Sunday 9 / 11 / 2014
@Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
مكتب اشور لالستنساخ
ANTI-HYPERTENSIVES
Lecture 1
Total lectures NO. 13
Dr. Mohammed Rashad

Antihypertensives
Hypertension is defined as a persistant elevation of systolic &/or diastolic B.P to above
140/90 mmHg in person aged 18 years or olden.
Aetiolog :-
Primary, essential, multifactorial, age, genetics, environmental, weight, race.
Secondary hypertension :
Mechanisms for controlling B.P:-
1. Baroreceptors & the sympathetic N.S (moment to moment regulation of B.P – short
term)
2. Rennin-angiotensin-aldosterone (long term regulation of B.P - RAAS)
Classification of antihypertensive drugs
1. ACE inhibitors
Captopril, Enalpril, Lisinopril
2. Angiotensin II – receptor antagonists (ARBs)
Losartan, valsartan, telmisartan
3. Rennin inhibitors
Aliskiren
4. calcium channel blockers (CCBs)
nifidipine, verapamil, deltiazem, amlodipine, nicardipine, nimodipine.
5. Diuretics
Thiazides : H.ch.thiazide, chlorthalidone, indapamide
High ceiling : furosemide
K
+
sparing: spirenolactone, triamterene, amiloride
6. B adrenergic blockers
Proprandol, atendol, metoprolol
