Sunday 22 / 3 / 2015
©Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
مكتب اشور لالستنساخ
ANTI-PROTOZOAL DRUGS
Lecture 3
Total lectures NO. 47
Dr. Huda Al-Qadhi
2 |
P a g e
Chemotherapy for Malaria:
Life cycle of Malaria parasite:
An infected female anopheles mosquito injects sporozoites. Sporozoites migrate
to the liver, where they form merozoites. Merozoites are released and invade red
blood cells. In RBC, the merozoite becomes a trophozoite.The trophozoite
multiplies, producing new merozoites. These are released when the RBC ruptures,
and they can infect other RBCs. Some merozoites become gametocytes. The
female mosquito picks up gametocytes from an infected human. The sexual cycle
occurs in the mosquito, where sporozoites are formed.
Drug Classification:
1. Tissue Schizonticides: Drugs that eliminate developing or dormant liver
forms.
2. Blood Schizonticides: Drugs that act on erythrocytic parasites.
3. Gametocides: Drug that kill sexual stages and prevent transmission to
mosquitoes.
Radical Cure: Elimination of both hepatic and erythrocytic stages.
NOTE: No one available agent can reliably affect a radical cure.
Chloroquine:
Chloroquine is a synthetic 4-aminoquinoline formulated as the phosphate salt for
oral use.
Pharmacokinetics:
Chloroquine is a rapidly and completely absorbed following oral administration.
The drug concentrates in erythrocytes and some tissues. Thus it has a very large
apparent volume of distribution . The drug also penetrates into the CNS and
traverses the placenta. Chloroquine is dealkylated by the hepatic mixed function
oxidase system and is principally excreted in the urine.
Anti-Malarial Action:
3 |
P a g e
Chloroquine is a highly effective blood Schizonticide. It's also moderately
effective against gametocytes of P. vivax, P. ovale and P. malariae.
Chloroquine is not active against liver stage parasites.
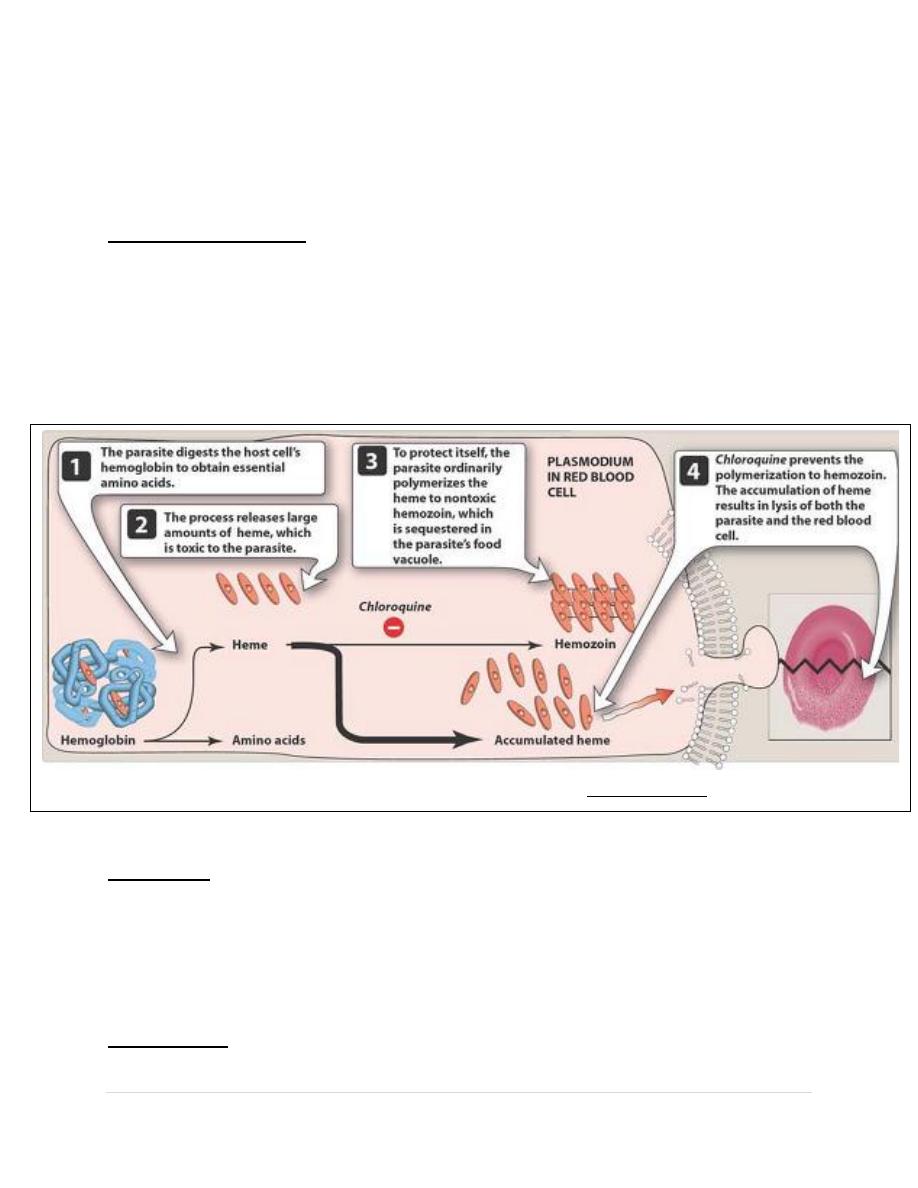
Mechanism of Action:
After traversing the erythrocytic and plasmodial membranes, Chloroquine is
concentrated in the organism's acidic food vacuoles. Chloroquine specifically
