Sunday 2 / 11 / 2014
@Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
"Pharmacology
مكتب اشور لالستنساخ
ADRENERGIC SYSTEM
Lecture 5
Total lectures NO. 11
Dr. Haidar Al-Shakarchi
Page 2
Adrenoceptor Blocking Drugs:
Alpha-Adrenoceptor Blocking Drugs:
The first generation of alpha adrenoceptor blockers were non-selective, blocking
both alpha
1
and alpha
2
receptors.In general, blockade of alpha-receptors
reduces the sympathetic tone of blood vessels resulting in decreased TPR.When
subjects taking an alpha-blocker rise from supine to erect posture the
sympathetic system is activated via baroreceptors. The normal vasoconstrictive
(alpha
1
) effect( to maintain blood pressure) is blocked by the drug, and the
failure of this response results in postural (orthostatic) hypotension.The
sympathetic system is further activated to release more and more
transmitter.This increase in transmitter would normally be reduced by negative
feedback via alpha
2
adrenoceptors; but these receptors are blocked too. The
excess transmitter(noreinephrine) released is free to act on the beta-
adrenoceptors ( beta 1) causing an unpleasant tachycardia and increased
cardiac output.So reflex cardiac stimulation is due to barorecepter reflex and
blocking the alpha
2
receptors of the cardiac symathetic nerves.
It is for this reason(unsuccessful in maintaining lowered B.P.) that non-selective
alpha-blockers are not used ALONE in essential hypertension.
An alpha
1
-blocker that spares the alpha
2
receptor, so that negative feedback
inhibition of noradrenaline is maintained, is more useful in hypertension.
The nonselective alpha-blockers include:
phentolamine, phenoxybenzamine and prazosin.
The selective alpha
1
receptor blockers include:
prazosin, terazosin,and doxazosin
treatment of hypertension and
tamsulosin and alfuozosin
treatment of B.P.H.
Page 3
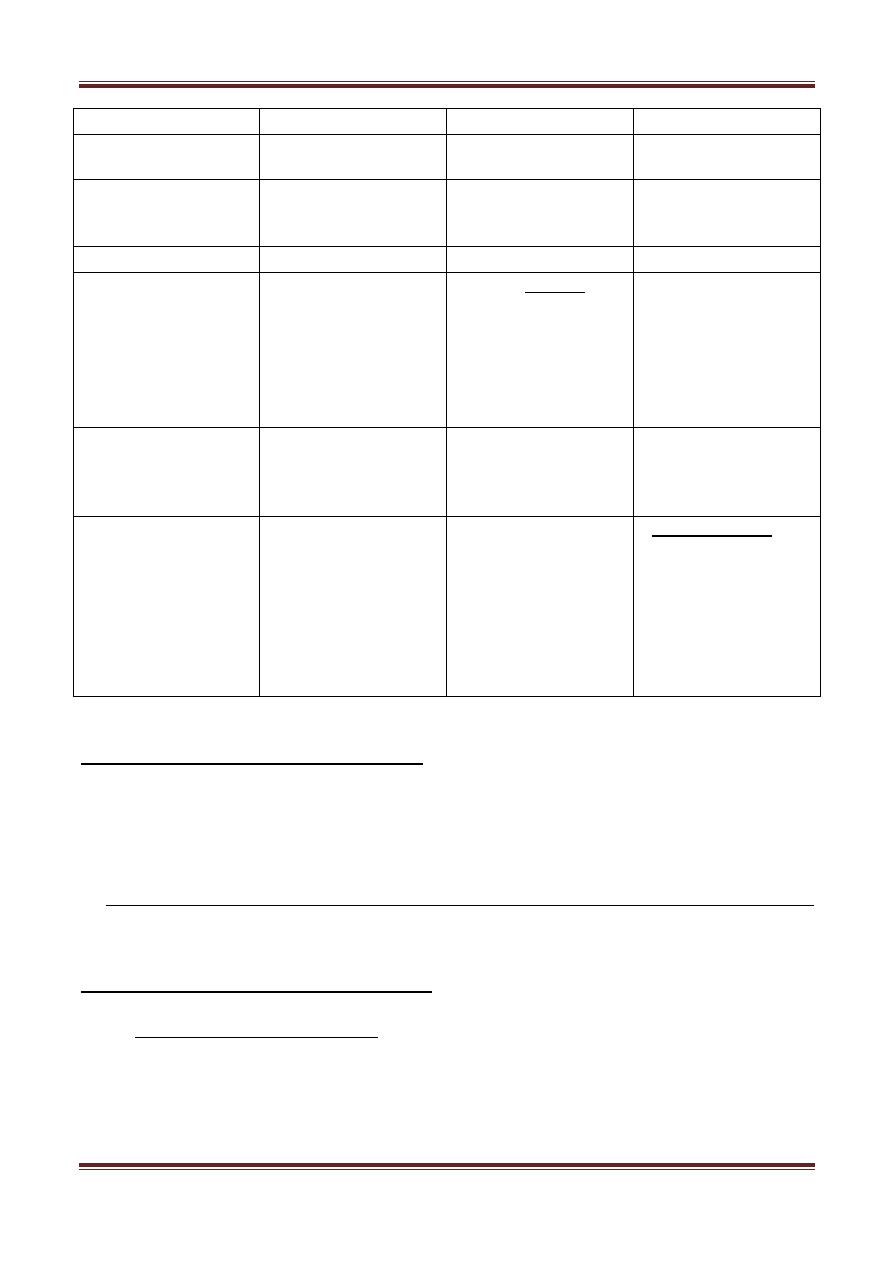
Phentolamine
Phenoxybenzamine
Prazosin
Receptor Blocking
Alpha
1
=Alpha
2
(non-selective)
Alpha
1
> Alpha
2
(non-selective)
Only alpha
1
(Selective)
Reversibility
Reversible
Irreversible, binds
covalently to alpha
