Transplantation
&Graft Rejection
Lecture No. 4/2014; General Medicine
Prof. Dr. Zainalabideen A. Abdulla
MRCPI, DTM&H., Ph.D, FRCPath. (U.K.)
Transplantation and Graft Rejection
Transplantation provides the opportunity for definitive treatment of end-stage organ disease. The common solid organs transplanted are the kidney and the liver, and less frequently are the heart, lung, and pancreas. Bone marrow transplantation is also common(Figure 1).Aim of the lecture:
The most common transplantations (kidney, bone marrow and liver) are discussed from medical point of view.
Kidney transplantation
The major problem in transplantation is the shortage of organ donors. The organs are either: 1. cadaveric (previously healthy who experienced brain stem death, e.g. accident or cerebro-vascular events, and is more successful if C3F positive).2. living related donation (usually close relatives such as siblings).
Indications of renal transplants
Renal transplant is used for end-stage renal failure (ESRF) caused by:1. Diabetes mellitus
2. Glomerulonephritis
3. Renovascular disease/vasculitis
4. Pyelonephritis
5. Hypertension
6. Adult polycystic kidney disease (APKD)
Contra-indications to receiving a renal transplant
• Predicted patient survival of less than 5 years (e.g. malignancy, severe heart disease);- Age of patient >7o years or <1 year (relative).
2. Predicted risk of graft loss of > 50% at 1 year
3. Patients unable to comply with immuno-
suppressant therapy
4. Immunosuppression predicted to cause life-threatening complications (e.g. malignancy, or chronic viral infections)
5. Body mass index (BMI) is of >30
6. Patients with severe vascular access problems
Renal replacement therapy (dialysis or transplantation)
This can be predicted by:
1. Gum hypertrophy and other signs of immunosuuppression
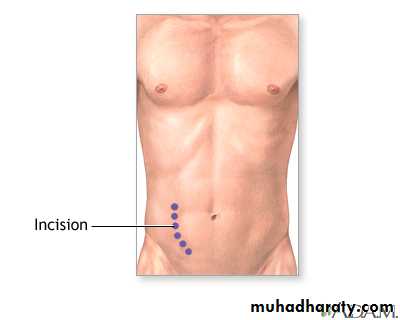
2. Scars including permacath scar (central venous, or right subclavian), peritoneal dialysis scar, and large iliac fossa scars
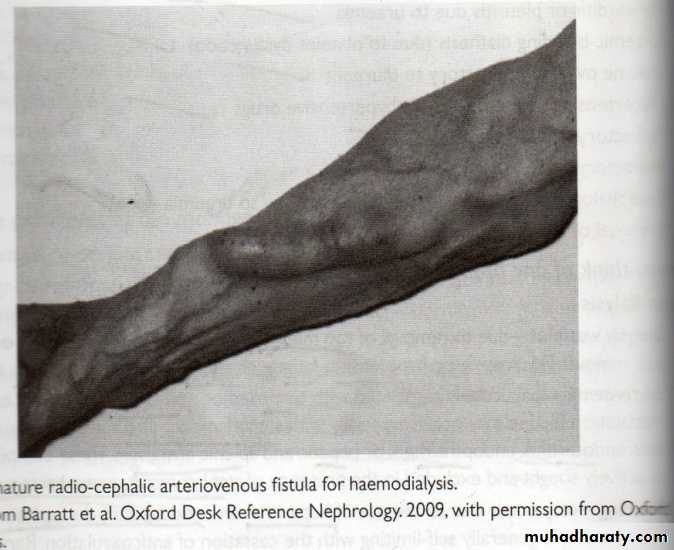
3. AV fistula (mainly forearm): Palpable thrill, Bruit (by Stethoscope Bell), and fresh needle marks (indicates the fistula is in use); Figure 3.
4. Medic alert necklace
5. Glucose testing pricks on fingers/lipohyper- or hypo-trophy (insulin use)
6. Facial lipoatrophy- suggests mesangio-capillary glomerulonephritis
7. Butterfly face indicating SLE
8. Nail dystrophy
9. Papilloma/warts
10. Ankle oedema
11. Parathyroid scars (hyperparathyroidism is common in chronic renal failure)
Examination of the abdomen in renal transplants
Multiple abdominal scars including large incisional scar (left, right or both; some-times called Ruiterford- Morrison incision- Figure 3). Still red/purple scars are implying recent surgery or steroid therapy.Look for a mass below the scar at the right/left iliac fossa in particular for:
1. Palpate the margins (often smooth)
2. Estimate the size (usually 8 cm X 5 cm)
3. Tender or non-tender
4. Consistency (often a firm mass)
5. Percuss over the mass (usually a dull percussion note)
Auscultate for bruits
Clues pointing towards a failing kidney transplant
1. Signs of fluid overload2. Hypertension
3. Tenderness over the graft
4. A tunneled line for haemodialysis
5. Signs of uraemia
6. Cushingoid features
Graft rejections in renal transplants
The most successful transplants are between monozygotic twins and between HLA very well-compatible (matched) donors and recipients. The types of rejections and their timing (occurrence) are:
Hyperacute (minutes to hours)
Acute vascular or cellular (5-30 days)
Chronic allograft failure (>30 days)
Hyperacute rejection
This is due to presence of pre-existing antibodies against the receipt HLA antigens causing thrombosis and tissue necrosis with bleeding. These antibodies can be detected by pre-transplantation cross-matching and so is very rarely seen in clinical practice nowadays. There is no treatment for it except the removal of the graft.Acute vascular rejection
This is vasculitis due to antibodies formed after transplantation and complement reactions (C4d positive in tissue staining).Acute cellular rejection
This is type IV hypersensitivity due to CD4 and CD8 reactions. The patient may have fever, pain and tenderness over the graft.
