Dr. Abdulla Al-Farttoosi
Lec. 3
Trematodes
Thurs.
26 / 3 / 2015
Done by : Ali Kareem
2014 – 2015
مكتب اشور لالستنساخ
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
2
INFECTIONS CAUSED BY HELMINTHS
Objectives :
To define Trematodes .
To determine types, life cycle and methods of its trasmission
To describe its epidemiology.
To recognize Clinical features of infestation with Trematodes.
To recognize investigations used for its diagnosis
To evaluate management of Trematodes
Helminths (from the Greek Helmins, meaning worm) include three groups of
parasitic worm large multicellular organisms with complex tissues and
organs.
Trematodes (flukes)
These leaf-shaped worms are parasitic to humans and animals. Their
complex life cycles may involve one or more intermediate hosts, often
freshwater molluscs.
Common Features of Human Trematodes
1- Most adult trematodes are dorsoventrally flattened, bilaterally symmetric,
leaf-shaped or tongue-like.
2- All of them have two suckers, an oral and a ventral sucker.
3- The digestive tract is degenerate. The end of intestine is a cecum without
anus.
4- The reproductive system is developed and hermaphroditic.
5- Excretory system includes flame cells, capillaries, collecting tubules and an
excretory bladder.
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
3
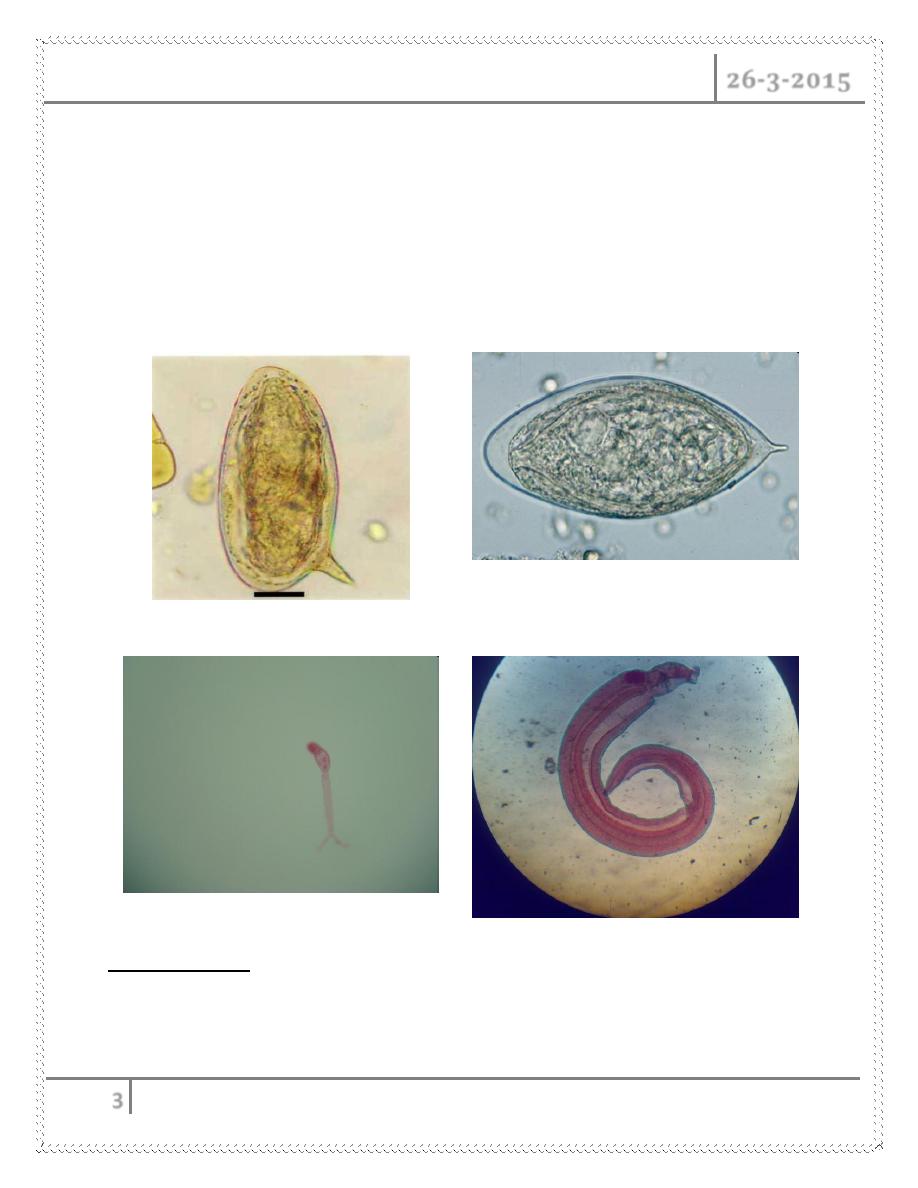
6- Eggs of most species have an operculum (lid) and/or a small spine (knob).
