Drugs /AgentsInhibitors of cell wall synthesis
Inhibitors of bacterial cell wall biosynthesisIn principle, drugs that inhibit bacterial cell wall synthesis will exhibit selective toxicity, because the drug targets are unique to bacteria and are not present in human cells.
In practice,this principle is valid, and inhibitors of cell wall synthesis such as the B-lactams are drugs of choice for many bacterial infections.
The availability of B-lactam drugs with distinct antimicrobial spectra permits their use in a wide variety of clinical setting.
Inhibitors of bacterial cell wall biosynthesis
The B-lactam drugs are bactericidal and relatively non-toxic to human cells. This attractive pharmacological property has led to overuse and misuse, resulting in the emergence of drug-resistant bacteria.Resistance due to B-lactamase production can sometimes be overcome by using a B-lactamase inhibitors in combination with the B-lactam drug.
Resistance due to an alteration in the B-lactam target often cannot be surmounted, and a different drug class must be used for treatment.
MoA of PCN
Penicillin-binding proteins (PBPs): Targets for B-lactam drugsPenicillin-binding proteins (PBPs = transpeptidase enzymes) differ among bacterial species.
PBPs differ in their affinities for B-lactam drugs.
Therefore, bacteria can differ in susceptibility to B-lactam drugs because their transpeptidase enzymes are different.
Mutation in a PBP can confer resistance to B-lactam drugs examples.
Example
Methicillin-Resistant Staph. Aureus
Penicillin-resistant Strep. Pneumoniae
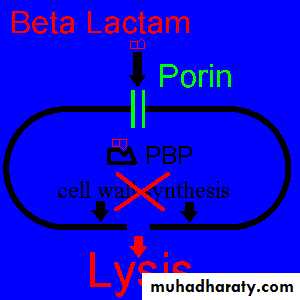
All β-lactam antibiotics interfere with the synthesis of the bacterial cell wall peptidoglycan. After attachment to penicillin-binding proteins on bacteria (there may be seven or more types in different organisms), they inhibit the transpeptidation enzyme that crosslinks the peptide chains attached to the backbone of the peptidoglycan.
The final bactericidal event is the inactivation of an inhibitor of autolytic enzymes in the cell wall, leading to lysis of the bacterium.
Enzymes that cleave B-lactam drugs
B-lactamases cleave the C-N bond of the B-lactam ring, inactivating the drug.Production of B-lactamase is a major cause of resistance.
There are many different B-lactamases, and they vary in specificity.
Development of drugs that inactivate B-lactamse has helped combat resistance.
B-lactam action
B-lactam drugs must:Penetrate outer membrane
Escape inactivation
Bind to target enzymes
Resistance can be due to
Lack of membrane penetrationInactivation by B-lactamase
Altered target PBPs
Semi-synthetic drugs have modification that:
Improve penetration through porins, enhancing Gram - negative activity.
Decrease B-lactames susceptibility, broadening spectrum
Alter PBP binding pattern, changing spectrum.
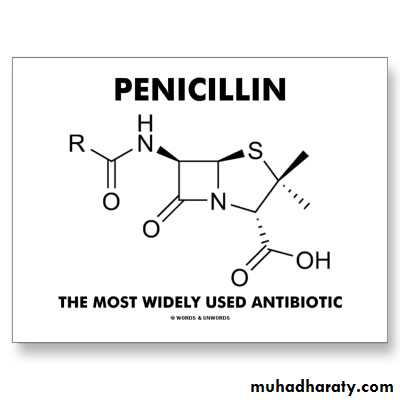
PENICILLINS
MOA: inhibit bacterial cell wall synthesis - bactericidal!Target: PBP (cell wall transpeptidase)
Lactam antibiotics
PCN are polar: Mostly Excreted primarily by kidneys
Exceptions: Nafcillin, Oxacillin
Dose adjustment needed in renally insufficient patients
Tissue penetration: good
Lung, liver, kidney, muscle, boneSide Effects:
Diarrhea: 5-10%
Rash: 4-10%
Fever: 4-8%
Neutropenia: 1-4%
Thrombocytopenia: 1-2%
Hypersensitivity Rxn
Most common AE and PCN may be the most common cause of drug allergy.
Seizures: 1%
Adverse Effects of PCN
Allergic reactions include various skin rashes, serum-sickness (rare), and anaphylaxis (rare).
Assume cross-allergenicity among PCNs.
N&V: reflect direct irritation of the GI tract and/or alterations in bowler flora.
In renal failure, Na+ or K+ toxicity can produce Seizures.
Natural PCNs
AgentsPen G (PO), Pen VK, Benzathine PCN (long acting IM injection, used in syphilis)
GRAM +
Strep:
Pneumo, ABCG: >60% susc.
Viridans: 30-60% susc.
Enterococcus:
Faecalis >60%
Faecium 30-60%
Very little clinically relevant gram –
PCN G: neisseria meningitidis
Anaerobes:
Actinomyces: 30-60%
Clostridium (not difficile): >60%
Peptostreptococcus: >60%
Coverage
Penicillinase Resistant PCNs (Anti-Staph PCNs)
Agents
Methicillin
Oxacillin
Nafcillin
Dicloxacillin (PO)
Primary Coverage
GRAM +
Staph (MSSA & Epi): >60%
Strep:
Pneumo, ABCG: >60% susc.
Viridans: 30-60% susc.
NO enterococcus
NO GRAM - coverage
Nafcillin, oxacillin:
High Na+ in IV forms, watch out in HTN patientsHepatically eliminated, do not need renal adjustment
Amino PCNs
• Agents• Ampicillin, Amoxicillin, Bacampicillin
• Primary Coverage
• GRAM +
• Strep:
• Pneumo, ABCG: >60% susc.
• Viridans: 30-60% susc.
• Staph Epi: >60%
• Enterococcus (both): >60%
Created to add some Gram - coverage
GRAM -
>60%: Proteus, Neisseria meningitidis
30-60%: H. Influenzae, E. Coli, Salmonella sp., Shigella sp.
- Anaerobes:
>60%: Clostridium (not difficile), Peptostreptococcus
30-60%: Actinomyces
Anti-Pseudomonal PCNs(Carboxypenicillins, Ureidopenicillins)
Agents
Piperacillin, Ticarcillin
Primary Coverage:
GRAM +
>60%: Strep Pneumo, Strep ABCG
30-60%: Strep viridans, Enterococcus (both)
Anaerobes:
>60%: Clostridium (not difficile), Peptostreptococcus
GRAM -
>60%:
Pseudomonas, Citrobacter, Enterobacter, Proteus, E. Coli, Salmonella, Shigella, Neisseria
Klebsiella (Pip only), Serratia (Ticar only)
30-60%: H. Influenzae, Moraxella (Pip only)
Lactamase Inhibitor PCNs
AgentsAugmentin: PO Amoxicillin/Clavulanate
Timentin: IV Ticarcillin/Clavulanate
Zosyn: IV Piperacillin/Tazobactam
Unasyn: IV Ampicillin/Sulbactam
Increase coverage to Lactamase Producing:
Staph
Neisseria
H. Influenzae
Klebsiella
Proteus
Augmentin, Unasyn do NOT cover Pseudomonas