7. Alpha adrenergic blockers
Prazosin, terazosin, doxazosin
8. Beta & alpha adrenergic blockers
Labetalol, carvedilol
9. Central sympathetics
Clonidine, methyldopa
10. Vasodilators:
Arteriolar (hydralazine, minoxidil, dinzoxide)
Arteriolar + venous (Na nitroprusside)
Chemical strategies
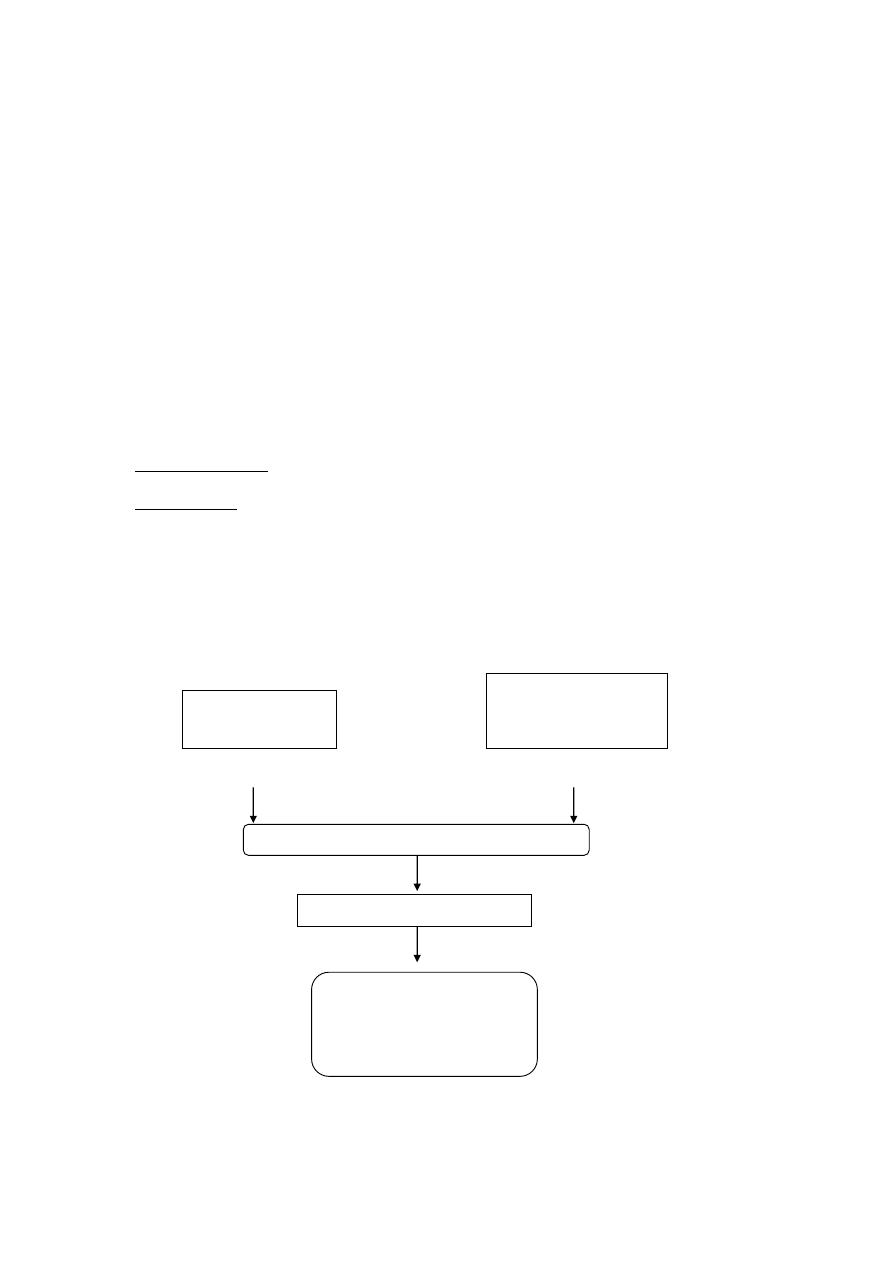
Drug therapy : ACD scheme for antihypertensive therapy
the treatment target blood pressure of <140/<85 suggested by British hypertension
society (BHS) will increase the patient needing 2 or more drugs
a simple stepped regemen is the (ACD) scheme in the following (2006-NICE & BHS)
A
C or D
add
ACD scheme for escalation of antihypertensive therapy (A= ACE inhibitor___C=CC
blocker___D=diuretic)
Younger than 55
years
55 years or older
Or blacke of any age
A+C or A+D
A+C+D
Further diuretic or
Alpha-blocker or
Beta-blocker
Step 1
Step 2
Step 3
Step 4
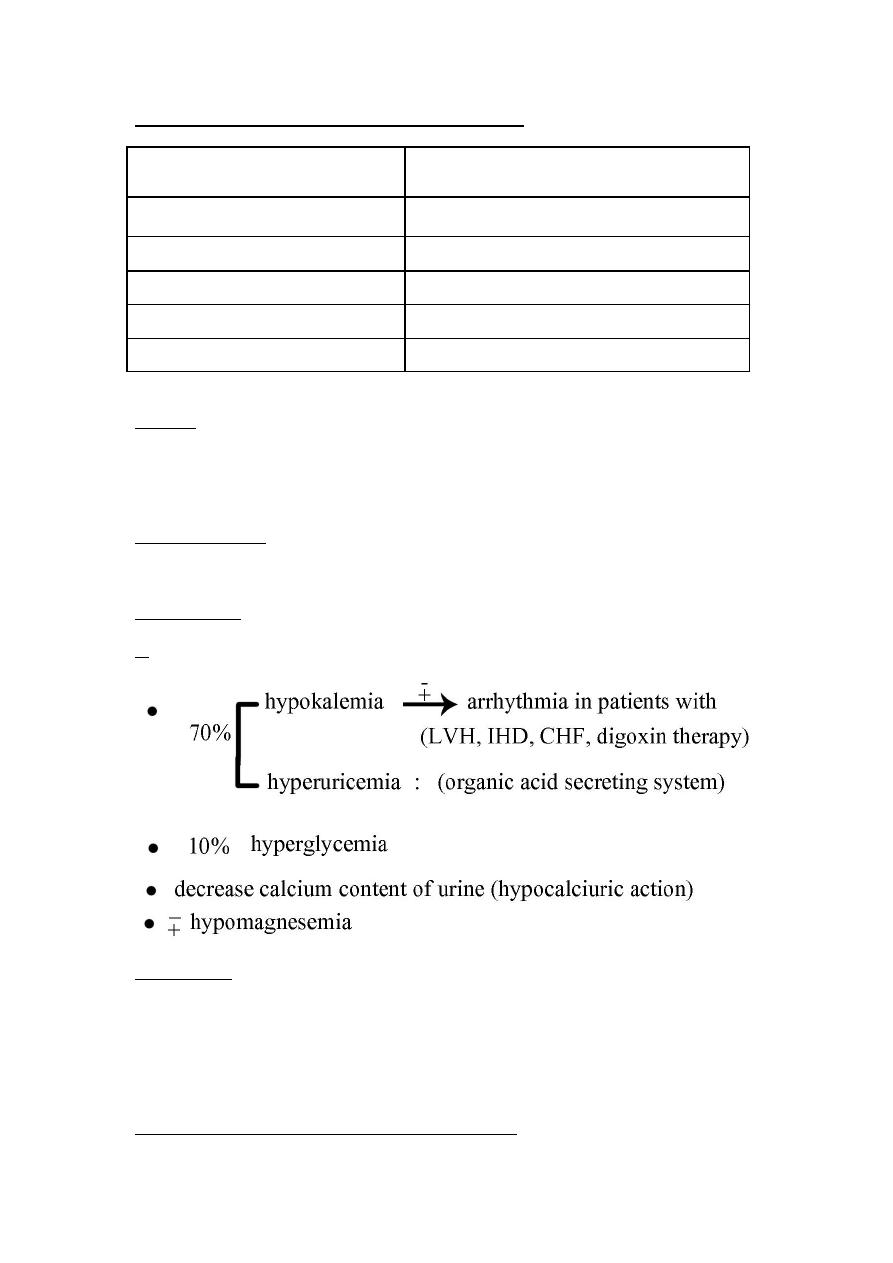
Treatment of HPT in patients with concomitant diseases.
HPT + angina (high risk)
Beta blockers Ca
+2
blockers
HPT + diabetes
Diuretics ACEIs ARBs
HPT + stroke (recurrent)
ACEIs
HPT + heart failure
D
B ACEIs ARBs
HPT + MI (previous)
