

Learning Objectives
•
At the end of the lecture you have to know
What is inflammation and its types
What are the major components of
inflammation.
The roles of inflammatory mediatores
Clinical significace of inflammation.

Inflammation
Acute
Chronic
Granulamatous
Define inflammation?
Inflammation is defined as the response of a living
vascularized tissue to harmful agents.
It consists principally of:
vascular changes associated with leukocytes infiltration
and systemic reaction.
Inflammation is fundamental and common
pathologic process seen in many disease states.
What are the types of inflammation???
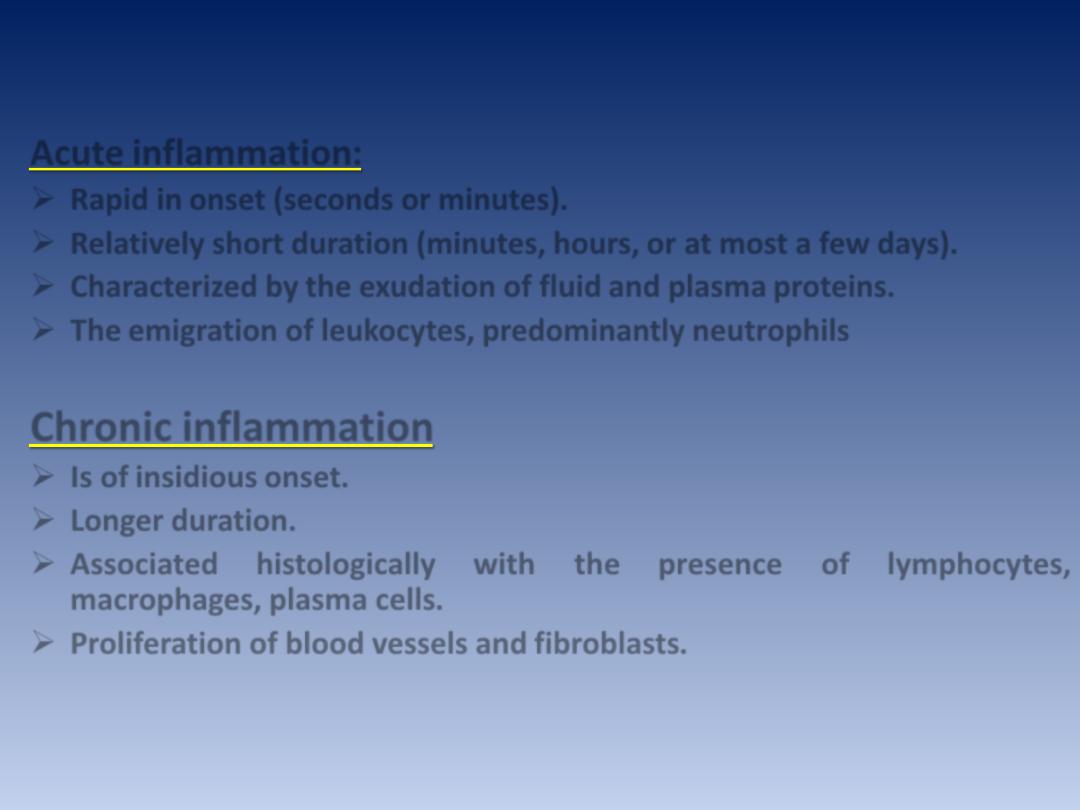
Acute inflammation:
Rapid in onset (seconds or minutes).
Relatively short duration (minutes, hours, or at most a few days).
Characterized by the exudation of fluid and plasma proteins.
The emigration of leukocytes, predominantly neutrophils
Chronic inflammation
Is of insidious onset.
Longer duration.
Associated histologically with the presence of lymphocytes,
macrophages, plasma cells.
Proliferation of blood vessels and fibroblasts
.
In both forms of inflammation:
Tissue necrosis of varying extent occurs.
The vascular and cellular reactions of both acute
and chronic inflammation are mediated by
chemical substances (chemical mediators) that
are derived from plasma proteins or cells.
Such substances, acting singly, in combinations,
or in sequence, amplify the inflammatory
response and influence its evolution.
What are the cardinal signs of
inflammation??
Rubor
Calor
Tumor
Dolor
5
th
(functio laesa)
HISTORICAL
HIGHLIGHTS

Acute inflammation
STIMULI
for acute inflammation
• INFECTIOUS
• PHYSICAL
• CHEMICAL
• Tissue Necrosis
• Foreign Bodies (FBs)
• Immune “responses”, or “complexes”
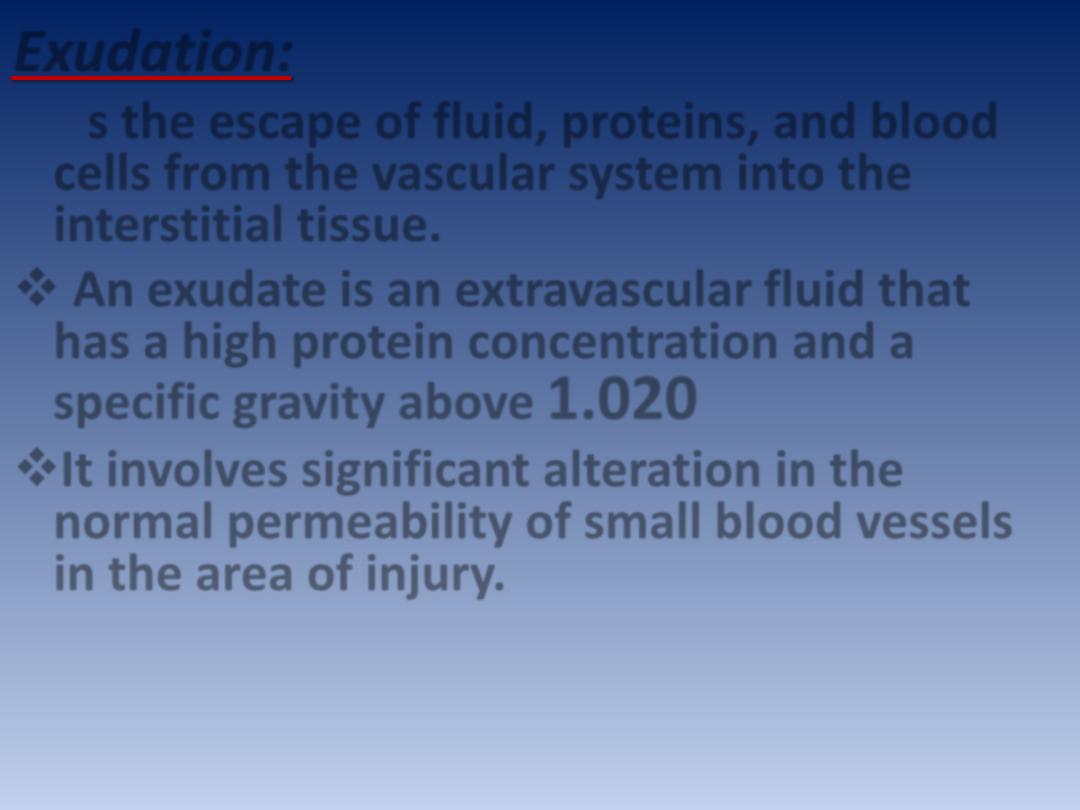
Exudation:
Is the escape of fluid, proteins, and blood
cells from the vascular system into the
interstitial tissue.
An exudate is an extravascular fluid that
has a high protein concentration and a
specific gravity above
1.020
It involves significant alteration in the
normal permeability of small blood vessels
in the area of injury.
Transudate:
Is a fluid with low protein content (most of
which is albumin)
A specific gravity of less than
1.012
It is essentially an ultrafiltrate of blood plasma
that results from osmotic or hydrostatic
imbalance across the vessel wall without an
increase in vascular permeability.
What are the major components of acute
inflammation?
A. Vasodilation associated with increased
blood flow.
B. Increased vascular permeability
associated with decreased blood flow.
C. Emigration and activation of leukocytes
and phagocytosis.

