Sunday 15 / 3 / 2015
©Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
مكتب اشور لالستنساخ
ANTI-FUNGAL DRUGS
Lecture 8
Total lectures NO. 46
Dr. Mohammed Rashad
2
Antifungal Drugs
Dr.Mohammed Rashad
I.OVERVIEW
• Infectious diseases caused by fungi are called mycoses (chronic)
• Some are superficial and some involve the skin
• butfungi may also penetrate the skin, causing subcutaneous
infections.
• Thefungal infections that are most difficult to treat are the
systemic mycoses (life threatening).
• The fungal cell membrane contains ergosterol rather than the
cholesterol
II.DRUGS FOR SUBCUTANEOUS AND SYSTEMICMYCOTIC INFECTIONS
A.Amphotericin B
• In spite ofits toxic potential, amphotericin B is the drug of choice
for the treatment of life-threatening systemic mycoses.
1. Mechanism of action:
• binds to ergosterol in the plasma
• they form pores (channels) disrupt membrane allowing
electrolytes to leak from the cell, resulting in cell death.
2. Antifungal spectrum:
• Amphotericin B is either fungicidal or fungistatic
• It is effective for Candida, Histoplasma, Cryptococcus,Coccidioides,
Blastomyces, and Aspergillus.
• Amphotericin B is also used in the treatment of leishmaniasis.
3
3. Resistance:
• is associated with decreased ergosterol
4. Pharmacokinetics:
• intravenous (IV) infusion.
• AMPHOTEC, ABELCET, and AMBISOME. These liposomal
preparations reduced renal and infusion toxicity.
• Amphotericin B is extensively bound to plasma proteins and is
distributed throughout the body.
5. Adverse effects:
• Amphotericin B has a low therapeutic index.
• Small test doses to assess the negative responses, such
asanaphylaxis or convulsions.
• Fever and chills: usually subsidewith repeated administration of
the drug.
• Renal impairment: Creatinine clearance can drop.
• Hypotension: shock-like,hypokalemia.
• Anemia: a reversible suppression of erythrocyte production.
• Neurologic effects: Intrathecal administration can cause serious
neurologic problems.
• Thrombophlebitis: Adding heparin to alleviate this problem.
B. Flucytosine
1. Mechanism of action
• 5-FC is converted to 5-fluorodeoxyuridine.
4
• This false nucleotide inhibits thymidylate,an essential DNA
component.
2. Antifungal spectrum:
• 5-FC is fungistatic.
• It is effective in combination with itraconazole for treating
chromoblastomycosis and in combination with amphotericin B for
treating candidiasis and cryptococcosis.
3. Pharmacokinetics:
• oral route and penetrates well into the CSF,Excretion by
glomerular filtration.
4. Adverse effects:
• reversible neutropenia, thrombocytopenia, and dose-related bone
marrow depression.
• Reversible hepatic dysfunction with elevation of serum
transaminases and alkaline phosphatase.
• Gastrointestinal disturbances and severe enterocolitis.
