Dr. Alaa Al-Deen
Lec. 4
Giardiasis, Ricketssia,
and Botulism
Wed 8/ 4 / 2015
2014 – 2015
ﻣﻜﺘﺐ ﺍﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
1
GIARDIASIS
Morphologically distinct cyst, which is the stage of the parasite usually found in
the feces.
But it is the resistant cyst that survives outside the body and is responsible for
transmission.
Cysts do not tolerate heating, but do remain viable for months in cold fresh
water.
Ingestion of as few as 10 cysts is sufficient to cause infection in humans.
Person-to-person transmission occurs where fecal hygiene is poor.
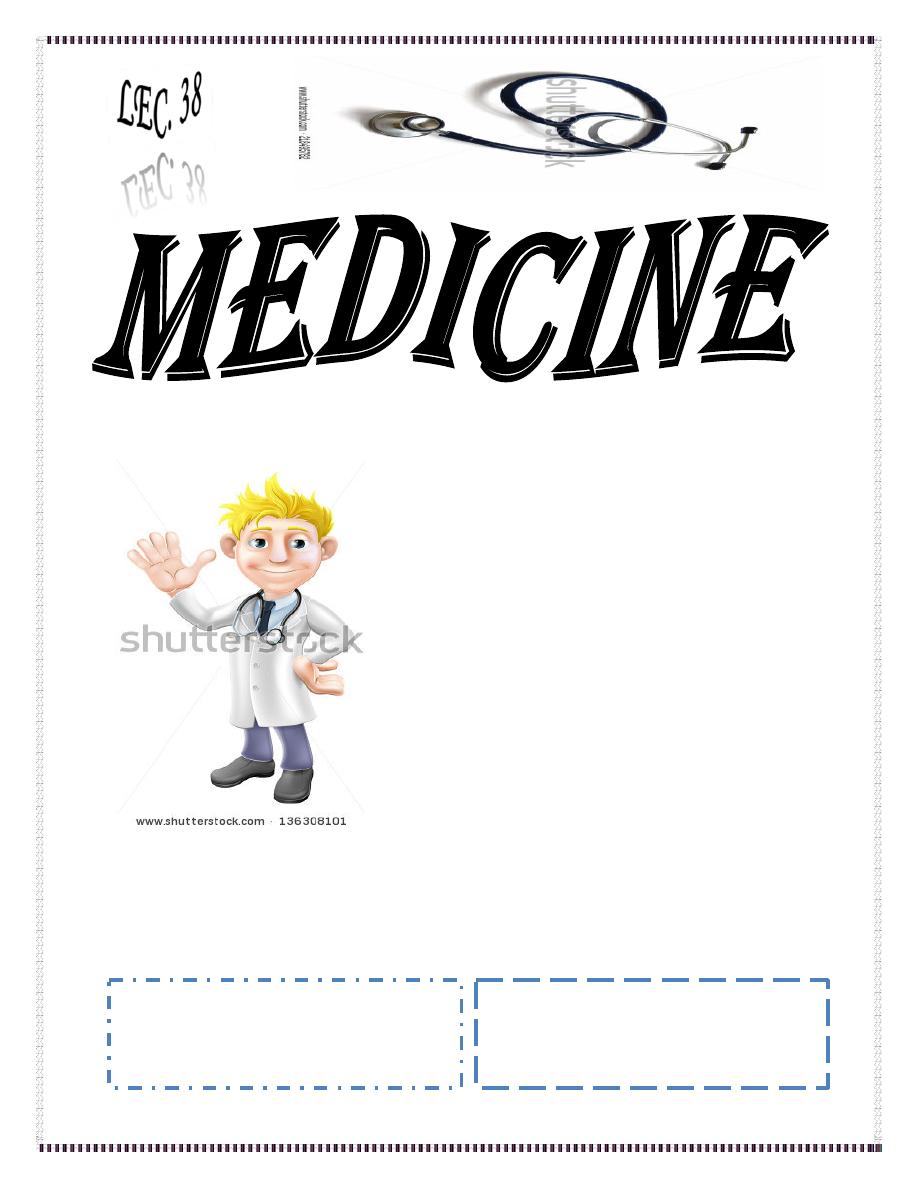
Life Cycle
Cysts are responsible for
transmission.
