Dr. Mustafa Nema
Lec. 2
TYPHOID FEVER
Mon
23 / 2 / 2015
Done by : Ali Kareem
2014 – 2015
مكتب اشور لالستنساخ
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
2
TYPHOID FEVER
Objectives
At the end of this lecture, the student should be able to :
Define typhoid fever
State how can the disease being transmitted.
Describe the presenting symptoms
List the diagnostic methods
Determine the treatment plan.
Describe the complications
INTRODUCTION
Salmonellae microorganism constitute a genus of more than 2300 serotypes
that are highly adapted for growth in both humans and animals and that
cause a wide spectrum of disease.
The growth of S. typhi and S. paratyphi A and B is restricted to human hosts,
in whom these organisms cause enteric (typhoid) fever.
Enteric fever is endemic in most developing regions.
In history..
400 BC Athens plaque
1907 Mary Maroon cooker
1948 chloramphenicol
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
3
Bacteriology
Three major Salmonella antigenic determinants:
Somatic O antigen [lipopolysaccharide (LPS) cell-wall components],
Surface Vi antigen
Flagellar H antigen.
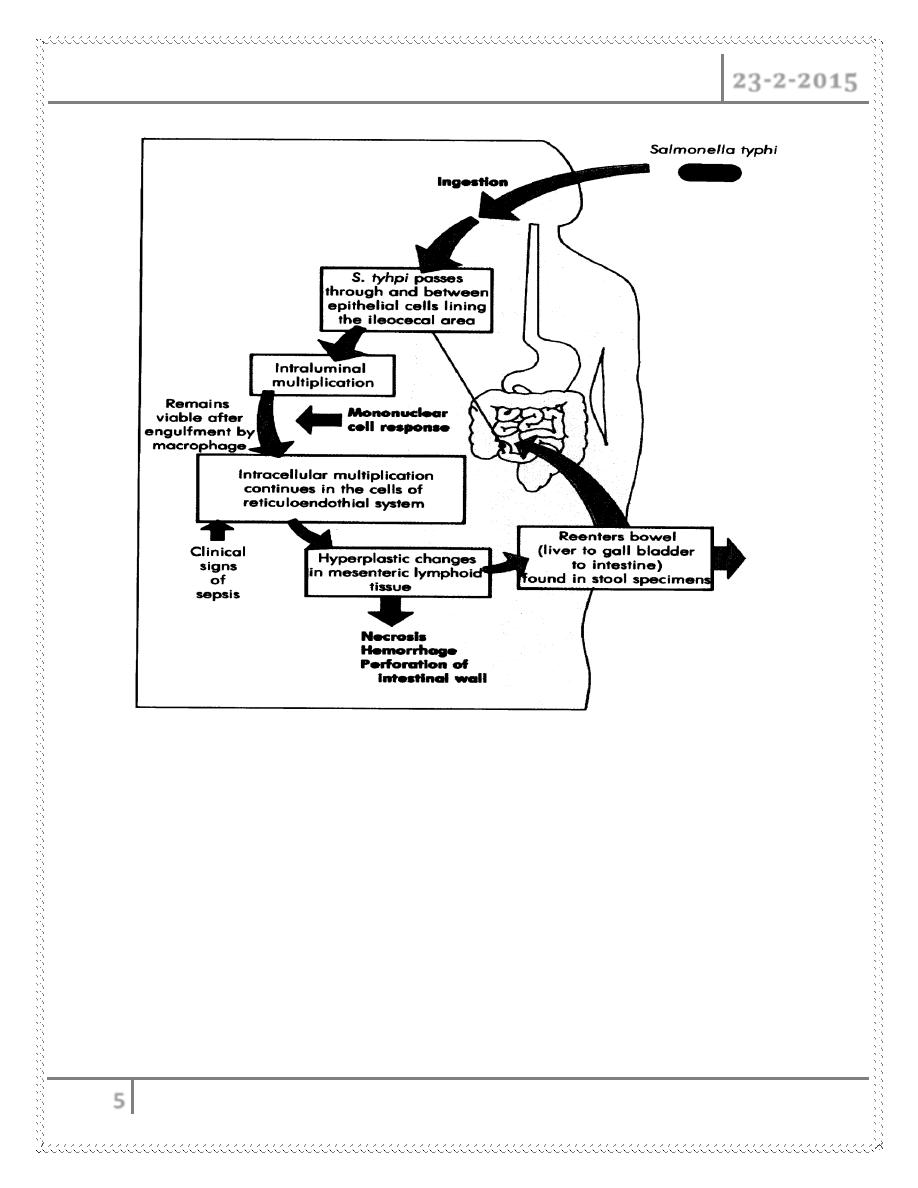
PATHOGENESIS
All Salmonella infections begin with ingestion of organisms in contaminated
food or water.
