Sunday 8 / 3 / 2015
©Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
مكتب اشور لالستنساخ
ANTI-MICROBIAL DRUGS
Lecture 11
Total lectures NO. 43
Dr. Haidar Al-Shakarchi
Pharmacology
Anti-Microbial Drugs 5
1
Dr. Haidar Al-Shakarchi
Lec. 11
Macrolides:
Erythromycin was the 1
st
of macrolides to find clinical application, both as a drug
of choice and as an alternative to penicillin in individuals who are allergic to B-
lactam antibiotics. The newer members of this family are clarithromycin and
azithromycin. Telithromycin is the first ketolide that has been approved.
Mechanism of Action:
The macrolides bind irreversibly to a site on the 50s subunit of bacterial
ribosome, thus inhibiting the translocation steps of protein synthesis. They may
also interfere at other steps, such as transpeptidation. Generally considered to be
bacteriostatic, they may be bactericidal at higher doses. Their binding site is either
identical or in close proximity to that for clindamycin and chloramphenicol.
Antibiotic Spectrum:
1. Erythromycin: this drug is effective against many of the same organisms as
penicillin G. Erythromycin is effective against gram +ve organisms,
especially Staphylococci, Streptococci, Pneumococci and Corynebacteria.
Gram –ve organisms such as Neisseria species, bordetella and legionella are
susceptible. Spirochetes (Treponema pallidum), mycoplasma pneumoniae ,
Chlamydia pneumoniae and Chlamydia trachomatis are also susceptible.
2. Clarithromycin: this antibiotic has a spectrum of antibacterial activity
similar to that of Erythromycin, but:
a. It's also effective against Haemophilus influenzae.
b. It has a higher activity against Chlamydia, Legionella, Moraxella,
Ureaplasma species and Helicobacter pylori.
c. It's active against Mycobacterium-avium intracellular complex (MAC) in
AIDs patients with disseminated infections.
3. Azithromycin: Azithromycin and erythromycin are virtually identical with
respect to antimicrobial activity except that Azithromycin is:
a. Less active against streptococci and staphylococci.
Pharmacology
Anti-Microbial Drugs 5
2
Dr. Haidar Al-Shakarchi
Lec. 11
b. far more active against respiratory infections due to H. influenzae and
Moraxella catarrhalis.
c. the preferred therapy for urethritis caused by Chlamydia trachomatis.
d. active against mycobacterium avium intracellular complex (MAC) in
AIDs patients with disseminated infections.
4. Telithromycin: this drug has an antibacterial spectrum similar to that of
azithromycin.The structural modification within ketolides neutralizes the
most common resistance mechanisms that make macrolides ineffective.
Resistance:
Resistance to erythromycin became a serious clinical problem. Several
mechanisms have been identified: (1) the inability of the organism to take up the
antibiotic or the presence of an efflux pump, (2) a decreased affinity of the 50s
ribosomal subunit for the antibiotic (3) the presence of a plasmid associated
erythromycin esterase. Both clarithromycin and azithromycin show cross
resistance with erythromycin, but telithromycin can be effective against macrolide
resistant organisms.
Pharmacokinetics:
1. Administration:
The erythromycin base is destroyed by gastric acid, thus either enteric
coated tablets or esterified forms of the antibiotic are administrated.
Clarithromycin, azithromycin and telithromycin are stable to stomach acid
and are readily absorbed. Food interferes with the absorption of
erythromycin and azithromycin but can increase that of clarithromycin.
Azithromycin is available for IV infusion.
2. Distribution:
Erythromycin distributes well to all body fluids except the CSF. It's one of
the few antibiotics that diffuse into prostatic fluid and it has the unique
characteristics of accumulating in macrophages. Similarly, clarithromycin,
azithromycin and telithromycin are widely distributed in the tissues. Serum
levels of azithromycin are low; the drug is concentrated in neutrophils,

Pharmacology
Anti-Microbial Drugs 5
3
Dr. Haidar Al-Shakarchi
Lec. 11
macrophages and fibroblasts. Azithromycin has the longest half-life (>40
hours) and largest volume of distribution among the four drugs.
