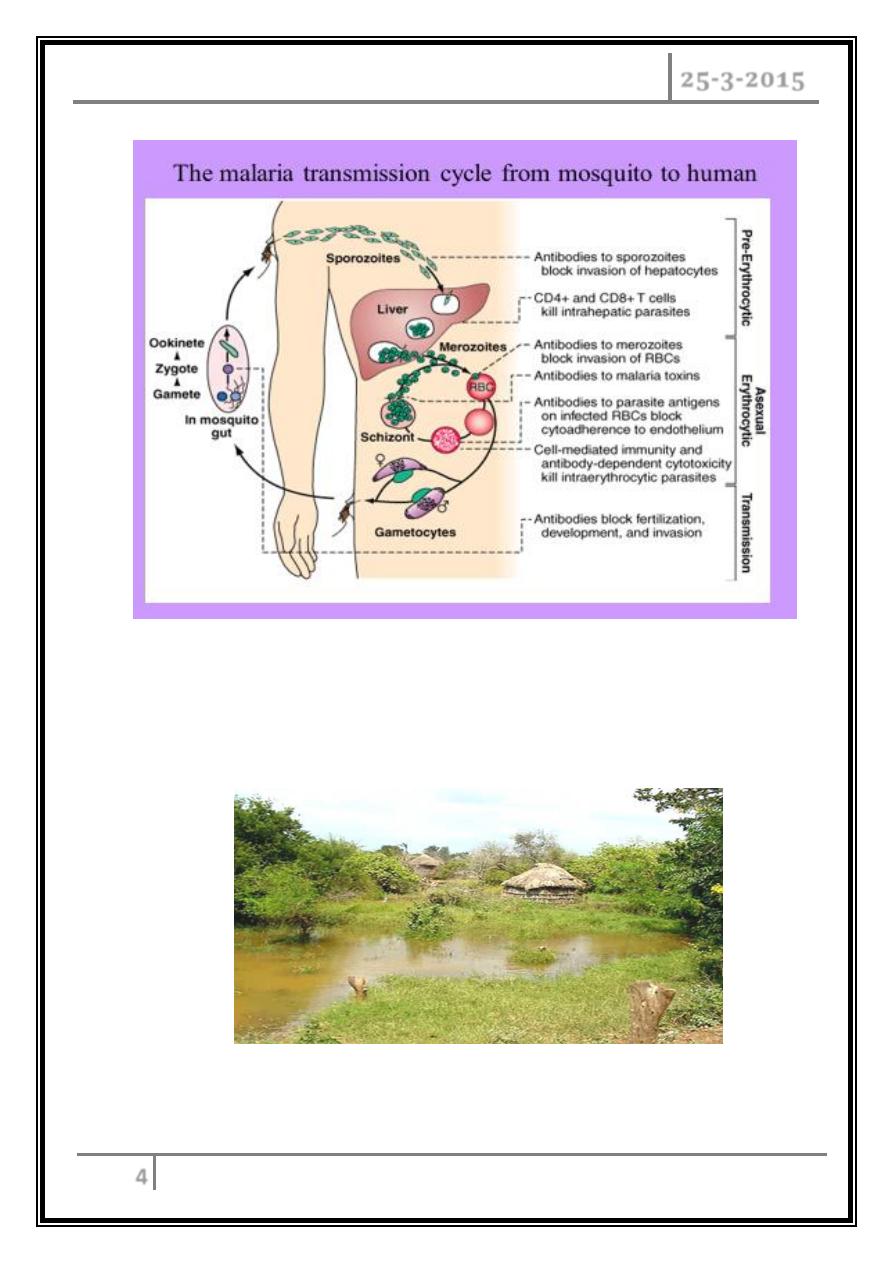
Life cycle of the malarial parasite
The female anopheline mosquito becomes infected when it feeds on human
blood containing gametocytes, the sexual forms of the malarial parasite.
Development in the mosquito takes from 7 to 20 days, and results in
sporozoites accumulating in the salivary glands which are inoculated into the
human blood stream.
