Dr. Mustafa Nema
Lec. 4
INFECTION IN
IMMUNOCOMPROMIZED
PATIENT
4 / 3 / 2015
2014 – 2015
ﻣﻜﺘﺐ ﺍﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
1
Infection in immuncompromized patient
Dr.Mustafa Nema
Baghdad College of Medicine
2015
Objectives
Describe the main types of immunocompromised conditions
Review the causes of immune suppression
List the major types of infections associated with altered immunity
Outline management of such infections
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
2
Case scenarios
Case 1
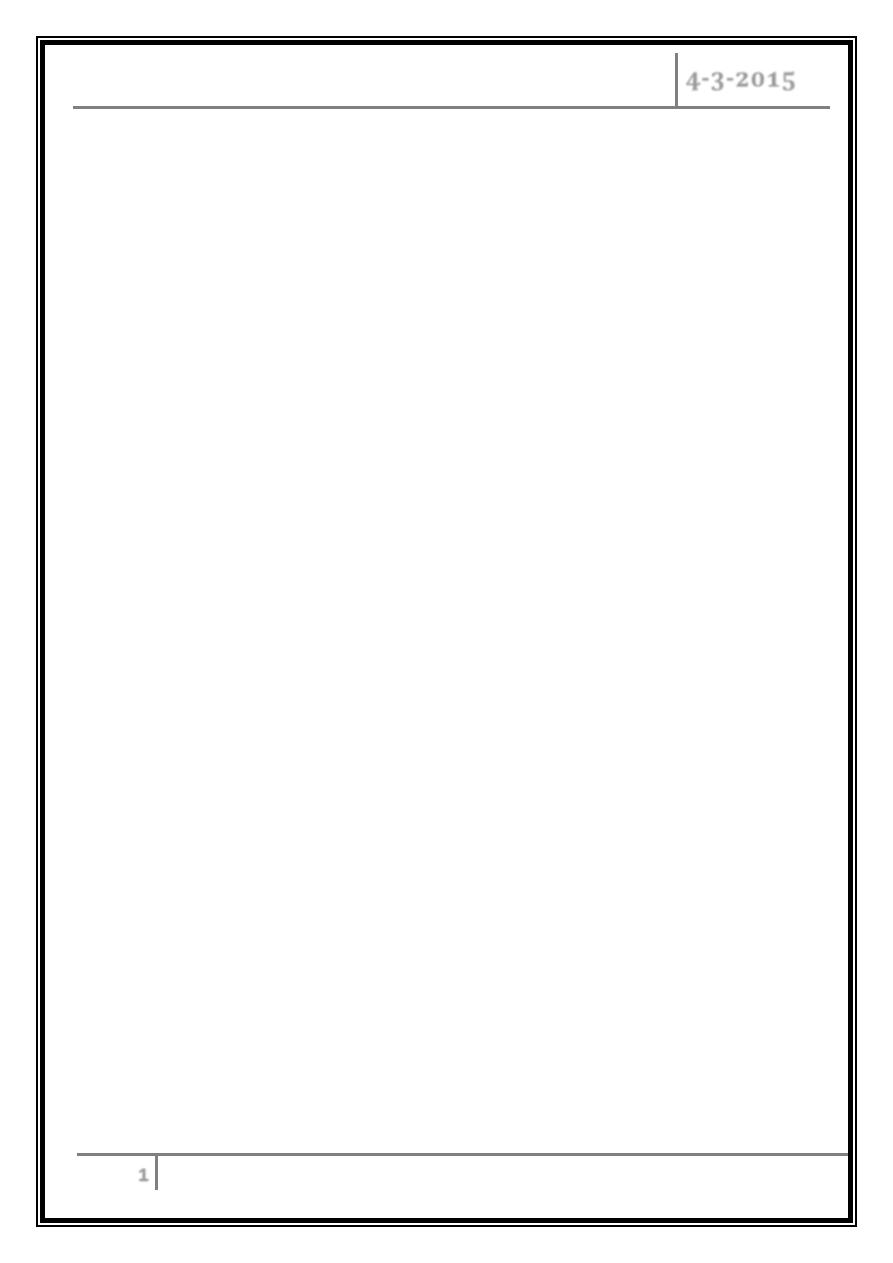
• A 23 years old male presented with recurrent pneumonias. He was responding
well to i.v antibiotics with each hospitalization.
• Blood culture /sputum Gram’s stain and culture showed pneumococcal
pneumoniae.
• He had Hx of abdominal trauma during childhood and laparatomy (abdominal
operation) done
– Lobar pneumonia due to Streptococcus pneumoniae.
– Extensive right middle lobe consolidation.
• Why he had recurrent type of similar microorganism?