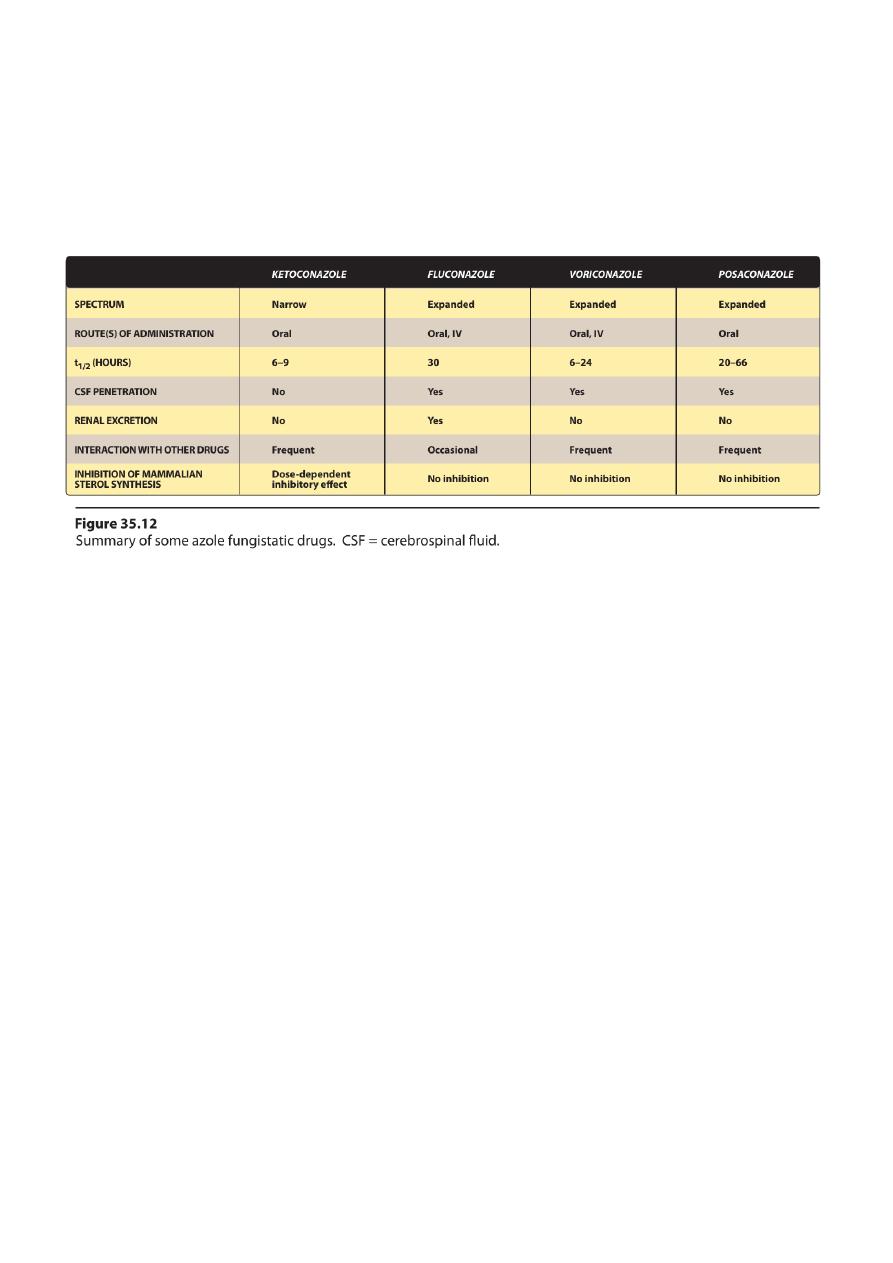
C. Ketoconazole
Ketoconazole was the first orally active azole available for the treatment
of systemic mycoses.
1. Mechanism of action:
• Azoles are predominantly fungistatic.
• They inhibit cytochrome P450 enzyme,thereby blocking the
demethylation of lanosterol to ergosterol.
• This inhibition disrupts membrane structure and function, which,
in turn, inhibits fungal cell growth.

5
• The drug also inhibits human gonadal and adrenal steroid
synthesis, leading to decreased testosterone and cortisol
production.
2. Antifungal spectrum:
• Oral ketoconazole is active against many fungi,including
Histoplasma, Blastomyces, Candida, and Coccidioides, but not
aspergillus species.
• Itraconazole has largely replaced ketoconazole in the treatment of
most mycoses because of: 1) its broader spectrum, 2)greater
potency, and 3) fewer adverse effects.
• Topical ketoconazole is used to treat tinea corporis, tinea cruris,
and tineapedis.
• Also, topical ketoconazole is used to treat tinea
versicolor,cutaneous candidiasis.
• It is also used topically in the treatment of seborrheic dermatitis
and dandruff.
3. Pharmacokinetics:
• ketoconazole requires gastric acid for dissolution and is absorbed
through the intestinal mucosa.
• Ketoconazole is extensively bound to plasma proteins.
• Extensive metabolism occurs in the liver, and excretion is primarily
through the bile.
4. Adverse effects:
• Allergies
• dose-dependent gastrointestinal disturbances are the most
• Endocrine effects, gynecomastia, decreased libido, impotence,
and menstrual irregularities, result from the blocking of androgen
and adrenal steroid synthesis.
