Dr. Abdulla Al-Farttoosi
Lec. 4
Nematodes
Wed 1 / 4 / 2015
2014 – 2015
ﻣﻜﺘﺐ ﺍﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
1
NEMATODES
Objectives
To define nematodes.
To determine methods of its classification.
To describe its epidemiology.
To recognize life cycle and Clinical features of nematodes infection.
To asses and investigate a case of nematodes infection.
To evaluate lines of management of nematodes.
Introducion
The nematodes, or roundworms, that are of medical significance can be
classified as either tissue or intestinal parasites.
Intestinal human nematodes: Ancylostoma duodenale, Necator americanus,
Strongyloides stercoralis, Ascaris lumbricoides, Enterobius vermicularis,
Trichuris trichiura.
Tissue-dwelling human nematodes: Wuchereria bancrofti, Brugia malayi, Loa
loa, Onchocerca volvulus, Dracunculus medinensis, Mansonella perstans,
Dirofilaria immitis.
Zoonotic nematodes: Trichinella spiralis
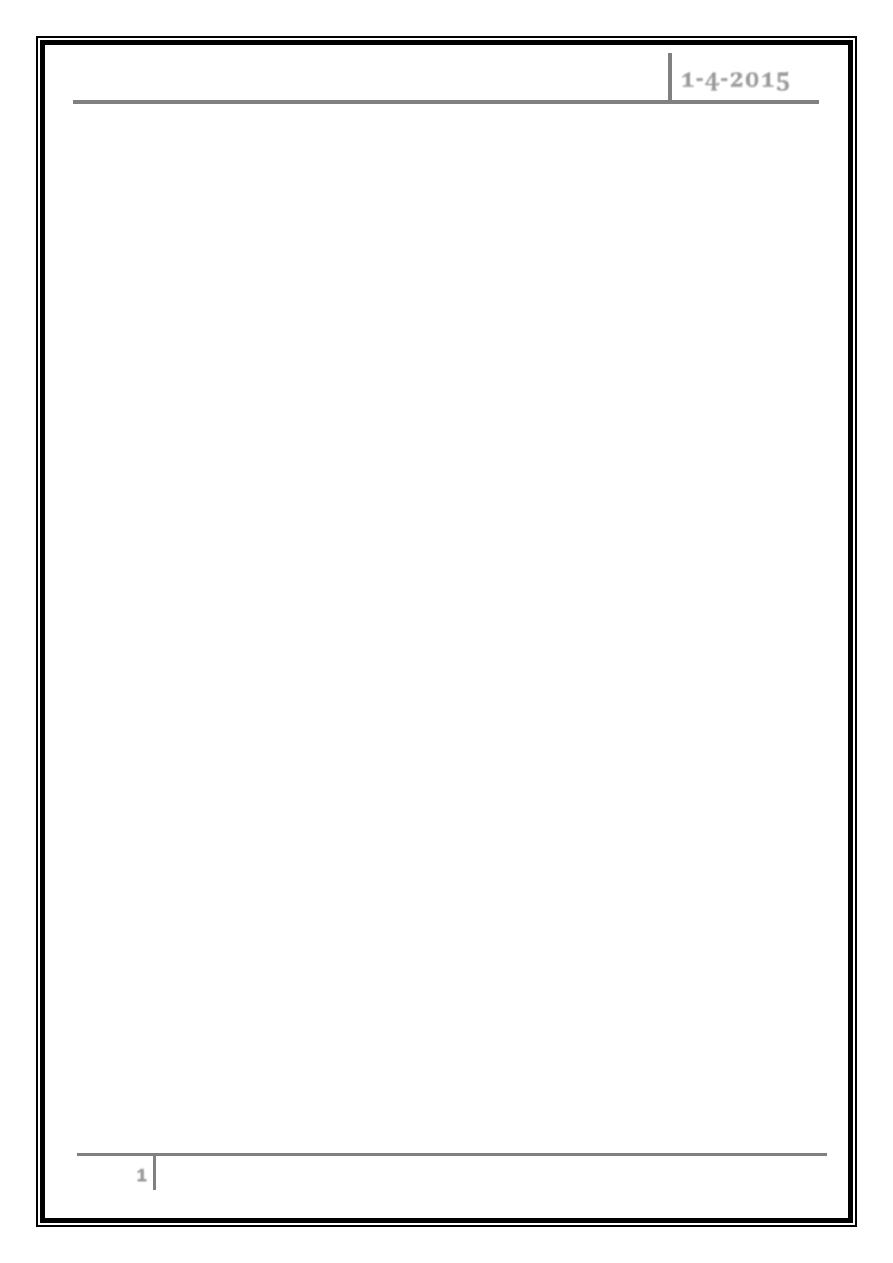
TRICHINELLOSIS
Etiology:
