Sunday 15 / 2 / 2015
©Ali Kareem 2014-2015
Name
:
______________________________
Class
:
_______________________________
مكتب اشور لالستنساخ
ANTI-PSYCHOTIC DRUGS
Lecture 6
Total lectures NO. 36
Dr. Naseer Al-Harchan

2
Antipsychotics
Schizophrenia
Etiology
Exact etiology unknown
Genetic predisposition
Intrauterine, birth or postnatal complications
Viral CNS infections
Environmental stressors (biochemical or social)
No evidence of association with poor parenting
Pathophysiology
No consistent neuropathology or biomarkers for schizophrenia
Increased dopamine in mesolimbic pathways causes delusions and
hallucinations
Dopamine deficiency in mesocortical and nigrostriatal pathways
causes negative symptoms (apathy, withdrawal)
Hallocinogens produce effect through action on 5-HT2 receptors
Antipsychotics
Typical / Conventional antipsychotics
Atypical antipsychotics
3
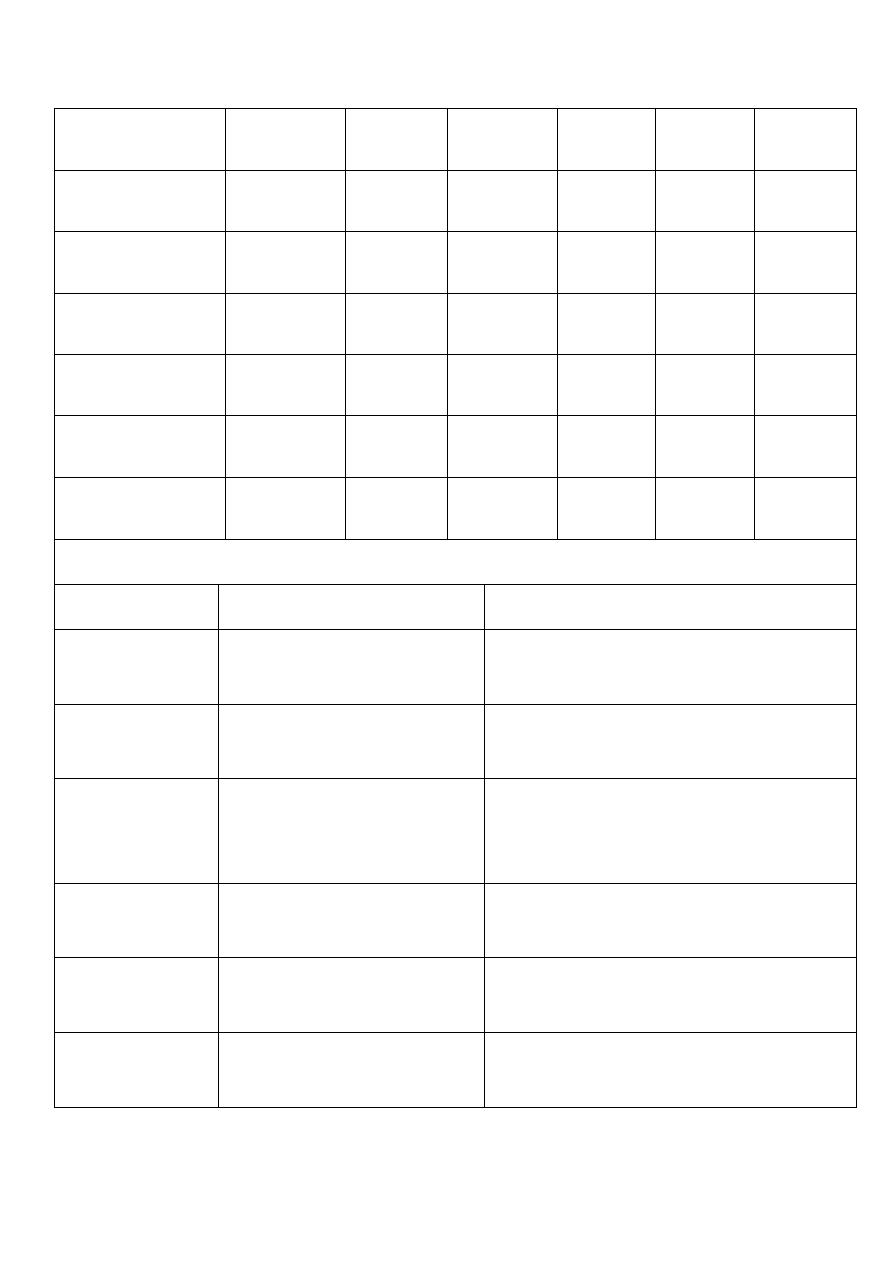
Typical / conventional antipsychotics
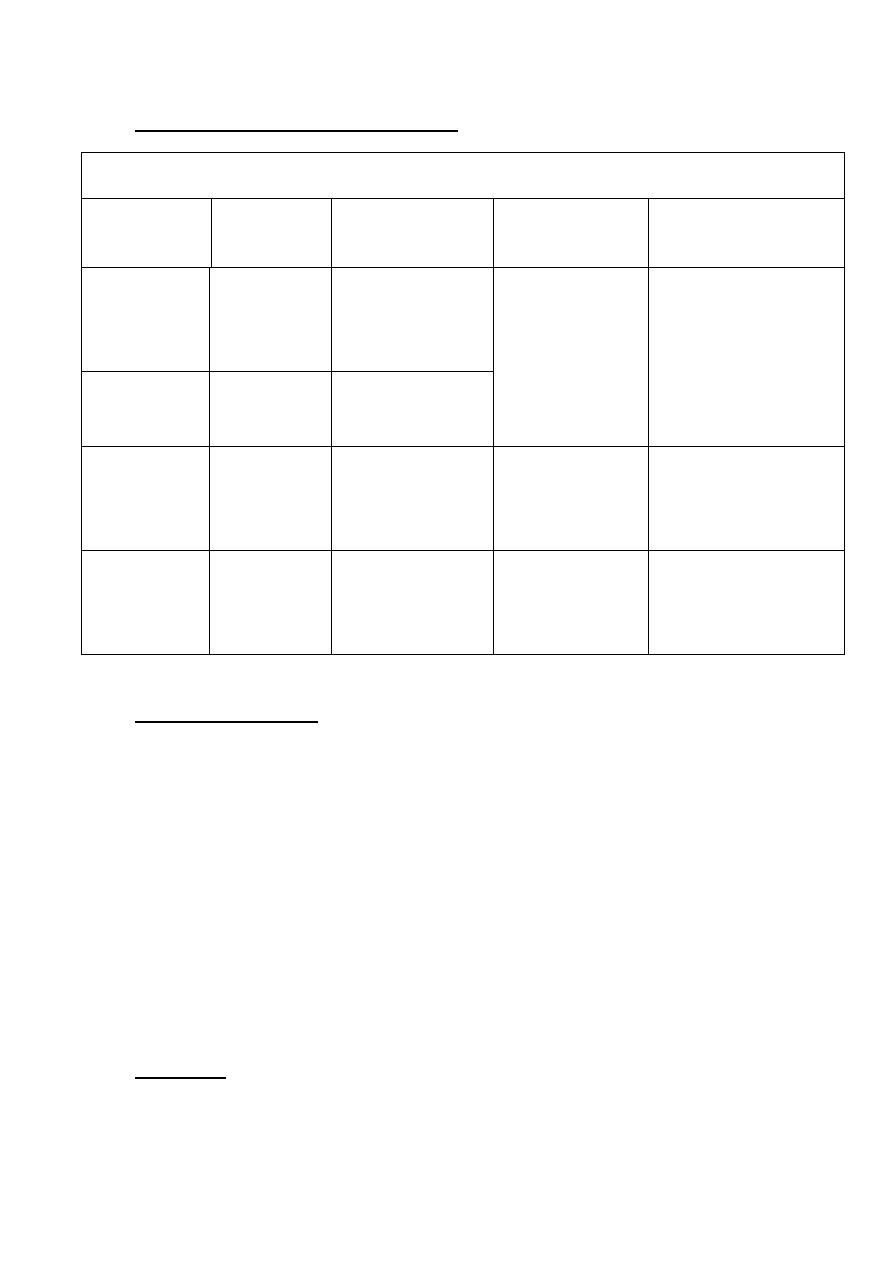
Dopamine receptors in various tracks
Track
Origin
Innervations
Function
Antipsychotic effect
Mesolimbic
Midbrain,V
entral
tegmental
Limbic structure,
nucleus
accumbens
Emotional and
intellectual
Hallucinations,
deulsions,
disordered cognition
Mesocortical Ventral
tegmental
Frontal cortex
Nigrostriatal Substantia
nigra
Basal ganglia
Extrapyramidal
system
movement
Motor
symptomatology
Tubero-
infundubular
Hypothalam
us
Pituitary gland
Regulate
endocrine
functions
Plasma prolactin
levels
Mechanism of action
Blocks receptors for dopamine, acetylcholine, histamine and
norepinephrine
