Dr. Mustafa Nema
Lec. 3
LEPTOSPIROSIS
Mon
2 / 3 / 2015
Done by : Ibraheem Qais
2014 – 2015
مكتب اشور لالستنساخ
1 |
P a g e
Objectives
At the end of this lecture, the student should be able to:
• Identify the causative agent of leptospirosis.
• Determine the ways of disease transmission.
• Describe how patients with this disease present.
• Clarify management and prevention plan.
Case scenario
• A 29 year’s old male presented to the hospital with fever, headache, marked
muscle and joint pain.
• 3 days later, he deteriorated and developed skin rash, red conjunctivae,
yellowish discoloration of sclera and low urine output. His urine looks dark.
• Then he developed severe dyspnea and his consciousness decreased.
• He works as a farmer, with many animals around.
• How can you approach the diagnosis?
2 |
P a g e
Introduction
Adolf Weil's described in 1886 a disease with fever and jaundice.
Rats as a carrier (reservoir host) were then identified.
Causative agent
• Leptospirosis is one of the most common zoonotic diseases, favoured by a
tropical climate and “flooding”, but occurring worldwide.
• More than 200 subtypes present.
• Leptospira interrogans is pathogenic for humans.
3 |
P a g e
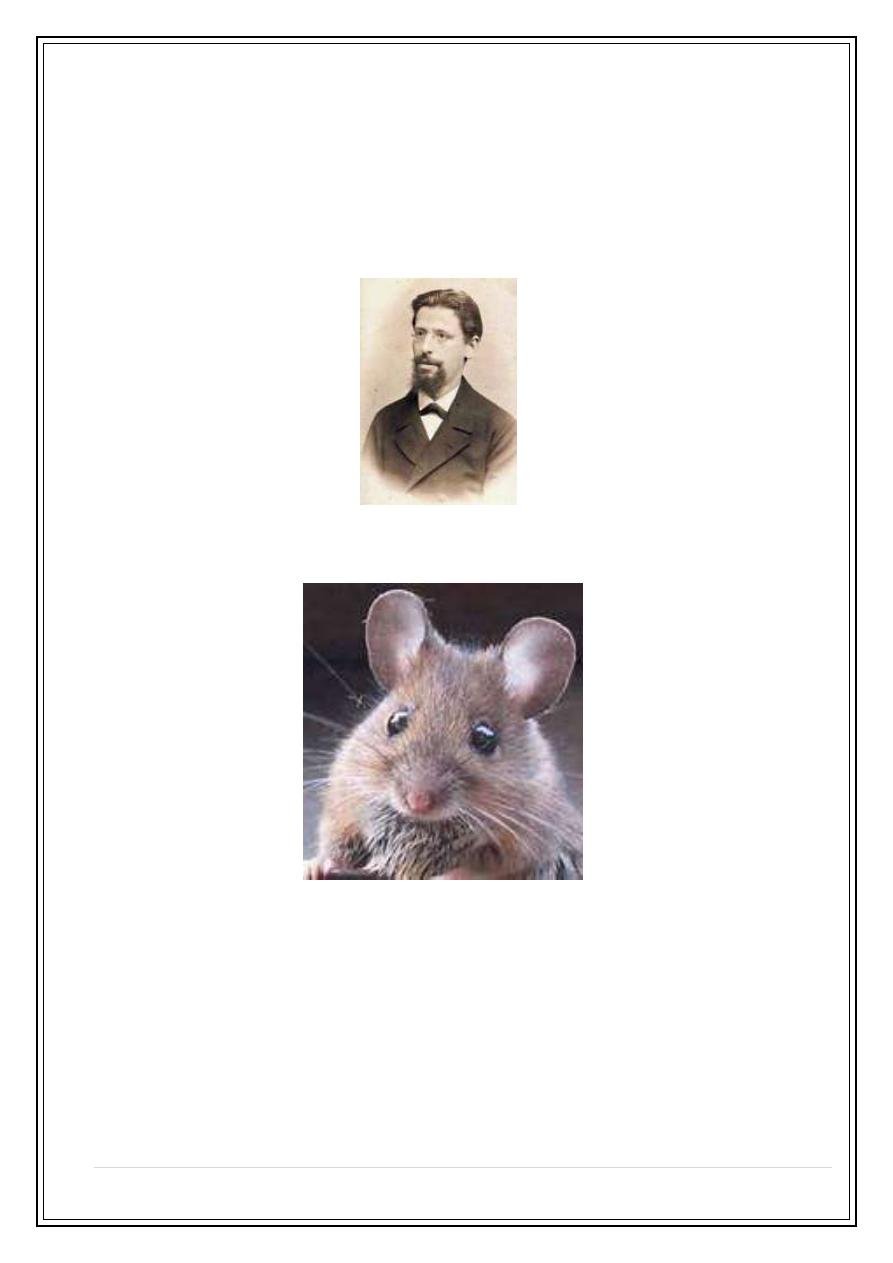
• The etiologic agent is a motile spirochete.