T. spiralis and six other Trichinella species cause human infection.
Life Cycle and Epidemiology:
Infection results when humans ingest meat (usually pork) that contains cysts
with Trichinella larvae. During the first week of infection, the larvae invade the
small-bowel mucosa; during the second and third weeks, they mature into adult
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
2
worms, which release new larvae that migrate to striated muscles via the
circulation and encyst.
Clinical Features:
Light infections (<10 larvae per gram of muscle) are asymptomatic. A burden
of >50 larvae per gram can cause fatal disease.
Week 1: diarrhea, abdominal pain, constipation, nausea, and/or vomiting.
Week 2: hypersensitivity reactions with fever and hypereosinophilia;
periorbital and facial edema; hemorrhages in conjunctivae, retina, and nail
beds; maculopapular rash, headache, cough, dyspnea, and dysphagia.
Deaths are usually due to myocarditis with arrhythmias or CHF and are less
often caused by pneumonitis or encephalitis.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
3
Weeks 2-3: myositis, myalgias, muscle edema, weakness (especially in
extraocular muscles, biceps, neck, lower back, and diaphragm). Symptoms
peak at 3 weeks; convalescence is prolonged.
Diagnosis:
Eosinophilia in >90% of pts, peaking at a level of >50% at 2–4 weeks.
Elevated IgE and muscle enzyme levels; increase in specific antibody titers by
week 3.
A definitive diagnosis is made by the detection of larvae on biopsy of at least
1 g of muscle tissue. Yields are highest near tendon insertions.
Treatment:
Drugs are ineffective against muscle larvae, but mebendazole and
albendazole may be active against enteric-stage parasites. Glucocorticoids
(1 mg/kg daily for 5 days) may reduce severe myositis and myocarditis.
Prevention:
Cooking pork until it is no longer pink or freezing it at -15
o
C for 3 weeks kills
larvae and prevents infection.
VISCERAL AND OCULAR LARVA MIGRANS
Etiology:
Most cases of larva migrans are caused by Toxocara canis.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
4
Life Cycle and Epidemiology:
Infection results when humans—most often preschool children—ingest soil
contaminated by puppy feces that contain infective T. canis eggs. Larvae penetrate
the intestinal mucosa and disseminate hematogenously to a wide variety of organs
(e.g., liver, lungs, CNS), provoking intense eosinophilic granulomatous responses.
Clinical Features:
Heavy infections may cause fever, malaise, anorexia, weight loss, cough,
wheezing, rashes, and hepatosplenomegaly. Ocular disease usually develops in
older children or young adults and may cause an eosinophilic mass that mimics
retinoblastoma, endophthalmitis, uveitis, or chorioretinitis.
Diagnosis:
o No eggs are found in the stool because larvae do not develop into adult
worms.
o Blood eosinophilia up to 90%, leukocytosis, and hypergammaglobulinemia
may be evident.
o Toxocaral antibodies detected by ELISA can confirm the diagnosis.
Treatmen:
Glucocorticoids can reduce inflammatory complications. Only ocular infections
require treatment: albendazole (800 mg bid for adults and 400 mg bid for children)
for 5–20 days in conjunction with glucocorticoids.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
5
CUTANEOUS LARVA MIGRANS
This disease is caused by larvae of animal hookworms, usually the dog and cat
hookworm Ancylostoma braziliense. Larvae in contaminated soil penetrate human
skin; erythematous lesions form along the tracks of their migration and advance
several centimeters each day. Pruritus is intense. Vesicles or bullae may form.
Ivermectin (a single dose of 200 g/kg) or albendazole (200 mg bid for 3 days) can
relieve the symptoms of this self-limited infestation.
Intestinal Nematode Infections
Intestinal nematodes infect >1 billion persons worldwide in regions with poor
sanitation, particularly in developing countries in the tropics or subtropics. These
parasites contribute to malnutrition and diminished work capacity.