Current theory suggests dopamine2 (D2) receptors suppresses
psychotic symptoms
All typical antipsychotics block D2 receptors
Close correlation between clinical potency and potency as D2
receptor antagonists
Properties
Effective in reducing positive symptoms during acute episodes and in
preventing their reoccurrence
4
Less effective in treating negative symptoms
Some concern that they may exacerbate negative symptoms by
causing akinesia
Higher incidence of EPS / sedation / anticholinergic Adverse effects
Potency
All have same ability to relieve symptoms of psychosis
Differ from one another in terms of potency
i.e. size of dose to achieve a given response
When administered in therapeutically equivalent doses, all drugs
elicit equivalent antipsychotic response
Low potency
Chlorpromazine, thioridazine
Medium potency
Perphenazine
High potency
Trifluoperazine, thiothixene, fluphenazine, haloperidol, pimozide
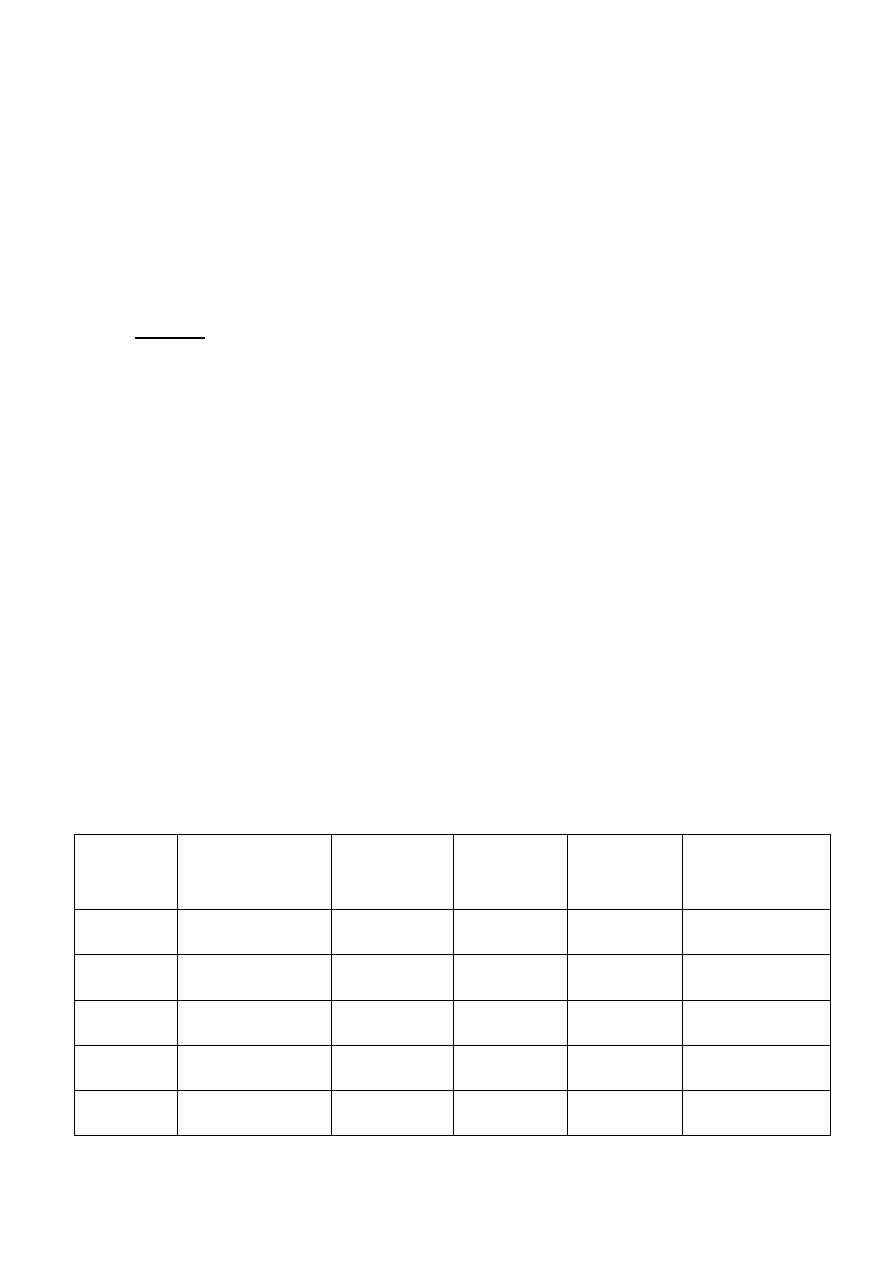
Potency
Drug
Equiv oral
dose (mg)
EPS
Sedation
Anticholinergic
s/e
Low
Chlorpromazine 100
Moderate
High
Moderate
Pericyazine
NA
Low
High
Low
Thioridazine
100
Low
High
High
Moderate Perphenazine
10
Moderate
Moderate
Low
High
Trifluoperazine 5
High
Low
Low
5
Thiotheixene
2
High
Low
Low
Fluphenazine
2
High
Low
Low
Haloperidol
2
High
Low
Low
Pimozide
0.5
High
Moderate
Moderate
Sulpiride
200
Low
Moderate
Low
Comparison of representative antipsychotics
Drug
Advantages
Disadvantages
Chlorpromazine
Generic, inexpensive
Many adverse
effects (esp.
autonomic)
Thioridazine
Slight EPS, generic
Cardiotoxicity (QT
prolongation)