Sporozoites disappear from human blood within half an hour and enter the
liver.
After some days merozoites leave the liver and invade red blood cells, where
further asexual cycles of multiplication take place, producing schizonts.
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
3
Rupture of the schizont releases more merozoites into the blood and causes
fever, the periodicity of which depends on the species of parasite.
P. vivax and P. ovale may persist in liver cells as dormant forms, hypnozoites,
capable of developing into merozoites months or years later.
Thus the first attack of clinical malaria may occur long after the patient has left
the endemic area, and the disease may relapse after treatment if drugs that kill
only the erythrocytic stage of the parasite are given.
P. falciparum and P. malariae have no persistent exo-erythrocytic phase but
recrudescence of fever may result from multiplication of parasites in red cells
which have not been eliminated by treatment and immune processes.
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
4
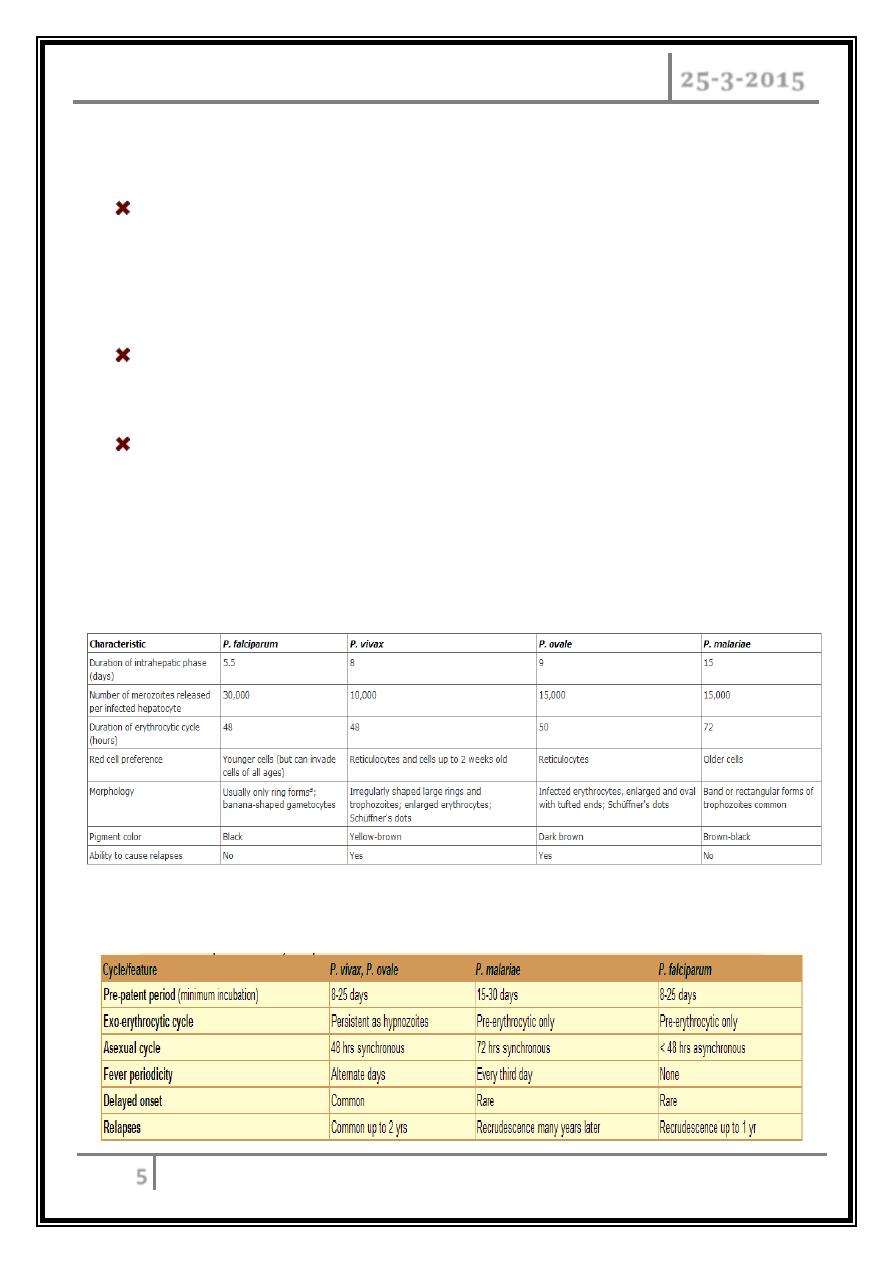
- A warm, humid climate - temperatures between 16°C and 40°C and abundant
rainfall have anopheles mosquitoes.