• What is the importance of operation history?
• What type of antibiotic was effective?
• What other conditions that could case similar effects?
•
Suggest a future plan to prevent recurrent infection
.
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
3
Case 2
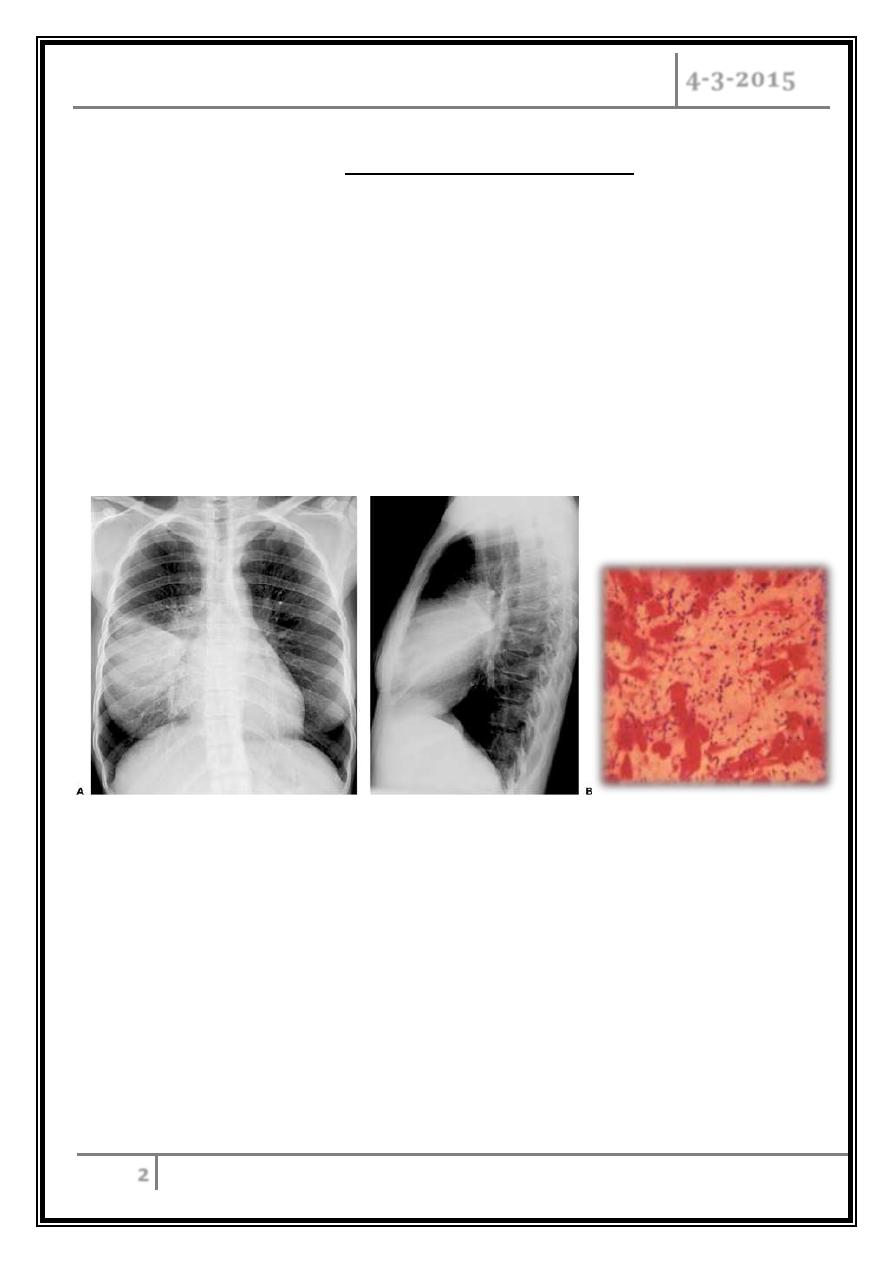
• A young female with acute
myeloid leukemia receiving
chemotherapy developed fever
40
0
C and cough.
•
You arrange for CXR which show
no much abnormality. CT chest
done and shown
.
• Neutrophil count is 1 x 109/L
• Multiple iv antibiotics given for 4 days with no response.
• What is the most likely Dx?
• What treament should be given now?
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
4
Introduction
Immunity
Two Intrinsic Defense Systems
1. Innate (nonspecific) system.
e.g. Skin, mucosa and some antimicrobial proteins.
2. Adaptive (specific) defense system
Humoral immunity ( B cells, ab producing) .
Cell- mediated immunity (T cells non-ab producing ).
Immune-competent and immune-compromised body
When immune system function is normal = immune-competent and vice versa with
immune-compromised.
