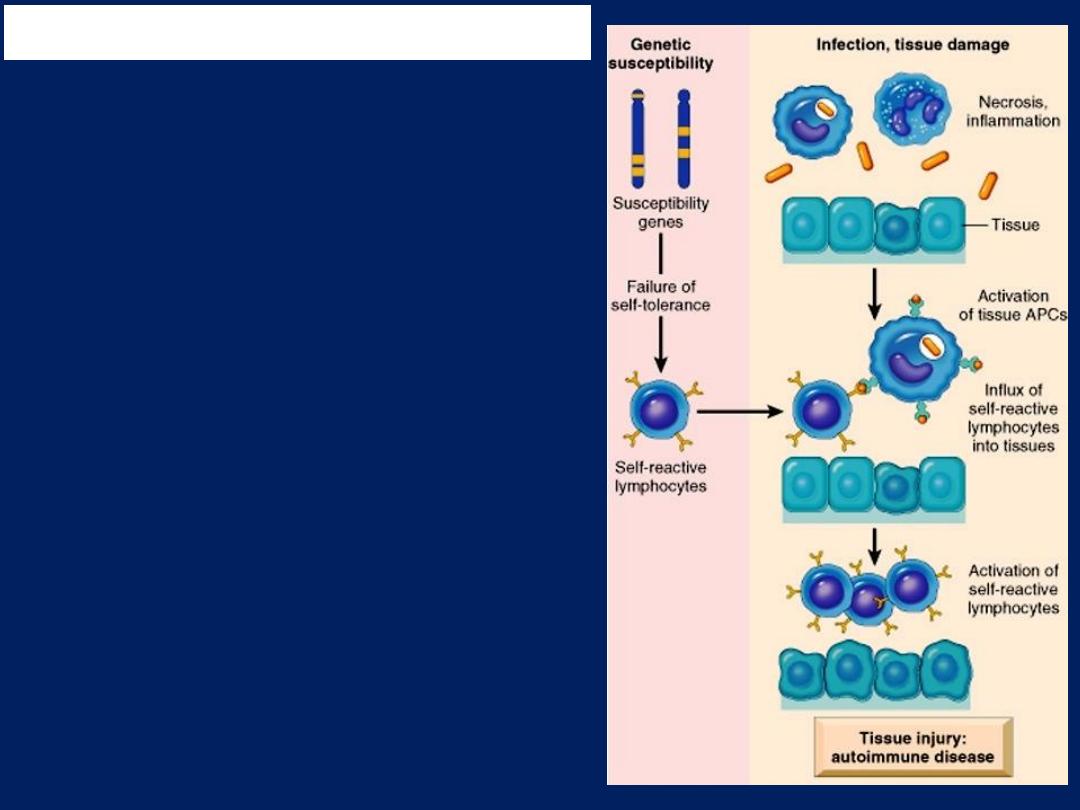
Autoimmunity results from
multiple factors:
●Susceptibility genes
that may
interfere with self-tolerance.
●Environmental triggers
(tissue injury, inflammation)
that promote lymphocyte
entry into tissues, activation of
self-reactive lymphocytes, and
tissue damage.