B ACEIs
HPT + chronic renal disease
ACEIs ARBs
Diuretics
-Low dose is safe & effective in preventing stroke, MI & CHF ( decrease mortality)
-Superior to B-blockers for treatment of HPT in older adult
I- thiazide diuretics
Mechanism of action of thiazide in treatment of HPT :
Adverse effects
II-
Loop diuretics
act even in patients with poor renal function
cause decreased renal vascular resistance & increase renal blood flow
loop diuretics increase the calcium content of urine
III-Potassium-sparing diuretics (reduced K
+
loss in urine)
Amilorid & triametrine (inhibitors of sodium transport & late distal & collecting
ducts)
Spirinolactone (cardiac remodeling in heart failure) & eplerenone (aldosterone-
receptor antagonist)
Alpha-beta- adrenoreceptor blocking agents
labetalol & carvedilol block α1, β1 & β2 receptors.
carvedilol: 1- an effective hyperantitensive
2-mainly used in treatment of heart failure (reduce mortality)
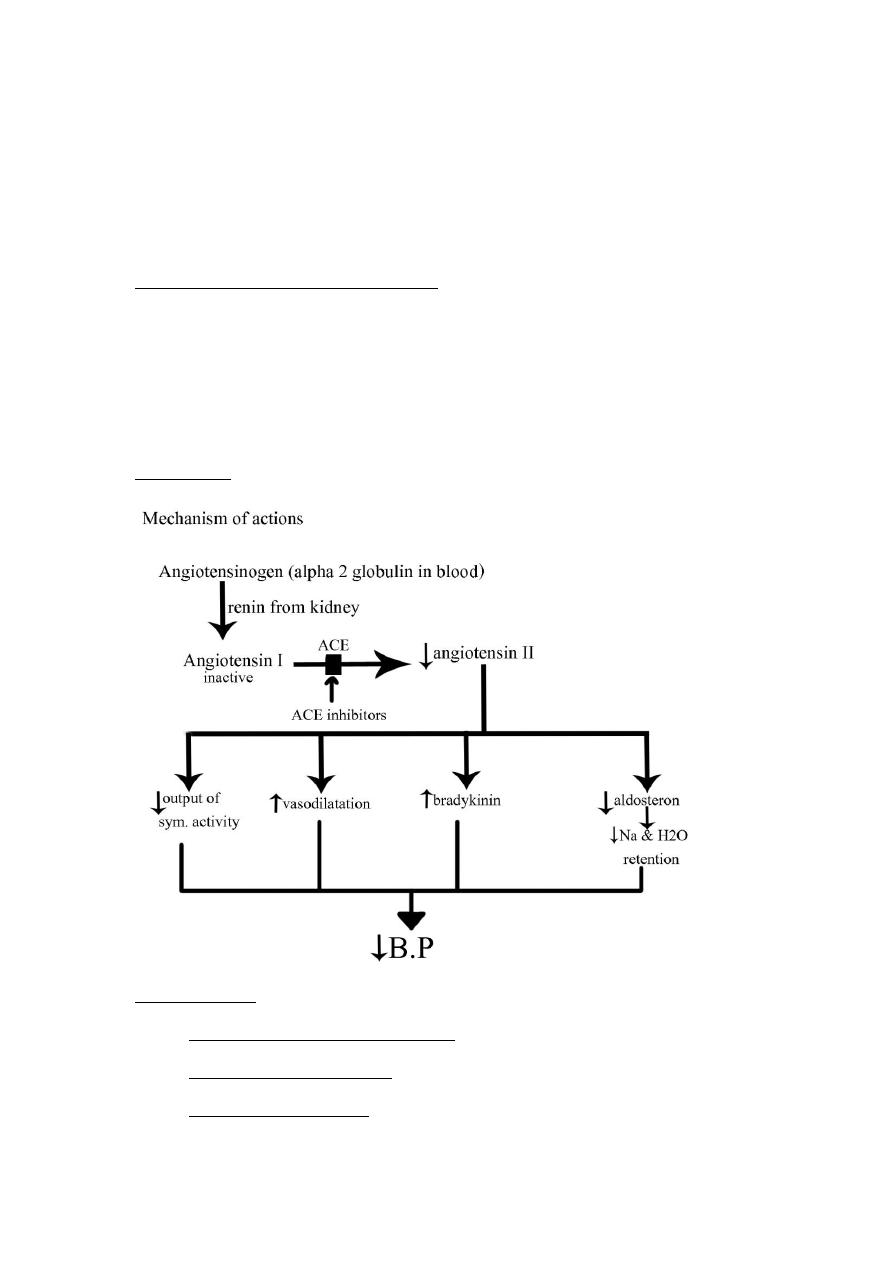
ACE inhibitors
Therapeutic uses:
1. Hypertensive patients (white & young)
2. CHF (congestive heart failure)
3. Myocardial infarction (MI)
4. Prophylaxis in high cardiovascular risk subjects
5. Diabetic nephropathy
6. Scleroaderma crisis
Adverse effects :
1. Common side effects
Dry cough (10%) due to increase level of bradykinin
Rash, fever, altered taste
Hyperkalemia & hypotension
2. Angioedema : is rare but potentially threatening due to increase level of bradykinin
3. 1
st
dose syncope
4. Reversible renal failure in patient with severe bilateral renal artery stenosis
5. Fetotoxic & should not be used during pregnancy
Angiotensin II-receptor antagonists
The angiotensin II receptor blockers (ARBs).
Losartan, valsantan, candesartan, ebrosantan, ibresantan, olmesantan & telmisantan.
Pharmacological effects :
1. They produce arteriolar & venous dilation
2. They block aldosteron secretion & decrease Na & H2O retention
3. ARBs don't increase bradykinin level.
Uses :
In hypertensive diabetics (ARBs decrease nephrotoxicity of diabetes)
Side effects : - similar to those of ACEIs
-
The risks of cough & angioedema are significantly decreased
-
ABRs are also fetotoxic
Decrease
B.P
Renin inhibitors (Aliskiren)
Effects:
-
Aliskiren directly inhibits rinin & thus acts earlier in the RA.AS than ACEIs or ARBs.