ASCARIASIS
Etiology:
Ascariasis is caused by Ascaris lumbricoides, the largest intestinal nematode,
which reaches lengths up to 40 cm. The parasite is transmitted via fecally
contaminated soil.
Life Cycle:
Swallowed eggs hatch in the intestine, larvae invade the mucosa, migrate to
the lungs, break into the alveoli, ascend the bronchial tree, are swallowed, reach
the small intestine, mature, and produce up to 240,000 eggs per day that pass in
the feces.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
6
Clinical Features:
Most infections have a low worm burden and are asymptomatic. During lung
migration of the parasite, patients may develop a cough and substernal discomfort,
occasionally with dyspnea or blood-tinged sputum, fever, and eosinophilia.
Eosinophilic pneumonitis (Lo¨ffler’s syndrome) may be evident. Heavy infections
occasionally cause pain, small-bowel obstruction, perforation, volvulus, biliary
obstruction and colic, or pancreatitis.
Laboratory Findings:
Ascaris eggs (65 by 45 µm) can be found in fecal samples. Adult worms can
pass in the stool or through the mouth or nose. During the transpulmonary
migratory phase, larvae can be found in sputum or gastric aspirates.
Treatment:
A single dose of albendazole (400 mg) or mebendazole (500 mg) is effective.
Pyrantel pamoate (a single dose of11 mg/kg, up to 1 g) is safe in pregnancy.
HOOKWORM
Etiology:
One-fourth of the world’s population is infected with one of two hookworm
species: Ancylostoma duodenale or Necator americanus.
Life Cycle:
Infectious larvae penetrate the skin, reach the lungs via the bloodstream,
invade the alveoli, ascend the airways, are swallowed, reach the small intestine,
mature into adult worms, attach to the mucosa, and suck blood and interstitial
fluid.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
7
Clinical Features:
Most infections are asymptomatic. Chronic infection causes iron deficiency
and—in marginally nourished persons—progressive anemia and hypoproteinemia,
weakness, shortness of breath, and skin depigmentation.
Laboratory Findings:
Hookworm eggs (40 by 60 µm) can be found in the feces. Stool concentration
may be needed for the diagnosis of light infections.
Treatment:
Albendazole (400 mg once), mebendazole (500 mg once), or pyrantel
pamoate (11 mg/kg daily for 3 days) is effective. Nutritional support and iron
replacement are undertaken as needed.
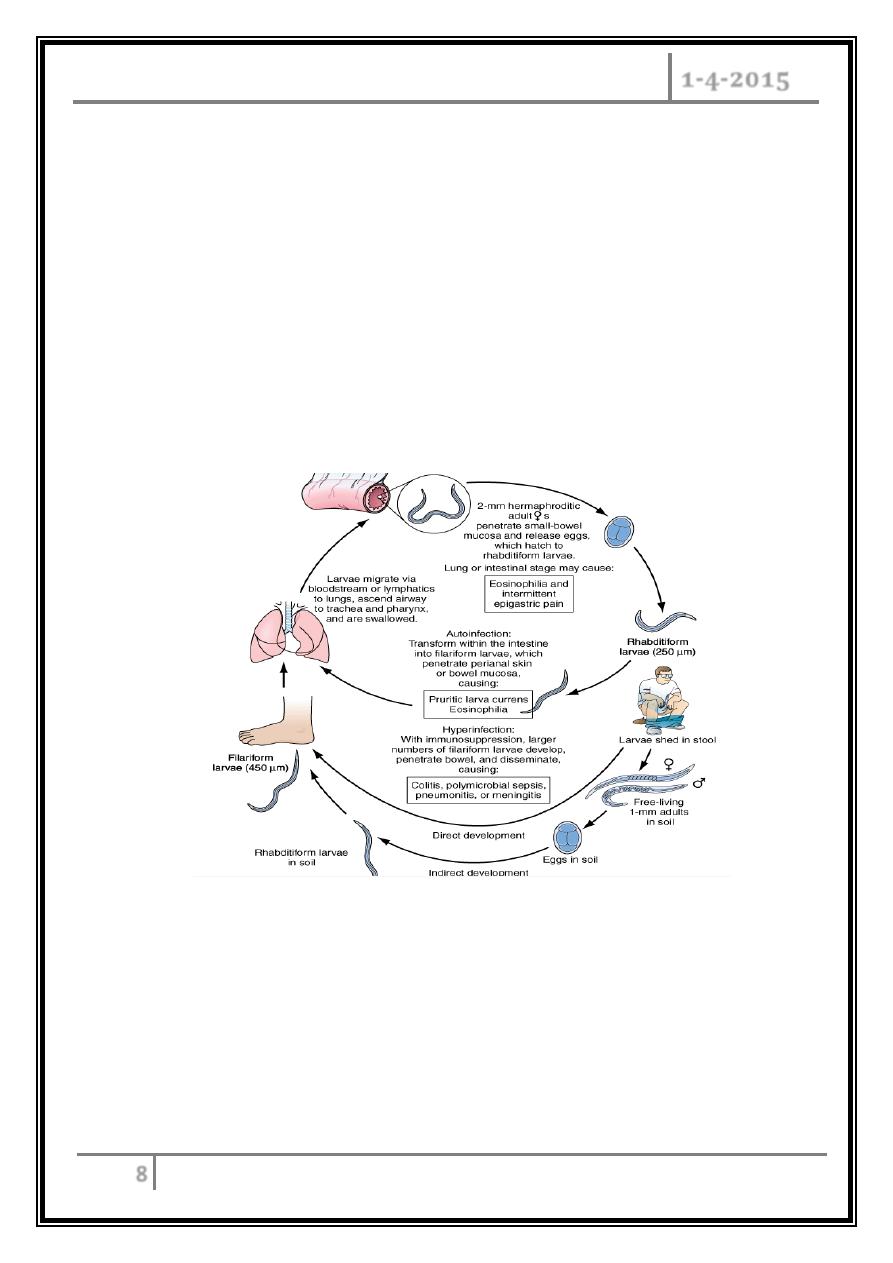
STRONGYLOIDIASIS
Etiology and Epidemiology:
Unlike other helminthes, Strongyloides stercoralis can replicate in the human
host, permitting ongoing cycles of autoinfection from endogenously produced