Immunodeficiency (or immune deficiency) is a state in which the immune system's
ability to fight infectious disease is compromised or absent.
Immune deficiency may arise through primary (intrinsic) defects in immune
function, but is much more commonly due to secondary causes, including drug
therapy, malignancy and ageing.
Immunocompromising conditions:
Primary
Secondary
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
5
Primary (Congenital) conditions
Congenital conditions most commonly affect the newborn and children
e.g. :
– Primary deficiencies of B and∓ T cells
– Primary phagocyte deficiencies e.g Chronic granulomatous disease.
– Complement pathway deficiencies e.g. Deficiency of the regulatory protein C1
inhibitor.
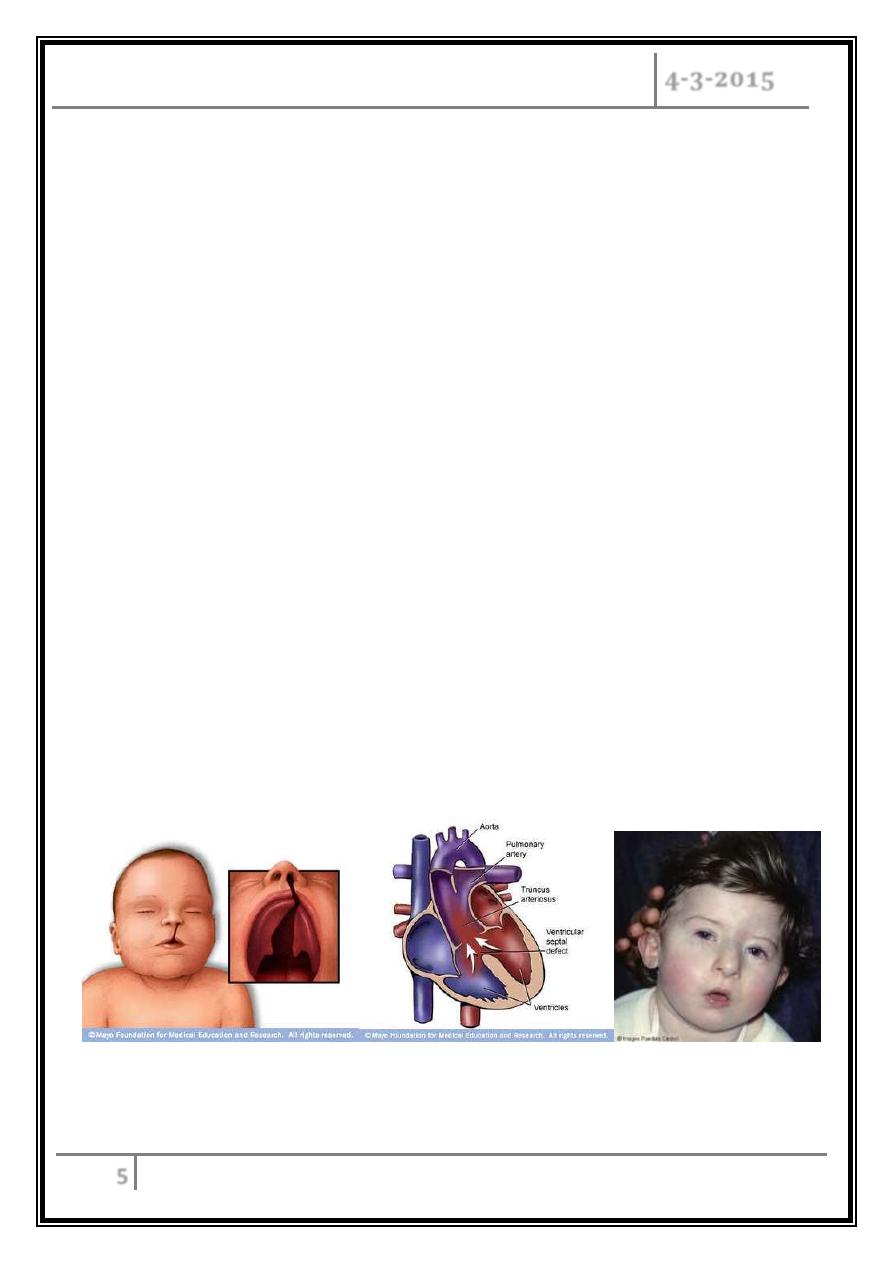
Examples of primary immune deficiency
Example 1
Primary T-lymphocyte deficiencies:
o Characterised by recurrent viral, protozoal and fungal infections .
o Very low numbers of circulating T cells.
o Present in childhood e.g. DiGeorge syndrome
o DiGeorge syndrome : associated with multiple abnormalities, including
congenital heart disease, hypocalcaemia tracheo-oesophageal fistulae, cleft
lip and palate, and absent thymic development.