Cysts and trophozoites are
found in feces.
Ingested by host.
Importance of animal
reservoirs is unclear.
If food is contaminated with Giardia cysts after cooking or preparation, food-
borne transmission can occur.
Water-borne transmission accounts for episodic infections (e.g., in campers
and other travelers) and for massive epidemics in metropolitan areas.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
2
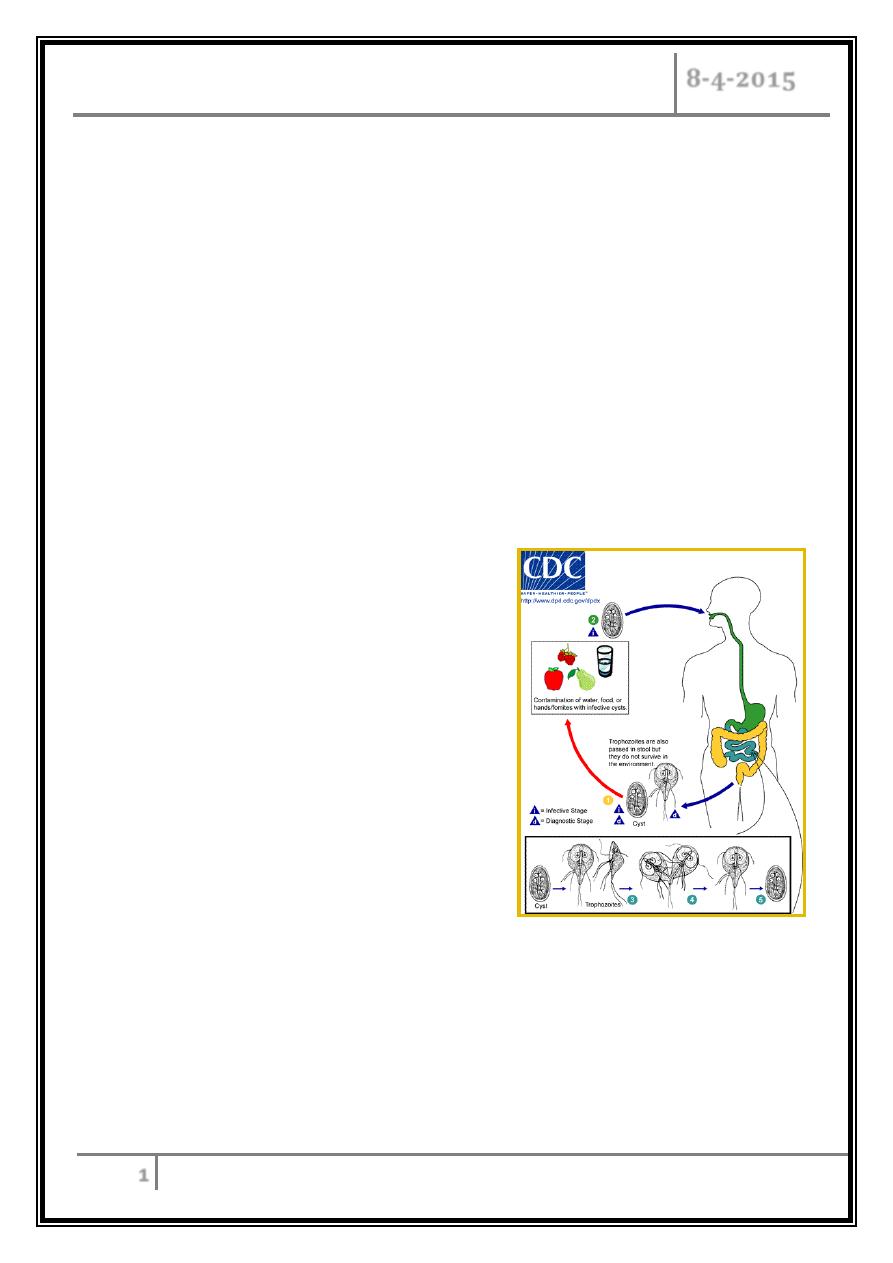
Cyst of Giardia duodenalis
Giardia duodenalis Trophozoite
Light microscope photos of trophozoites
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
3
Pathophysiology
Although trophozoites adhere to the epithelium, they do not cause invasive or
locally destructive alterations.