Vascular Changes
• Changes in Vascular Flow and
Caliber
• Increased Vascular
Permeability
and increased blood flow :
Vasodilation
A.
This is, sometimes, preceded by a transient
constriction of arterioles, lasting a few seconds.
Vasodilation first involves the arterioles, which
leads to an increase in blood flow; this in turn leads
to opening of new capillary beds in the area with
subsequent dilation of capillaries & venules.
This process allows more blood to flow into the
area, a process known as “active hyperemia”
(hyper- = increased; -emia = blood). These changes
explain the clinically noted heat and redness.

Vasodilation is induced by the
action of several mediators (such
as histamine) on vascular smooth
muscles.
Autonomic nerve impulses may
also play a role in relaxation of
arteriolar smooth muscle leading
to their dilation.
B. Increased Vascular Permeability and decreased
blood flow:
Increased vascular permeability leads to the
escape of exudates into the extravascular tissue.
This is driven by the increased hydrostatic
pressure owing to increased blood flow
through the dilated vessels and is
perpetuated through the loss of proteins
from the plasma that reduces the
intravascular
osmotic
pressure
and
increases the osmotic pressure of the
interstitial fluid.
hat are the mechanisms of increased vascular
W
permeability??
due to
venules
Formation of endothelial gaps in
.
1
is elicited by
.
endothelial cells contraction
,
bradykinin
histamine,
several mediators e.g.
.
leukotrienes
and
Binding of these mediators to receptors on
endothelial cells leads to stimulation of
contractile proteins (such as myosin). The
result is contraction of the endothelial cells
and separation of intercellular junctions that
eventuate in intercellular gaps formation.
retraction
Junctional
.
2
caused by chemical mediators such as
TNF and IL-1;