The developed egg contains a miracidium.
7- They are biohelminths. Only getting into fresh water can eggs develop. Their
intermediate hosts are in water. 1st intermediate hosts are all snails and 2nd
intermediate hosts varies from species.
8- Infetive stage is usually a metacercria
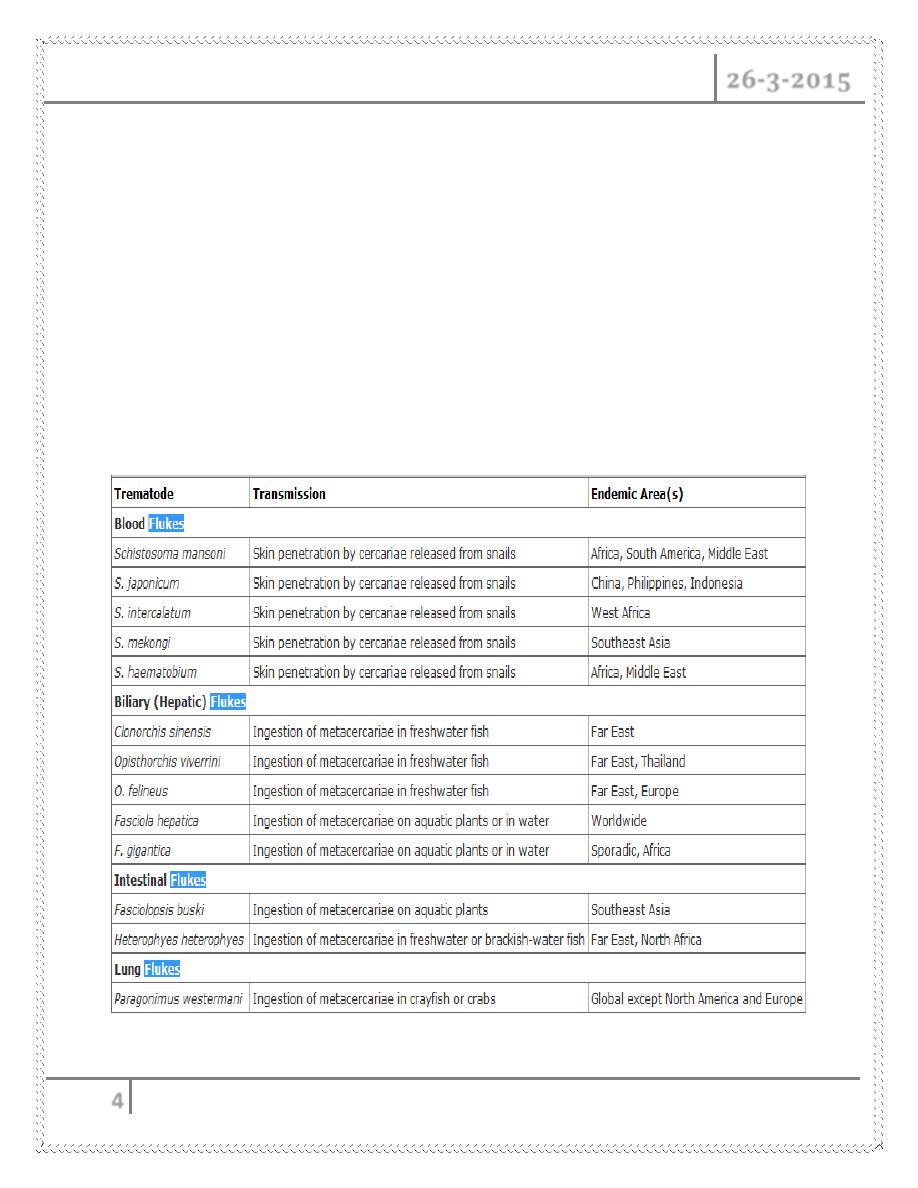
TREMATODES
The trematodes, or flatworms, may be classified according to the tissues
invaded by the adult flukes. The life cycle involves a definitive mammalian
Schistosoma mansoni egg
Schistosoma haematobium egg
Schistosoma spp. Cercaria
Schistosoma mansoni adult
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
4
host in whom adult worms produce eggs and an intermediate host (e.g.,
snails) in which larval forms multiply.