Fluphenazine
Generic, depot available
(?) increased
tardive dyskinesia
Thiothixene
(?) decreased tardive dyskinesia
Uncertain
Haloperidol
Generic, injection and depot A/V,
few autonomic s/e
Prominent EPS
Receptor blockade and Adverse effects
Receptor type
Consequence of blockade
D2 dopaminergic
Extrapyramidal symptoms; prolactin release
6
H1 histaminergic
Sedation
Muscarinic cholinergic
Dry mouth, blurred vision, urinary retention,
constipation, tachycardia
Alpha1-adrenergic
Orthostatic hypotension; reflex tachycardia
5-HT2 serotonergic
Weight gain
Adverse effects
Extrapyramidal symptoms (EPS)
Early reactions – can be managed with drugs
Acute dystonia
Parkinsonism
Akathisia
Late reaction – drug treatment unsatisfactory
Tardive dyskinesia (TD)
Early reactions occur less frequently with low potency
drugs
Risk of TD is equal with all agents
Acute dystonia
Develops within a few hours to 5 days after first dose
Muscle spasm of tongue, face, neck and back
Oculogyric crisis (involuntary upward deviation of
eyeballs)

7
Opisthotonus (tetanic spasm of back muscles, causing
trunk to arch forward, while head and lower limbs are
thrust backwards)
Laryngeal dystonia can impair respiration
Management
Anticholinergics (Benztropine,
diphenhydramine IM/IV)
Lower or split dosing
Switch agent
Add scheduled benztropine / diphenhydramine
with antipsychotic
Parkinsonism (neuroleptic induced)
Occurs within first month of therapy
Bradykinesia, mask-like facies, drooling, tremor,
rigidity, shuffling gait, cogwheeling, stooped posture
Shares same symptoms with Parkinson’s disease