these induce structural reorganization of
the cytoskeleton of the cells
.
3. Direct endothelial cell injury as by burns
or infections
.
Because of endothelial
damage
and
exposure
of
the
subendothelial thrombogenic collagen,
this type is frequently associated with
platelets
adhesion
with
subsequent
thrombosis.
4. Leukocyte-dependant injury due to
accumulation of leukocytes and their
activation products (such as toxic oxygen
radicals and proteolytic enzymes) during
the inflammatory response.
These lead to
endothelial cell damage.
phagocytosis
Emigration and activation of leukocytes and
A critical function of inflammation is to :
• Deliver leukocytes to the site of injury
• Activate the leukocytes to defend the host.
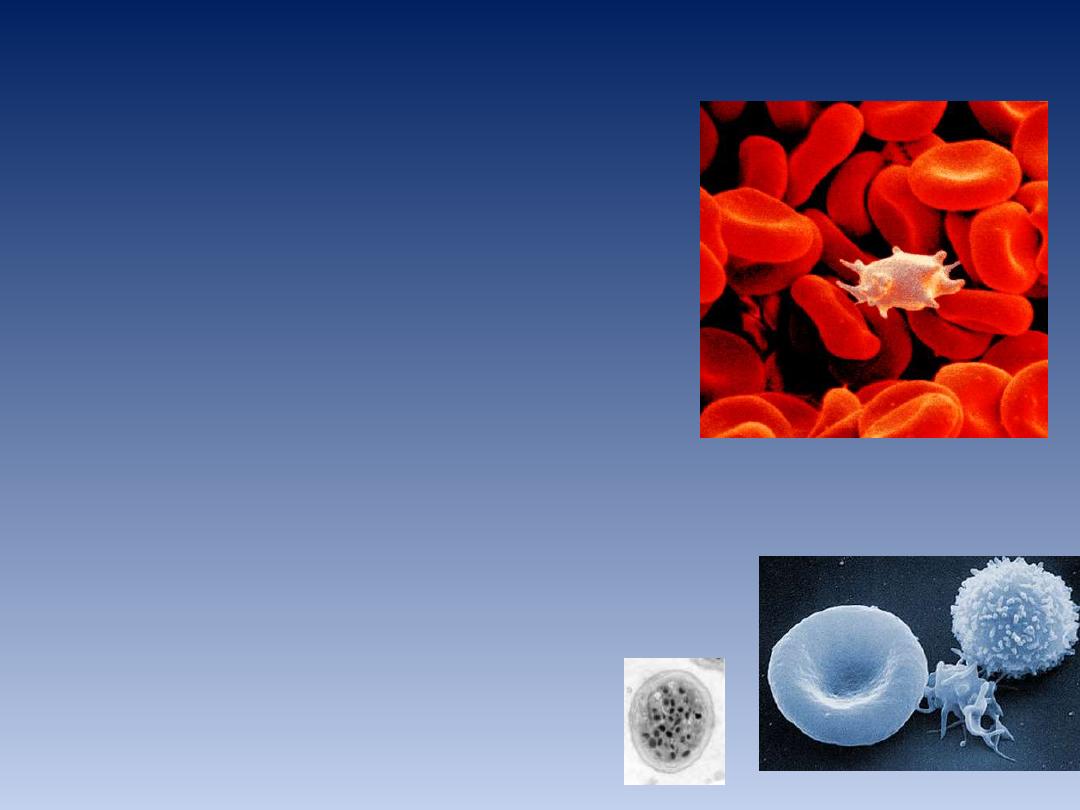
Leukocytes:
offending agents
Kill bacteria and other microbes.
Get rid of necrotic tissue and foreign substances.
However, these cells may induce tissue damage and prolong
inflammation.
The journey of leukocytes from the vessel lumen to the
interstitial tissue is called extravasation.
This can be divided into the following steps:
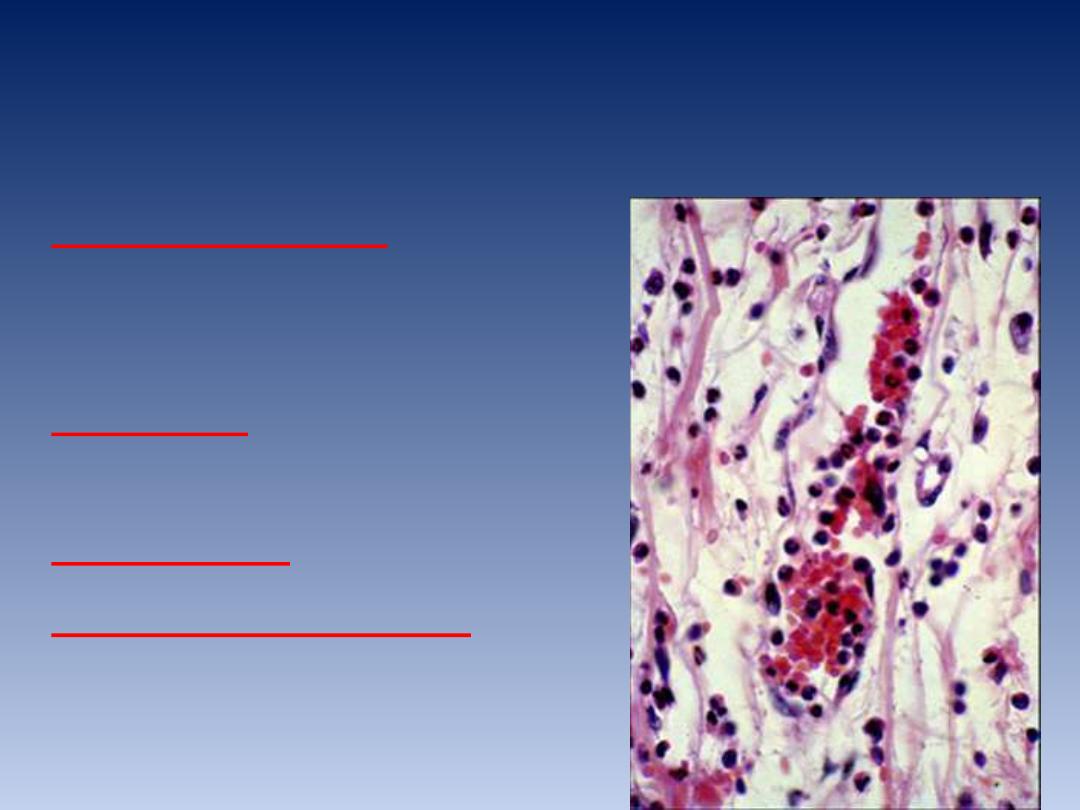
EXTRAVASATION of PMNs
• MARGINATION
(PMN’s go toward
wall)
• ROLLING
(tumbling
and HEAPING)
• ADHESION
• TRANSMIGRATION
(DIAPEDESIS)
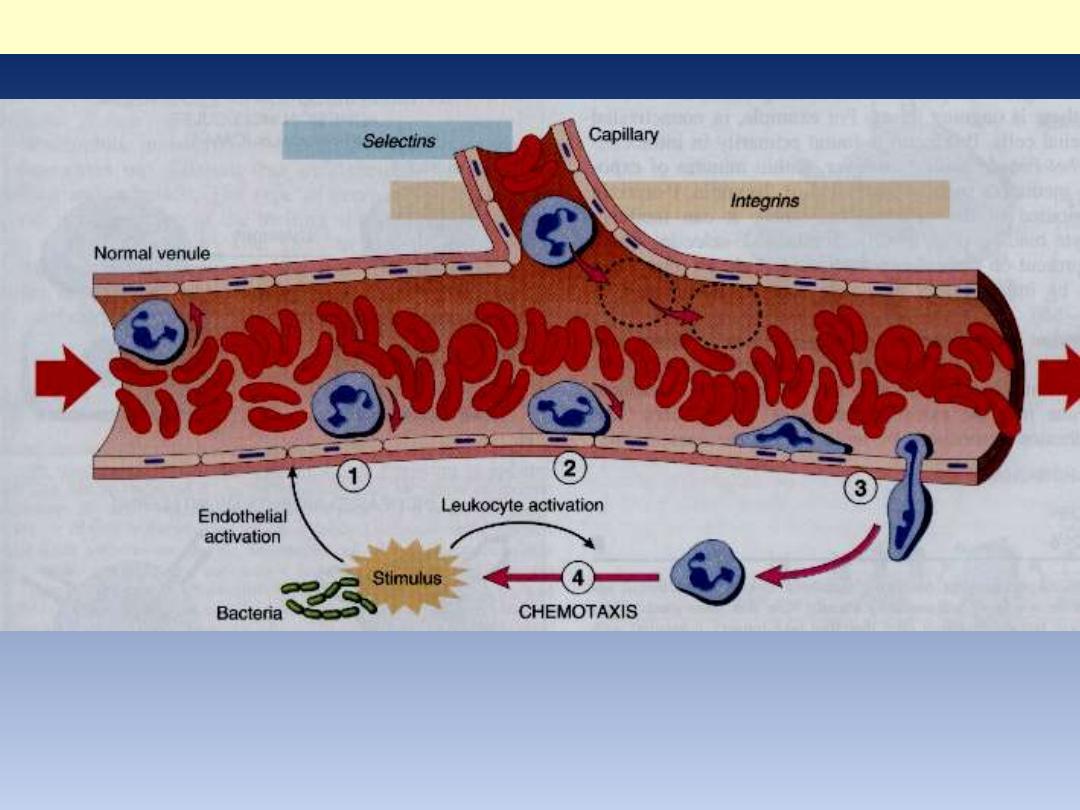
Sequence of events in leukocytes emigration in inflammation:
1. Margination 2. rolling 3. adhesion 4. transmigration and movement
toward injurious agent (stimulus)
Emigration of neutrophils
What is Chemotaxis???
Chemotaxis is defined as locomotion
oriented along a chemical gradient of
chemoattractants.
All granulocytes, monocytes and, to a lesser
extent, lymphocytes respond to
chemoattractants (chemotactic stimuli) with
varying rates of speed.
Both exogenous and endogenous substances can
act as chemoattractants. The former is
exemplified by bacterial products.