The lactose intolerance and significant malabsorption that develop in a minority
of infected adults and children are clinical signs of the loss of brush border
enzyme activities.
In most infections the morphology of the bowel is unaltered, but in a few cases—
usually in chronically infected, symptomatic patients—the histopathologic
findings (including flattened villi) and the clinical manifestations resemble those
of tropical sprue and gluten-sensitive enteropathy.
The natural history of Giardia infection varies markedly. Infections may be
aborted, transient, recurrent, or chronic. Parasite as well as host factors may be
important in determining the course of infection and disease.
Both cellular and humoral responses develop in human infections, but their
precise roles in the control of infection and/or disease are
unknown.
Because patients with hypogammaglobulinemia commonly suffer from
prolonged, severe infections that are poorly responsive to treatment, humoral
immune responses appear to be important.
Clinical Manifestations
Disease manifestations of giardiasis range from asymptomatic carriage to
fulminant diarrhea and malabsorption.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
4
Most infected persons are asymptomatic.
Symptoms my develop suddenly or gradually.
In persons with acute giardiasis, symptoms develop after an incubation period
that lasts at least 5 to 6 days and usually 1 to 3 weeks.
Prominent early symptoms include:
- Diarrhea
- Abdominal pain
- Bloating, belching, flatus
- Nausea and vomiting.
- Although diarrhea is common, upper intestinal manifestations such as
nausea, vomiting, bloating, and abdominal pain may predominate.
Individuals with chronic giardiasis may present with or without having
experienced an antecedent acute symptomatic episode.
Diarrhea is not necessarily prominent, but increased flatus, loose stools, and (in
some instances) weight loss occurs.
Symptoms may be continual or episodic and can persist for years.
Fever, the presence of blood and/or mucus in the stools, and other signs and
symptoms of colitis are uncommon and suggest a different diagnosis or a
concomitant illness.
Symptoms tend to be intermittent yet recurring and gradually debilitating, in
contrast with the acute disabling symptoms associated with many enteric
bacterial infections.
Because of the less severe illness and the propensity for chronic infections,
patients may seek medical advice late in the course of the illness; however,
disease can be severe, resulting in malabsorption, weight loss, growth
retardation, dehydration, and (in rare cases) death.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
5
Giardiasis can be life-threatening in patients with hypogammaglobulinemia and is
typically difficult to treat and eradicate.
Although Giardia can cause enteric illness in patients with AIDS, neither the
course of infection nor the response to treatment differs for patients with and
without AIDS.
Diagnosis
Giardiasis is diagnosed by the detection of parasite antigen in the feces or by the
identification of cysts in the feces or of trophozoites in the feces or small
intestines. The diagnosis is sometimes difficult to establish.
Direct examination of fresh or properly preserved stools as well as concentration
methods should be used.
Because cyst excretion is variable and may be undetectable at times, repeated
examination of stool, sampling of duodenal fluid, and biopsy of the small intestine
may be required to detect the parasite.
Tests for parasitic antigen in stool are at least as sensitive and specific as good
microscopic examinations and are easier to perform.
All of these methods occasionally yield false-negative results.