Pathogenesis of Autoimmunity
Pathogenesis of Autoimmunity
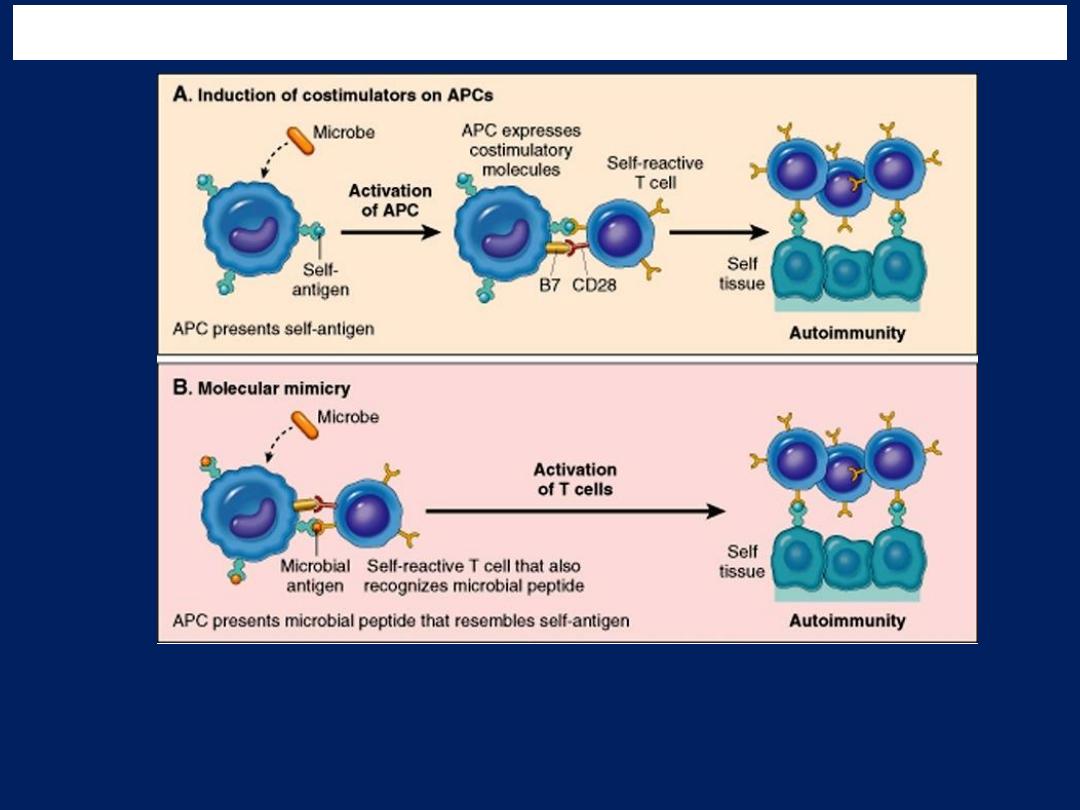
Postulated role of infections in autoimmunity. Infections may promote
activation of self-reactive lymphocytes by inducing the expression of
costimulators (A), or microbial antigens may mimic self-antigens and activate
self-reactive lymphocytes as a cross-reaction (B).
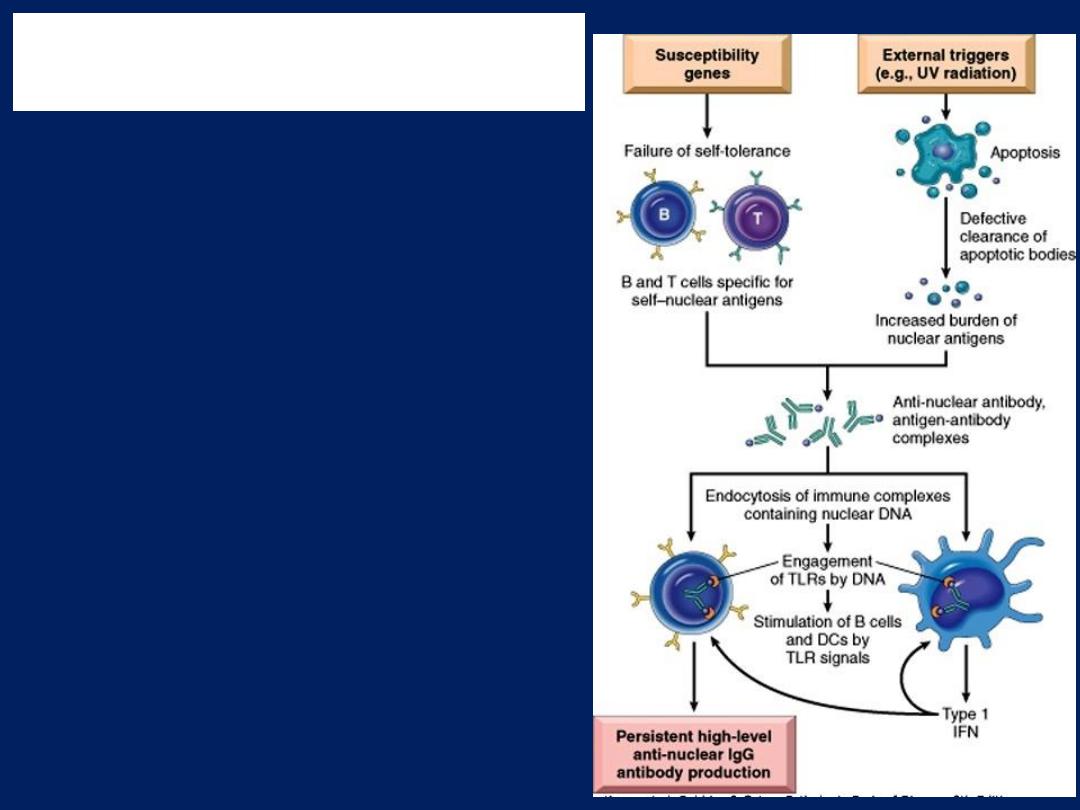
●Susceptibility genes
interfere
with the maintenance of self-
tolerance
.