3. Fate:
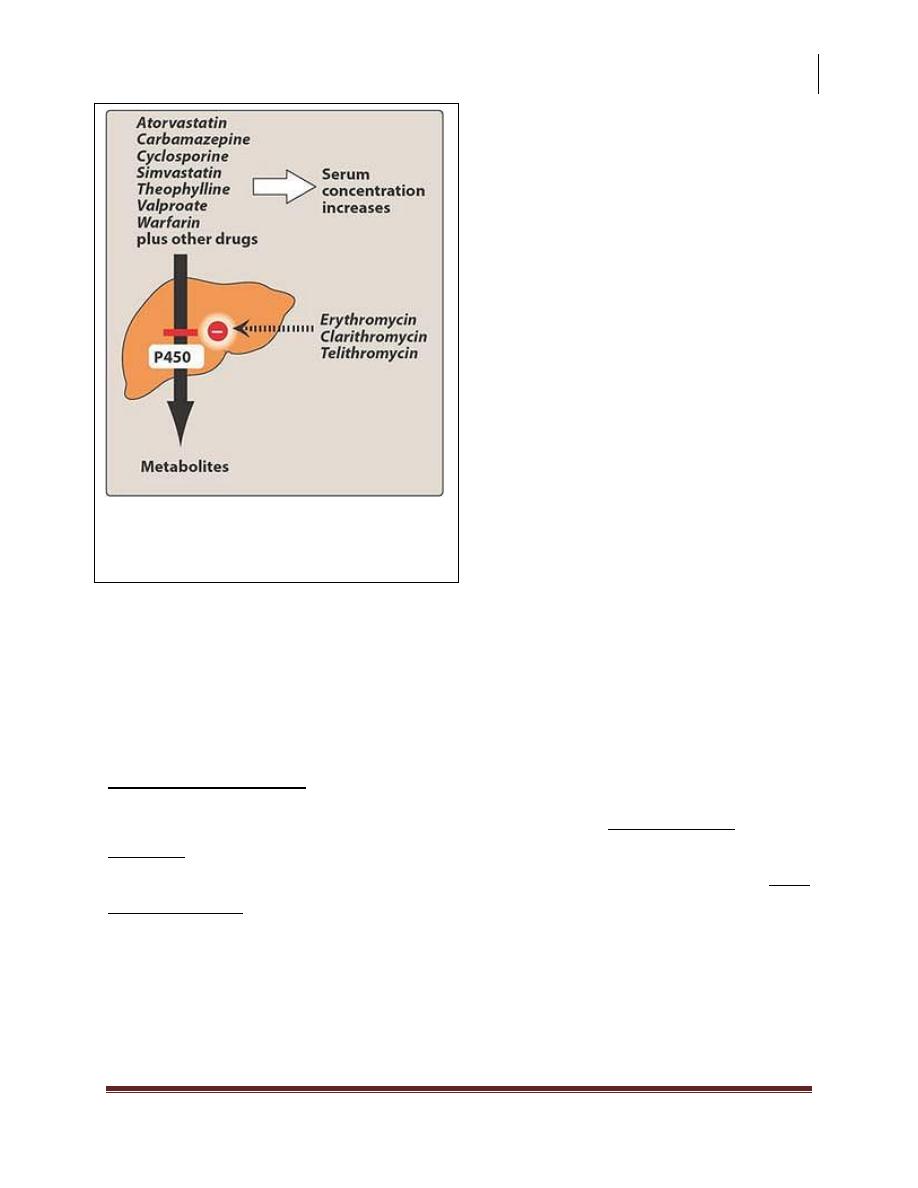
Erythromycin, clarithromycin and telithromycin are metabolized and are
known to inhibit the oxidation of a number of drugs through their interaction
with cytochrome p450 system.
4. Excretion:
Erythromycin and azithromycin are primarily concentrated and excreted in
an active form in the bile. Partial reabsorption occurs through the
enterohepatic circulation. Inactive metabolites are excreted in urine.
Adverse effects:
1. Epigastric Distress: this side effect is common and can lead to poor patient
compliance for erythromycin. Clarithromycin and azithromycin seem to be
better tolerated by the patient, but GIT problems are their most common
side effects.
2. Cholestatic jaundice: this side effect occurs especially with estolate form of
erythromycin, presumably as the result of a hypersensitivity reaction to the
estolate form.
3. Ototoxicity: transient deafness has been associated with erythromycin,
especially at high doses.
4. Contraindications: patients with hepatic dysfunction should be treated with
caution with erythromycin, azithromycin or telithromycin because these
drugs accumulate in the liver.
5. Interactions: Erythromycin, clarithromycin and telithromycin inhibit the
hepatic metabolism of some drugs which can lead to toxic accumulation of
these compounds e.g. astemizole, terfenadine, carbamazepine, valporate,
theophylline, warfarin and cyclosporine. An interaction with digoxin may
occur. In this case the antibiotic eliminates a species of intestinal flora that
ordinarily inactivates digoxin, thus leading to greater reabsorption of the
drug from the enterohepatic circulation. No interactions have been reported
for azithromycin.