6
• Frank hepatitis occurs rarely, but requires immediate cessation.
5.Drug interactions and contraindications:
• By inhibiting CYP450,ketoconazole can potentiate the toxicities of
drugs such a scyclosporine.
• Rifampin, an inducer of the CYP450 system, can shorten the
duration of action of ketoconazole.
• Drugs that decrease gastric acidity, such as H2-receptor blockers,
antacids, and proton-pump inhibitors, can decrease absorption of
ketoconazole.
• Finally, ketoconazole is teratogenic in animals, and it should not
be given during pregnancy.
D. Fluconazole
• It is clinically important because of its:
• lack of the endocrine side effects of ketoconazole
• excellent penetrability into theCSF
• Fluconazole is employed prophylactically in bone marrow
transplants
• The drug of choice for Cryptococcus for most candidemias, and for
coccidioidomycosis.
• Fluconazoleis effective against most forms of mucocutaneous
candidiasis.
• For the treatment of vaginal candidiasis, the dose is 150 mg as a
singleoral dose.
• The adverse effects: Nausea, vomiting, and rashes are a problem.
• There is a caution for patients with liver dysfunction.
7
• Fluconazole is teratogenic, and should not be used in pregnancy.
E. Itraconazole
• Itraconazoleis an antifungal agent with a broad antifungal
spectrum.
• Like fluconazole, it is a synthetic triazole and also lacks the
endocrinologic side effects of ketoconazole.
• Itraconazole is the drug of choice for the treatment of
blastomycosis, sporotrichosis, paracoccidioidomycosis, and
histoplasmosis.
• Itraconazole is well absorbed orally, but it requires acid for
dissolution.
• Adverse effects include nausea and vomiting, rash, hypokalemia,
hypertension,edema, and headache.
• Itraconazole should be avoided in pregnancy.
• The capsules should not be taken by patients with evidence of
ventricular dysfunction.
F. Voriconazole
• Voriconazole, a triazole, has the advantage of being a broad-
spectrum antifungal agent.
• It is available for both IV and oral administration and is
approximately 96 percent bioavailable.
• Voriconazole is approved for the treatment of invasive
aspergillosis and has replaced amphotericin B
• Voriconazole is also approved for treatment of serious infections.
• Side effects are similar to those of the other azoles.
8
• High trough concentrations are associated with visual and
auditory hallucinations.
G. Posaconazole
• It was approved in 2006 to prevent Candida and Aspergillus
infections.
• posaconazoleis used in the treatment of Mucor species and other
zygomycetes.
• Todate, amphotericin B formulations are the only other antifungal
agents available for treatment of zygomycete infections.
• The most common side effects are gastrointestinal issues (nausea,
vomiting, diarrhea, and abdominal pain) and headaches.
• Rare cases of hemolytic uremic syndrome, thrombotic
thrombocytopenic purpura, and pulmonary embolus.
• To be effective,posaconazole must be administered with a high fat
meal.
H. Echinocandins
• Echinocandins interfere with the synthesis of the fungal cell wall,
leading to lysis and cell death.
• Caspofungin, micafungin, and anidulafungin are available for IV
adminstration once daily.
1. Caspofungin:
• Caspofungin has activity against Aspergillus and most Candida
species resistant to azoles.
• Adverse effects include fever,rash, nausea, and phlebitis. Flushing
occurs.
9
• The dose of caspofungindoes not need to be adjusted in renal
impairment but is warranted with moderate hepatic dysfunction
• Caspofungin is a second-line antifungal for those who have failed
or cannot tolerate amphotericin B or an azole.
2. Micafungin and anidulafungin:
• Micafungin and anidulafungin have similar efficacy against
Candida species.
• The dose does not need to be adjusted in renal impairment or
mild-to-moderate hepatic dysfunction.
• they are not substrates for CYP450 enzymes and do not have any
associated drug interactions.
III. DRUGS FOR CUTANEOUS MYCOTIC INFECTIONS
A.Squaleneepoxidase inhibitors
These agents act by inhibiting squaleneepoxidase, resulting in the
blocking of ergosterol.
1. Terbinafine:
• Oral terbinafine is the drug of choice for treating
dermatophytoses and, especially, onychomycoses (fungal
infections of nails).