binds to heme released from the digestion of the host cells' hemoglobin, preventing
its polymerization to hemozin (a pigment). The increased pH and accumulation of
the toxic heme result in oxidative damage to the membranes, leading to lysis of
both the parasite and the RBC.
Resistance: Chloroquine resistant P. falciparum exhibit multigenic alternations
that confer a high level of resistance. When a chloroquine resistant organism is
encountered, therapy usually consists of an orally administrated combination of
quinine, pyrimethamine and a sulfonamide,such as sulfadoxine.
Clinical uses:
Action of chloroquine on the formation of hemozoin by Plasmodium species.
4 |
P a g e
1.
Chloroquine is the drug of choice for the treatment of non-falciparum and
sensitive falciparum malaria. It rapidly terminates fever (in 24-48 hours)
and clears parasitemia (in 48-72 hours).
2.
Chloroquine is the preferred chemo-prophylactic agent in malarious
regions without resistant falciparum malaria.
3.
Chloroquine may be used for amebic liver abscesses that fail initial therapy
with metronidazole.
4.
Chloroquine has been used successfully for its anti-inflammatory effect in
rheumatoid Arthritis. The following mechanisms have been proposed:
(1)
suppression of T-lymphocyte response to mitogens,
(2)
decreased leukocyte
chemotaxis,
(3)
stabilization of lysosomal enzymes,
(4)
inhibition of DNA and
RNA synthesis and
(5)
the trapping of free radicals.
Adverse Effects:
At high doses, some toxic effects occur such as gastro-intestinal upset, pruritis,
headache and blurred vision. Discoloration of the nail beds and mucous
membranes may be seen on chronic administration. Rare reactions include
hemolysis in G6PD deficient persons, seizures, agranulocytosis and ECG
changes. Patients with psoriasis or porphyria should not be treated with
chloroquine, because an acute attack may be provoked.Chloroquine is considered
safe in pregnancy.
Quinine
Quinine is derived from the bark of the cinchona tree. Quinidine is the
dextrorotatory stereoisomer of quinine. Taken orally, Quinine is well distributed
throughout the body and can reach the fetus.