larvae. Autoinfection is most common among immunocompromised hosts,
including those receiving glucocorticoids. Hyperinfection and widespread larval
dissemination can occur in these patients. However, severe disease due to
Strongyloides is unusual in HIV-infected patients.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
8
Life Cycle:
Infection results when filariform larvae in fecally contaminated soil penetrate
the skin or mucous membranes. Larvae travel through the bloodstream to the
lungs, break through alveolar spaces, ascend the bronchial tree, are swallowed,
reach the small intestine, mature into adult worms, and penetrate the mucosa of
the proximal small bowel; eggs hatch in intestinal mucosa.
Rhabditiform larvae can pass with the feces into the soil or can develop into
filariform larvae that penetrate the colonic wall or perianal skin and enter the
circulation to establish ongoing autoinfection.
Clinical Features:
Uncomplicated disease is associated with mild cutaneous and/or abdominal
manifestations such as urticaria, larva currens (a pathognomonic, pruritic,
erythematous eruption along the course of larval migration that may advance up to
10 cm/h), abdominal pain, nausea, diarrhea, bleeding, and weight loss. Colitis,
enteritis, or malabsorption can develop.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
9
Diagnosis:
Eosinophilia is common, with levels that fluctuate over time. Eggs are rarely
found in feces because they hatch in the colon. A single stool examination detects
rhabditiform larvae (200–250 µm long) in about one-third ofuncomplicated
infections. If stool examinations are negative, duodenojejunal contents can be
sampled. Antibodies can be detected by ELISA. In disseminated infection, filariform
larvae (550 µm long) can be found in stool or at sites of larval migration.
Treatment:
Ivermectin (200 µg/kg daily for 1 or 2 days) is more effective than albendazole
(400 mg daily for 3 days, repeated at 2 weeks) and is better tolerated than
thiabendazole (25 mg/kg bid for 2 days). Disseminated disease should be treated
for 5–7 days.
ENTEROBIASIS
Etiology:
Enterobiasis (pinworm) is caused by Enterobius vermicularis.
Life Cycle:
Adult worms dwell in the bowel lumen and migrate nocturnally out into the
perianal region, releasing immature eggs that become infective within hours.
Autoinfection results from perianal scratching and transport of infective eggs to the
mouth. Person-to-person spread occurs. Pinworm is common among schoolchildren
and their household contacts and among institutionalized populations.