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
6
Example 2
Primary B cell (antibody) deficiency:
o
Selective IgA deficiency:
– Is the most common primary immune deficiency that can also present in
adulthood.
– In most patients, low or undetectable IgA is an incidental finding with no
clinical sequelae.
– However, 30% of individuals experience recurrent mild respiratory and
gastrointestinal infections.
– In some patients, there is a compensatory increase in serum IgG levels.
– Specific treatment is generally not required.
o
Other Antibodies defeciencies: e.g. Ig G, IgM.
Investigations
Investigations include serum immunoglobulins, B and T lymphocyte counts in blood.
Management
With the exception of individuals with selective IgA deficiency, patients with other
antibody deficiencies (like IgG, IgM) require aggressive treatment of infections,
and prophylactic antibiotics may be indicated.
The mainstay of treatment is life-long immunoglobulin replacement therapy.
Immunization is generally not effective especially with IgG deficiency. Why?
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
7
Secondary immune deficiencies
Secondary immune deficiencies are much more common than primary immune
deficiencies.
Causes of secondary immune deficiency
Physiological
• Ageing
• Prematurity
• Pregnancy
Infection
• HIV
• Measles
• Mycobacterial infection
Iatrogenic
• Immunosuppressive therapy
• Corticosteroids
• Stem cell transplantation
• Radiation injury
Malignancy
• B-cell malignancies including
leukaemia, lymphoma and myeloma
• Solid tumours
• Thymoma
Biochemical and nutritional disorders
• Malnutrition
• Renal insufficiency/dialysis
• Diabetes mellitus
• Specific mineral deficiencies, e.g.
iron, zinc
Other conditions
• Burns
• Asplenia/hyposplenism
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
8
How can a patient with immune deficiency presents
to you and how can you manage?
Most patients with an immune deficiency present with: Recurrent Infections.
An immunocompromised person may be particularly vulnerable to opportunistic
infections (An infection caused by an organism that does not normally cause
disease), in addition to normal infections that could affect everyone.
In primary immune deficiency…
• Many warning signs may help in suspecting the presence of primary immune
deficiency in newborn /childhood.
• The presence of ≥ 2 warning signs may indicate an underlying primary
immunodeficiency:
o ≥ 4 new ear infections
within 1 yr
o ≥ 2 serious sinus infections
within 1 yr
o ≥ 2 months on antibiotics
with little effect
o ≥ 2 pneumonias within 1
yr
o Failure of an infant to gain
weight or grow normally
o Recurrent, deep skin or
organ abscesses
o Persistent thrush in mouth
or fungal infection on skin
o Need for intravenous
antibiotics to clear
infections
o ≥ 2 deep-seated infections,
including septicaemia
o A family history of primary
immune deficiency
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
9
When secondary immune deficiency suspected…
the following should be addressed in the
history:
Identification of the immunosuppressant factors, and nature of the immune
defect.
Any past infections and their treatment.
Opportunistic infections.
Prophylactic medicines and vaccinations administered.
Examination:
Examination should include inspection of the normal physical barriers provided by
skin and mucosal surfaces and, in particular, central venous catheters, the mouth,
sinuses, ears and perianal area. ( Do Not forget hidden areas ).
The areas around fingernails and toenails should also be inspected closely.
Investigations
• If the clinical features do not suggest a specific infection, then initial investigations
should include:
– A full blood count with differential count.
– Blood glucose, urea and liver function tests.
– Inflammatory markers: erythrocyte sedimentation rate (ESR) and C-reactive
protein (CRP).
– A test for antibodies to HIV-1
• Chest X-ray and chest CT scan should be considered when respiratory symptoms
occur.
• Abdominal imaging may also be warranted, particularly if there is right lower
quadrant pain, which may indicate typhlitis (inflammation of the caecum) in
neutropenic patients.
• Culture of the blood, central venous catheter site, urine, and stool if related
symptoms and sign present.
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
10
Specific conditions
Neutropenic fever
A reduction in neutrophil count (usually less than 1.5 × 109/L) is called
neutropenia
Neutropenia is a common complication of malignancy.
It is usually secondary to chemotherapy but may occur with radiotherapy if
large amounts of bone marrow are irradiated.
It may also happened due to malignant infiltration of the bone marrow.
The risk of bacterial infection is related to the degree of neutropenia, with
counts lower than 0.5 × 109/L considered to be critically low.
The risk of sepsis is related to the severity and duration of neutropenia and
the presence of other risk factors such as intravenous or bladder catheters.
Neutropenic fever is an emergency in cancer patients as, if left untreated, it
can result in septicaemia with a high mortality rate.