Treatment
o
Cure rates with metronidazole (400 mg thrice daily for 10 days).
o
Tinidazole, 2gm single dose.
o
Furazolidone is used principally for children.
o
Nitazoxanide is recently approved for the treatment of giardiasis in children.
o
Paromomycin, an oral aminoglycoside that is not well absorbed, can be given to
symptomatic pregnant patients.
o
Patients in whom initial treatment fails can be re-treated with a longer course.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
6
o
Almost all patients respond to therapy and are cured, although some with chronic
giardiasis experience delayed resolution of symptoms after eradication of Giardia.
o
Those who remain infected after repeated treatments should be evaluated for
re-infection through family members, close personal contacts, environmental
sources, hypogammaglobulinemia.
o
In cases refractory to multiple treatment courses, prolonged therapy with
metronidazole (750 mg thrice daily for 21 days), alone or in combination with
quinacrine, has been successful.
o
When children attending day-care centers infect an entire family, treatment of all
infected family members, including asymptomatic carriers, may be required to
prevent re-infection.
Prevention
Although Giardia is extremely infectious, disease can be prevented by the
exclusive consumption of non-contaminated food and water.
Cooking food adequately, boiling or filtering potentially contaminated water
prevent infection
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
7
RICKETTSIAL DISEASES
All rickettsial disease are transmitted by insect vector except Q fever which
transmitted through respiratory spread.
Occur throughout world and named for the geographic region.
Pathophysiology of all rickettsia includes vasculitis and DIC.
All are associated with rash except Q fever.
All are characterized by fever, headache, myalgia, maculopapular or vesicular
rash.
The clinical characteristic is the presence of eschar that occur at the site of the
tick bite.
They are self-limited, but treatment is recommended.
Rickettsiae are obligate intracellular organisms appearing as gram-negative
coccobacilli and short bacilli.
Patient present acutely with headache, rash and sometime neurological feature.
These organisms have mammalian reservoirs.
Transmitted by contact or exposure to lice, fleas or ticks.
Infection through skin from excreta of arthropods or saliva of some biting infected
vectors.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
8