- Vegetation nearby to provide shade for the mosquito to hide during the day
and digest the blood meal from the night before.
A high risk area – vegetation cover and standing water during the wet season
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
5
Pathology
Red cells infected with malaria are prone to haemolysis. This is most severe
with P. falciparum, which invades red cells of all ages but especially young cells;
P. vivax and P. ovale invade reticulocytes, and P. malariae invades normoblasts,
so that infections remain lighter.
Anaemia may be profound and is worsened by dyserythropoiesis,
splenomegaly and depletion of folate stores.
In P. falciparum malaria, red cells containing trophozoites adhere to vascular
endothelium in post-capillary venules in brain, kidney, liver, lungs and gut. The
vessels become congested, resulting in widespread organ damage which is
exacerbated by rupture of schizonts, liberating toxic and antigenic substances.
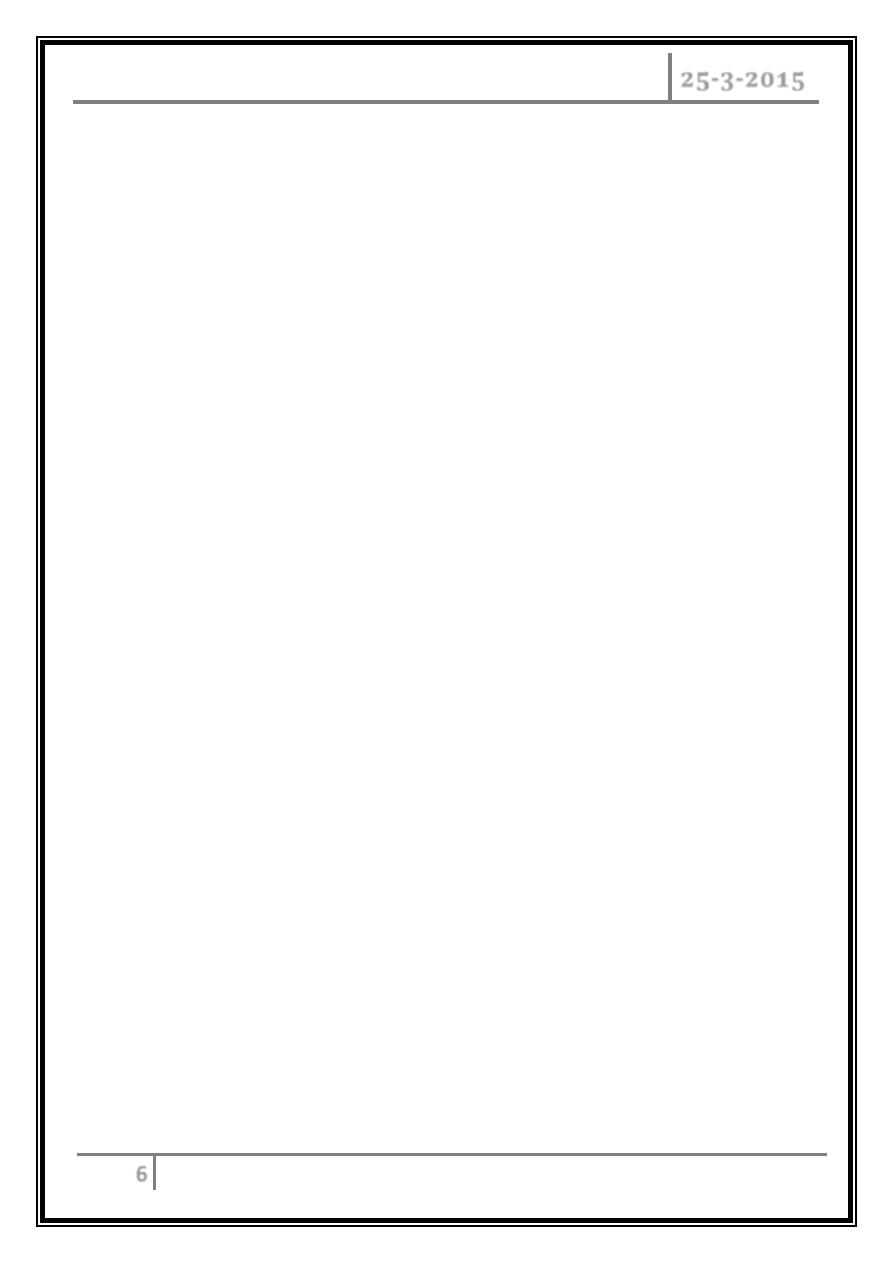
Characteristics of Plasmodium Species Infecting Humans
Relationships between life cycle of parasite and clinical features of malaria
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
6
Erythrocyte Changes in Malaria
After invading an erythrocyte, the growing malarial parasite progressively
consumes and degrades intracellular proteins, principally hemoglobin. The
potentially toxic heme is detoxified by polymerization to biologically inert
hemozoin (malaria pigment).
The parasite also alters the RBC membrane by changing its transport
properties, exposing cryptic surface antigens, and inserting new parasite-
derived proteins.
The RBC becomes more irregular in shape, more antigenic, and less
deformable.
In P. falciparum infections, membrane protuberances appear on the
erythrocyte's surface 12–15 h after the cell's invasion. These "knobs" extrude a
high-molecular-weight, antigenically variant, strain-specific erythrocyte
membrane adhesive protein (PfEMP1) that mediates attachment to receptors