• Leptospirosis present in wildlife and in many domestic animals.
• The organisms persist indefinitely in the convoluted tubules of the kidney of the
animal host and are shed into the urine in massive numbers, but infection is
asymptomatic in the host.
4 |
P a g e
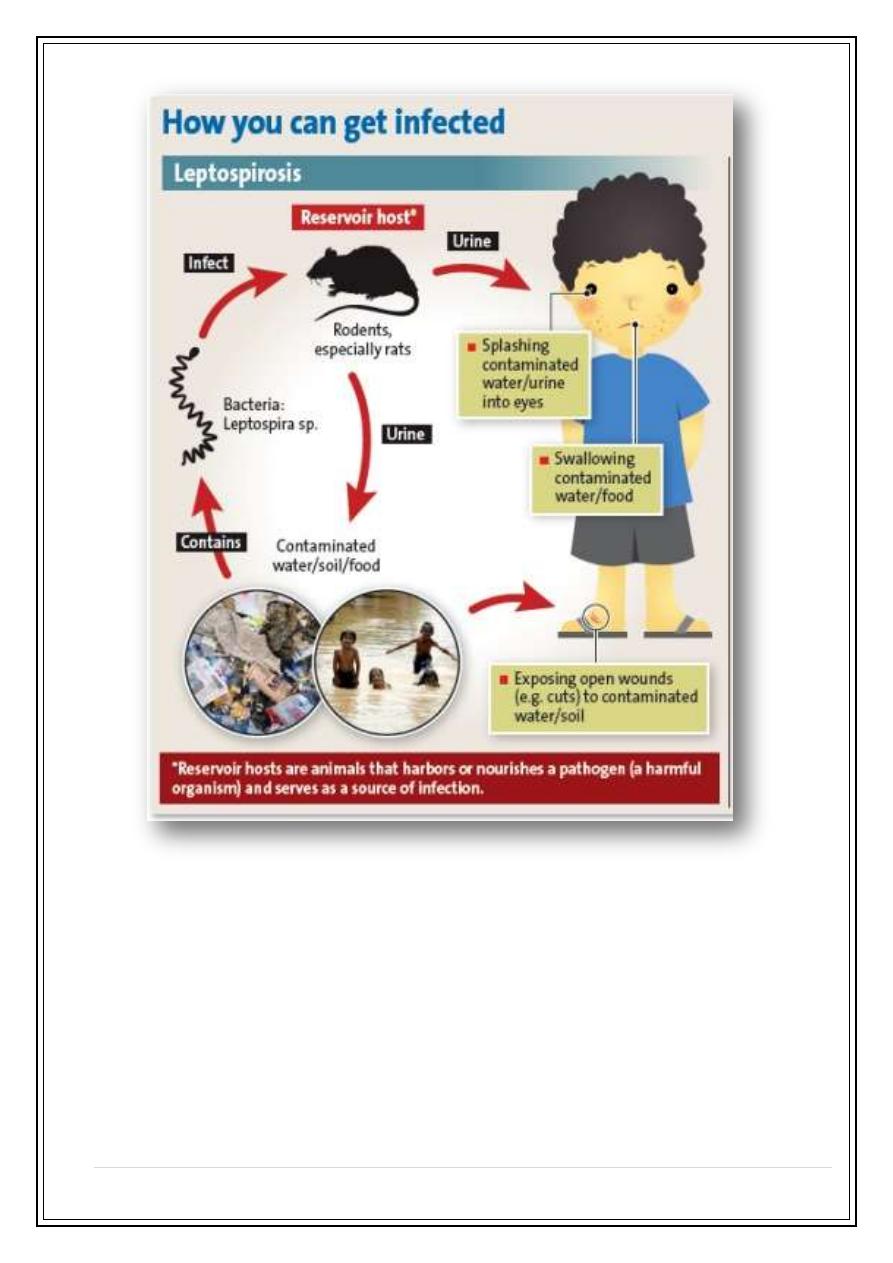
• The bacteria that cause leptospirosis are spread through the urine of infected
animals, which can get into water or soil and can survive there for weeks to
months.
• Many different kinds of wild and domestic animals carry the bacterium.
• The most frequent hosts are rodents, especially the common rat.
• Other animals can include, but are not limited to:
–
Cattle
–
Horses
–
Dogs
–
Wild animals
5 |
P a g e
Who is at risk?
• Farmers
• Mine workers
• Sewer workers
• Slaughterhouse workers
