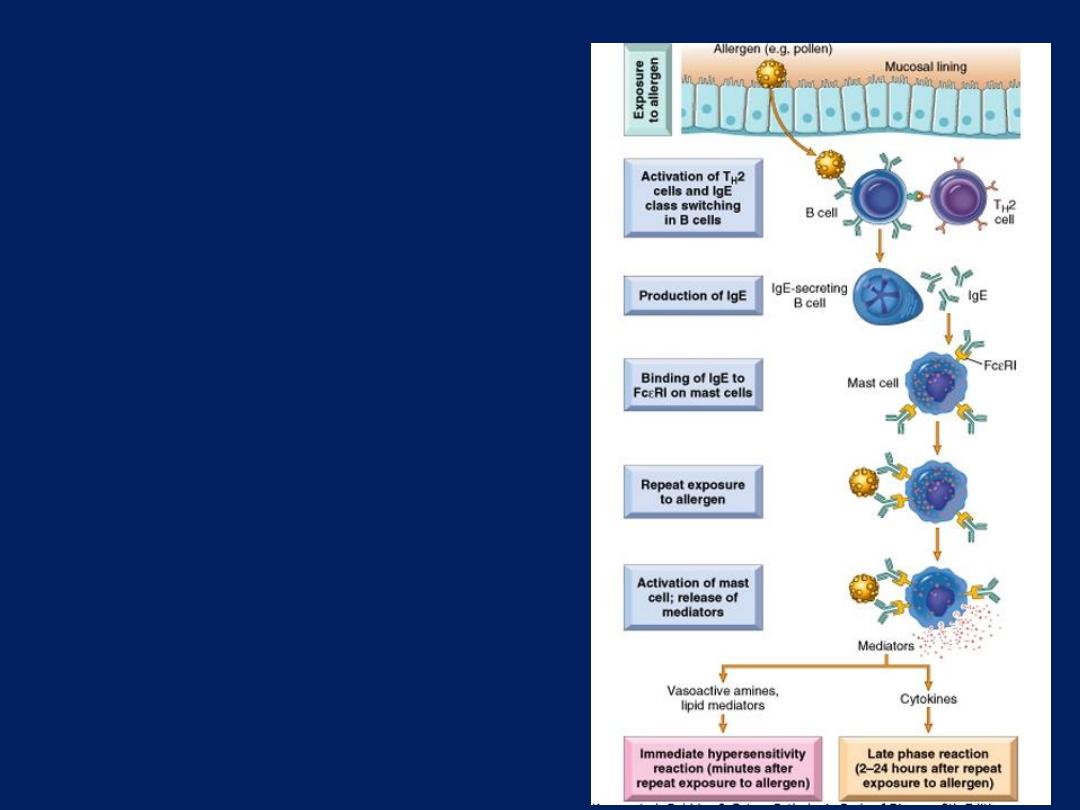
Sequence of events in immediate
(type I) hypersensitivity.
Immediate hypersensitivity
reactions are initiated by the
introduction of an allergen, which
stimulates T
H
2 responses and IgE
production in genetically
susceptible individuals. IgE binds
to Fc receptors on mast cells, and
subsequent exposure to the
allergen activates the mast cells to
secrete the mediators that are
responsible for the pathologic
manifestations of immediate
hypersensitivity
Immediate (Type I)
Hypersensitivity
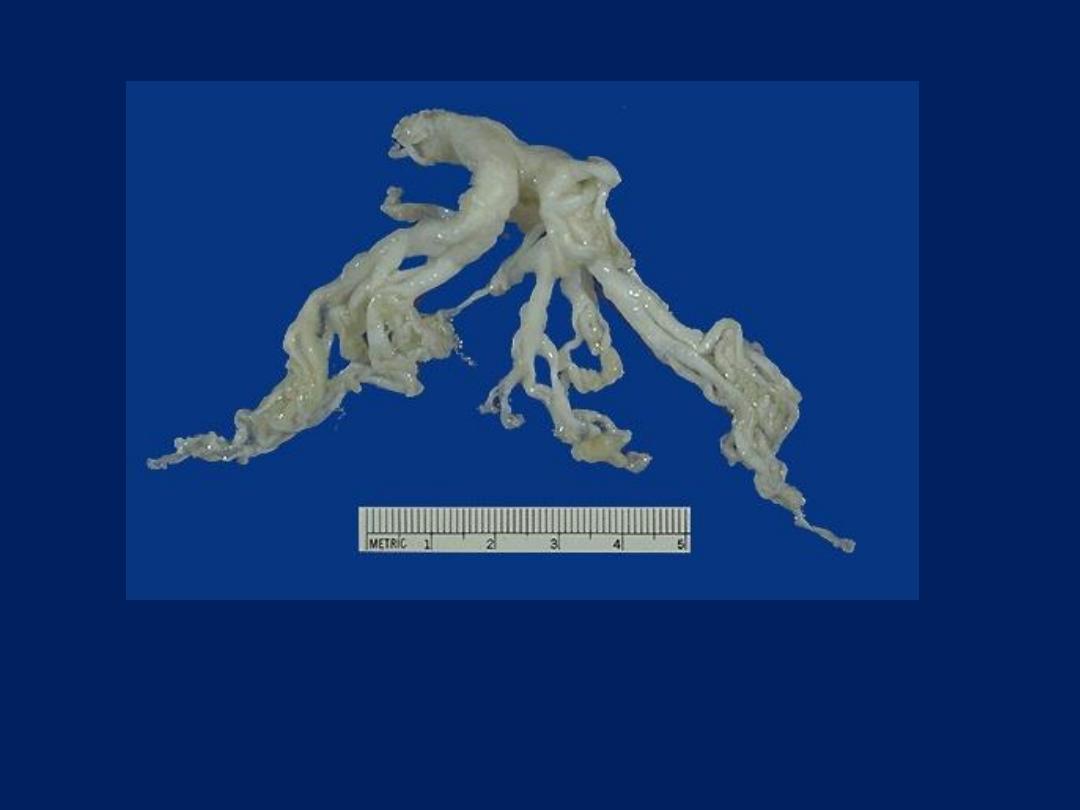
This cast of the bronchial tree is formed of inspissated mucus and was coughed
up by a patient during an asthmatic attack. The outpouring of mucus from
hypertrophied bronchial submucosal glands, the bronchoconstriction, and