-
It lower B.P & effective as ARBs, ACEIs, thiazides
-
It can be combined with diuretics , ACEIs, ARBs or CCB… etc
S/E :
-
Diarrhea at high dose
-
Cough & angioedema < ACEIs - Fetotoxic
Centrally acting adrenergic drugs
Alpha2 adrenoreceptor agonists
1. Clonidine
Therapeutic uses :
HPT that not respond to 2 or more drugs
HPT complicated by renal disease.
(Clonidine does not decrease renal blood flow or GFR
with diuretics : Clonidine (⇧ or ⇩ ) produce H2O & Na retention
Migraine prophylaxis, menopausal flashing, chorea with low dose & mimorale
Adverse effects:
-
Sedation
-
Dry nose
-
Rebound HPT following abrupt withdrawal of the drug. So the drug should be
withdrawal slowly.
Methyldopa
Therapeutic uses :
1. Hypertensive patients with renal insufficiency
2. Hypertensive pregnant patients (safety profile)
Adverse effects :
Sedation (frequent) lead to failure of male sexual function
Nightmares, depression, involuntary movements
Score or black tongue
Nausea, flatulence, constipation
Positive coomb's test with occasionally hemolytic anaemia, leucopenia,
thrombocytopenia
Hepatitis
Gynaccomastia & lactation due to interference with dopaminergic suprresion of
prolactin secretion
Vasodilators
(Direct acting smooth muscle relaxant)
Pharmacological actions :
1. Relaxant of vascular smooth muscle ⟶ VD ⟶ ⇩PR ⟶ ⇩ BP
2. Reflex stimulation of heart ⟶⇧heart rate & O2 consumption ⟶ +or - angina
pectoris, MI or heart failure ( in predisposes individuals )
3. ⇧Plasma rennin ⟶ Na
+
& H2O retention
Hydralazine
Direct vasodilator acting primary on arteries & arterioles ⟶ ⇩ PR ⟶ ⇩BP
Reflex ⟶ ⇧ HR & CO
Therapeutic uses :
1. Hypertension in pregnancy (lack of teratogenecity)
2. Moderately severe hypertension(always with B-blocker & diuretics)
Adverse effects :
-
Headache, tachycardia
-
Nausea, sweeting
-
Arrhythmia & precipitation of angina
-
A lupus-like syndrome can occur with ( huge dose or slow acetylators)
But it is reversible on discontinuation of the drug.
Minoxidil
This drug causes dilatation of resistance vessels. Arterioles but not venules
Therapeutic uses :
1. Orally : for treatment of severe to malignant HPT that is refractory to other drugs.
Reflex tachycardia & fluid retention may be severe & require the concomitant use of loop
diuretics & β blockers
2. Topically to treat man pattern baldness
S/E :
1. Serious Na & H2O retention ⟶ volume overload (edema & congestive heart failure)
2. Hypertrichosis (the growth of body hair)
Diazoxide
Its emergency use is obsolete because of excessive hypotension outweigh the benefit.
Three other vasodilator find a role outside hypertension :
1. Nicorandil : in angina
2. Papaverine : in male erectile dysfunction
3. Alprostadil :I.V for patency of ductus arteriosus
Hypertensive Emergency
The therapeutic goal to rapidly reduce B.P
a. Na nitroprusside
-
It is administered intravenously, it is poisonous if given orally because of its
hydrolysis to cyanide
-
It is light sensitive & should be protected from light
Pharmacological actions :
1. Reduce B.P in all patients regardless of the cause of HPT
2. Has little effect outside the vascular system
3. Acts equally on arterial (⇩P.R) & venous (preload) smooth muscle
-
It is metabolized rapidly (t
1/2
= minutes) & requires continuous infusion to maintain
its hypotensive action
Adverse effects :
1. Hypotension caused by overdose
2. Cyanide toxicity (rare) & treated by infusion of Nathiosulfate
Cyanide + Nathiosulfate ⟶ thiocyanate (less toxic & eliminated by kidneys)
a. Other drugs :
1. Labetolol (IV) α & β blockers
2. Nicardipine (IV) Ca channel blockers
3. Fenoldopam (IV) D
1
agonist