Immuno- suppression is required for prevention and treatment of these conditions. Plasmapheresis may be effective in physical removal of the antibodies.
Chronic allograft failure
This may be due to immunological mechanism or non-immunological ones such as hypertension, hyperlipidaemia and chronic drug toxicity.Immunosuppressive drugs (ISD)
Two or more (ISD) are used in synergistic combinations to minimize drug side effects in the prevention and treatment of these types of rejections (see Lecture 3).The main risks of using these agents are infections and malignancy.
The risk of infections is minimized by prophylactic use of medications (e.g. ganciclovir for CMV, cotrimoxazole for Pneumocystis) and immunization by killed vaccines. Malignancy may arise mainly due to failure of suppressed T-cells to control viral infection such as lymphoma (EBV virus), Kaposi’s sarcoma (human herpesvirus 8) or skin tumours (human papillomavirus) or anti-cancer surveillance mechanisms leading to lung, breast and colon cancers.
Bone marrow and peripheral blood stem cell transplantation
Blood and marrow transplantation (BMT) is the transplantation of haematopoietic stem cell and is of two types:
1. Allogeneic transplant
2. Autologus transplant
Allogeneic transplant
Stem cells are taken from the blood or bone marrow of HLA-identical siblings, or closely HLA-matched volunteer unrelated donor (VUD) to patients < 55 years of age (better < 20 years). The BMT is given to the patient (recipient) intravenously (home to bone marrow), after chemotherapy with or without radiotherapy that destroys malignant cells, immunosuppresses the recipient and ablating the haemotopietic tissues. Enough erythrocytes, granulocytes, and platelets are produced after 3-4 weeks of engraftment. The immune system of the recipient is boosted by infusion of T-cells taken from the donor, so called donor lymphocyte infusion (DLI). Long term immunosuppression by fludarabine (purine analogue given orally and I.V.) and cyclophosphamide is required in so called reduced-intensity BMT.Indications for allogeneic BMT
1. Acute myeloid leukaemia (AML)2. Chronic myeloid leukaemia (CML) resistant to imitanib (Mab)
3. Acute lymphoblastic leukaemia (ALL)
4. Severe aplastic anaemia
5. Myelofibrosis
6. Severe immunodeficiency syndromes
7. Myelodysplastic syndrom
Complications of allogeneic BMT
1. Mucositis2. Infections: Herpes simplex, bacterial, fungal, CMV, Varicella zoster, and Peumocystis jirovecii
3. Cataract
4. Pneumonitis
5. Infertility
6. Acute/chronic GvHD (the acute in first 100 days post-transplantation)
Autologus transplant
Stem cells are harvested from the blood or bone marrow of the same patient.
Indications to autologus BMT
1. AML
2. Myeloma
3. HD and high grade NHL
4. Mantle cell lymphoma
The outcome of autologous BMT is better than allogeneic BMT since it does not require immunosuppressant, with no risk of GvHD, quicker engraftment in 2-3 weeks, and mortality of about 5%.
Liver transplantation
It is the replacement of a diseased liver with a healthy liver from another person (orthotopic “same place” allograft). The surgery takes usually 5-6 hours (up to 18 hours).• Whole cadaveric liver
• Portion
Usually the right lobe of living donor liver transplant (LDLT)
which is very suitable for paediatrics liver transplant.
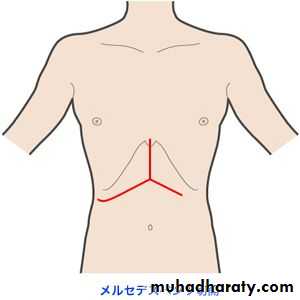
The abdomen shows what is called an inverted Mercedes-Benz
incision (Figure 4). Full liver functions are achieved in 4-6
weeks.
Post-transplantation immunosuppression is required using corticosteroids, plus calcineurin inhibitors (cyclosporin or tacrolimus) plus mycophenolate mofetil. Rejection episodes are experienced such as hyperacute (anti-recipient antibodies and complement), acute (T-cell mediated with cytokines), and chronic (after 1 year post-transplantation).
Indications of liver transplantation
1. Cirrhosis2. Hepatocellular carcinoma with:
- One lesion < 5 cm
- Up to 3 lesions < 3 cm
- No extra-hepatic manifestations
- No vascular invasion
These conditions are commonly the result of alcohol abuse, hepatitis C or hepatitis B infections. Stop drinking alcohol 6 months before transplantation is a must.