• Neutropenic fever is an emergency in cancer
patients as, if left untreated, it can result in
septicaemia with a high mortality rate.
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
11
Clinical features
– The typical presentation is high fever and affected patients are often non-
specifically unwell.
– Hypotension is an adverse prognostic feature and may progress to systemic
circulatory shutdown and organ failure.
Investigations and Treatment
o An infection screen should be performed.
o Typical first-line empirical therapy consists of an anti-pseudomonal β-lactam
(ceftazidime, cefotaxime or meropenem), or a combination of an aminoglycoside
and a broad-spectrum penicillin with anti-pseudomonal activity (gentamicin and
piperacillin).
o Metronidazole should be added if anaerobic infection is suspected.
o Flucloxacillin or vancomycin when Gram-positive infection is suspected (for
example, in patients with central lines).
o If there is no response after 36–48 hours, treatment with amphotericin B should
be considered to cover fungal infection.
o Other supportive therapy, including intravenous fluids and dialysis, may be
required.
Infections in transplant recipients
Infections in solid transplant recipients are grouped according to the time of
onset.
Those in the first month are related to the underlying condition or surgical
complications.
Those occurring 1–6 months after transplantation are characteristic of impaired
T-cell function.
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
12
Types of immune deficiency, causes and
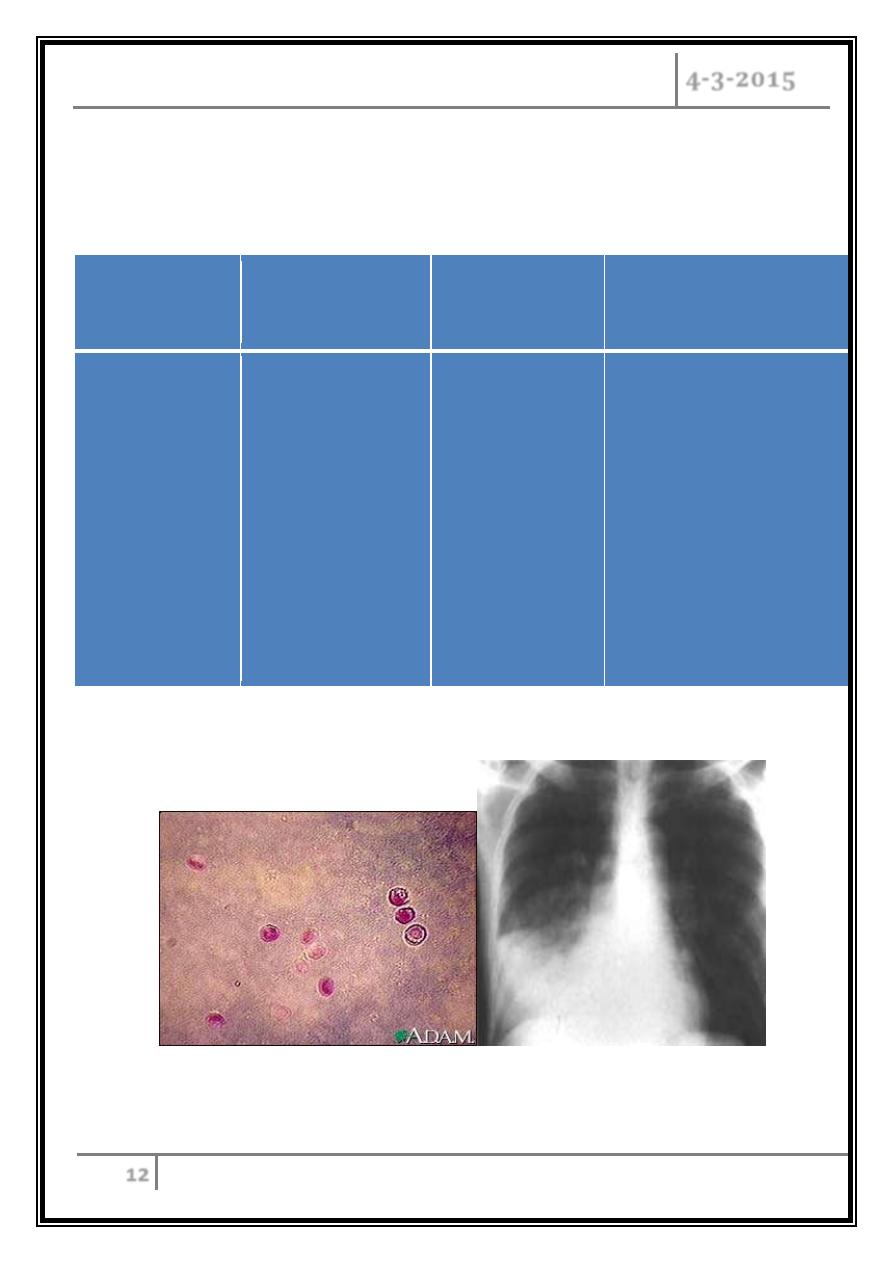
resultant infection
Type of immune
deficiency
Affected
components
Main causes
Main pathogens of
resultant infections
Humoral
immune
deficiency
B cells, plasma
cells or antibodies
o Primary
humoral
o Multiple
myeloma
o Chronic
lymphoid
leukemia
o AIDS
o Streptococcus
pneumoniae
o Hemophilus
influenzae
o Pneumocystis
jirovecii
o Giardia intestinalis
o Cryptosporidium
parvum
Cryptosporidium parvum Strept pneuomonia
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
13
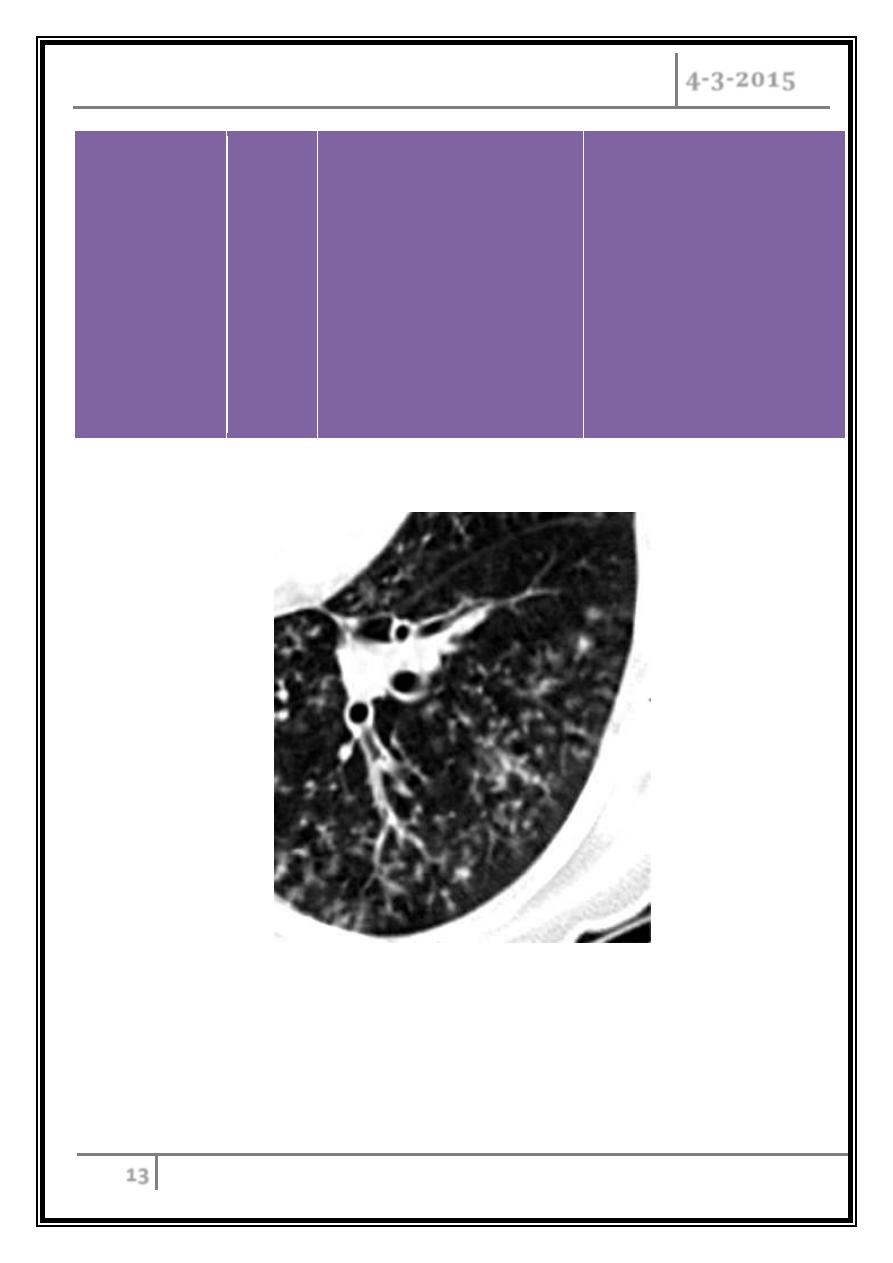
T cell
deficiency
T cells
Marrow and other
transplantation
AIDS
Cancer chemotherapy
Lymphoma
Glucocorticoid
therapy
Intracellular
pathogens, including
Herpes simplex virus,
Mycobacterium,
Listeria, and
intracellular fungal
infections.