Management
Centrally acting anticholinergics (scheduled
benztropine / diphenhydramine / benzhexol
with antipsychotics) and amantadine
Avoid levodopa as it may counteract
antipsychotic effects
Switch to atypical antipsychotics for severe
symptoms
Akathisia
Develop within first 2 months of therapy

8
Compulsive, restless movement
Symptoms of anxiety, agitation
Management
Beta blockers (propranolol)
Benzodiazepines (e.g. lorazepam)
Anticholinergics (e.g. benztropine, benzhexol)
Reduce antipsychotic dosage or switch to low
potency agent
Tardive dyskinesia (TD)
Develops months to years after therapy
Involuntary choreoathetoid (twisting, writhing,
worm-like) movements of tongue and face
Can interfere with chewing, swallowing and speaking
Symptoms are usually irreversible
Management
Some manufacturers suggest drug withdrawal
at earliest signs of TD (fine vermicular
movements of tongue) may halt its full
development
Gradual drug withdrawal (to avoid dyskinesia)
Use lowest effective dose
Atypical antypsychotic for mild TD
Clozapine for severe, distressing TD
Inconsistent results with
Diazepam, clonazepam, valproate

9
Propranolol, clonidine
Vitamin E
Other Adverse effects
Neuroleptic malignant syndrome (NMS)
Rare but serious reaction, 0.2% of patients on
neuroleptics
High fever, autonomic instability, mental status
changes, leaden rigidity, elevated CK, WBC,
myoglobinuria
Management
Discontinue antipsychotic
Paracetamol for hyperthermia
IV fluids for hydration
Benzodiazepines for anxiety
Dantrolene for rigidity and hyperthermia
Bromocriptine for CNS toxicity