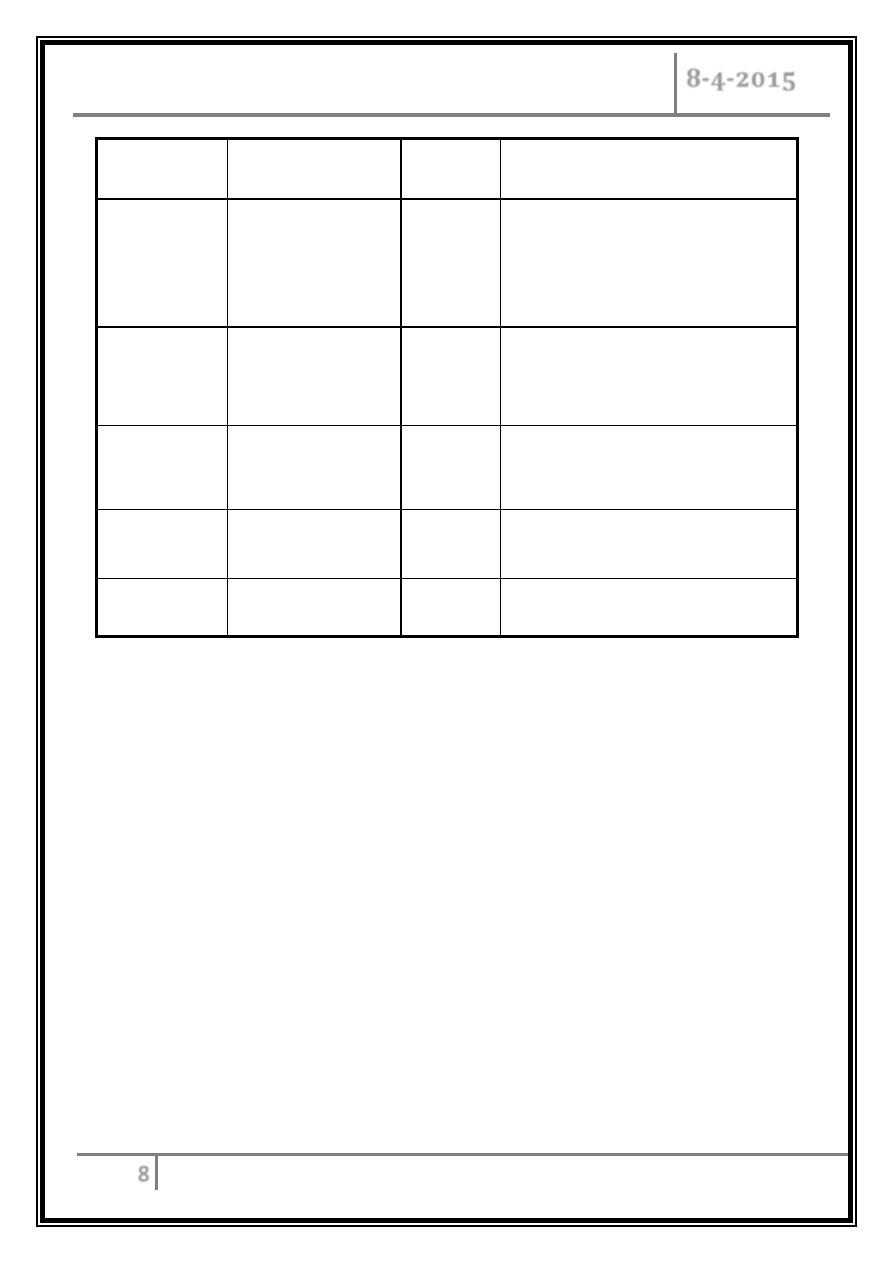
Disease
Organism
Vector
Reservoir
Rocky
Mountain
spotted
fever
R. Rickettsii
Tick
Tick, wild rodents
Scrub
typhus
R. Tsutsugamushi Laval
Mite
(chiggers)
Mites, wild rodents
Epidemic
typhus
R. Prowazekii
Louse
Humans, squirrel fleas, flying
squirrels
Murine
typhus
R. Tiphi
Flea
Wild rodents
Q fever
Coxiella Burnetii
None
Cattle, sheep, goats, cats
Endemic Murine Typhus (Flea-Borne)
Caused by R. typhi.
It has a rat reservoir.
It is transmitted by fleas.
Humans become infected when rickettsia laden flea feces are scratched into
pruritic bite lesions; less often, the flea bite itself transmits the organisms.
Flea bites are not often recalled by pts, but exposure to animals such as cats,
opossums, raccoons, skunks, and rats is reported by 40%.
Symptoms resemble of mild louse born typhus.
Rash scanty and transient.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
9
Clinical Features
Prodromal symptoms 1–3 days before the abrupt onset of chills and fever
include headache, myalgia, arthralgia, nausea, and malaise.
Rash is apparent at presentation (usually _4 days after symptom onset)
maculo-papular rash that involves the trunk more than the extremities,
Is seldom petechial, and rarely involves the face, palms, or soles.
Pulmonary disease is common, causing a hacking, nonproductive cough.
Almost one-fourth of pts who undergo CXR have pulmonary densities due to
interstitial pneumonia, pulmonary edema, and pleural effusions/
Abdominal pain
Confusion, stupor, seizures, ataxia, coma.
Jaundice occurs less commonly.
Diagnosis
As with other rickettsial diseases, a reliable diagnostic laboratory test in the
early phase of illness is not available.
Thus, the diagnosis is usually based upon the typical clinical findings
developing in an appropriate epidemiologic setting.
The exposure history may not be helpful, since most patients do not
remember a flea bite or contact with rodents.
Anemia, leukocytosis, thrombocytopenia.
Hyponatremia.
Increased hepatic aminotransferase levels.
Prerenal azotemia.
The diagnosis can be based on immunofluorescence assay that detects a
fourfold serum antibody increase to a titer 1:64 or a single titer 1:128.
Skin biopsy.
PCR amplification of R. typhi from blood.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
10
The Differential Diagnosis
The classic viral exanthems, such as rubella and measles, as well as numerous
other viral infections (e.g. mononucleosis, Coxsackievirus , Echo virus).