• Enumerate the Endogenous chemoattractants

Endogenous chemoattractants, however,
include several chemical mediators:
1. Components of the complement system,
particularly C5a
2. Products of the lipoxygenase pathway,
mainly leukotriene B4 (LTB4)
3. Cytokines (secreted from cells) e.g., IL-8

What are the steps of
phagocytosis?
PHAGOCYTOSIS
RECOGNITION
ENGULFMENT
KILLING
DEGRADATION/DIGESTION)

Phagocytosis involves three distinct but
interrelated steps:
1. Recognition and attachment of the particle
to be ingested by the leukocyte
2. Its engulfment, with subsequent formation
of a phagocytic vacuole
3. Killing and degradation of the ingested
material.

The efficiency of phagocytosis is greatly
enhanced when microbes are opsonized by
specific proteins (opsonins) for which the
phagocytes express high-affinity receptors.
The major opsonins are
IgG
C3b
Plasma lactin.
………………………………………………………………………
…………………………..
• Microbial killing is accomplished largely by
oxygen-dependent
mechanisms,
which
depends on the production of
particularly
H2O2..
Oxygen-
independent degradation depends on the
release of granules, containing proteolytic
enzymes such as defensins (antibacterial
peptide attacking bacterial cell membrane),
proteolytic enzymes such as elastases,
lysozymes, and cationic proteins
Cells of acute inflammation
Cells
Activity
Phagocytosis Inflammation
Neutrophil
Proteases,
oxidases
+
Acute
Eosinophil
histamine
+
Acute,
Chronic
Macrophage
Antigen
processing,
digestion
+
Late acute,
chronic

CHEMICAL MEDIATORS OF
INFLAMMATION
CHEMICAL MEDIATORS
• From plasma or cells
• Have “triggering” stimuli
• Usually have specific targets
• Can cause a “cascade”
• Are short lived