Anti-Malarial Action:
Quinine is a rapidly acting, highly effective blood schizonticide. It's gametocidal
against P. vivax and P. ovale. It's NOT effective against liver stage parasites.
5 |
P a g e
Clinical uses:
1. Parenteral treatment of severe falciparum malaria. Quinine or quinidine
is the treatment of choice for severe falciparum malaria.
2. Oral treatment of falciparum malaria. Quinine is appropriate first line
therapy for uncomplicated falciparum malaria. Quinine is commonly used
with doxycycline to shorten quinine's duration of use and limit toxicity.
Mechanism of Action:
Quinine and quinidine interfere with heme polymerization resulting in the death
of the erythrocytic form of the plasmodial parasite.
Adverse Effects:
1. Cinchonism: A syndrome causing nausea, vomiting, tinnitus and vertigo is
the major adverse effect. These effects are reversible and are not considered
to be reasons for suspending therapy.
2. Positive Coombs test for hemolytic anemia. Quinine treatment should be
suspended.
3. Hemolysis with G6PD deficiency.
4. Potentiation of neuromuscular blocking agents and elevation of digoxin
levels.
Primaquine:
Primaquine is a synthetic 8-aminoquinoline. It's well absorbed on oral
administration and is not concentrated in tissues. It's rapidly oxidized to many
compounds.
Anti-Malarial Action:
1. Eradicates primary exoerythrocytic forms of P. falciparum and P. vivax.
2. Eradicates secondary exoerythrocytic forms of recurring malarias (P. vivax
and P. ovale). Primaquine is the only agent that can lead to radical cures of
6 |
P a g e
P. vivax and P. ovale malaria, which may remain in the liver after the
erythrocytic form of the disease is eliminated.
3. Destroys in the blood the gametocytic forms of all 4 plasmodia.
It is not effective against the erythrocytic stage of malaria.
Mechanism of Action:
Primaquine is a tissue schizonticide. Metabolites of it are believed to act as
oxidants that are responsible for the schizonticidal action as well as for the
hemolysis and methemoglobinemia encountered as toxicities.
Adverse Effects:
1. Drug induced hemolytic Anemia in patients with genetically low levels of
glucose 6 phosphate dehydrogenase.
2. Abdominal discomfort especially when administrated in combination with
chloroquine.
3. Occasional methemoglobinemia.
4. Rarely granulocytopenia and agranulocytosis.
Contraindications:
1) Patients should be tested for G6PD deficiency before primaquine is
prescripted. When the patient is deficient in G6PD, treatment strategies may
consist of (1) withholding therapy, (2) treating patients with standard dosing
for 14 days (3) treating with weekly primaquine for 8 weeks.
2) During pregnancy
Inhibitors of Folate synthesis:
7 |
P a g e
Pyrimethamine:
Pyrimethamine is adequately absorbed, bound to plasma proteins and has an
elimination half-life of about 3.5 days. It's extensively metabolized before
excretion. Fansidar is a fixed combination of the sulfonamide sulfadoxine and
pyrimethamine.
Anti-Malarial Action:
Pyrimethamine acts slowly against erythrocytic forms of susceptible strains of all
4 human malaria species. It also acts as a strong sporontocide in the mosquito's gut
when the mosquito ingests it with the blood of the human host. Thus it's a blood
Schizonticide and sporontocide.
Mechanism of Action:
Pyrimethamine inhibits plasmodial dihydrofolate reductase at much lower
concentrations than those needed to inhibit the mammalian enzyme. The inhibition
deprives the protozoan of tetrahydrofolate – a cofactor required in the de novo
synthesis of purines and pyrimidines and in the interconversion of certain amino
acids.
Clinical usese:
1. Fansidar is used to treat chloroquine –resistant falciparum malaria.
2. Fansidar is used as presumptive therapy of falciparum malaria.
3. Pyrimethamine, in combination with sulfadiazine is first line therapy for the
treatment of toxoplasmosis.