• Veterinarians and animal caretakers
• Fish workers
• Dairy farmers
• Military personnel
What are the ways of transmission?
• Leptospires can enter their human through intact skin or mucous membranes,
but entry is facilitated by cuts and abrasions.
• Prolonged immersion in contaminated water will also favour invasion, as the
spirochete can survive in water for months.
• Drinking contaminated water can also cause infection.
• Outbreaks of leptospirosis are usually caused by exposure to contaminated
water, such as floodwaters.
• Person to person transmission is rare.
6 |
P a g e
7 |
P a g e
How can a patient with leptospirosis presents?
• The incubation period averages 1–2 weeks.
• After a relatively brief bacteraemia, invading organisms are distributed
throughout the body, mainly in kidneys, liver, meninges and brain.
Signs and symptoms
In humans, Leptospirosis can cause a wide range of symptoms, including:
• High fever
• Headache
• Chills
• Muscle aches
• Vomiting
• Jaundice
• Red eyes
• Abdominal Pain
• Diarrhea
• Rash
8 |
P a g e
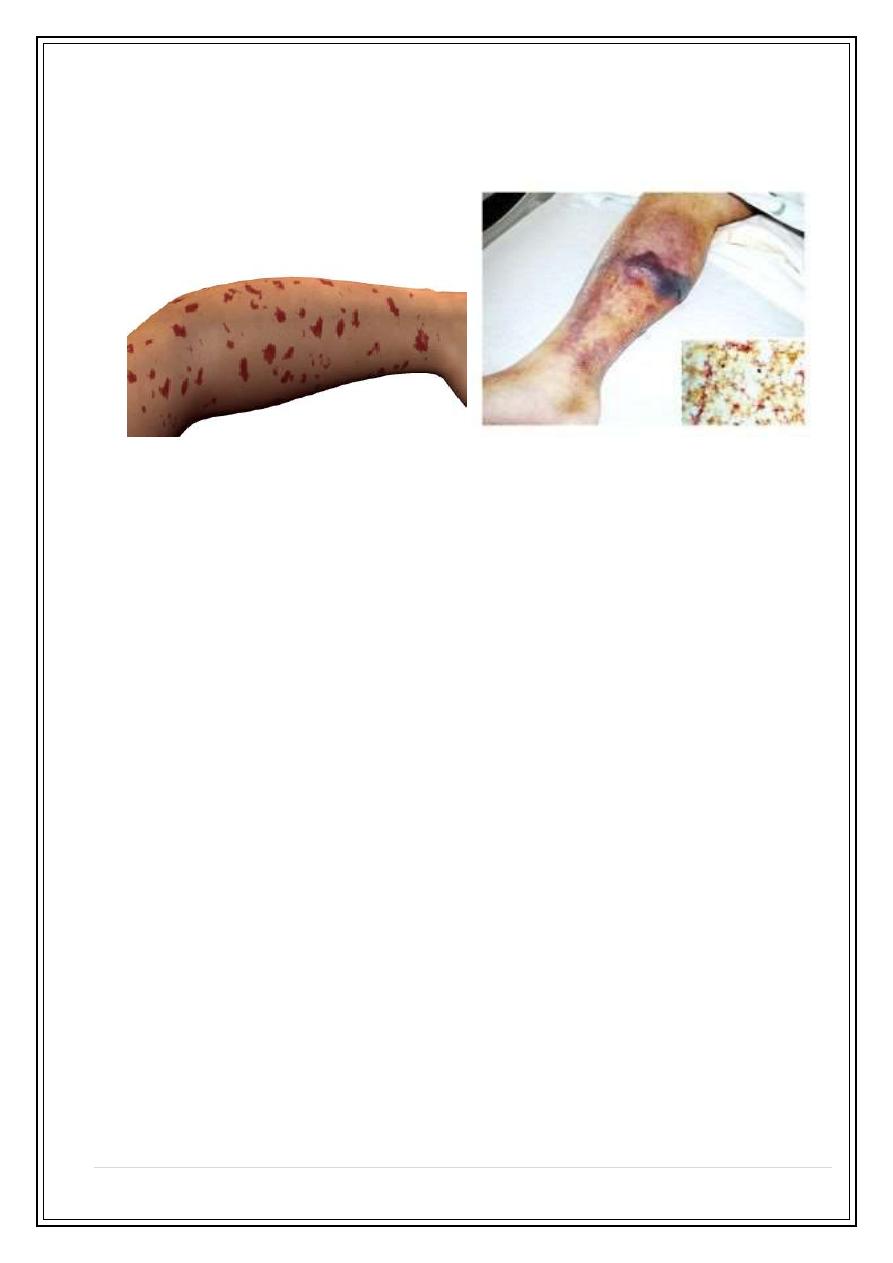
Four main clinical syndromes can be discerned and clinical features can involve
multiple organ systems:
1. Bacteraemic leptospirosis
2. Aseptic meningitis
3. Icteric* leptospirosis (Weil’s disease)
4. Pulmonary syndrome
*icteric= jaundice
1. Bacteraemic leptospirosis
• Bacteraemia can produce a nonspecific illness with high fever, weakness,
muscle pain and tenderness (especially of the calf and back), intense headache,
photophobia, and sometimes diarrhoea and vomiting.