Worms do not multiply within the definitive host. Human infection results
from either direct penetration of intact skin or ingestion.
Blood flukes: Schistosoma haematobium, S. mansoni, S. japonicum, S.
mekongi, S. intercalatum
Lung flukes: Paragonimus spp.
Hepatobiliary flukes: Clonorchis sinensis, Fasciola hepatica, Opisthorchis
felineus
Intestinal flukes: Fasciolopsis buski
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
5
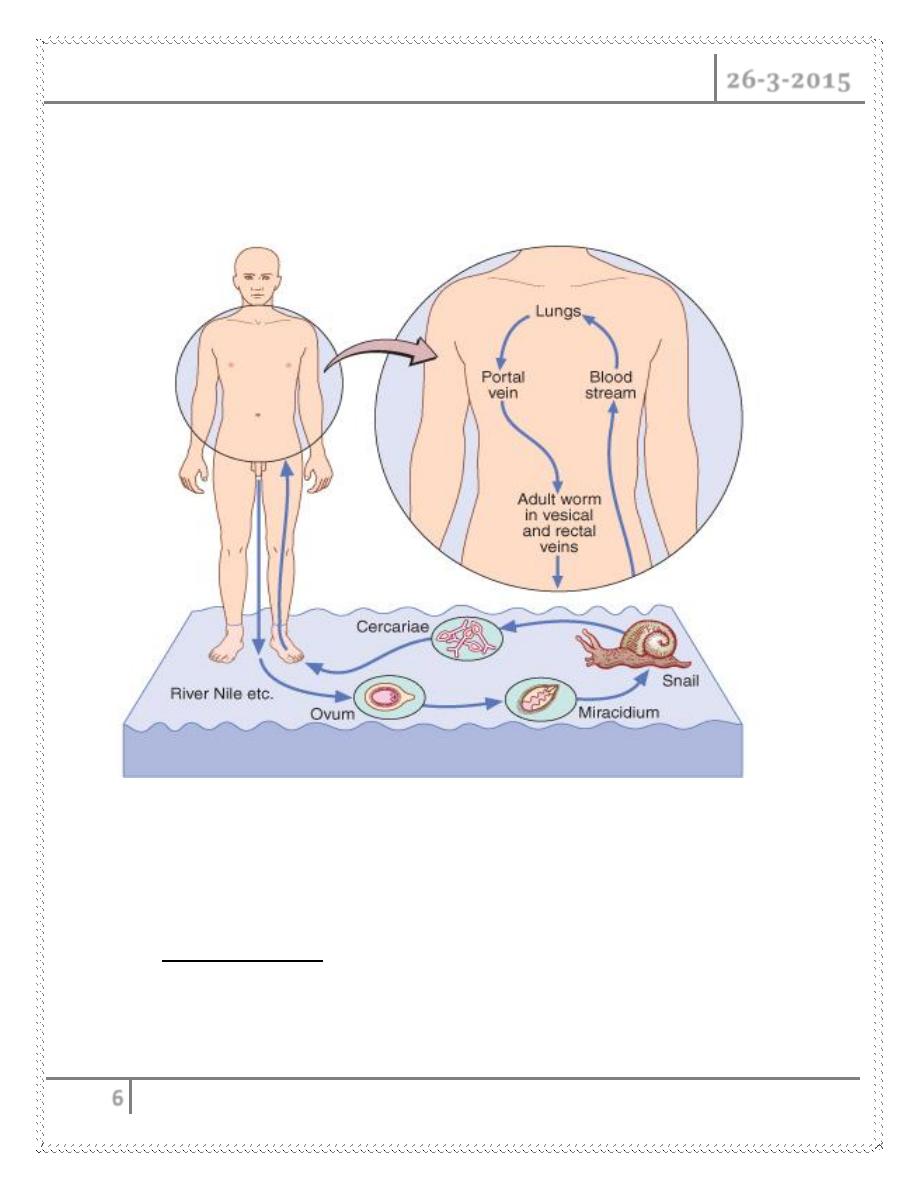
Schistosomiasis ( Bilharziasis )
Etiology
Schistosomes are blood flukes that infect 200–300 million persons worldwide. Five
species cause human schistosomiasis.