CLASSIC MEDIATORS
• HISTAMINE
• SEROTONIN
• COMPLEMENT
• KININS
• CLOTTING FACTORS
• Arachidonic acid
metabolites
• NITRIC OXIDE
• PLATELET ACTIVATING
FACTOR (PAF)
• CYTOKINES
• /CHEMOKINES
• LYSOSOME
CONSTITUENTS
• FREE RADICALS
• NEUROPEPTIDES
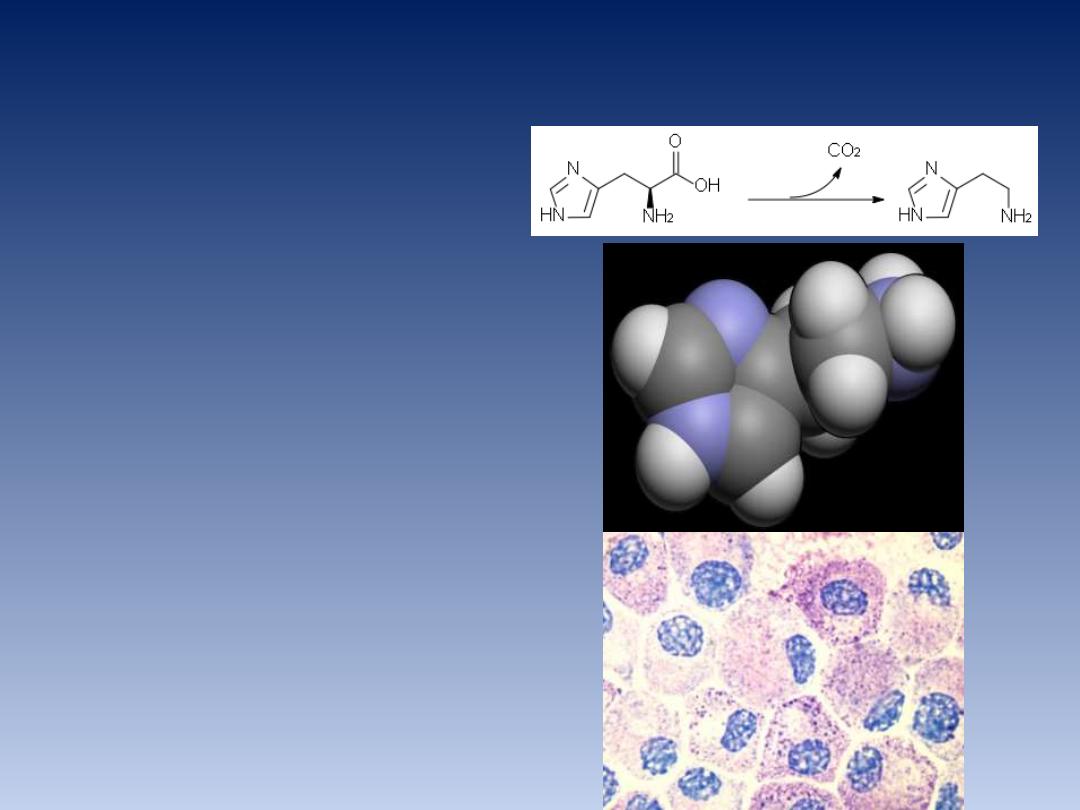
HISTAMINE
• Mast Cells,
basophils
• POWERFUL
Vasodilator
• Vasoactive
“amine”
• IgE on mast cell
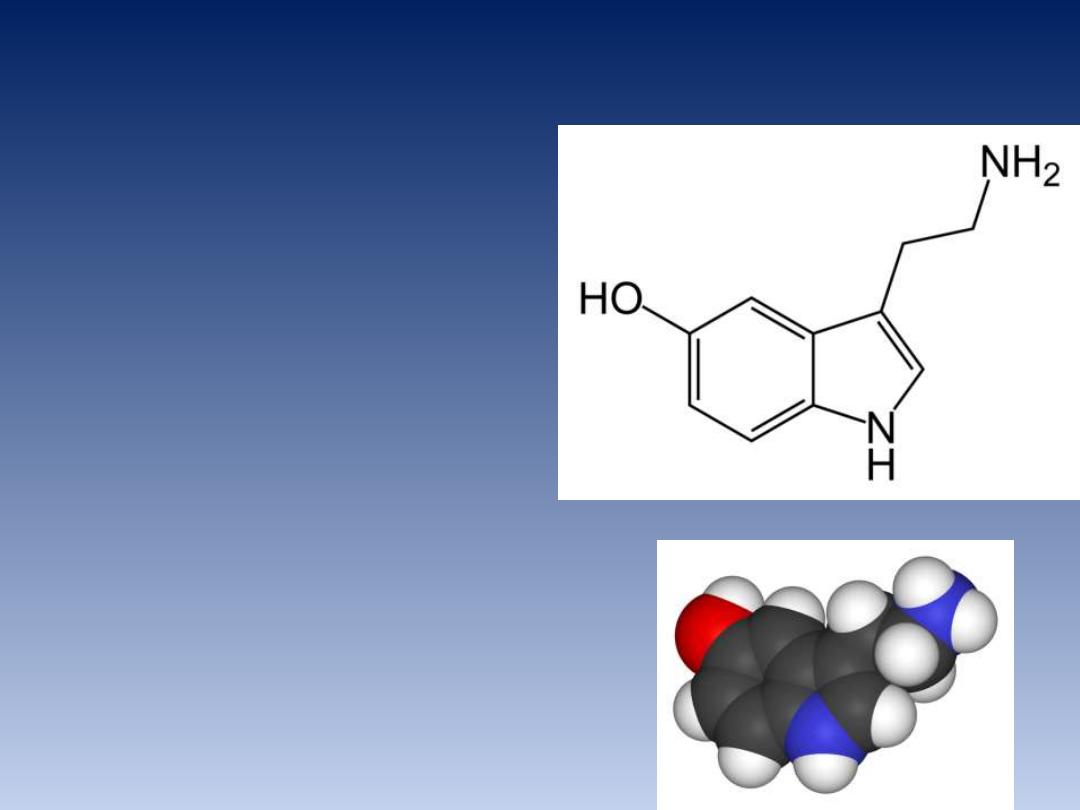
SEROTONIN
• (5HT
,
5
-
H
ydroxy-
T
ryptamine
)
• Platelets and
EnteroChromaffin Cells
• Also vasodilatation, but
more indirect
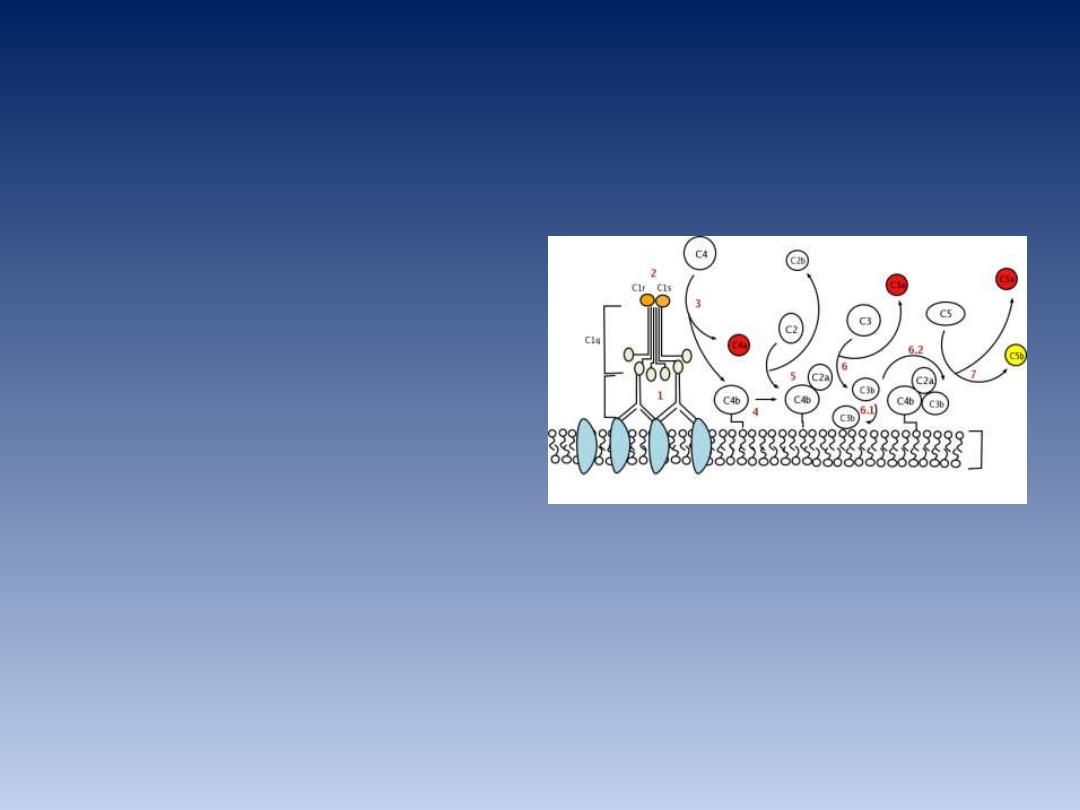
COMPLEMENT SYSTEM
• i.
Vascular phenomena:
C3a, C5a
stimulate histamine release from
mast cells and thereby increase
vascular permeability and cause
vasodilation.
• ii.
Chemoattractants:
for e.g. C5a is
a powerful chemotactic agent for
neutrophils, monocytes,
eosinophils, and basophils.
• iii.
Opsonins:
when fixed to the
bacterial cell wall, C3b acts as an
opsonin and favor phagocytosis by
neutrophils and macrophages.
KININ SYSTEM
• BRADYKININ is KEY component
• ALSO from circulating plasma
• BRADYKININ
has actions similar to those of
histamine.