If megaloblastic anemia occurs with pyrimethamine treatment, it may be reversed
with Leucovorin.
Antibiotics:
Folate antagonists, sulfonamides, tetracycline, doxycycline, clindamycin and
azithromycin.
Mefloquine:

8 |
P a g e
Mefloquine is absorbed well after oral administration and concentrates in the liver
and the lung. It has a long half-life (17 days) because of its concentration in
various tissues. The drug undergoes extensive metabolism. Its major excretory
route is the feces.
Mefloquine appears to be promising as an effective single agent for suppressing
and curing infections caused by multi-drug resistant forms of P. falciparum.
Adverse reactions at high doses range from nausea, vomiting and dizziness to
disorientation, hallucinations, and depression.
Artemisinin:
It's available for the treatment of severe, multi-drug resistant P. falciparum
malaria. It's the only drug reliably effective against quinine-resistant strains.
Artemisinin-resistant P. falciparum has not yet been identified.
Artemisinin is very rapidly acting blood schizonticide against all human malaria
parasites.
The anti-malarial action of artemisinin involves the production of free radicals
within the plasmodial food vacuole, following cleavage of the drugs endoperoxide
bridge by heme iron in parasitized erythrocytes.
(End of lecture 8)
Treatment of Amebiasis
Amebiasis is an infection with Entamoeba histolytica.
9 |
P a g e
Classification of amebicidal drugs:
Therapeutic agents are classified as luminal, systemic or mixed (luminal
and systemic) amebicides according to the site where the drug is effective.
Luminal amebicides (diloxanide furoate, iodoquinol & paromomycin) act on
the parasite in the lumen of the bowel.
Whereas systemic amebicides (chloroquine, dehydroemetine & emetine) are
effective against amebas in the intestinal wall and liver.
Mixed amebicides (metronidazole) are effective against both the luminal &
systemic forms of the disease, although luminal concentrations are too low
for single drug treatment.
Treatment of Specific forms of Amebiasis:
1. Asymptomatic intestinal infection: asymptomatic carriers are treated with a
luminal amebicide.
2. Amebic colitis: metronidazole plus a luminal amebicide is the treatment of
choice for colitis & dysentery. Tetracycline & erythromycin are alternative drugs.
3. Extraintestinal infections: the treatment of choice of liver abscesses is
metronidazole plus a luminal amebicide. If initial therapy fails, then the addition
of chloroquine to a repeat course of metronidazole may be helpful.
Dehydroemetine and emetine are toxic alternative drugs.
Metronidazole:
Metronidazole, a nitroimidazole, is the drug of choice for the treatment of extra
luminal amebiasis. It kills trophozoites but not cysts of E. histolytica & effectively
eradicates intestinal & extra intestinal tissue infections.
Pharmacokinetics:
Oral Metronidazole is readily absorbed & permeates all tissues by simple
diffusion. The ½ life of the unchanged drug is 7.5 hours. Metabolism of the
10 |
P a g e
drug depends on hepatic oxidation by mixed function oxidase, followed by
glucuronylation. The drug accumulates in patients with severe hepatic
disease. The parent drug & its metabolites are excreted in the urine.
Mechanism of action:
Some anaerobic protozoa parasites (including amebas) possess electron
transport proteins that participate in metabolic electron removal reactions.
The nitro group of metronidazole is able to serve as an electron acceptor,
forming reduced cytotoxic compounds that bind to proteins & DNA
resulting in cell death.
Clinical uses:
1. Amebiasis: metronidazole is the mixed amebicide of choice for treating
amebic infections, it kills the E. histolytica trophozoites. Tinidazole, a
related nitroimidazole, appears to have similar activity & a better toxicity
profile.
2. Giardiasis: metronidazole is the treatment of choice for infections
caused by Giardia lamblia.
3. Trichomoniasis: metronidazole is the treatment of choice for infections
caused by Trichomonas vaginalis.