The intestinal species
Schistosoma mansoni: found in South America, Africa, and the Middle East.
S. japonicum: found in China, the Philippines, and Indonesia.
S. mekongi: found in Southeast Asia.
S. intercalatum: found in West and Central Africa.
The urinary species
S. haematobium: found in Africa and the Middle East
Pathogenesis
o Infection is initiated by penetration of intact skin by infective cercariae—the
form of the parasite released from snails in freshwater bodies.
o As they mature into schistosomes, the parasites reach the portal vein, mate,
then migrate to the venules of the bladder and ureters (S. haematobium) or
the mesentery (S. mansoni, S. japonicum, S. mekongi, S. intercalatum) and
deposit eggs.
o Some mature ova are extruded into the intestinal or urinary lumina, from
which they may be voided and ultimately may reach water and perpetuate
the life cycle. The persistence of other ova in tissues leads to a
granulomatous host response and fibrosis.
o Factors governing disease manifestations include the intensity and duration
of infection, the site of egg deposition, and the genetic characteristics of the
host.
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
6
o In the liver, granulomata cause presinusoidal portal blockage,
hemodynamic changes (including portal hypertension), and periportal
fibrosis. Similar processes occur in the bladder.
Clinical Features
In general, disease manifestations of schistosomiasis occur in three stages, which
vary not only by species but also by intensity of infection and other host factors,
such as age and genetics.
1. Cercarial invasion :
a form of dermatitis may be observed. This so-called swimmers’ itch
occurs most often with S. mansoni and S. japonicum infections,
manifesting 2 or 3 days after invasion as an itchy maculopapular rash
on the affected areas of the skin.
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
7
The condition is particularly severe when humans are exposed to
avian schistosomes. Cercarial dermatitis is a self-limiting clinical
entity
2. Worm maturation and at the beginning of oviposition (i.e., 4 to 8 weeks
after skin invasion) :
acute schistosomiasis or Katayama fever
Serum sickness–like syndrome with fever, generalized
lymphadenopathy, and hepatosplenomegaly.
High degree of peripheral blood eosinophilia.
Parasite-specific antibodies may be detected before schistosome eggs
are identified in excreta.
The course of acute schistosomiasis is generally benign, but deaths
are occasionally reported in association with heavy exposure to
schistosomes.
3. Chronic schistosomiasis : species-dependent
A- Intestinal and hepatosplenic disease
By Intestinal species (S. mansoni, S. japonicum, S. mekongi, and S.
intercalatum).
Intestinal phase
During the intestinal phase, which may begin a few months after
infection and may last for years, symptomatic patients
characteristically have colicky abdominal pain and bloody diarrhea.
Patients may also report fatigue and an inability to perform daily
routine functions and may show evidence of growth retardation.
The severity of intestinal schistosomiasis is often related to the
intensity of the worm burden. The disease runs a chronic course but
rarely progresses to a functional level (e.g., malabsorption) or to
anatomical lesions of the gut. The exception is colonic polyposis,
which has been seen in some endemic areas, such as Egypt.
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
8
Hepatosplenic phase
The hepatosplenic phase of disease manifests early (during the first
year of infection, particularly in children) with enlargement of the
liver due to parasite-induced granulomatous lesions.
Hepatomegaly is seen in 15 to 20% of infected individuals. In
subsequent phases of infection, presinusoidal blockage of blood flow
leads to portal hypertension and splenomegaly. Moreover, portal
hypertension may lead to varices at the lower end of the esophagus
and at other sites.