receptor
Reversible
Administration
Injection (emergency)
Orally and Injection
Orally and Injection
Active Metabolite
It's a prodrug ;
undergoes
biotransformation to
the active form, a
delay of a few hours
occurs before alpha
blockade develops
Duration of Action
Short
Long (14-48) hours
because it depends on
the synthesis new
adrenoceptors
Intermediate
Side effects
(peculiar to the
drug)
Others are listed
below
Diarrhea and
increased gastric acid
production.
Agonists at
muscarinic and
histamine receptors.
Alkylating agent,
causes tumors in
animals.
Blocks ACh and
histamine receptors.
First dose effect,the
first dose may cause
brisk hypotension
sufficient to cause loss
of consciousness.
Initiate treatment
with a low dose and
on going to bed.
Common side effects of Alpha Blockers:
1) Hypotension and postural hypotension.
2) Tachycardia and worsening angina
3) Nasal stuffiness and red sclerae
4) In the male, failure of ejaculation and retrograde ejaculation
Therapeutic uses of alpha-blockers:
1) Peripheral vascular disease:
Individuals with Raynaud's Phenomenon and other conditions involving
excessive reversible vasospasm in the peripheral circulation do benefit from
alpha-blockers, though calcium channel blocker may be preferable for many
Page 4
patients . However there's no evidence that the effects are significant when
morphological changes limit flow in the vessels.
2) Urinary obstruction:
Alpha-receptor blockade was found to be helpful in benign prostatic
hyperplasia(B.P.H.).The mechanism of action involves partial reversal of smooth
muscle contraction in the enlarged prostate and in the bladder neck. The efficacy of
several alpha
1
receptor antagonists in patients with BPH was
demonstrated.Tamsulosin is more potent inhibitor of the alpha
1A
receptor found on
the smooth muscle of the prostate.In the tratment of B.P.H., a 5α-reductase
inhibitor e.g. finasteride may be used.
3) Local Vasoconstrictor Excess:
They're useful to reverse the intense local vasoconstriction caused by
accidental infiltration of alpha-agonist into subcutaneous tissue during I.V.
administration.