4. Anaerobic infections: metronidazole finds extensive use in the treatment
of infections caused by anaerobic cocci, anaerobic gram –ve bacilli
(for example, Bacteroides species) & anaerobic gram +ve bacilli
(clostridium difficile). Metronidazole is the drug of choice for the
treatment of pseudomembranous colitis caused by clostridium
difficile & is also effective in the treatment of brain abscesses caused
by these organisms.
Adverse effects:
1. Nausea, vomiting, epigastric distress & abdominal cramps.
2. An unpleasant metallic taste.

11 |
P a g e
3. Oral moniliasis, dysuria, dark urine.
4. Pancreatitis & CNS toxicity (ataxia, seizures,and paresthesias).
5. Disulfiram-like effect occurs if taken with alcohol.
6. Potentiation of coumarin-type anticoagulants.
Iodoquinol:
Iodoquinol, a halogenated hydroxyquinolone, is amebicidal against E. histolytica
& is effective against the luminal trophozoite & cyst forms but not against
trophozoites in the intestinal wall or extra intestinal tissues.
Side effects from iodoquinol include rash, diarrhea & dose-related peripheral
neuropathy, including a rare optic neuritis.
Diloxanide furoate:
Diloxanide furoate is useful in the treatment of asymptomatic shedders of cysts.
Its only indication is in the treatment on intestinal amebiasis. After oral
administration, diloxanide furoate is hydrolyzed in the intestinal mucosa, the
resulting free diloxanide is about 90% absorbed.However, the unabsorbed drug is
the active amebicide. Adverse effects are mild & include flatulence, dryness of the
mouth & pruritis. The drug is contraindicated in pregnant woman & children under
2 years of age.
Paromomycin:
Paromomycin, an aminoglycoside antibiotic, is only effective against intestinal
(luminal) forms of E. histolytica, because it is not significantly absorbed from the
GIT. Although directly amebicidal, paromomycin also exerts its antiamebic actions
by reducing the population of intestinal flora.
Chloroquine:

12 |
P a g e
Chloroquine is used in combination with metronidazole & diloxanide furoate to
treat & prevent amebic liver abscess
Emetine & dehydroemetine:
Emetine & dehydroemetine are effective against tissue trophozoites of E.
histolytica, but because of major toxicity concerns they’ve been almost completely
replaced by metronidazole. The drugs should be used to treat amebic dysentery or
amebic liver abscess for the minimum period needed to relieve severe symptoms
(usually 3-5 days). They should not be taken for more than 10 days.
The drugs inhibit protein synthesis by blocking chain elongation. Intramuscular
injection is the preferred route. Among the unwanted effects are pain at the site on
injection, cardiotoxicity, neuromuscular weakness & rashes.
CHEMOTHERAPY FOR LEISHMANIASIS:
There’re 3 types of leishmaniasis: cutaneous, mucocutaneous & visceral.
Pentavalent antimonials, such as sodium stibogluconate, are the conventional
therapy used in the treatment of leishmaniasis, with petamidine & amphotericin B
as backup agents. Allopurinol has also been reported to be effective.
Sodium stibogluconate :
The exact mechanism of action hasn’t been determined. Evidence for inhibition
of glycolysis in the parasite at the phosphofructokinase reaction has been found. It
has been proposed that reduction to the trivalent antimony compound is essential
for activity. Adverse effects include pain at the injection site, gastrointestinal
upsets & cardiac arrhythmias.
Anthelmintic DRUGS
1. Drugs for treatment of Nematodes:

13 |
P a g e
Mebendazole:
Mebendazole inhibits microtubule synthesis in nematodes thus irreversibly
impairing glucose uptake. Affected parasites are expelled with feces. Little of an
oral dose (that is chewed) is absorbed by the body, unless it is taken with a high fat
meal. It undergoes 1
st
pass metabolism to inactive compounds. It is the drug of
choice in the treatment of infections by:
1. Whipworm (Trichuris trichiura).
2. Pinworm (Enterobius vermicularis).
3. Hookworm (Ancylostoma duodenale).
4. Roundworm (Ascaris lumbricoides).
Patients may complain of abdominal pain &diarrhea.