●External triggers
lead to
persistence of nuclear antigens.
The result is an antibody
response against self–nuclear
antigens, which is amplified by
the action of nucleic acids on
dendritic cells (DCs) and B cells,
and the production of type 1
interferons. (TLRs: Toll-like
receptors).
Pathogenesis of systemic lupus
erythematosus
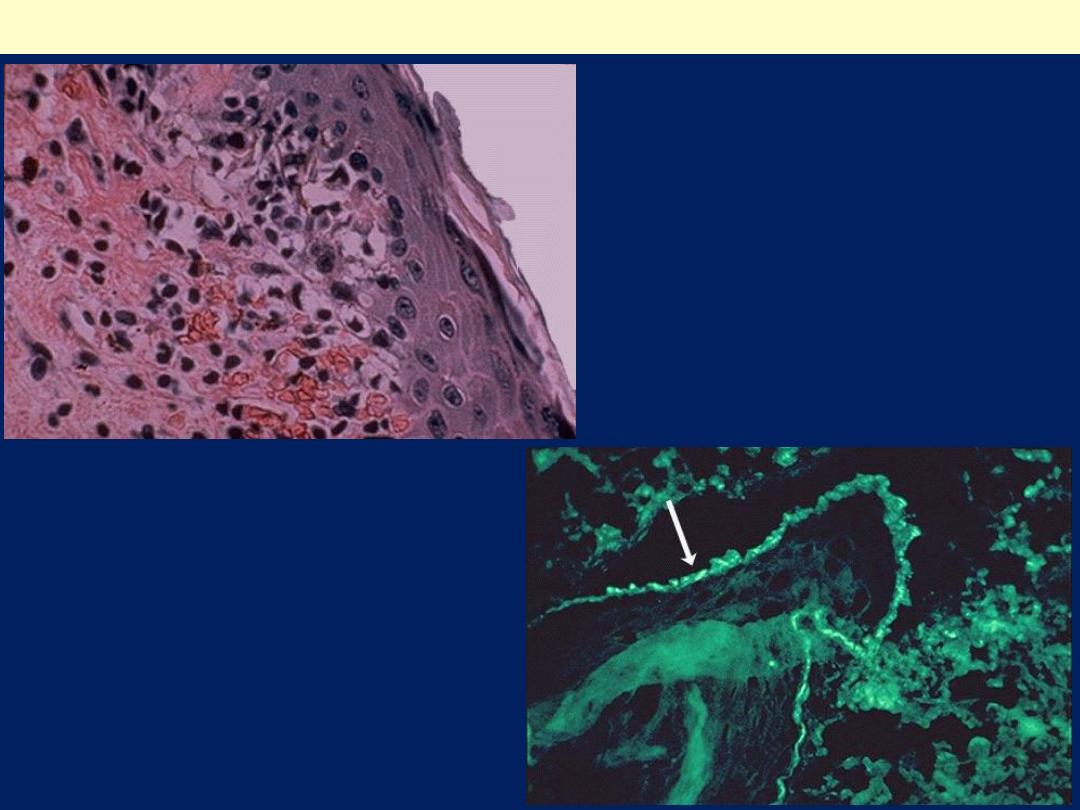
SLE: Skin
Immunofluorescence stain with
antibody to complement or
immunoglobulin:
Brightly fluorescing band
along the dermal epidermal
junction that indicates immune
complex deposits are present.