After symptom resolution
Some suggest to wait for at least 2 weeks
before resuming
Use lowest effective dose
Avoid high potency agents
Consider atypical antipsychotics

01
However, NMS has been reported from
patients taking clozapine, risperidone,
olanzapine and quetiapine
Prolactinemia
D2 receptor blockade decreases dopamine inhibition
of prolactin
Results in galactorrhea, amenorrhea, loss of libido
Managed with bromocriptine
Sedation
Administer once daily at bedtime
Seizures
Haloperidol has a lower risk of seizures
Anticonvulsants (beware or possible interaction with
antipsychotic)
Atypical antipsychotics
Refers to newer agents
Also known as
“Serotonin-dopamine antagonists”
Postsynaptic effects at 5-HT2A and D2 receptors
Mechanism of action
Similar blocking effect on D2 receptors
Seem to be a little more selective, targeting the intended
pathway to a larger degree than the others

00
Also block or partially block serotonin receptors
(particularly 5HT2A, C and 5HT1A receptors)
Aripiprazole: dopamine partial agonist (novel mechanism)
Properties
Available evidence to show advantage for some (clozapine,
risperidone, olanzapine) but not all atypicals when
compared with typicals
At least as effective as typicals for positive symptoms
May be more efficacious for negative and cognitive
symptoms (still under debate)
Less frequently associated with EPS
More risk of weight gain, new onset diabetes,
hyperlipidemia
Novel agents, more expensive
Potency
All atypical antipsychotics are equally effective at
therapeutic doses
Except clozapine
Most effective antipsychotic