Drug reactions.
Other rickettsial diseases, such as RMSF and epidemic typhus.
Treatment
Doxycycline (100 mg bid for 7–15 days) or chloramphenicol (500 mg qid for 7-
15 days) is effective.
Epidemic Typhus (Louse-Borne)
o Caused by R. prowazekii.
o Transmitted by the human body louse.
o The louse lives on clothes and is found in poor hygienic conditions, particularly
in colder climates and classically at times of war or natural disaster.
o Human here is the reservoir
o Vector: louse (pediculus).
o Incubation peroid 10-14 days.
o Fever, headache, and general pains followed by a rash that spreads from trunk
to the entire body appear on day 4-7, except palms, face and soles.
o Conjunctiva suffusion, splenomegaly, cerebral obtundation are common.
o Can be complicated by encephalitis and myocarditis.
o Fever resolve after 2 weeks.
o Diagnosis by identification of rickettsia in smear or culture of skin lesion.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
11
Q FEVER
Coxiella burnetii. a small gram-negative organism, causes Q fever.
The organism can exist as a highly infectious.
It is an intracellular organism, but it can be extracellular by forming spores that
allow its survival in harsh environments for prolonged periods.
Q fever is a zoonosis
It is worldwide.
The primary sources of human infection are infected cattle, sheep, and goats,
but cats, rabbits, pigeons, and dogs can transmit disease as well.
C. burnetii localizes to the uterus and mammary glands of infected female
mammals.
It is reactivated in pregnancy and is found at high concentrations in the
placenta.
At parturition, the organismis dispersed as an aerosol, and infection usually
follows inhalation.
Abattoir workers, veterinarians, and others persons who have contact with
infected animals are at risk.
Exposure to newborn animals or infected products of conception poses the
highest risk.
C. burnetii is shed in the milk for weeks to months after parturition
Ingestion of contaminated milk is believed to be an important route of
transmission in some areas, although the evidence is contradictory.
Clinical Features
Acute Q fever: The incubation period ranges from 3 to 30 days.
Symptoms are often nonspecific (e.g., fever, fatigue, headache, chills, sweats,
nausea, vomiting, diarrhea, and cough).
Rash developed in 20% and it is not characteristic.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
12
Pneumonia: most cases are mild, with a non-productive cough, fever, and
minimal auscultatory abnormalities; however, some patients present with
acute respiratory distress.
Pleural effusion, multiple rounded opacities on CXR are common and are
highly suggestive of Q fever pneumonia.
Hepatitis can occur and may be with granulama formation.
The WBC count is usually normal.
Thrombocytopenia.
During recovery, reactive thrombocytosis can develop and cause deep vein
thrombosis.
Chronic Q fever: This uncommon entity almost always implies endocarditis,
occurring in pts with prior valvulvar heart disease, immunosuppression, or
chronic renal failure.
Vegetations are seen in only 12% of cases and manifest as nodules on the
valve.
Osteomyelitis.
Encephalitis.
Hepatomegaly and/or splenomegaly in combination with a positive
rheumatoid factor high ESR, high C-reactive protein level, and/or increased
globulin concentration, suggests the diagnosis.
Although C. burnetii can be isolated by a shell-vial technique, most
laboratories are not permitted to attempt isolation because of its highly
contagious nature.
PCR testing of tissue or biopsy specimens can be used.
But serology is the most common diagnostic tool.
IFA is the method of choice, but complement fixation and ELISA are also used.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
13
Treatment
Acute Q fever is treated with doxycycline (100 mg bid for 14 days).
Quinolones are also efficacious.
Treatment for chronic Q fever is problematic and require prolong treatment
should include at least two agents active against C. burnetii.
The combination of rifampin (300 mg once daily) plus doxycycline (100 mg bid)
or ciprofloxacin (750 mg bid) has been used with success.
Botulism
Clostridium botulinum
- Gram positive.
- Obligate anaerobic bacillus.
- Spore-forming.
- Ubiquitous.
- Resistant to heat, light, drying and radiation.