Patients with schistosomal liver disease may have right-upper-
quadrant ―dragging‖ pain during the hepatomegaly phase, and this
pain may move to the left upper quadrant as splenomegaly
progresses. Bleeding from esophageal varices may, however, be the
first clinical manifestation of this phase.
Patients may experience repeated bleeding but seem to tolerate its
impact, since an adequate total hepatic blood flow permits normal
liver function for a considerable period in schistosomal
hepatomegaly.
In late-stage disease, typical fibrotic changes occur along with liver
function deterioration and the onset of ascites, hypoalbuminemia, and
defects in coagulation.
Intercurrent viral infections of the liver (especially hepatitis B and C)
or nutritional deficiencies may well accelerate or exacerbate the
deterioration of hepatic function.
B- Vesical infection : by S. haematobium infection.
The clinical manifestations occur relatively early and involve a
relatively high percentage of individuals. Up to 80% of children
infected with S. haematobium have dysuria, frequency, and hematuria,
which may be terminal.
Urine examination reveals blood and albumin as well as an unusually
high frequency of bacterial urinary tract infection and urinary
sediment cellular metaplasia.
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
9
These manifestations correlate with intensity of infection, the presence
of urinary bladder granulomas, and subsequent ulceration. Along
with the local effects of granuloma formation in the urinary bladder,
obstruction of the lower end of the ureters results in hydroureter and
hydronephrosis, which can be seen in 25 to 50% of infected children.
As infection progresses, bladder granulomas undergo fibrosis; the
result is the presence of typical sandy patches visible on cystoscopy.
In many endemic areas, an association between squamous cell
carcinoma of the bladder and S. haematobium infection has been
observed.
Such malignancy is detected in a younger age group than is
transitional cell carcinoma. In fact, S. haematobium has now been
classified as a human carcinogen.
C- Pulmonary schistosomiasis :
Embolized eggs lodge in small arterioles, producing acute necrotizing
arteriolitis and granuloma formation. After the development of
arteriolitis and granuloma formation, fibrous tissue deposition is
detected and leads to endarteritis obliterans, pulmonary hypertension,
and cor pulmonale.
The most frequent symptoms are cough, fever, and dyspnea; ascites
and hemoptysis are less frequently encountered.
D- CNS schistosomiasis : is important but less common than pulmonary
schistosomiasis.
It characteristically occurs as cerebral disease due to S. japonicum
infection.
Migratory worms deposit eggs in the brain and induce a
granulomatous response. Jacksonian epilepsy due to S. japonicum
infection is the second most common cause of epilepsy in these areas.
S. mansoni and S. haematobium infections have been associated with
transverse myelitis. This syndrome is thought to be due to eggs
traveling to the venous plexus around the spinal cord. Patients usually
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
10
present with acute or rapidly progressing lower-leg weakness
accompanied by sphincter dysfunction.
DIAGNOSIS
Central to correct diagnosis is a thorough inquiry into travel history and
exposure to freshwater bodies, whether slow or fast running.
In cases of Katayama fever, prompt diagnosis is essential and is based on
clinical presentation, high-level peripheral blood eosinophilia, and a
positive serologic assay for schistosomal antibodies.
Two tests are available: a screening test/enzyme-linked immunosorbent
assay (FAST-ELISA) and the confirmatory enzyme-linked
immunoelectrotransfer blot (EITB).
Both tests are highly sensitive and 96% specific. In some instances,
examination of stool or urine for ova may yield positive results.
Individuals with established infection are diagnosed by a combination of
geographic history, characteristic clinical presentation, and presence of
schistosome ova in excreta.
The diagnosis may also be established with the serologic assays mentioned
above or with those that detect circulating schistosome antigens.
These assays can be applied either to blood or to other body fluids (e.g.,
cerebrospinal fluid). For stool examination, the Kato thick smear or any
other concentration method generally identifies all but the most lightly
infected individuals. Urine may be examined by microscopy of sediment or
by filtration of a known volume through Nuclepore filters.