• It is 1)better tolerated, 2)requires shorter duration of therapy, and
3)is more effective than either itraconazole or griseofulvin.
a. Mechanism of action:
• Terbinafine inhibits fungal squaleneepoxidase, decreasing the
synthesis of ergosterol.
• This plus the accumulation of toxic amounts of squalene result in
the death of the fungal cell.

01
b. Antifungal spectrum:
• Topical terbinafine is active against Trichophyton.
• It
• Topical terbinafine 1% cream and solution are used to treat
tineapedis, tineacorporis, and tineacruris.
• Therapy is prolonged(usually about 3 months) but considerably
shorter than that with griseofulvin.
c. Pharmacokinetics:
• Terbinafine is available for oral and topical administration
• Terbinafine is deposited in the skin, nails, and fat.
• Terbinafine accumulates in breast milk.
• A prolonged terminal half-life of 200 to400 hours may reflect the
slow release from these tissues.
d. Adverse effects:
• The most common are gastrointestinal disturbances, headache,
and rash.
• Taste and visual disturbanceshave been reported.
• Rarelyterbinafine may cause hepatotoxicity and neutropenia.
2. Naftifine:
• Naftifine is active against Trichophyton and Epidermophyton.
• Naftifine 1% cream and gel is used for topical treatment of
tineacorporis, tineacruris, and tineapedis.

00
3. Butenafine:
• Butenafine is active against Trichophyton, Epidermophyton, and
Malassezia.
• Butenafine 1% cream is used for topical treatment of
tineacorporis,tineacruris, interdigital tineapedis, and
tineaversicolor.
4. Griseofulvin
• Griseofulvin has been largely replaced by oral terbinafine for the
treatment of dermatophytic infections of the nails,although it is
still used for ringworm and dermatophytosis of the skin and hair.
• Griseofulvin requires treatment of 6 to 12 months in duration.
• Griseofulvin accumulates in newly synthesized, keratin-containing
tissue, where it causes disruption of the mitotic spindle and
inhibition of fungal mitosis
• absorption is enhanced by high-fat meals
• Griseofulvin induces hepatic CYP450 activity.
5. Nystatin
• Nystatinis a polyene antibiotic
• mechanism of action, and resistance profile resemble those of
amphotericin B.
• Its use is restricted to topical treatment of Candida infections
because of its systemic toxicity.
• The drug is negligibly absorbed from the gastrointestinal tract, and
it is never used parenterally.
• It is administered as an oral agent (“swish and swallow” or “swish
and spit”) for the topical treatment of oral candidiasis.
6. Imidazoles

02
• butoconazole, clotrimazole, econazole, ketoconazole, miconazole
• As a class of topical agents, they have a wide range ofactivity
against Epidermophyton, Microsporum, Trichophyton, Candida
albicans, and Malassezia furfur
• Topical use is associated with contact dermatitis, vulvar irritation,
and edema.
• No significant difference in clinical outcomes is associated with
any azole or nystatin in the treatment of vulvar candidiasis.
7. Ciclopirox
• Ciclopirox inhibits the transport of essential elements in the fungal
cell
• Ciclopirox is active against Trichophyton, Epidermophyton,
Microsporum,Candida albicans, and Malassezia.
• Ciclopirox 1% shampoo is used for treatment of seborrheic
dermatitis.
• Ciclopirox 0.77% gel is used for treatment of interdigital
tineapedis, tineacorporis, and seborrheic dermatitis.
• Ciclopirox 8% solution is used for treatment of onychomycosis of
nails.
• Ciclopirox 0.77% cream and suspension is used for treatment of
dermatomycosis, candidiasis, and tineaversicolor.
8. Tolnaftate
• Tolnaftate distorts the hyphae and stunts mycelia growth in
susceptible fungi.
• Tolnaftate is active against Epidermophyton,Microsporum, and
Malassezia furfur. [Note: Tolnaftate is not effective against
Candida.]
03
• Tolnaftate is used to treat tineapedis, tineacruris, and
tineacorporis.
• It is available as a 1% solution, cream, and powder.
Done by
Ali Kareem