Clinical Features:
Perianal pruritus is the cardinal symptom and is often worst at night.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
10
Diagnosis:
Eggs in the perianal region are detected by application of cellulose acetate
tape in the morning. Eggs measure 55 by 25 µm and are flattened on one side.
Treatment:
One dose of mebendazole (100 mg), albendazole (400 mg), or pyrantel
pamoate (11 mg/kg; maximum, 1 g) is given, with the same treatment repeated
after 10–14 days. Household members should also be treated.
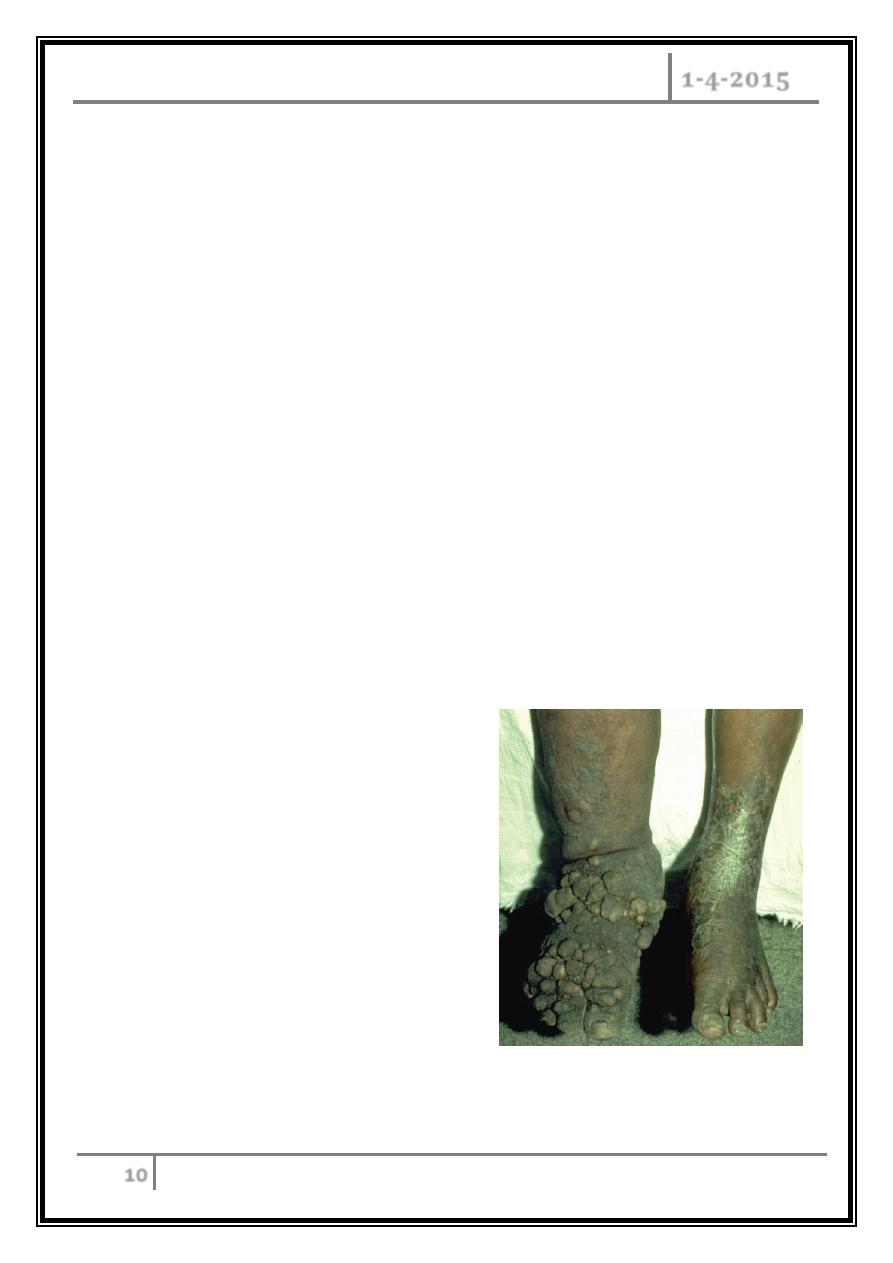
Filarial and Related Infections
Filarial worms are nematodes that dwell in the SC tissue and lymphatics. More than
170 million people are infected worldwide. Infection is established only with
repeated and prolonged exposures to infective larvae. Disease tends to be more
intense and acute in newly exposed individuals than in natives of endemic areas.