- Specific conditions for germination.
- Anaerobic conditions.
- Warmth (10-50
o
C).
- Mild alkalinity.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
14
History
1793, Justinius Kerner … “Wurstgift” .
“Botulus” = Latin for sausage.
1895, Emile von Ermengem … Isolated organism during Belgium outbreak.
Mechanism of Toxin Action
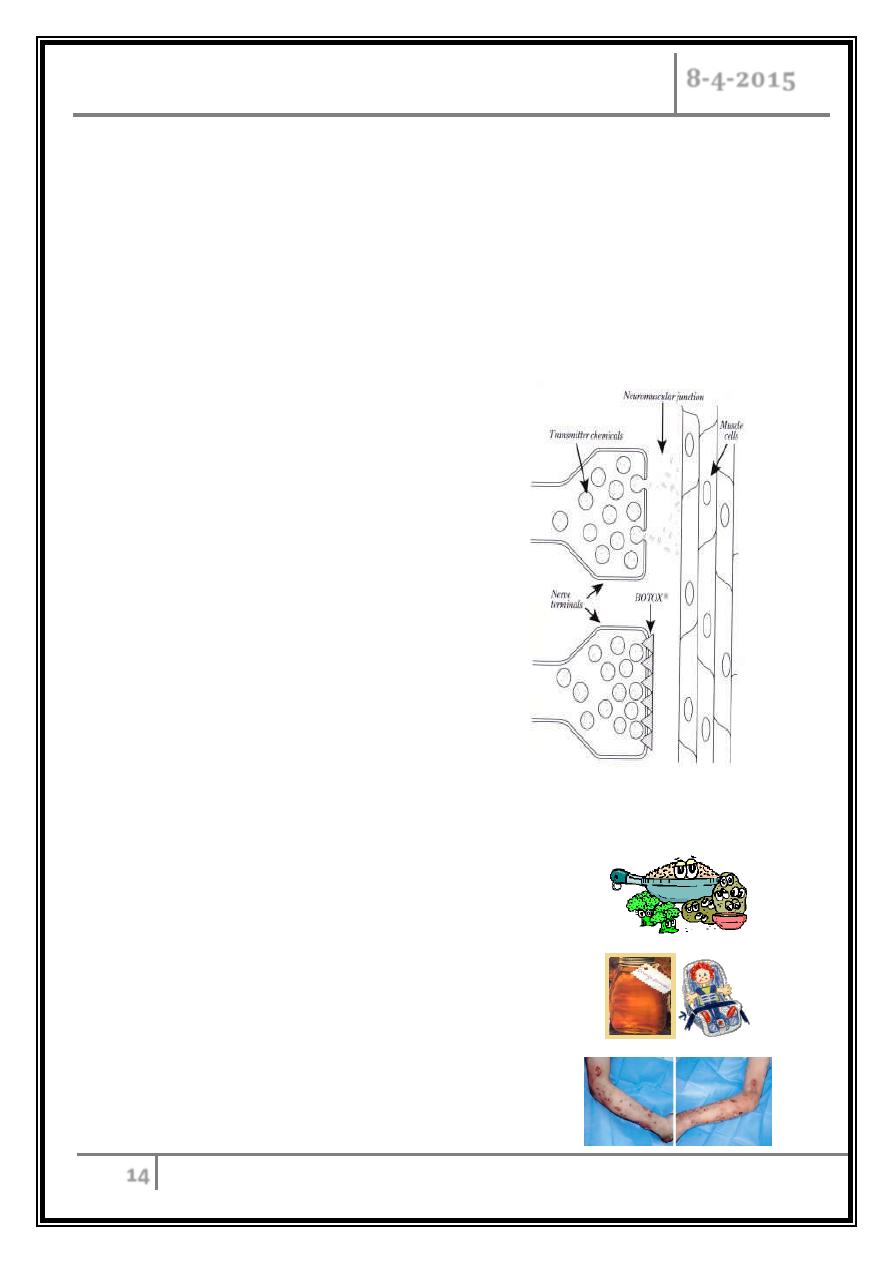
Clostridium botulinum produces a
heat-labile neurotoxin that inhibits
acetylcholine release from cholinergic
terminals at the motor end plate.