Kato thick smear and Nuclepore filtration provide quantitative data on the
intensity of infection, which is of value in assessing the degree of tissue
damage and in monitoring the effect of chemotherapy.
Finally, schistosome infection may be diagnosed by examination of tissue
samples, typically rectal biopsies; other biopsy procedures (e.g., liver
biopsy) are not needed, except in special circumstances.
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
11
Differential diagnosis of schistosomal hepatomegaly must include viral
hepatitis of all etiologies, miliary tuberculosis, malaria, visceral
leishmaniasis, ethanol abuse, and causes of hepatic and portal vein
obstruction. Of patients with these conditions, only a few may present with
organomegaly and relatively intact liver function.
The differential diagnosis of hematuria in S. haematobium infection includes
bacterial cystitis, tuberculosis, urinary stones, and malignancy.
TREATMENT
Treatment of schistosomiasis depends on the stage of infection and the
clinical presentation.
Other than topical dermatologic applications for relief of itching, no specific
treatment is indicated for cercarial dermatitis caused by avian schistosomes.
Therapy for acute schistosomiasis or Katayama fever needs to be adjusted
appropriately for each case. In severe acute schistosomiasis, management in
an acute-care setting is necessary, with supportive measures and
consideration of glucocorticoid treatment. Once the acute critical phase is
over, specific chemotherapy is indicated.
For all individuals with infection established by either the demonstration of
schistosome eggs or positive serology, treatment to eradicate the parasite
should be administered. The drug of choice is praziquantel, which results in
parasitologic cure in 85% of cases and reduces egg counts by >90%.
The recommended doses are 20 mg/kg bid for 1 day for S. mansoni, S.
intercalatum, and S. haematobium infections and 20 mg/kg tid for 1 day for
S. japonicum and S. mekongi infections. The effect of antischistosomal
treatment on disease manifestations varies by stage.
Early hepatomegaly and bladder lesions are known to resolve following
chemotherapy, but the late established manifestations, such as fibrosis, do
not change.
Additional management modalities are needed for individuals with other
manifestations, such as hepatocellular failure or recurrent hematemesis. The
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
12
use of these interventions is guided by general medical and surgical
principles.
PREVENTION
o Travelers should avoid contact with all freshwater bodies. In endemic areas,
several control measures have been used, including application of
molluscicides, provision of sanitary water and means for sewage disposal,
chemotherapy, and health education.
o Current recommendations to countries endemic for schistosomiasis
emphasize the use of multiple approaches.
o Particularly with the advent of an oral, safe, and effective antischistosomal
agent, chemotherapy has been most successful in reducing the intensity of
infection and reversing disease.
Liver (Biliary) Flukes
Stool ova and parasite (O & P) examination diagnoses infection with liver flukes.
Clonorchiasis and opisthorchiasis occur in Southeast Asia. Infection is
acquired by ingestion of contaminated raw freshwater fish.
Chronic infection causes cholangitis, cholangiohepatitis, and biliary
obstruction and is associated with cholangiocarcinoma. Therapy for acute
infection consists of praziquantel administration (25 mg/kg tid for 1 day).
Fascioliasis is endemic in sheep-raising countries. Infection is acquired by
ingestion of contaminated aquatic plants (e.g., watercress). Acute disease
causes fever, RUQ pain, hepatomegaly, and eosinophilia.
Chronic infection is associated with bile duct obstruction and biliary
cirrhosis. For treatment, triclabendazole is given as a single dose of10
mg/kg.
TREMATODES Dr. Abdulla Al-Farttoosi
26-3-2015
13
Lung Flukes
Infection with Paragonimus spp. is acquired by ingestion of contaminated
crayfish and freshwater crabs.
Acute infection causes lung hemorrhage, necrosis with cyst formation, and
parenchymal eosinophilic infiltrates. A productive cough, with brownish or
bloody sputum, in association with peripheral blood eosinophilia is the
usual presentation in pts with heavy infection.
In chronic cases, bronchitis or bronchiectasis may predominate. CNS
disease can also occur and can result in seizures. The diagnosis is made by
O & P examination of sputum or stool. Praziquantel (25 mg/kg tid for 1 day)
is the therapeutic agent of choice.
D
N
E
#
Done by
Ali Kareem