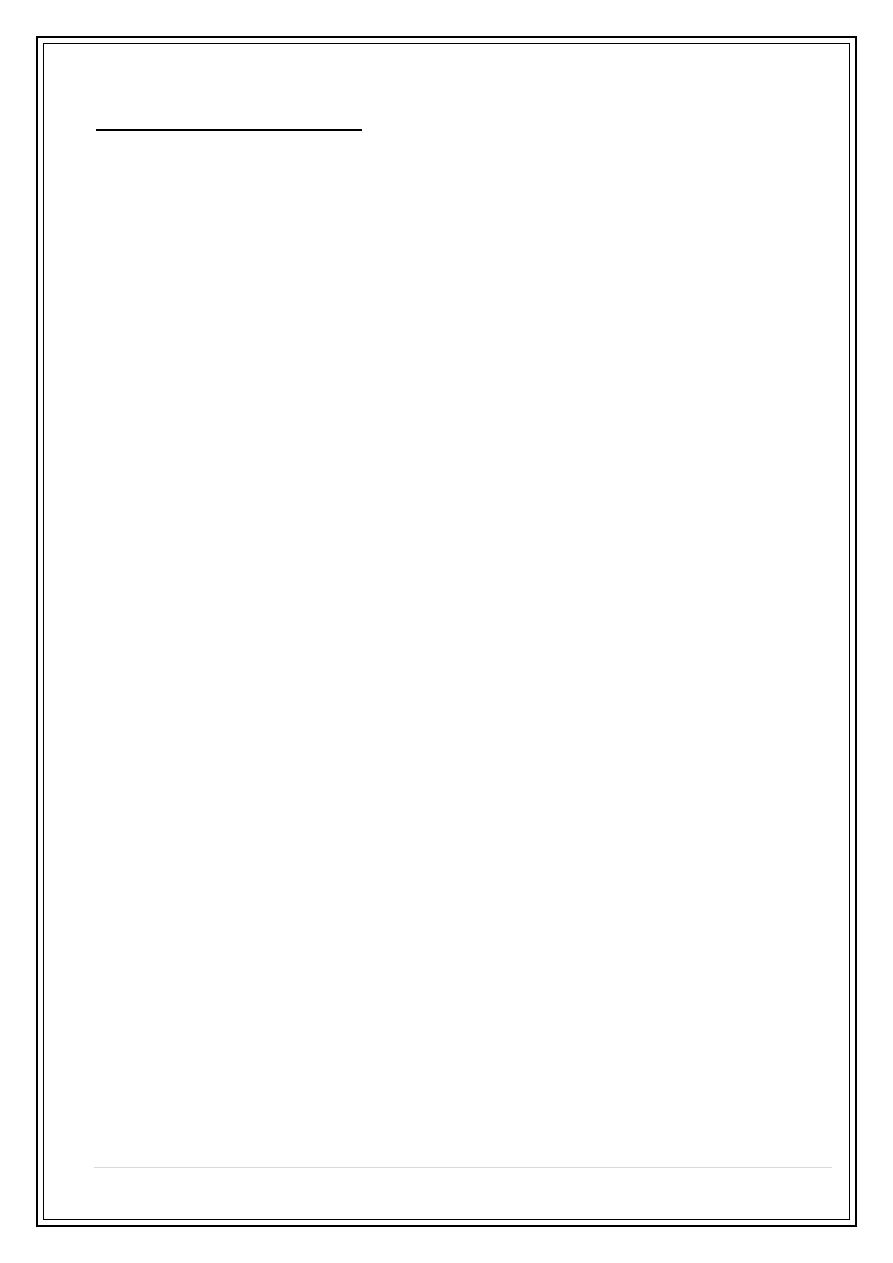
• Conjunctival congestion is the only notable physical sign.
• The illness comes to an end after about 1 week, or else merges into one of the
other forms of infection.
2. Aseptic meningitis
• This illness is very difficult to distinguish from viral meningitis.
• The conjunctivae may be congested but there are no other differentiating signs.
• Laboratory clues include a neutrophil leucocytosis and abnormal liver function
tests.
3. Icteric leptospirosis (Weil’s disease)
• Fewer than 10% of symptomatic infections result in severe jaundice.
• Weil’s disease is a dramatic life-threatening event, characterised by fever,
haemorrhages, jaundice and renal impairment.