The infectious dose of Salmonella varies from 103 to 106 colony-forming
units.
Salmonellae resist the low pH of the stomach—a powerful component of
host defense.
The following conditions increase susceptibility to Salmonella infection :
1- Conditions that decrease stomach acidity (e.g. an age of 1year and antacid
ingestion)
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
4
2- Conditions that decrease intestinal integrity (inflammatory bowel disease,
history of gastrointestinal surgery).
3- Alteration of the intestinal flora by antibiotic administration.
Once salmonellae reach the small intestines, the bacteria again encounter
numerous host defenses, including bile salts, lysozyme, complement, and
antimicrobial peptides—all components of the host’s innate immune
response.
The salmonellae next penetrate the mucous layer of the gut.
Two major types of Salmonella infections :
1- Typhoid fever (Enteric fever) caused by S.typhi and S.paratyphi.
2- Non-typhoidal Salmonellosis: when other types of Salmonella
microorganisms cause gastroenteritis.
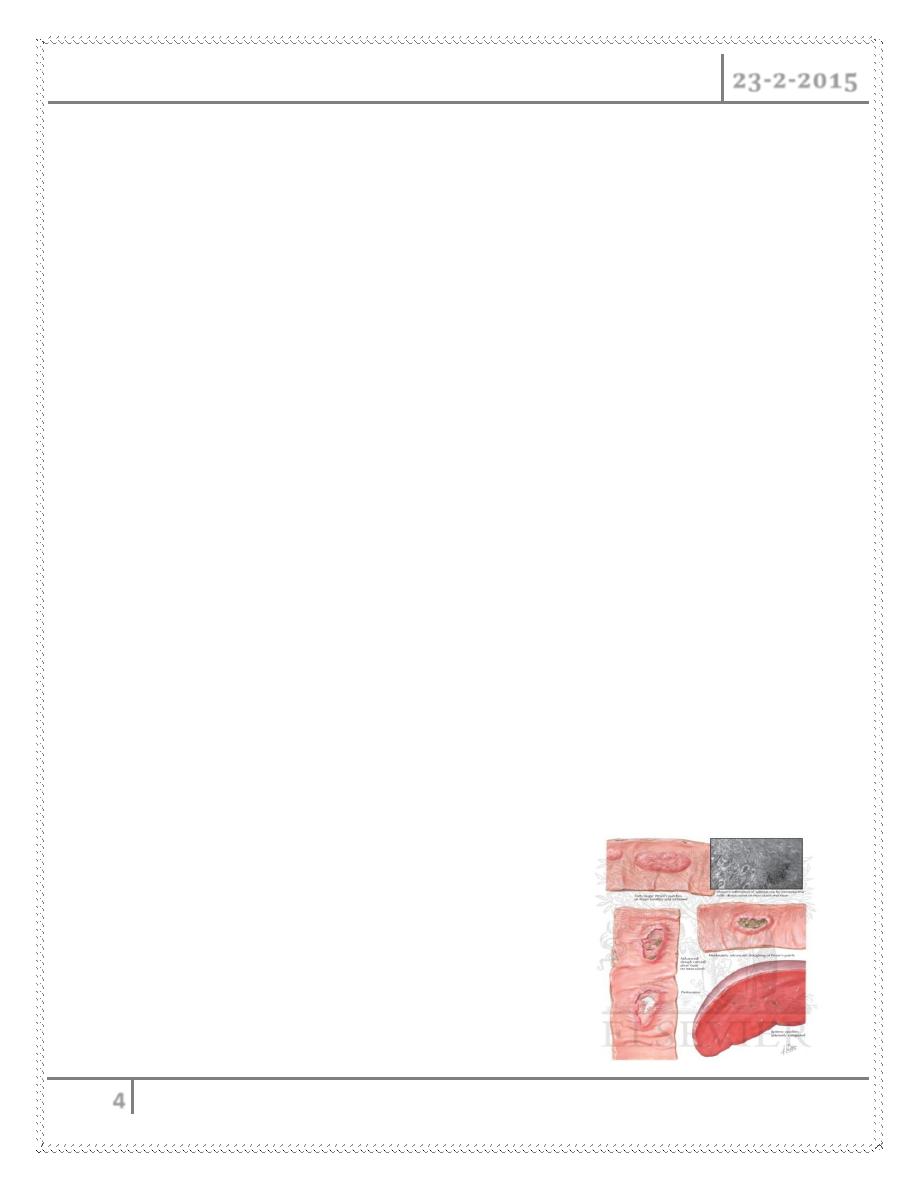
1- Typhoid (Enteric Fever)
After crossing the epithelial layer of the small intestine, S. typhi and S.
paratyphi, which cause enteric (typhoid) fever, are phagocytosed by
macrophages.