dehydration all contribute to the formation of mucus plugs that can block
airways in asthmatic patients.
Immediate (Type I) Hypersensitivity:
Asthma
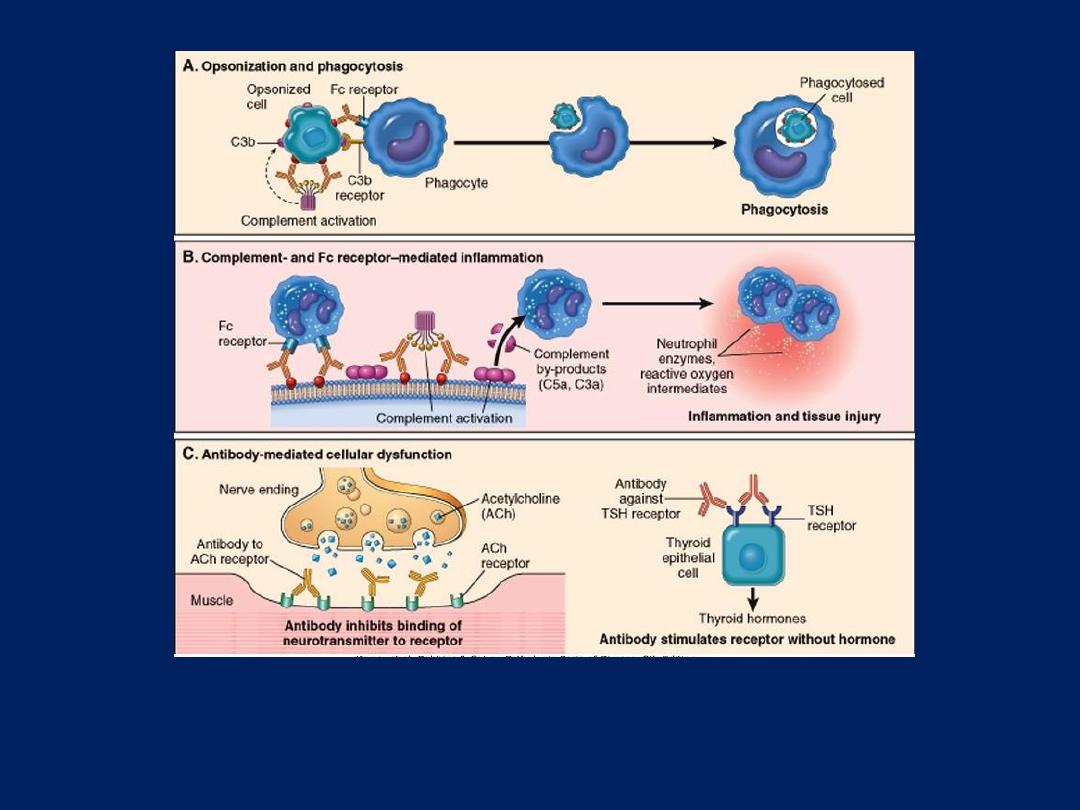
Antibody-Mediated (Type II) Hypersensitivity
A: Opsonization of cells by antibodies and complement components and ingestion by phagocytes. B: Inflammation
induced by antibody binding to Fc receptors of leukocytes and by complement breakdown products. C: Anti-
receptor antibodies disturb the normal function of receptors. In these examples, antibodies to the acetylcholine
(ACh) receptor impair neuromuscular transmission in myasthenia gravis, and antibodies against the thyroid-
stimulating hormone (TSH) receptor activate thyroid cells in Graves disease.