Inflammatory skin infiltrate
in the upper dermis in which
the basal layer is undergoing
vacuolization and dissolution,
and there is purpura with
RBC's in the upper dermis
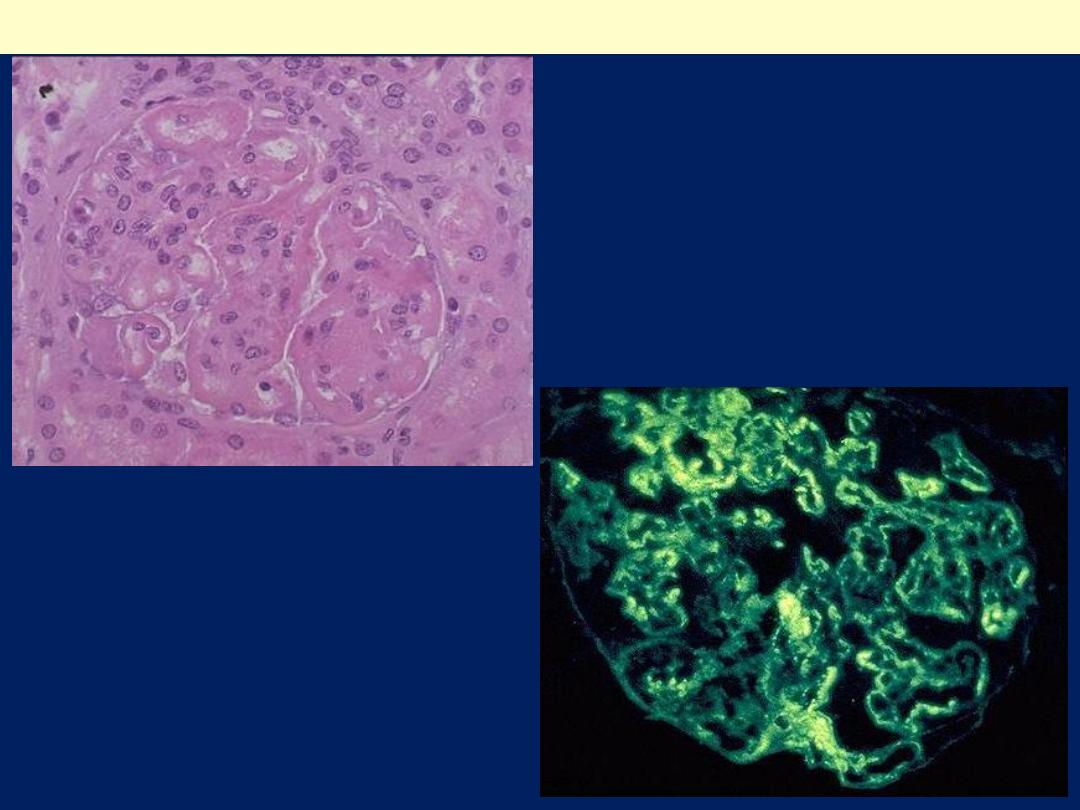
SLE: Lupus Nephritis
A sclerotic glomerulus with
thickened capillary loops in
a patient with lupus
nephritis.
immunofluorescence staining is
performed, here with antibody to
IgG, then a granular pattern of
immunofluorescence is seen,
indicative of deposition of immune
complexes in the basement
membranes of the glomerular
capillary loops.