on venular and capillary endothelium—an event termed cytoadherence.
In P. falciparum infections, membrane protuberances appear on the
erythrocyte's surface 12–15 h after the cell's invasion.
Several vascular receptors have been identified, of which intercellular adhesion
molecule 1 (ICAM-1) is probably the most important in the brain, chondroitin
sulfate B in the placenta, and CD36 in most other organs.
The infected erythrocytes stick inside and eventually block capillaries and
venules. At the same stage, these P. falciparum–infected RBCs may also adhere
to uninfected RBCs (to form rosettes) and to other parasitized erythrocytes
(agglutination).
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
7
The processes of cytoadherence, rosetting, and agglutination are central to the
pathogenesis of falciparum malaria. They result in the sequestration of RBCs
containing mature forms of the parasite in vital organs (particularly the brain),
where they interfere with microcirculatory flow and metabolism.
Sequestered parasites continue to develop out of reach of the principal host
defense mechanism: splenic processing and filtration.
As a consequence, only the younger ring forms of the asexual parasites are
seen circulating in the peripheral blood in falciparum malaria, and the level of
peripheral parasitemia underestimates the true number of parasites within the
body.
Severe malaria is also associated with reduced deformability of the uninfected
erythrocytes, which compromises their passage through the partially
obstructed capillaries and venules and shortens RBC survival.
In the other three ("benign") malarias, sequestration does not occur, and all
stages of the parasite's development are evident on peripheral blood smears.
Whereas P. vivax, P. ovale, and P. malariae show a marked predilection for
either young RBCs (P. vivax, P. ovale) or old cells (P. malariae) and produce a
level of parasitemia that is seldom >2%, P. falciparum can invade erythrocytes
of all ages and may be associated with very high levels of parasitemia.