Categories of Human Botulism
1. Foodborne botulism.
2. Infant botulism.
3. Wound botulism.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
15
Botulism usually is caused by the ingestion of contaminated food (home-
canned products and improperly prepared or handled commercial foods).
Wound botulism results from contaminated traumatic wounds.
Neonatal botulism can result from consumption of contaminated honey.
Fifty percent of food-borne outbreaks in the US are caused by type A toxins.
The most commonly isolated neurotoxin is type A for canned foods and type E
for improperly fermented fish products.
Adult Clinical Symptomes
Nausea, vomiting, diarrhea.
Cranial nerve involvement, which almost always marks the onset of symptoms,
usually produces:
- Double vision.
- Difficulty speaking or swallowing.
Descending symmetrical flaccid paralysis.
Respiratory muscle paralysis.
Paralytic ileus, severe constipation.
Urinary retention is common.
Typically, they have no fever or it is rare.
Patients are usually alert and oriented.
Ptosis is frequent; the pupillary reflexes may be depressed.
Fixed or dilated pupils are noted in half of patients.
The gag reflex may be suppressed.
Have intact deep tendon reflexes.
Sensory findings are usually absent.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
16
Typical clinical scenario:
A patient presents with unexplained diplopia, fixed, dilated pupils; dry mouth;
and descending flaccid paralysis with normal sensation.
Infant Clinical Signs
Constipation.
Lethargy.
Poor feeding.
Weak cry.
Bulbar palsies.
Failure to thrive.
Children less than 1 year of age with these clinical signs with a progressive
weakness should be suspected of infant botulism. This can lead to impaired
respiration and sometimes death if not treated promptly. The child in this picture is
too weak to hold up its head as noted by the limp appearance of the neck and arms.
It was an infant case of botulism. 72% of natural botulism cases occur in children
under 1 year of age.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
17
Diagnosis
A diagnosis of botulism is clinical and must be considered in patients who are:
o With symmetric descending paralysis.
o Afebrile.
o Mentally intact.
Toxin in serum, stool, gastric aspirate, suspected food. (Feces are usually the
most reliable clinical sample in food-borne or infant botulism).
Culture of stool or gastric aspirate (takes 5-7 days).
Electromyography also diagnostic.
The most widely used and sensitive test for detecting botulism toxin is the
mouse neutralization test. Serum or stool with the suspected botulism
organism is injected into a mouse and observed for clinical signs of the
disease. Results are available in 48 hours.
Differentiated from?
Guillain-Barré syndrome and its variants, especially Miller-Fisher variant
paralysis:
History of antecedent infection.
Paresthesias often ascending.
Early areflexia.
EMG findings.
Myasthenia gravis:
Recurrent paralysis.
EMG findings
Stroke:
Paralysis often asymmetric.
Abnormal CNS image.
GIARDIASIS, RICKETTSIA Dr. Alaa Al-Deen
AND BOTULISM
8-4-2015
18
Lambert-Eaton syndrome:
EMG: increased strength with sustained contraction.
Evidence of lung carcinoma.
CNS infections, especially of the brainstem.
Treatment
Intensive care immediately. (Due to respiratory paralysis, a mechanical ventilator
will be needed if respiratory failure occurs)
Patients should be hospitalized and monitored closely, both clinically and by
spirometry, pulse oximetry, and measurement of arterial blood gases for incipient
respiratory failure.
Intravenous Equine antitoxin should be administered as soon as possible after
specimens are obtained for laboratory analysis.
In food-borne case, purging the gut with cathartics, enemas, and emetics to
remove unabsorbed toxin also may be of value.
Antibiotic therapy does not affect the course of illness.
Botulism immune globulin was approved for use on October 23, 2003 for the
treatment of infant botulism caused by types A and G.
… The End ...