• Conjunctival suffusion ( a characteristic sign of leptospirosis )
9 |
P a g e
10 |
P a g e
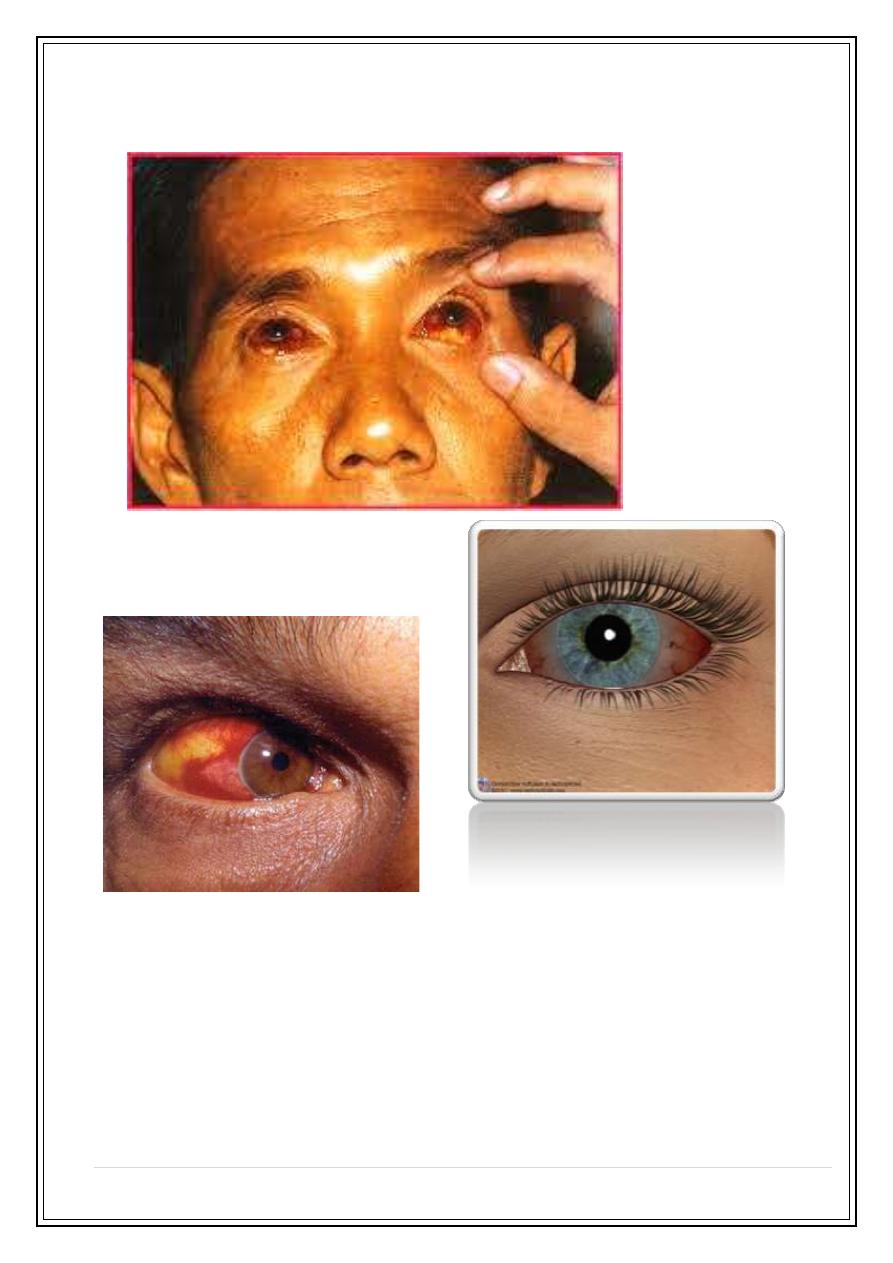
• The patient may have a rash, but the characteristic skin changes are purpura
and large areas of bruising.
• Jaundice is deep and the liver is enlarged.
• Renal failure, primarily caused by impaired renal perfusion and acute tubular
necrosis, manifests as oliguria or anuria.
• In severe cases there may be epistaxis, haematemesis and melaena.