Elephantiasis of the lower extremity
associated with Wuchereria
bancrofti infection.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
11
Life Cycle:
Insects transmit infective larvae to humans. Adult worms reside in lymphatics
or SC tissues; their offspring are microfilariae (200–250 µm long, 5–7 µm wide) that
either circulate in the blood or migrate through the skin. Subperiodic forms are
those that are present in peripheral blood at all times and peak in the afternoon.
Nocturnally periodic forms are scarce in peripheral blood by day and increase
by night. Adult worms live for years; microfilariae live for 3–36 months.
LYMPHATIC FILARIASIS
Etiology:
Wuchereria bancrofti, Brugia malayi, or B. timori can reside in lymphatic
channels or lymph nodes. W. bancrofti is most common and usually is nocturnally
periodic.
Pathology:
Adult worms cause inflammatory damage to the lymphatics.
Clinical Features:
Asymptomatic microfilaremia, hydrocele, acute adenolymphangitis (ADL), and
chronic lymphatic disease are the main clinical presentations. ADL is associated
with high fever, lymphatic inflammation, and transient local edema. W. bancrofti
particularly affects genital lymphatics. ADL may progress to lymphatic obstruction
and elephantiasis with brawny edema, thickening of the SC tissues, and
hyperkeratosis. Superinfection is a problem.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
12
Diagnosis:
Detection of the parasite is difficult, but microfilariae can be found in
peripheral blood, hydrocele fluid, and occasionally other body fluids. Timing of
blood collection is critical. Two assays are available to detect W. bancrofti
circulating antigens, and a PCR has been developed to detect DNA of both W.
bancrofti and B. malayi in the blood.
High-frequency ultrasound of the scrotum or the female breast can identify
motile adult worms. Patients have eosinophilia and elevated IgE levels. The
presence of antifilarial antibody supports the diagnosis, but cross-reactivity with
other helminthic infections makes interpretation difficult.
TREATMENT:
Diethylcarbamazine (DEC) given at 6 mg/kg daily for 12 days is the standard
regimen, but one dose may be equally efficacious.
An alternative is albendazole (400 mg bid for 21 days).
Prevention:
Mosquito control or personal protective equipment can minimize bites.
Mass annual distribution of albendazole with DEC or ivermectin for
community- based control reduces microfilaremia and interrupts
transmission.
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
13
ONCHOCERCIASIS
Etiology:
Onchocerciasis (“river blindness”) is caused by Onchocerca volvulus, is the
second leading cause of infectious blindness worldwide, and is transmitted by the
bite of an infected blackfly.
The blackfly vector breeds along free-flowing rivers and streams and restricts
its flight to an area within several kilometers of these breeding sites.
Life Cycle:
Larvae develop into adult worms that are found in SC nodules
(onchocercomata). After months or years, microfilariae migrate out of the nodules
and concentrate in the dermis.
Onchocerciasis affects primarily the skin, eyes, and lymph nodes. Microfilariae
cause inflammation and fibrosis. Neovascularization and corneal scarring cause
corneal opacities and blindness.
Clinical Features:
Skin: Pruritus and rash are the most common manifestations.
Onchocercomata: palpable and/or visible, firm and non-tender.
Ocular tissue: Conjunctivitis with photophobia is an early finding. Sclerosing
keratitis, anterior uveitis, iridocyclitis, and secondary glaucoma due to
anterior uveal tract deformity are complications.
Lymphadenopathy: especially in the inguinal and femoral areas
NEMATODES Dr. Abdulla Al-Farttoosi
1-4-2015
14
Diagnosis:
A definitive diagnosis is based on the finding of an adult worm in an excised
nodule or of microfilariae in a skin snip. Eosinophilia and elevated serum IgE levels
are common. Assays to detect specific antibodies and PCR to detect onchocercal
DNA in skin snips are available in some laboratories.
Treatment:
Nodules on the head should be excised to avoid ocular infection. Ivermectin in
a single dose of150 µg/kg given yearly or semiannually is the mainstay of
treatment.
Doxycycline therapy for 6 weeks may render adult female worms sterile for
long periods and also may target the Wolbachia endosymbiont.
... The end …