Contraindications: pregnancy &children under 2 years.
Pyrantel pamoate:
Pyrantel pamoate is poorly absorbed orally & exerts its effects in the intestinal
tract. It acts as a depolarizing neuromuscular blocking agent, causing persistent
activation of the parasites nicotinic receptors. The paralyzed worm is then expelled
from the host’s intestinal tract.
Pyrantel pamoate is effective in the treatment of infections caused by
roundworms, pinworms &hookworms. Adverse effects are mild & include nausea,
vomiting & diarrhea.
Thiabendazole:
Thiabendazole is effective against (1) strongyloidiasis (2) cutaneous Larva
migrans.(3) trichinosis.
Thiabendazole affects microtubular aggregation. It’s readily absorbed on oral
administration & is hydroxylated in the liver & excreted in the urine. It may cause
erythema multiforme & Stevens Johnson syndrome.
Ivermectin:
Ivermectin is the drug of choice in the treatment of:
14 |
P a g e
1. Strongyloidiasis.
2. Cutaneous Larva migrans.
3. Onchocerciasis.
Ivermectin targets the parasite’s Cl channel receptors. Chloride influx is
enhanced & hyperpolarization occurs, resulting in paralysis. It is contraindicated in
pregnancy.
Diethylcarbamazine:
Diethylcarbamazine is used in the treatment of filariasis because of its ability to
immobilize microfilariae.
2. Drugs for the treatment of trematodes:
Praziquantel:
Praziquantel is rapidly absorbed after oral administration & distributes into the
CSF. High levels occur in the bile. The drug is extensively metabolized & excreted
through the urine & bile. Praziquantel appears to increase the permeability of
trematode & cestode cell membrane to calcium, resulting in paralysis,
dislodgement & death.
Clinical uses:
1. Schistosomiasis: praziquantel is the drug of choice of all forms of
schistosomiasis (S. haematobium, S. mansoni & S. japonicum).
2. Other trematodes infections e.g. clonorchiasis.
3. Taeniasis & diphyllobothriasis: praziquantel results in high cure rates for
T. saginata, T. solium & D. latum.
4. Neurocysticercosis: albendazole is now the preferred drug.
5. Hymenolepis nana: praziquantel is the drug of choice for H. nana
infections.
15 |
P a g e
Adverse effects: common adverse effects include drowsiness, dizziness & GIT
upsets. The drug is not recommended for pregnant women or nursing mothers.
Contraindications: ocular cysticercosis.
3. Drugs for the treatment of cestodes:
Niclosamide:
The action of niclosamide has been ascribed to inhibition of the parasite’s
mitochondrial anaerobic phosphorylation of ADP, which produces energy in the
form of ATP. The drug is lethal for the cestode’s scolex & segments of cestodes,
but not for the ova. A laxative is administered prior to oral administration of
niclosamide to purge the bowel of all the dead segments & so preclude digestion &
liberation of the ova, which may lead to cysticercosis.
Clinical uses:
(1)
T. saginata, T.solium & Diphyllobothrium latum
(2)
H. nana.
Albendazole:
Albendazole inhibits microtubule synthesis & glucose uptake in nematodes. It is
erratically absorbed after oral administration & undergoes extensive 1
st
pass
metabolism, including formation of sulfoxide, which is also active. Albendazole &
its metabolites are primarily excreted in the urine.
Therapeutic application:
1. Cysticercosis (caused by Taenia Solium larvae).
2. Hydatid disease ( caused by Echinococcus granulosis)
Treatment of hydatid disease (3 months) has a risk of hepatotoxicity &
rarely, agranulocytosis or pancytopenia.
The drug shouldn’t be given during pregnancy or to children under 2 years
of age.
Done by
Ali Kareem