4) Pheochromocytoma:
Tumor of the adrenal medulla causing increased secretion of adrenaline and
noradrenalin resulting in hypertension, arrhythmia, angina and
hyperglycemia.
In case of emergency we use phentolamine I.V. while in chronic cases we use
phenoxybenzamine or prazosin.
5) Hypertension and Hypertensive emergencies:
A) Essential Hypertension:
The alpha-blockers have limited application in the management of
hypertension.If beta-blockers or diuretics fail to control hypertension,
prazosin or other SELECTIVE alpha
1
-blockers may be added.
B) Secondary Hypertension:
The alpha adrenoceptor antagonists are most useful when increased
blood pressure reflects excess circulating concentrations of
catecholamines which may result from:
Pheochromocytoma
Page 5
Interaction of tyramine containing food (e.g.cheese) with MAO
inhibitors
Clonidine withdrawal
In these circumstances, phentolamine (non-selective) can be used to
control high blood pressure.
Alpha
2
antagonists:
Yohimbine is a weak alpha
2
adrenoceptor blocking agent i.e. it blocks the negative
feedback receptor so that adrenergic activity is enhanced. It works at the level of
the C.N.S to increase sympathetic out flow to the periphery.
Therapeutic uses: They have so little clinical usefulness.An experimental interest
for use in:
1) Autonomic insufficiency.
2) May improve symptoms in patients with painful diabetic neuropathies.
3) Improves male sexual function i.e. useful for impotence.
4) Raynaud's phenomenon.
5) Type II diabetes: ( alpha
2
receptors inhibit insulin secretion).
6) Psychiatric depression.
Beta-Adrenoceptor Blocking Drugs:
These drugs antagonize the effects of catecholamines at beta-adrenoceptors.
All beta-blockers are competitive antagonists. The effects depend on the amount of
sympathetic tone present e.g. exercise.
Pharmacodynamics of beta-blockers:
1) Cardiovascular system
They have both negative inotropic and negative chronotropic effects
(i.e. reduce both contractility and automaticity, respectively).
Slowed AV conduction with an increased PR interval is a related result.
Page 6
Cardiac output, work, and O
2
consumption are decreased by blockade
of beta
1
receptors; these effects are useful in the treatment of angina.
The beta-blockers are effective in attenuating supraventricular cardiac
arrhythmias, but are generally less effective against ventricular
arrhythmias.
In the vascular system,beta receptor blockade opposes beta
2
mediated
vasodilation. This may result initially in a rise in peripheral resistance
from unopposed alpha-receptor mediated effects as the sympathetic
nervous system discharges in response to lowered blood pressure.
With chronic use peripheral resistance returns to about pre-treatment
levels or a little below. The reduction in the cardiac output leads to
decreased blood pressure.
Beta-blockers antagonize the release of renin . No postural
hypotension occurs since alpha
1
receptors that control vascular
resistance are unaffected.
2) Respiratory tract:
Blockade of beta
2
receptors in bronchial smooth muscle may lead to an
increase in airway resistance, particularly in patients with airway disease.
3) Eye:
Several beta-blockers reduce intraocular pressure especially in glaucoma.
The mechanism is decreased aqueous humor production.
4) Metabolic and Endocrine:
Reduced blood pressure cause a decrease in renal perfusion, resulting
in an increase in sodium retention and plasma volume.
Beta-antagonists inhibit sympathetic nervous system stimulation of
lipolysis.
They decrease glycogenolysis,and decrease glucagon secretion.
The chronic use of beta-blockers has been associated with increased
plasma concentrations of VLDL and decreased concentrations of HDL
cholesterol.
They enhance the hyperkalemia of muscular exercise.
Page 7
Pharmacokinetics:
First order kinetics applies to elimination from plasma but receptor block follows a
zero order decline. Thus the t half of pharmacodynamic effect exceeds the
elimination t half of the substance in blood.