Once phagocytosed, salmonellae disseminate throughout the body in
macrophages via the lymphatics and colonize reticuloendothelial tissues
(liver, spleen, lymph nodes, and bone marrow).
The recruitment of additional mononuclear
cells and lymphocytes to Peyer’s patches
can result in marked enlargement and
necrosis of the Peyer’s patches.
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
5
2- Non-typhoidal Salmonellosis
In contrast to enteric fever, which is characterized by an infiltration of
mononuclear cells into the small-bowel mucosa, nontyphoidal Salmonella
gastroenteritis is characterized by massive PMN (polymorphoneuclear
neutrophil) infiltration into both the large- and the small-bowel mucosa.
The degranulation and release of toxic substances by neutrophils may result
in damage to the intestinal mucosa, causing the inflammatory diarrhea
observed with nontyphoidal gastroenteritis.
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
6
TYPHOID (ENTERIC) FEVER
How can typhoid being transmitted?
Close contact with acutely infected individuals or chronic carriers.
The disease result from ingestion of contaminated food or water.
Laboratory workers can acquire the disease after laboratory accidents.
Food handler (especially restaurant workers) and local water/sewage
system disturbances forming an important pathways for infection.
What are the presenting symptoms and signs?
The incubation period for S. typhi ranges from 3 to 21 days. This variability
is most likely related to the size of the initial inoculum and the health and
immune status of the host.
A prodrome of nonspecific symptoms often precedes fever and includes
chills, headache, anorexia, cough, weakness, sore throat, dizziness, and
muscle pains.
1st week
Fever
Rose spots on trunk
Splenomegaly
Cough
Abdominal distension
Diarrhoea
2nd week
Increasing Fever
Headache
Myalgia
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
7
Relative bradycardia
Constipation
Diarrhoea and vomiting in children
End of 2
nd
week
Delirium, complications, then coma and death (if untreated).
The most prominent symptom of this systemic infection is prolonged fever
(38.8 to 40.5C).
Gastrointestinal symptoms are quite variable. Patients can present with
either diarrhea or constipation;
Diarrhea is more common among children 1 year of age.
20 to 40% of patients present with abdominal pain, although the majority
have abdominal tenderness over the course of the disease.
On patient’s examination..
Early physical findings of enteric fever include:
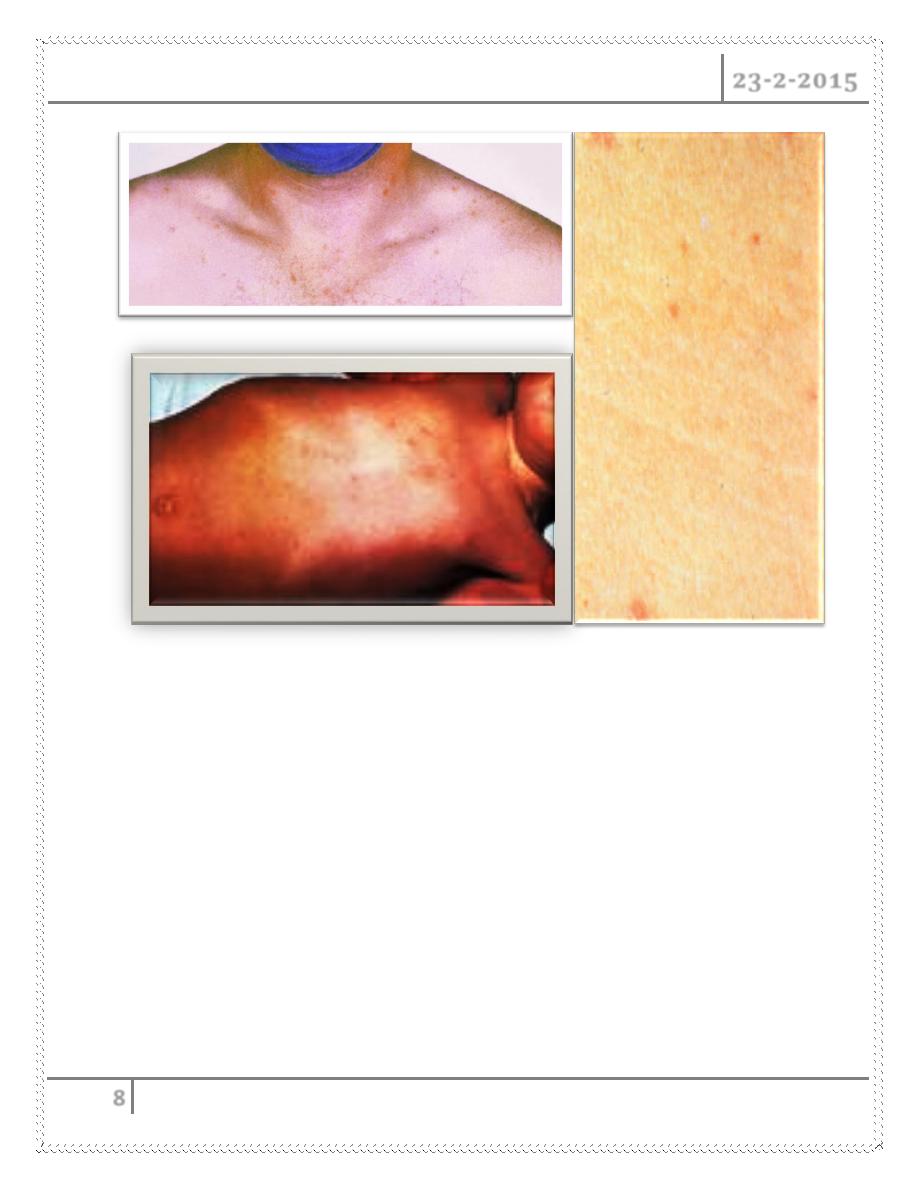
Rash ―rose spots‖
Hepatosplenomegaly
Epistaxis
The pulse is often slower than would be expected from the height of the
temperature, i.e. a relative bradycardia.
Rose spots are make up a faint, salmon-colored, blanching, maculopapular
rash located primarily on the trunk and chest.
The rash is evident in 30% of patients at the end of the first week and
resolves after 2 to 5 days without leaving a trace.
Salmonella can be cultured from punch biopsies of these lesions