• Weil’s disease may also be associated with myocarditis and encephalitis
• In severe cases there may be epistaxis, haematemesis and melaena.
• Weil’s disease may also be associated with myocarditis and encephalitis
4. Pulmonary syndrome
• This syndrome is characterised by haemoptysis, patchy lung infiltrates on chest
X-ray, and respiratory failure.
• Total bilateral lung consolidation and acute respiratory distress syndrom (ARDS)
with a high mortality (over 50%).
11 |
P a g e
Clinical
syndromes of
leptospirosis
In assessing a patient the most
important factor to apply is their risk
event (patient occupation, animal or
contaminated water contact), as this is
often the only clue to the potential
cause.
12 |
P a g e
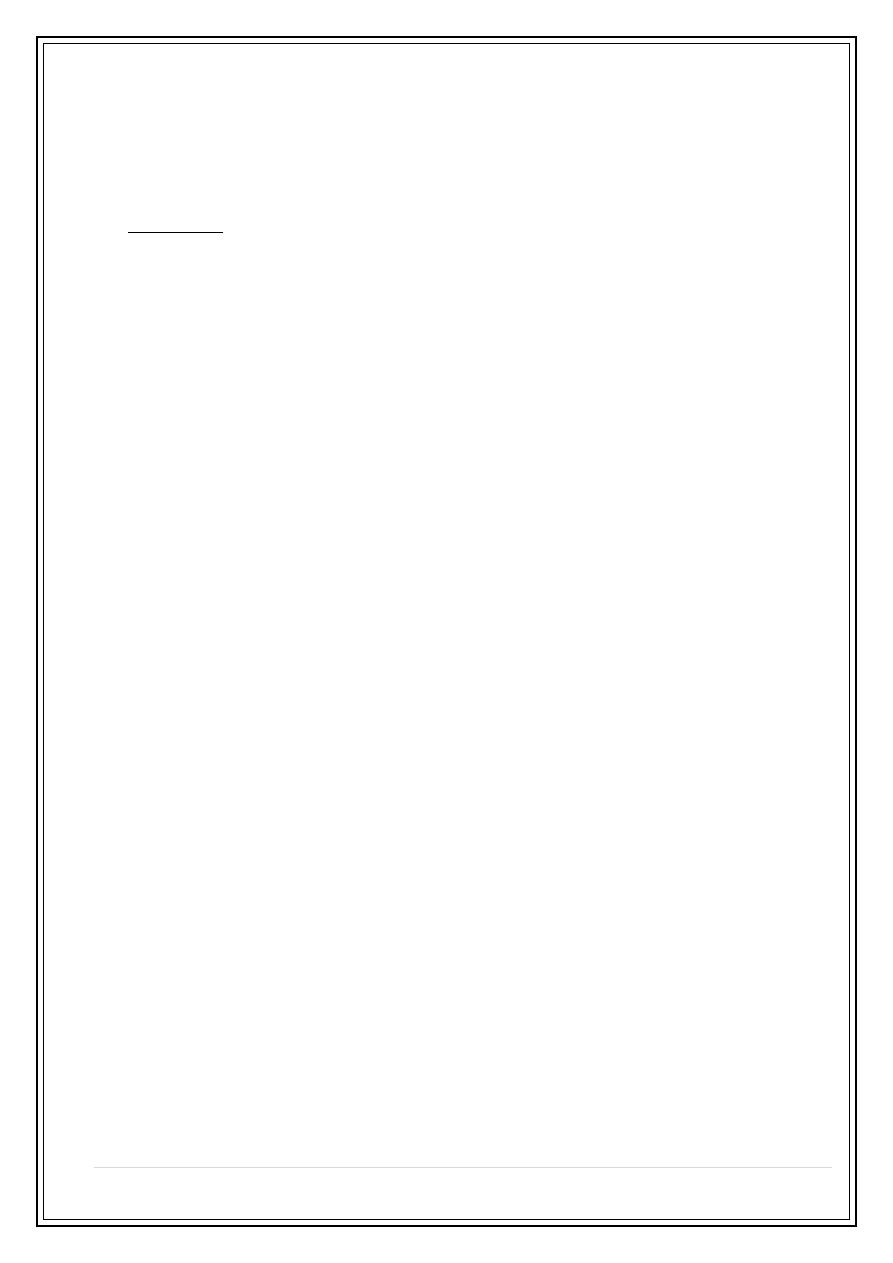
Investigations needed for diagnosis
• Blood cultures: are most likely to be positive if taken early.