Miliary TB

INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
14
Neutropenia
Neutrophil
granulocytes
o Chemotherapy
o Bone marrow
transplantation
o Dysfunction, such
as chronic
granulomatous
disease
o Oral
Streptococci
o Pseudomonas
aeruginosa
o Enterococcus
species
o Candida species
o Aspergillus
species
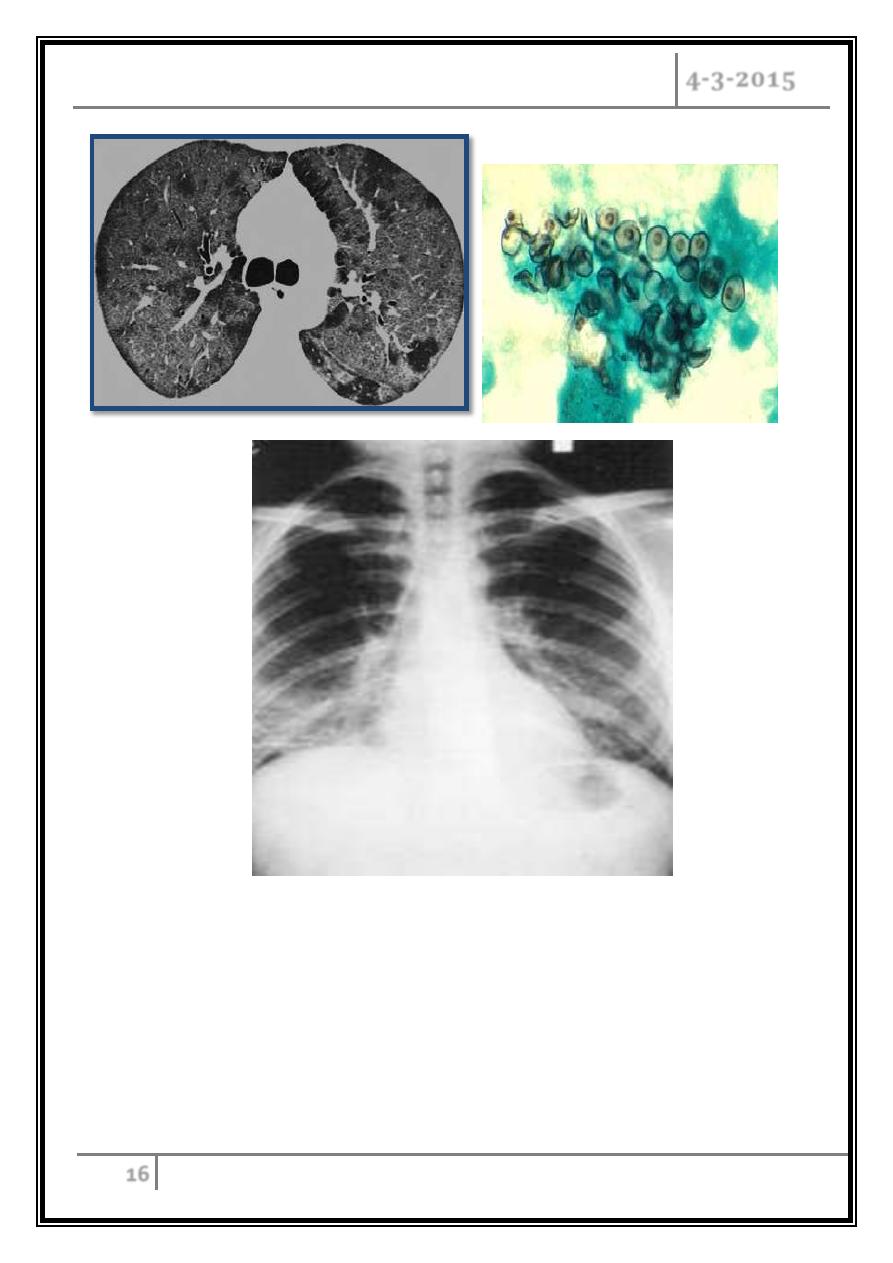
Aspergillus lung infection
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
15
Asplenia
Spleen
o
Splenectomy
o
Trauma
o
Sickle-cell anemia
Polysaccharide encapsulated
bacteria,particularly:
Streptococcus pneumoniae
Haemophilus influenzae
Neisseria meningitidis
Examples of Opportunistic infections
Bacterial
• Mycobacterial infections including
M.avium complex
• Legionellosis
• Nocardia
Viral
• CMV
• Herpes simplex
• Adenovirus
• Actinomycetes
Parasitic
• Pneumocystis jirovecii pneumonia
(PJP). the old name is P.carinii