CLOTTING
FACTORS
• Also from circulating plasma
• Coagulation, i.e., production of fibrin
• triggering recruitment of leukocytes
EICOSANOIDS
(ARACHIDONIC ACID DERIVATIVES)
Part of cell membranes
1)
Prostaglandins
(incl.
Thromboxanes)
2)
Leukotrienes
3)
Lipoxins
(new)
MULTIPLE ACTIONS AT MANY LEVELS

Prostaglandins
(thromboxanes included)
• Pain
•
TxA2 is a potent platelet-aggregating
agent and a vasoconstrictor
• Prostacyclin, has actions opposing that
of TxA2 in that it is a vasodilator, a
potent inhibitor of platelet aggregation

Leukotrienes
Chemotaxis
The principal actions of
lipoxins are to inhibit
neutrophil chemotaxis and
adhesion to endothelium
P
latelet-
A
ctivating
F
actor
(PAF)
• Phospholipid
• From MANY cells
• ACTIVATE PLATELETS,
powerfully

CYTOKINES/CHEMOKINES
• CYTOKINES
are PROTEINS produced by MANY
cells, but usually LYMPHOCYTES and
MACROPHAGES, numerous roles in acute and
chronic inflammation
–TNFα
,
IL-1
,
by macrophages
• CHEMOKINES
are small proteins which are
attractants for PMNs

N
ITRIC
O
XIDE
• Potent vasodilator
• NO and its derivatives are
microbicidal, and thus NO is
also a mediator of host
defense against infection
LYSOSOMAL CONSTITUENTS
• PRIMARY
• Also called
AZUROPHILIC, or
NON-specific
• Myeloperoxidase
• Lysozyme (Bact.)
• Acid Hydrolases
• SECONDARY
• Also called
SPECIFIC
• Lactoferrin
• Lysozyme
• Alkaline Phosphatase
• Collagenase