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
8
Host Response
Initially, the host responds to plasmodial infection by activating nonspecific
defense mechanisms. Splenic immunologic and filtrative clearance functions
are augmented in malaria.
The parasitized cells escaping splenic removal are destroyed when the schizont
ruptures.
The material released induces the activation of macrophages and the release of
pro-inflammatory mononuclear cell-derived cytokines, which cause fever and
exert other pathologic effects.
Temperatures of 40°C damage mature parasites; in untreated infections, the
effect of such temperatures is to further synchronize the parasitic cycle, with
eventual production of the regular fever spikes and rigors that originally served
to characterize the different malarias.
These regular fever patterns (tertian, every 2 days; quartan, every 3 days) are
seldom seen today in patients who receive prompt and effective antimalarial
treatment.
The decrease in risk for malaria in sickle cell disease, ovalocytosis, thalassemia,
and glucose-6-phosphate dehydrogenase deficiency (G6PD) appears to be
related to impaired parasite growth at low oxygen tensions.
Nonspecific host defense mechanisms stop the infection's expansion, and the
subsequent specific immune response controls the infection.
Immune individuals have a polyclonal increase in serum levels of IgM, IgG, and
IgA, although much of this antibody is unrelated to protection.
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
9
Several factors retard the development of cellular immunity to malaria. These
factors include the absence of major histocompatibility antigens on the surface
of infected RBCs, which precludes direct T cell recognition; malaria antigen-
specific immune unresponsiveness; and the enormous strain diversity of
malarial parasites, along with the ability of the parasites to express variant
immunodominant antigens on the erythrocyte surface that change during the
period of infection.
Symptoms typically begin 8–25 days following infection, or later in those who
have taken anti-malarial medications as prevention.
Initially flu-like symptoms, but can resemble septicemia, gastroenteritis,
and viral diseases.
The presentation may include headache, fever, shivering, joint
pain, vomiting, hemolytic anemia, jaundice, hemoglobin urea, retinal damage,
and convulsions.
The classic paroxysm:
A cyclical occurrence of sudden coldness, shivering and then fever and
sweating, occurring every two days (tertian fever) in P.vivax and P.ovale
infections, and every three days (quartan fever) for P. malariae.
P. falciparum infection can cause recurrent fever every 36–48 hours or a less
pronounced and almost continuous fever.
Severe malaria is usually caused by falciparum malaria which arises 9–30 days
after infection.
Individuals with cerebral malaria frequently exhibit neurological symptoms,
including abnormal posturing, nystagmus, opisthotonus, seizures, or coma.
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
10
Clinical features
P. falciparum infection
This is the most dangerous of the malarias and patients are either 'killed or
cured'. The onset is often insidious, with malaise, headache and vomiting. Cough and
mild diarrhoea are also common. The fever has no particular pattern. Jaundice is
common due to haemolysis and hepatic dysfunction. The liver and spleen enlarge and
may become tender. Anaemia develops rapidly, as does thrombocytopenia.
Severe manifestations/complications of falciparum malaria
o Coma (cerebral malaria).
o Hyperpyrexia.
o Convulsions.
o Hypoglycaemia
o Severe anaemia (packed cell
volume < 15%).
o Acute pulmonary oedema.
o Acute renal failure.
o Metabolic acidosis.
o Shock.
o Aspiration pneumonia.
o Hyperparasitaemia.
A patient with falciparum malaria, apparently not seriously ill, may rapidly
develop dangerous complications.
Cerebral malaria is manifested by confusion, seizures or coma, usually without
localizing signs.
Children die rapidly without any special symptoms other than fever.
Immunity is impaired in pregnancy and the parasite can preferentially bind to a
placental protein known as chondroitin sulphate A. Abortion and intrauterine
growth retardation from parasitisation of the maternal side of the placenta are
frequent. Previous splenectomy increases the risk of severe malaria.
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
11
P. vivax and P. ovale infection
In many cases the illness starts with several days of continued fever before the
development of classical bouts of fever on alternate days. Fever starts with a rigor.