pneomonia (PCP)
• Toxoplasmosis
• Cryptosporidiosis
• Generalised strongyloidiasis
Fungal
• Candidosis
• Cryptococcosis
• Aspergillosis
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
16
Pneumocystis jirovecii
( pneumonia )
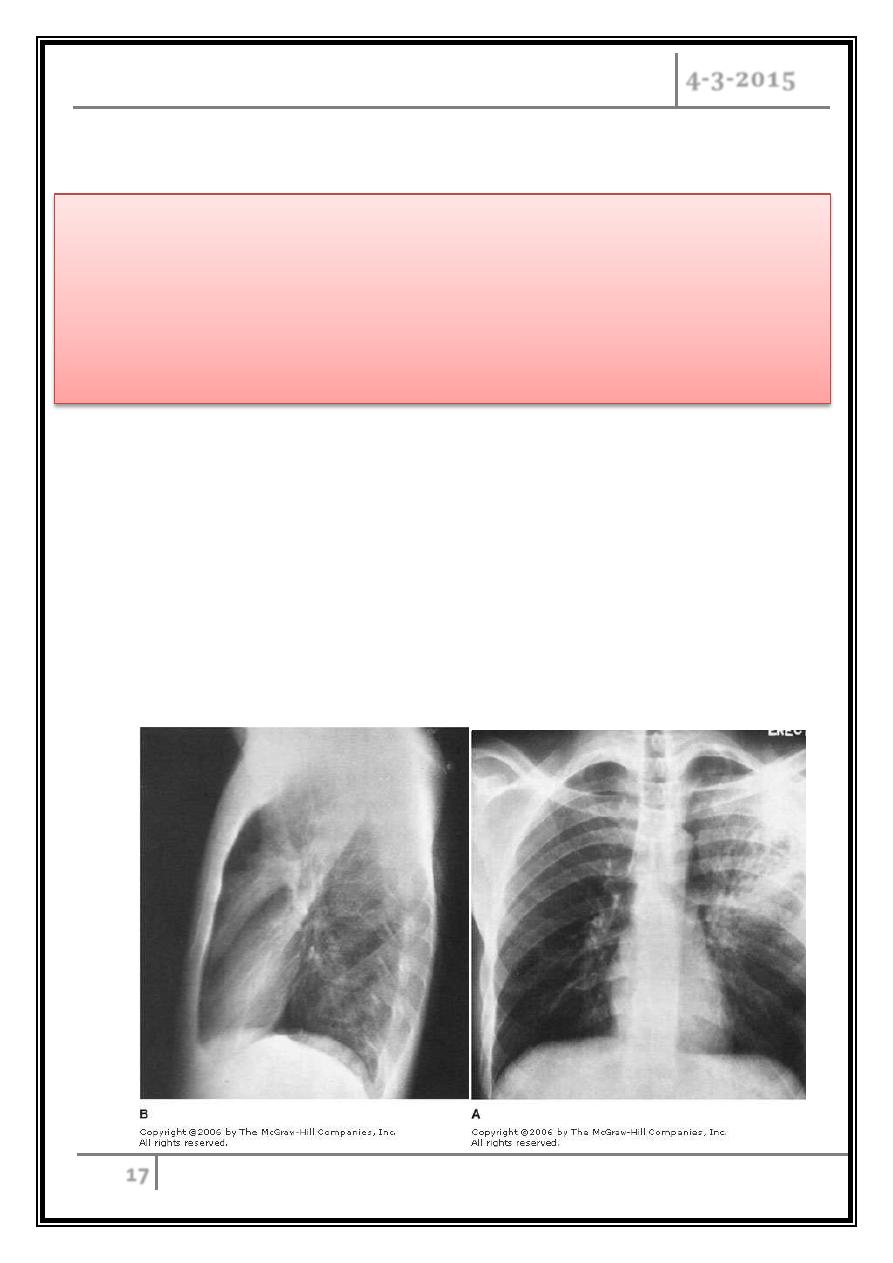
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
17
Vaccine
Case 3
• A 37 years old presented with chronic cough, fever and hemoptysis.
• He gave history of chronic steroid use for his poorly controlled asthma.
• His chest X ray shown.
New guidelines recommend that most
immunocompromised patients should
be vaccinated.
INFECTION IN IMMUNOCOMPROMIZED Dr.Mustafa Nema
PATIENT
4-3-2015
18
• What is the most likely Dx?
• Why he develop such type of infection?
• What is the treatment plan?
• What other conditions that could cause similar infection?
Readings
Davidson clinical and practice of medicine 22th ed. 2014.