For resistant schizophrenia
2
nd
line due to life-threatening side effect
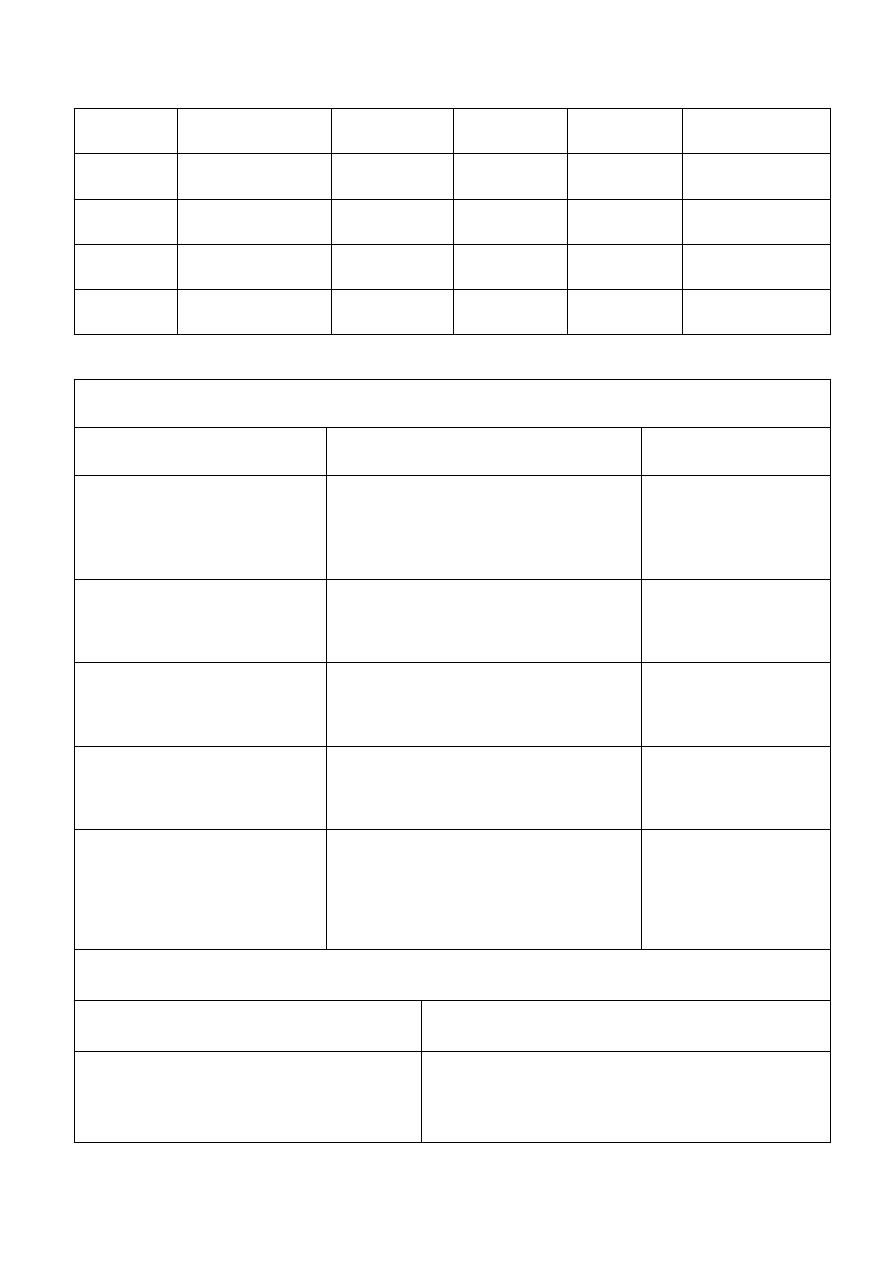
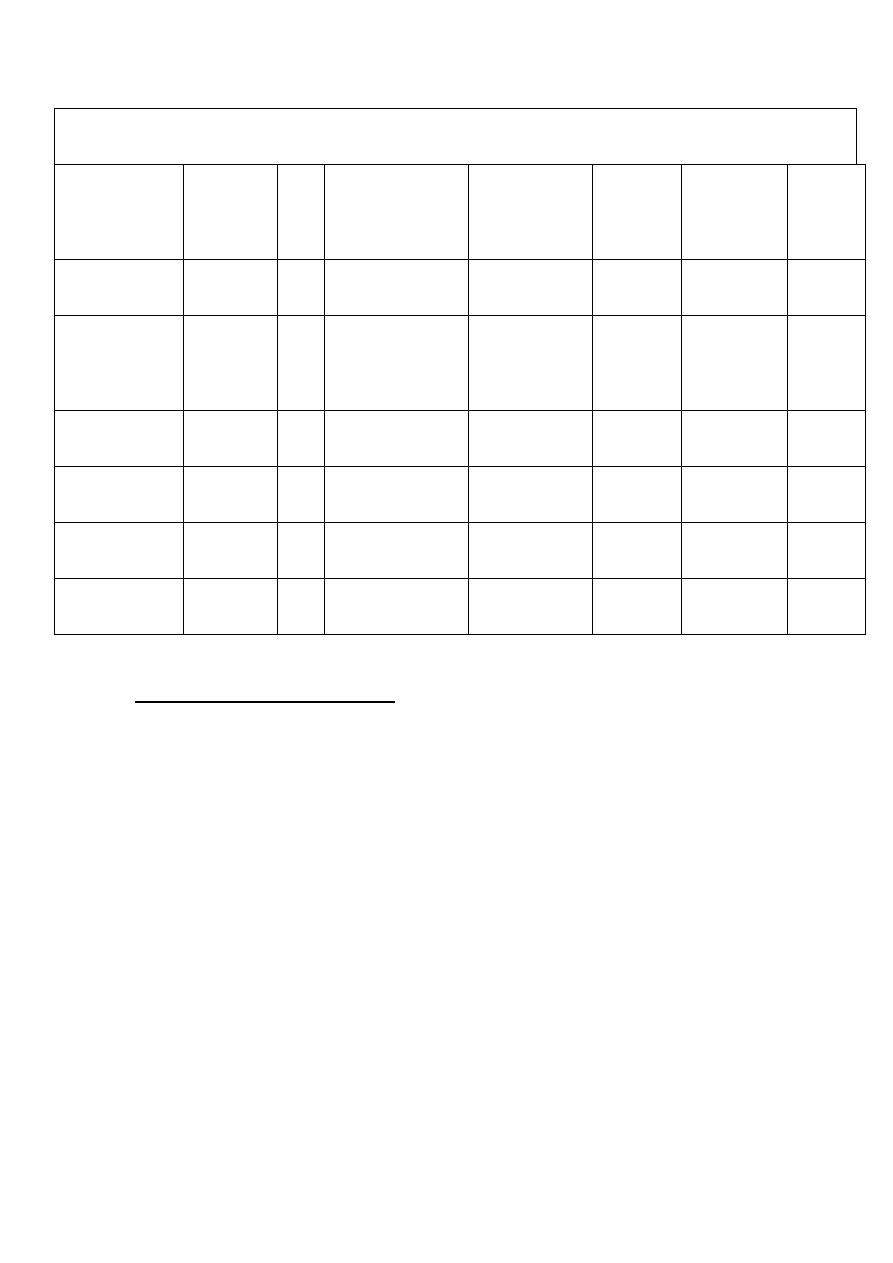
Relative receptor-binding of atypical antipsychotics
02
Drug
D1
D2
5-HT2
1
M1
H1
Clozapine
++
++
+++
+++
+++
+
Risperidone
-
+++
+++
+++
-
+
Olanzapine
++
++
+++
++
+++
++
Quetiapine
-
+
++
+++
+
+
Ziprasidone
+/-
++
+++
++
-
+
Aripiprazole
+
+++
++
++
-
+
Comparison of representative atypical antipsychotics
Drug
Advantages
Disadvantages
Clozapine
For treatment-resistant
cases, little EPS
Risk of fatal agranulocytosis
Risperidone
Broad efficacy, little or no
EPS at low doses
EPS and hypotension at high doses
Olanzapine
Effective with positive and
negative symptoms, little or
no EPS
Weight gain
Quetiapine
Similar to risperidone,
maybe less weight gain
Dose adjustment with associated
hypotension, bd dosing
Ziprasidone
Perhaps less weight gain
than clozapine, Inj A/V
QT prolongation
Aripiprazole
Less weight gain, novel
mechanism potential
Uncertain
03
Relative incidence of Adverse effects
Drugs
Sedation EPS Anticholinergic Orthostasis
Seizure
Prolactin
elevation
Weight
gain
Clozapine
++++
+
++++
++++
++++
0
++++
Risperidone
+++
+
++
+++
++
0 to ++++
++
Olanzapine
+++
+
+++
++
++
+
+++
Quetiapine
+++
+
++
++
++
0
++
Ziprasidone
++
+
++
++
++
0
+
Aripiprazole
++
+
++
++
++
0
+
1
st
line atypical antipsychotics
All atypicals except clozapine
NICE recommendations
Atypical antipsychotics considered when choosing 1
st
line treatment of newly diagnosed schizophrenia
Treatment option of choice for managing acute