The patient feels cold and the temperature rises to about 40 °C. After half an hour to
an hour the hot or flush phase begins. It lasts several hours and gives way to profuse
perspiration and a gradual fall in temperature. The cycle is repeated 48 hours later.
Gradually the spleen and liver enlarge and may become tender. Anaemia develops
slowly. Relapses are frequent in the first 2 years after leaving the malarious area and
infection may be acquired from blood transfusion.
P. malariae infection
This is usually associated with mild symptoms and bouts of fever every third
day. Parasitaemia may persist for many years with the occasional recrudescence of
fever, or without producing any symptoms. Chronic P. malariae infection causes
glomerulonephritis and long-term nephrotic syndrome in children.
Investigations
Giemsa-stained thick and thin blood films should be examined whenever
malaria is suspected.
With P. falciparum, only ring forms are normally seen in the early stages, while
with the other species all stages of the erythrocytic cycle may be found.
Gametocytes appear after about 2 weeks, persist after treatment and are
harmless, except that they are the source by which more mosquitoes become
infected.
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
12
Immunochromatographic tests for malaria antigens, such as OptiMal® (which
detects the Plasmodium lactate dehydrogenase of several species) and
ParasightF® (which detects the P. falciparum histidine-rich protein 2), are
extremely sensitive and specific for falciparum malaria but less so for other
species. They should be used in parallel with blood film examination but are
especially useful where the microscopist is less experienced in examining blood
films.
DNA detection (PCR) is used mainly in research and is useful for determining
whether a patient has a recrudescence of the same malaria parasite or a
reinfection with a new parasite.
Management
-
Mild P. falciparum malaria
Since P. falciparum is now resistant to chloroquine and sulfadoxine-
pyrimethamine (Fansidar) almost world-wide, an artemisinin-based
treatment is recommended. Co-artemether (CoArtem® or Riamet®)
contains artemether and lumefantrine and is given as 4 tablets at 0, 8, 24,
36, 48 and 60 hours.
Alternatives are quinine by mouth (600 mg of quinine salt every 8 hours for
5-7 days), together with or followed by either doxycycline (200 mg once
daily for 7 days) or clindamycin (450 mg every 8 hours for 7 days)
Doxycycline and artemether should be avoided in pregnancy.
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
13
-
Complicated P. falciparum malaria
Severe malaria should be considered in any non-immune patient with a
parasite count greater than 2% and is a medical emergency. Management
includes early and appropriate antimalarial chemotherapy, active treatment
of complications, correction of fluid, electrolyte and acid-base balance, and
avoidance of harmful ancillary treatments.
The treatment of choice is intravenous artesunate given as 2.4 mg/kg I.V. at
0, 12 and 24 hours and then once daily for 7 days.
Patients should be monitored by ECG, with special attention to QRS
duration and QT interval. Mefloquine should not be used for severe malaria
since no parenteral form is available.
Exchange transfusion has not been tested in randomized controlled trials
but may be beneficial for non-immune patients with persisting high
parasitaemias (> 10% circulating erythrocytes).
Management of non-falciparum malaria
P. vivax, P. ovale and P. malariae infections should be treated with oral
chloroquine: 600 mg chloroquine base followed by 300 mg base in 6 hours,
then 150 mg base 12-hourly for 2 more days. Some chloroquine resistance has
been reported.
Late relapses can be prevented by prescribing antimalarial drugs in suppressive
doses.
However, 'radical cure' is now achieved in most patients with P. vivax or P.
ovale malaria using a course of primaquine (15 mg daily for 14 days), which
destroys the hypnozoite phase in the liver. Haemolysis may develop in those
who are G6PD-deficient. Cyanosis due to the formation of methaemoglobin in
the red cells is more common but not dangerous.