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
8
On occasion, patients who remain toxic manifest neuropsychiatric
symptoms (delirium) with picking at bedclothes or imaginary objects.
COMPLICATIONS
Late complications, occurring in the third and fourth weeks of infection,
are most common in untreated adults and include intestinal perforation
and/or gastrointestinal hemorrhage.
These complications can develop despite clinical improvement and
presumably result from necrosis at the Peyer’s patches of the small
intestine.
Both complications are life-threatening and require immediate medical
and surgical interventions, with antibiotic coverage for polymicrobial
peritonitis and treatment of GIT hemorrhages, including bowel resection.
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
9
Rare complications (whose incidences are reduced by prompt antibiotic
treatment) include :
Pancreatitis,
Hepatic and splenic abscesses,
Endocarditis, pericarditis,
Orchitis,
Hepatitis,
Meningitis,
Nephritis,
Myocarditis,
Pneumonia,
Arthritis, osteomyelitis, and
Parotitis.
Paratyphoid
The onset is often more abrupt with acute enteritis.
The course tends to be shorter and
milder than that of typhoid fever
The rash may be more abundant
The intestinal complications less frequent.
DIAGNOSIS
Lab tests
1- Blood Culture :
Other than a positive culture, no specific laboratory test is diagnostic
for enteric fever (S. typhi or S. paratyphi), so it is the “gold standard”
test
A diagnosis can also be based on positive cultures of stool, urine,
rose spots, bone marrow, and gastric or intestinal secretions.
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
10
Unlike blood cultures, bone marrow cultures remain highly (90%)
sensitive despite 5 days of antibiotic therapy.
Culture of intestinal secretions can be positive despite a negative bone
marrow culture.
Stool cultures, while negative in most of cases during the first week,
can become positive during the third week of infection in untreated
patients.
Although the majority of patients clear bacteria from the stool by the
eighth week, a small percentage become chronic carriers and
continue to have positive stool cultures for at least 1 year.
2- Other ancillary tests:
WBC
- In the majority of cases, the white blood cell count is normal
despite high fever
- In 25% of cases, leukopenia and neutropenia are detectable..
- However, leukocytosis can develop in typhoid fever (especially in
children) during the first 10 days of the illness, or later if the
disease course is complicated by intestinal perforation or
secondary infection.
Liver function tests
- Moderately elevated values (aminotransferases, alkaline
phosphatase, and lactate dehydrogenase).
ECG
- Nonspecific ST and T wave abnormalities can be seen on ECG.
Serologic tests
- Several serologic tests, including the classic Widal test for ―febrile
agglutinins,‖ are available; however, given high rates of false-
positivity and false-negativity, these tests are not clinically useful.