schizophrenic episode
Considered when suffering unacceptable Adverse
effects from a conventional antipsychotic
Changing to an atypical not necessary if typical
controls symptoms adequately and no unacceptable
Adverse effects
04
2
nd
line atypical antipsychotic
Clozapine
Most effective antipsychotic for reducing symptoms
and preventing relapse
Use of clozapine effectively reduce suicide risk
1% risk of potentially fatal agranulocytosis
Acute pronounced leukopenia with great
reduction in number of neutrophil
Clozapine should be introduced if schizophrenia is
inadequately controlled despite sequential use of 2 or
more antipsychotic (one of which should be an
atypical) each for at least 6-8 weeks)
Rare cases of myocarditis and cardiomyopathy
Fatal
Most commonly in first 2 months
CSM recommendations
Physical exam and medical history before
starting
Persistent tachycardia esp. in first 2 weeks
should prompt observation for cardiomyopathy
If myocarditis or cardiomyopathy, stop
clozapine
Inform patients for unexplained fatigue,
dyspnea, tachypnea, chest pain, paipitation
and ask them to report these signs and
symptoms immediately

05
Non-antipsychotic agents
Benzodiazepines
Useful in some studies for anxiety, agitation, global
impairment and psychosis
Schizophrenic patients are prone to BZD abuse
Limit use to short trials (2-4 weeks) for management of
severe agitation and anxiety
Lithium
Limited role in schizophrenia monotherapy
Improve psychosis, depression, excitement, and irritability
when used with antipsychotic in some studies
Done by
Ali Kareem