Pharmacology
Anti-Microbial Drugs 5
4
Dr. Haidar Al-Shakarchi
Lec. 11
Chloramphenicol:
It's active against a wide range of gram +ve and gram –ve organisms. However,
because of its toxicity, its use is restricted to life-threatening infections for which
no alternatives exist.
Mechanism of Action:
The drug binds to the bacterial 50s ribosomal subunit and inhibits protein
synthesis at the peptidyl transferase reaction. Protein synthesis in mammalian
mitochondrial ribosome may be inhibited at high circulating levels, producing bone
marrow toxicity.
Inhibition of the cytochrome P450 system by
erythromycin,clarithromycin, and telithromycin.
Pharmacology
Anti-Microbial Drugs 5
5
Dr. Haidar Al-Shakarchi
Lec. 11
Antibacterial Spectrum:
Chloramphenicol, a broad spectrum antibiotic, is active not only against bacteria
but also against other microorganisms, such as rickettsiae. Pseudomonas
aeruginosa is not affected, nor are the Chlamydiae.
Chloramphenicol has excellent activity against anaerobes. The drug is either
bactericidal or (more commonly) bacteriostatic, depending on the organism.
Resistance:
1. Clinically significant resistance is due to production of chloramphenicol
acetyl transferase, a plasmid encoded enzyme that inactivates the drug.
2. Inability of the antibiotic to penetrate the organism.
Pharmacokinetics:
Chloramphenicol is completely absorbed via the oral route, widely distributed
throughout the body and readily enters the normal CSF. The drug inhibits the
hepatic cytochrome P450 system. Excretion of the drug depends on its conversion
in the liver to a glucuronide, which is then secreted by the renal tubule.
Chloramphenicol is also secreted into breast milk.
Adverse Effects:
The clinical use of chloramphenicol is limited to life-threatening infections
because of the serious adverse effects associated with its administration.
1. GIT upsets.
2. Overgrowth of Candida albicans may appear on mucous membrane.
3. Anemia:
a. Hemolytic anemia occurs in patients with low levels of glucose-6-
phosphate dehydrogenase.
b. Reversible anemia, which is apparently dose-related and occurs
concomitantly with therapy.
c. Aplastic anemia, which although rare is idiosyncratic and usually fatal.
It's independent of dose and may occur after therapy has been ceased.

Pharmacology
Anti-Microbial Drugs 5
6
Dr. Haidar Al-Shakarchi
Lec. 11
4. Gray Baby Syndrome: occurs in neonates if the dosage regimen of
chloramphenicol is not properly adjusted. Neonates have a low capacity to
glucuronylate the antibiotic and they've underdeveloped renal function. The
drug accumulates to the levels that interfere with the function of
mitochondrial ribosomes. This leads to depressed breathing, cardiovascular
collapse, cyanosis and death.
5. Interactions: Chloramphenicol inhibits some of the hepatic mixed-function
oxidase and thus blocks the metabolism of many drugs, thereby elevating
their concentration and potentiating their effects.
Clindamycin:
Clindamycin has a mechanism of action and resistance similar to those of
erythromycin. Clindamycin is employed primarily in the treatment of infections
caused by anaerobic bacteria, such as Bacteriodes fragilis, which often causes
abdominal infections associated with trauma. However, it's also significantly active
against non-enterococcal gram +ve cocci. It distributes well into all body fluids
except CSF. Penetration into bone occurs even in the absence of inflammation. The
most serious adverse effect is potentially fatal pseudomembranous colitis caused
by overgrowth of Clostridium difficile, which elaborates necrotizing toxins. Oral
administration of either metronidazole or vancomycin is usually effective in
controlling this serious problem.
Metronidazole is the drug of choice to treat pseudomembranous colitis.
Quinupristin/Daflopristin:
Quinupristin/Daflopristin is a mixture of 2 streptogramines. The drug is reserved
for the treatment of vancomycin resistant Enterococcus faecium (VRE). The
combination drug is bacteriostatic and has a long post antibiotic effect (PAE). It is
active primarily against gram-positive cocci.

Pharmacology
Anti-Microbial Drugs 5
7
Dr. Haidar Al-Shakarchi
Lec. 11
Adverse effects include venous irritation, arthralgia and hyperbilirubinemia.
Quinupristin/Dalfopristin inhibits cytochrome P450 isozyme.
Linezolid:
Linezolid was introduced recently to combat resistant gram +ve organisms, such
as methicillin and vancomycin resistant Staphylococcus aureus, vancomycin-
resistant Enterococcus faecium and Enterococcus faecelis, and penicillin-resistant
streptococci. Linezolid is completely absorbed on oral administration.It is well
tolerated, with some reports of GIT upset.
Done by
Ali Kareem