FREE RADICALS
• O2
–
(SUPEROXIDE)
•H2O2
(PEROXIDE)
•OH
-
(HYDROXYL RADICAL)
•
VERY VERY
DESTRUCTIVE

NEUROPEPTIDES
• SUBSTANCE P
which has many
biologic functions, including the
transmission
of
pain
signals,
regulation of blood pressure, and
increasing vascular permeability
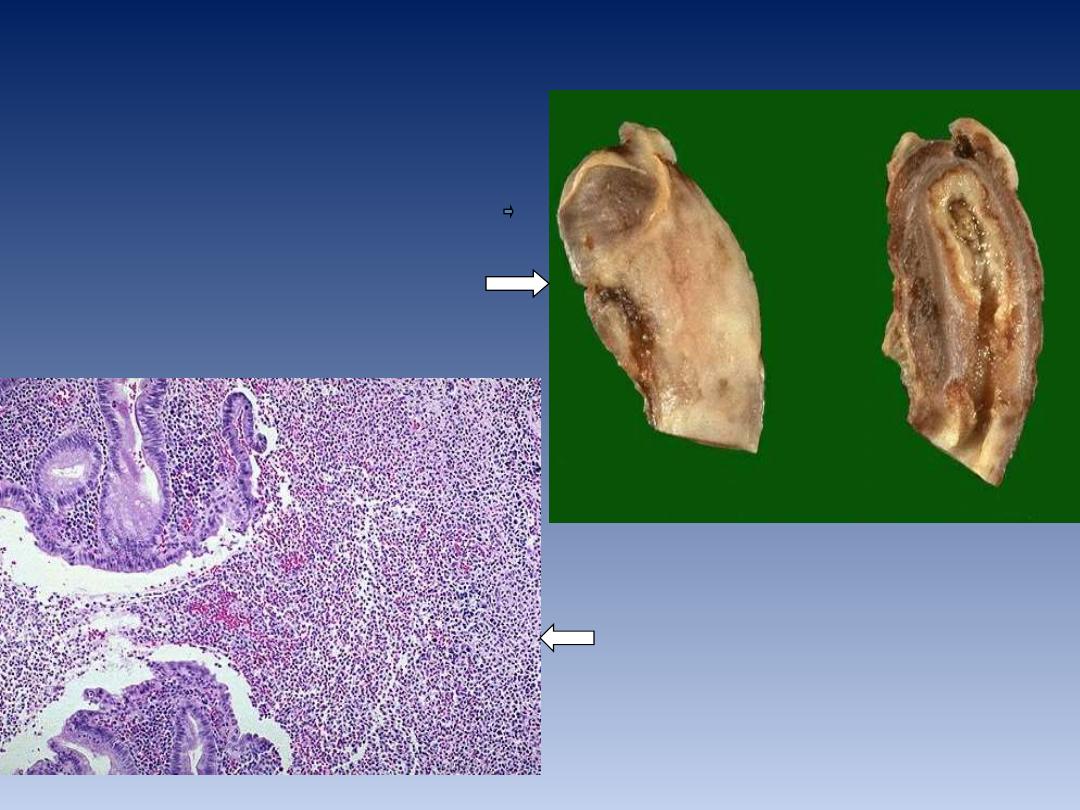
Appendix: acute suppurative inflammation
ulceration and undermining by an
extensive neutrophilic exudate
Upper half of excised appendix.
Lt: fibrino-purulent serosal
exudate
Rt: lumen filled with pus
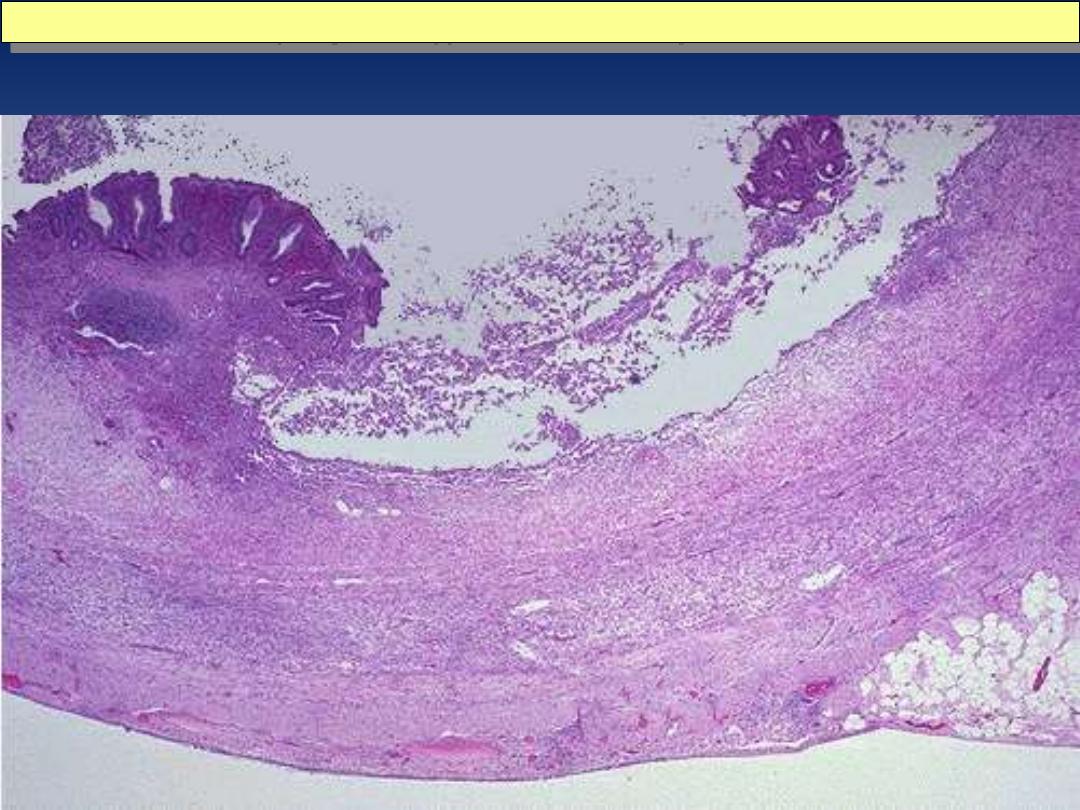
acute appendicitis: mucosal inflammation and necrosis.
Microscopically, acute appendicitis is marked by mucosal inflammation and necrosis.
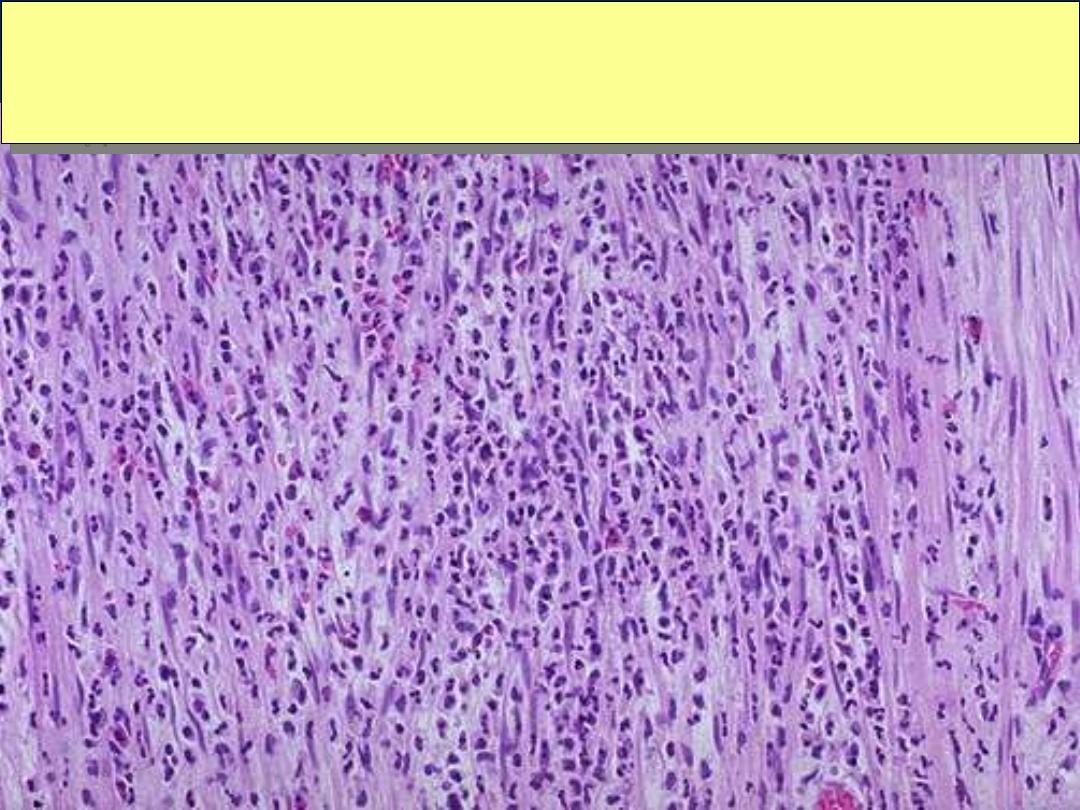
Transmural inflammation in acute appendicitis