Polymerase chain reaction and DNA probe assays are being
developed.
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
11
Differential Diagnosis
Since the clinical presentation of typhoid fever is relatively nondescript, the
diagnosis needs to be considered in any DDx include :
Malaria, hepatitis, bacterial enteritis amebic liver abscesses, and acute HIV
infection
TREATMENT
In the preantibiotic era, the mortality rate from typhoid fever was as high as
15%.
The introduction of treatment with chloramphenicol in 1948 greatly altered
the disease course, decreasing mortality to 1% and the duration of fever
from 14–28 days to 3–5 days.
Chloramphenicol remained the standard treatment for enteric fever, but two
problems emerged with this drug:
- Drug resistance
- The rare chloramphenicol-induced bone marrow toxicity.
Then, other drugs also found to be effective :
Quinolones
Third generation cephalosporins
Azithromycine
Ampicillin, Amoxicillin
Trimethoprim-sulfamethoxazole
Standard regimens
First-line
Ciprofloxacin 500 mg x2, orally for 10 days OR
Ceftriaxone 1–2 g IV or IM for 10–14 days
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
12
Alternative
Azithromycin 1 g Orally daily for 5 days OR
Chloramphenicol 2 to 3 g per day orally in four divided doses for 14 days.
Other drugs:
Ampicillin, Amoxicillin, TMS, Cefotaxime, Cefixime
Ciprofloxacine
Bactericidal and concentrated intracellularly and in the bile.
Result in more rapid defervescence than beta-lactam agents or
chloramphenicol because of more rapid elimination of intracellular
bacteria
Other management
In patients with severe disease (delirium, stupor, coma or shock), use of I.V
steroid will decrease mortality.
Surgery: indicated in cases of intestinal perforation.
Typhoid fever's danger doesn't end when symptoms disappear
Relapse
Relapse of typhoid fever after clinical cure is not uncommon and typically
occurs two to three weeks after resolution of fever.
An additional course of therapy with a drug to which the organism is clearly
sensitive is indicated for relapsing illness.
NB. Use of quinolones may reduce relapse rates.
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
13
Chronic Salmonellae carriers
Defined as excretion of the organism in stool for more than 12 months after
the acute infection.
Occurs in 1-5%.
They appear to have reached an immunologic equilibrium in which they are
chronically colonized, and may excrete large numbers of organisms, but
have high levels of systemic immunity and do not develop clinical disease
However, chronic carriers represent an infectious risk to others, particularly
if involved in food preparation.
For this reason, eradication of carriage is usually attempted once such
individuals are identified.
The incidence of chronic carriage is higher among women and among
persons with biliary abnormalities (e.g. gallstones, carcinoma of the
gallbladder and GIT malignancies), urinary stones (as well as concurrent
infection with Schistosoma haematobium) may assist chronic carrier state.
Ciprofloxacin (500 or 750 mg orally twice daily) for 2-4 weeks eliminated
carrier state.
PREVENTION
Cook it
+
Boil it + Hand Wash → Prenention
+
Peel it
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
14
Vaccine :
Typhoid vaccines — There are two vaccines available for protection against
S. typhi, oral and parenteral.
Neither is completely effective.
#END
Done by
Ali Kareem
Some MCQs
Q1/ The flagellar Ag is the :
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
15
A) Vi Ag
B) H Ag
C) O Ag
D) C Ag
Q2/ Non Typhoid Salmonella cause:
A) Hepatitis
B) Nephritis
C) Gasteroentritis
D) Pharyngitis
Q3/ The most important test for diagnosis of typhoid fever is:
A) Blood culture
B) Widal test
C) WBC count
D) PCR
Q4/ Drugs that lead to rapid fever lysis is :
A) Chloramphenicol
B) Ceftriaxone
C) Azithromucin
D) Ciprpfloxacin
Q5/ The following increase susceptibility to Salmonella infection EXCEPT:
TYPHOID FEVER Dr. Mustafa Nema
23-2-2015
16
A. Decrease stomach acidity
B. Old age
C. History of gastrointestinal surgery.
D. Alteration of the intestinal flora
Q6/ Physical findings of enteric fever include all of the following EXCEPT:
A. Tachcardia
B. Rose spots
C. Hepatosplenomegaly
D. Epistaxis
Q7/ Paratyphoid differ from typhoid by all of the following EXCEPT:
A. The onset is more abrupt
B. Shorter course
C. Frequent intestinal complications
D. More abundant rash
Q8/ The last culture that could remain positive is that taken from:
A. Urine
B. Stool
C. Bone marrow
D. Blood