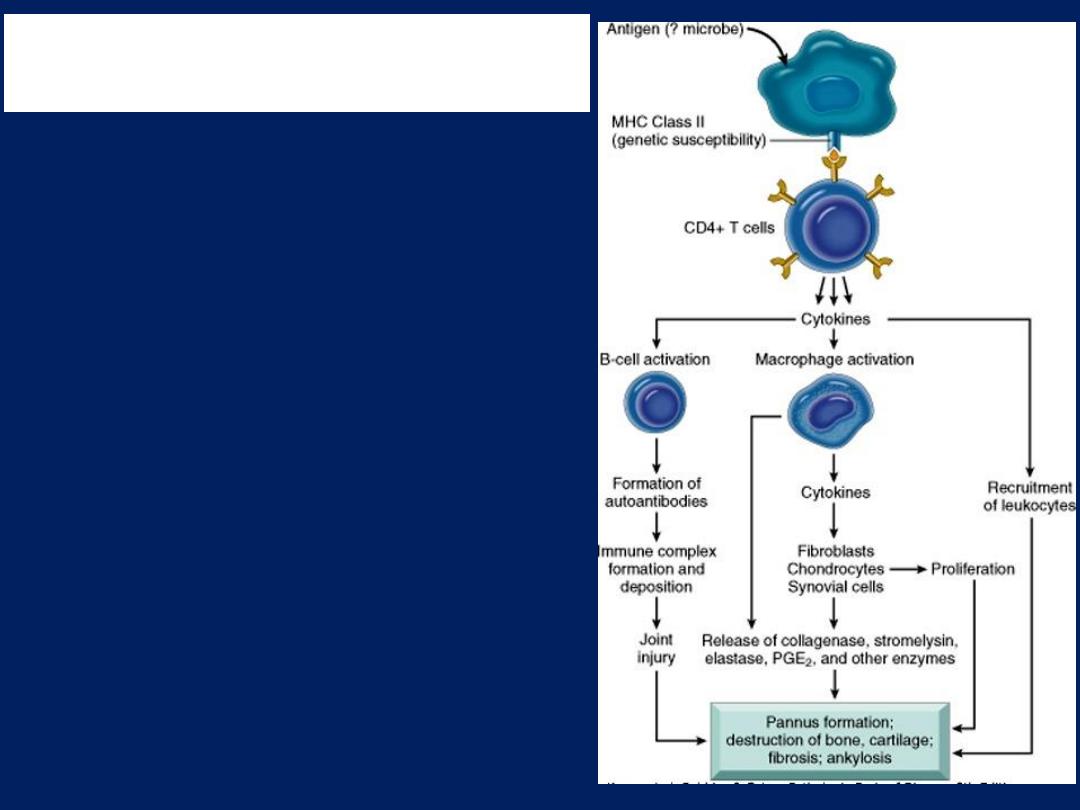
Immunopathogenesis of
Rheumatoid Arthritis
Rheumatoid arthritis
is triggered
by exposure of a genetically
susceptible host to an arthritogenic
antigen resulting in a breakdown of
immunological self-tolerance and a
chronic inflammatory reaction.
In this manner, an acute arthritis is
initiated, but it is the continuing
autoimmune reaction, the
activation of CD4+ helper T cells,