Neutrophils extend into and through the wall of the appendix in a case of acute appendicitis.
Clinically, the patient often presents with right lower quadrant
abdominal pain. Rebound tenderness is noted on physical examination. An elevated WBC count is
usually present.
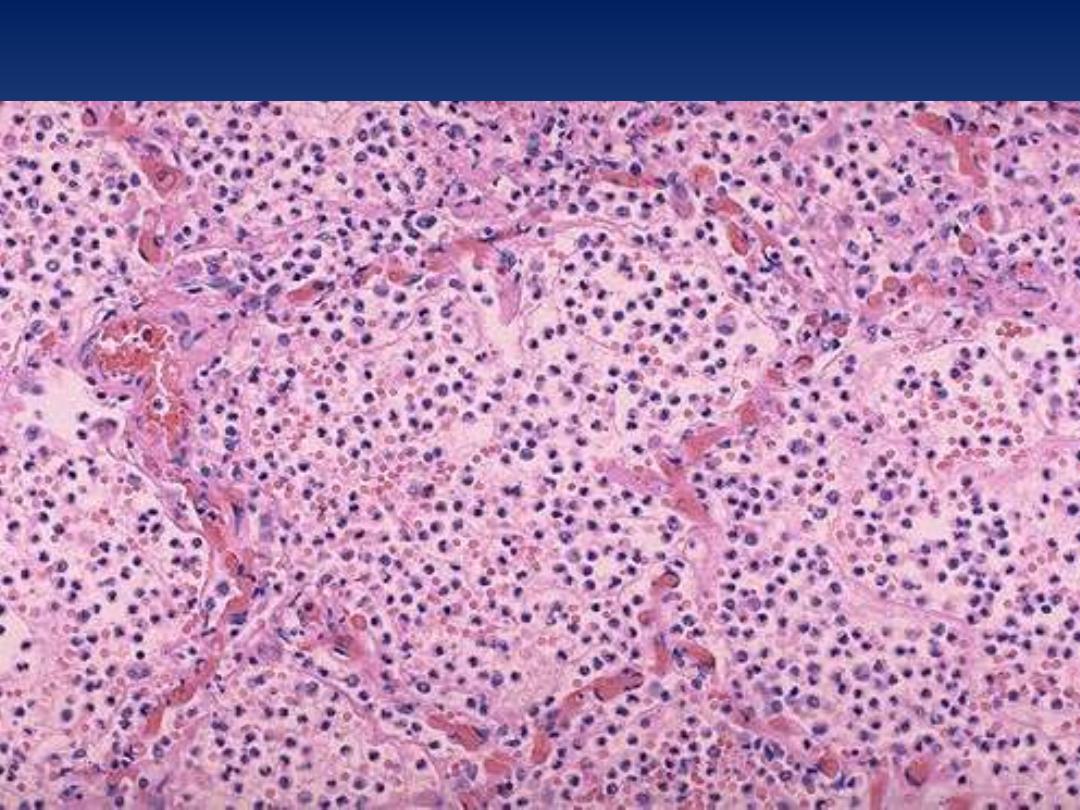
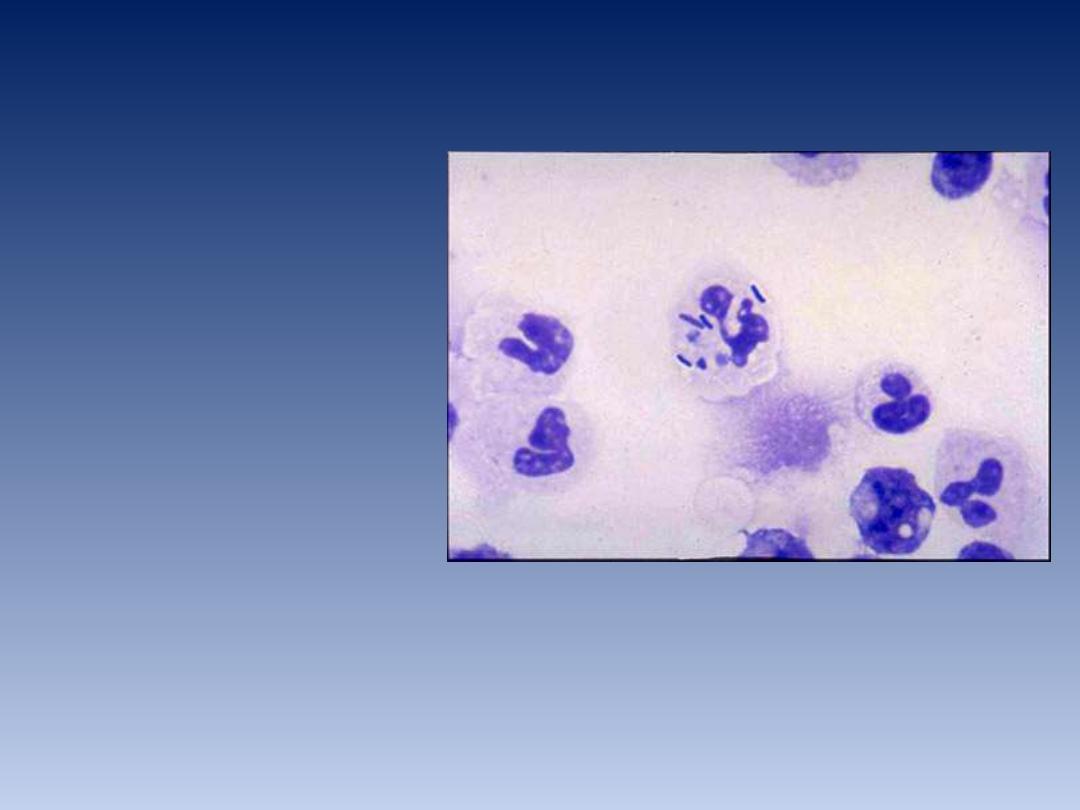
Acute pneumonia, microscopic
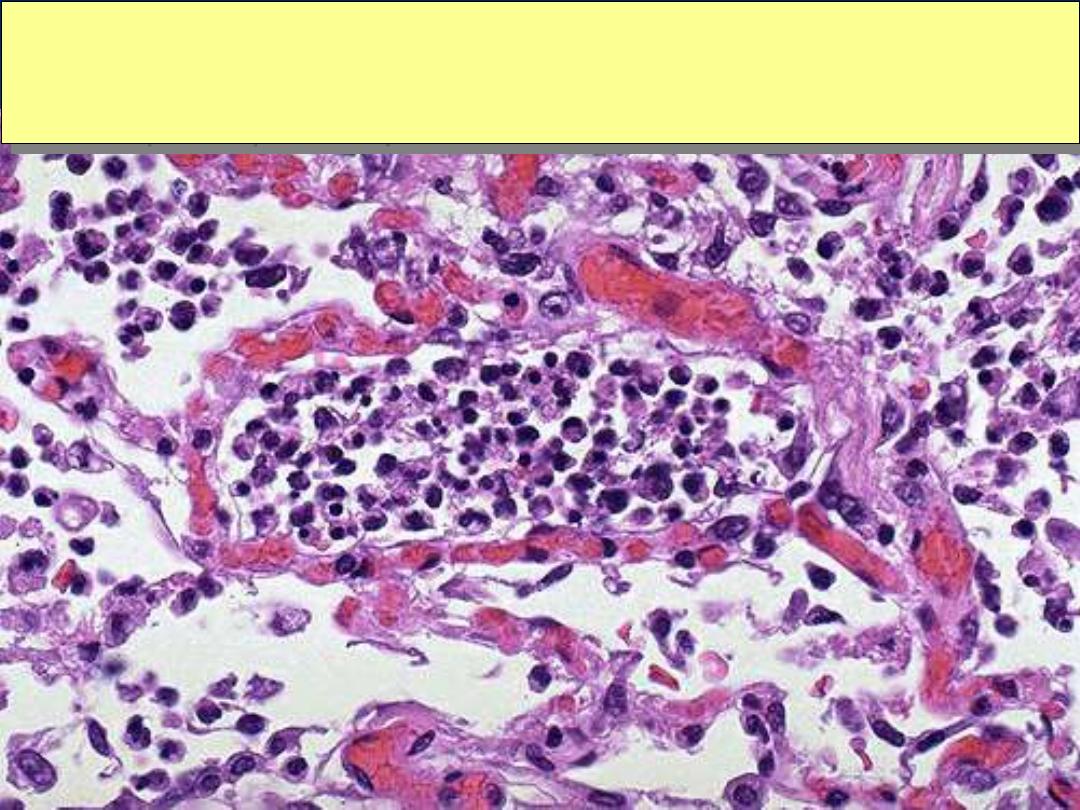
Acute pneumonia, microscopic
Acute bronchopneumonia, microscopic
The PMN's seen here are in alveoli, indicative of an acute bronchopneumonia of the lung. The
PMN's form an exudate in the alveoli. This patient had a "productive
“ cough because large
amounts of purulent sputum were produced. The source is seen here.