• Urine culture: Leptospires appear in the urine during the second week of
illness, and in untreated patients may be recovered on culture for several
months.
Serology:
Serological tests are diagnostic if seroconversion or a fourfold increase in
titre is demonstrated.
o The microscopic agglutination test (MAT) is the test of choice.
o ELISA and immunofluorescent (IF) techniques also useful.
PCR :
Detection of leptospiral DNA by PCR is possible in blood in early
symptomatic disease, and later on in urine and for many months thereafter.
13 |
P a g e
Other non specific tests
Blood test:
o Increase WBC is accompanied in severe infection by decrease platelets and
elevated blood levels of creatine kinase (CK enzyme) .
o In jaundiced patients, there is hepatitis (high liver enzymes) and the
prothrombin time (PT) may be prolonged.
o Acute renal failure is common with elevated blood urea and serum
creatinine.
The cerebrospinal fluid (CSF) in leptospiral meningitis shows elevated protein
level.
Differential diagnoses
Important differential diagnoses.
• Malaria
• Typhoid fever
• Acute viral hepatitis
• Acute viral meningitis
14 |
P a g e
Treatment
• The general care of the patient is critically important.
• Blood transfusion for haemorrhage and careful attention to renal failure, the
usual cause of death, are especially important.
• Renal failure is potentially reversible with adequate support, such as dialysis.
• The optimal antimicrobial regimen has not been established.
• Most infections are self-limiting.
• Therapy with either oral doxycycline (100 mg twice daily for 1 week) or
intravenous penicillin (900 mg 4 times daily for 1 week) is effective but may not
prevent the development of renal failure.
• Parenteral ceftriaxone (1 g daily) is as effective as penicillin.
• Uveitis is treated with a combination of systemic antibiotics and local
corticosteroids.
• There is no role for the routine use of corticosteroids in the management of
leptospirosis.
Prevention
• The risk of acquiring leptospirosis can be greatly reduced by:
Not swimming or wading in water that might be contaminated with animal
urine
Eliminating contact with potentially infected animals.
• Protective clothing or footwear should be worn by those exposed to
contaminated water or soil because of their job or recreational activities.
• Trials in military personnel have shown that infection with L. interrogans can be
prevented by taking prophylactic doxycycline 200 mg weekly.
15 |
P a g e
Case scenario
• A 29 year’s old male presented to the hospital with fever, headache, marked
muscle and joint pain.
• 3 days later, he deteriorated and developed skin rash, red conjuctivae,
yellowish discoloration of sclera and low urine output. His urine looks dark.
• Then he develped severe dyspnea and his consciousness decreased .
• He work as a farmer, with many animals around.
• How can you approach the diagnosis?
Summary
• Infection with Leptospira spirochetes occurs during contact with animal
reservoirs or an environment contaminated with their urine.
• The clinical course of leptospirosis ranges from a mild acute febrile illness to
life-threatening manifestations such as Weil’s disease, which consists of the
triad of jaundice, acute renal failure, and bleeding.
• Leptospirosis has also been recognized as an important cause of pulmonary
hemorrhage syndrome worldwide.
Further readings
• Davidson clinical and practice of medicine 22th ed. 2014.
• Goldman’s Cecil Medicine 24
th
ed 2012.
•