and the local release of
inflammatory mediators and
cytokines that ultimately destroys
the joint
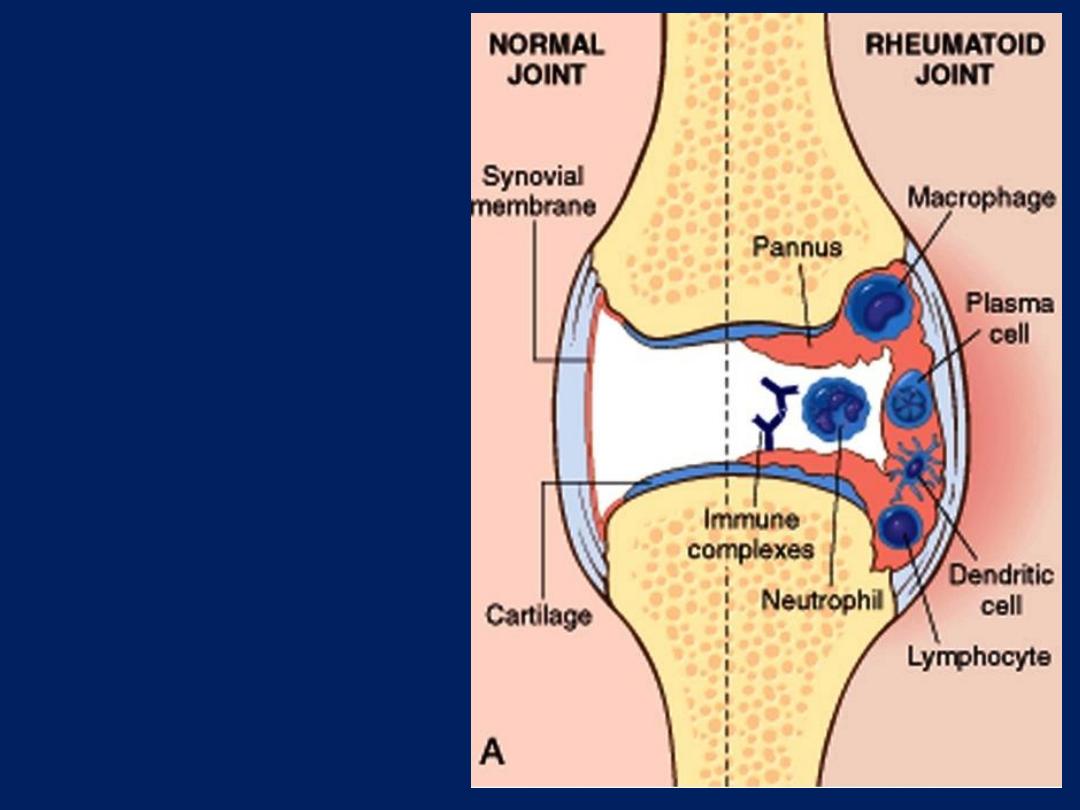
Rheumatoid
arthritis:
Schematic view of
the joint lesion
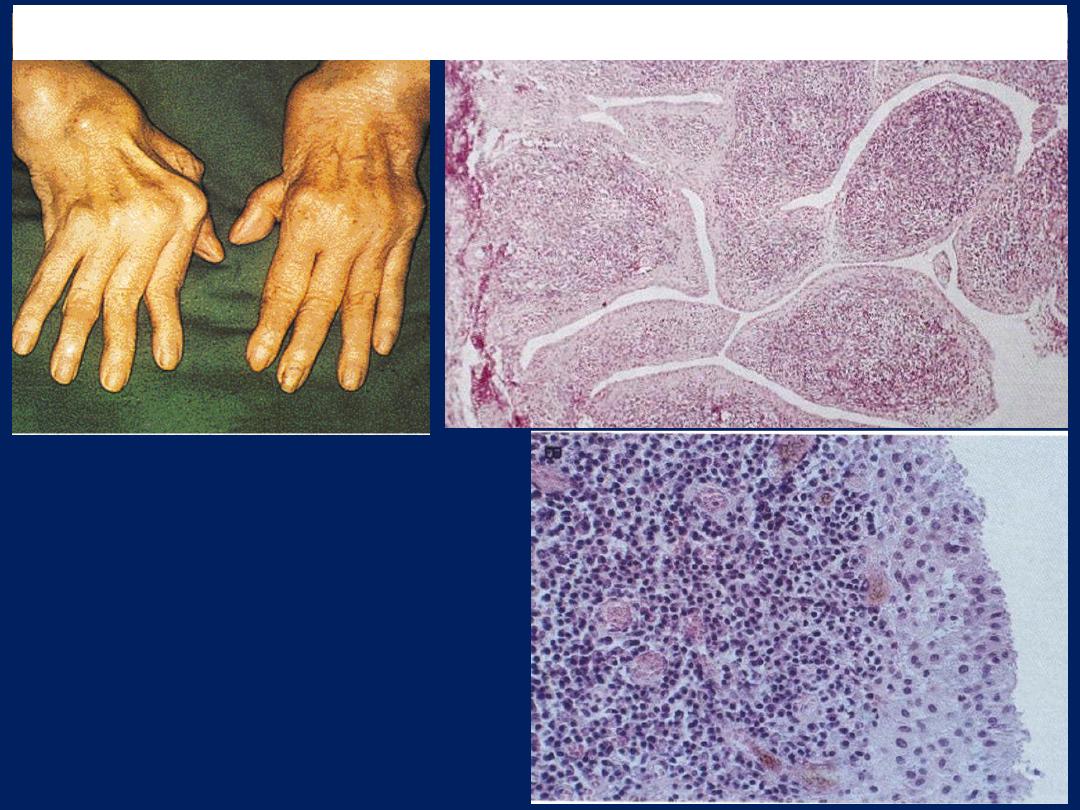
This is the synovium in
rheumatoid arthritis. There is
chronic inflammation with
lymphocytes and plasma cells
that produce the blue areas
beneath the nodular
proliferations
Rheumatoid Arthritis