MALARIA Dr. Abdulla Al-Farttoosi
25-3-2015
14
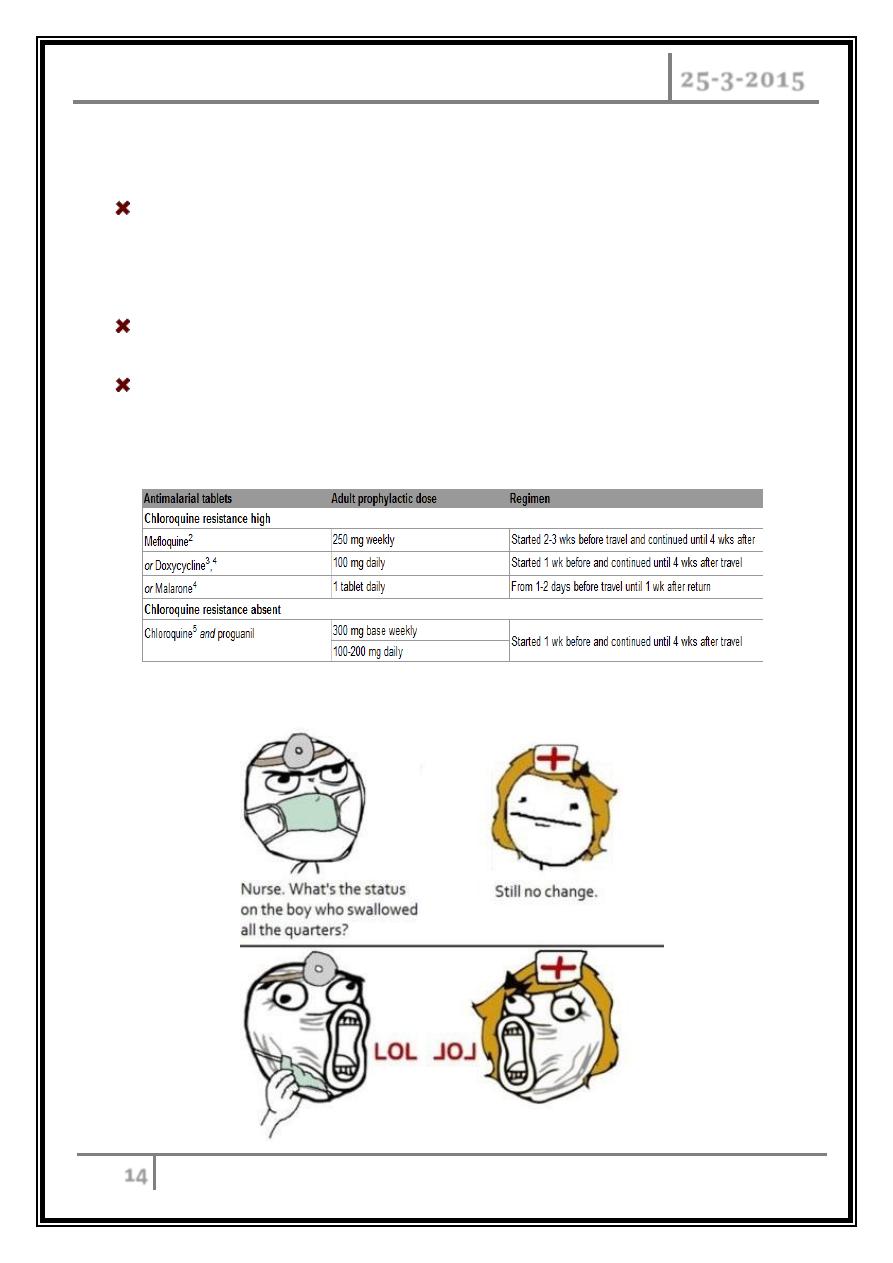
Prevention
Clinical attacks of malaria may be preventable with chemoprophylaxis using
chloroquine, atovaquone plus proguanil (Malarone), doxycycline or
mefloquine.
Pregnant and lactating women may take proguanil or chloroquine safely.
Prevention also involves advice about the use of high-percentage
diethyltoluamide (DEET), covering up extremities when out after dark and
sleeping under permethrin-impregnated mosquito nets.
… The end …