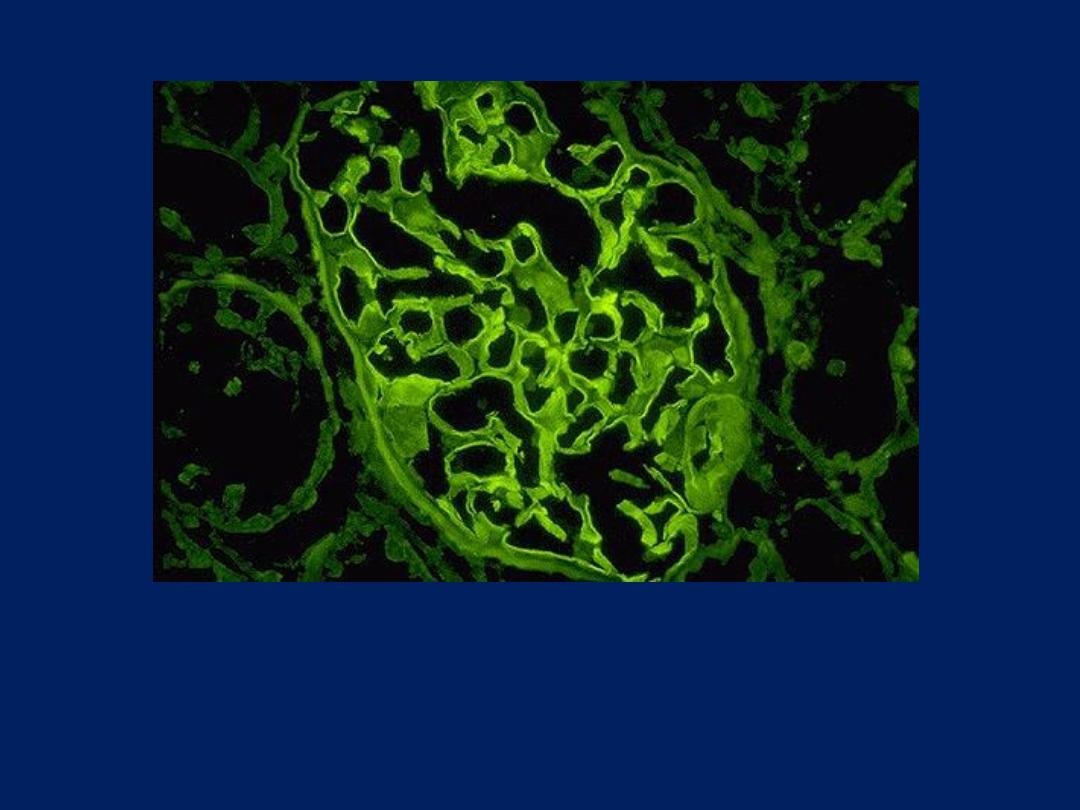
This immunofluorescence micrograph shows positivity with
antibody to IgG has a smooth, diffuse, linear pattern that is
characteristic for glomerular basement membrane antibody with
Goodpasture's syndrome.
Antibody-Mediated (Type II) Hypersensitivity:
Goodpasture's syndrome
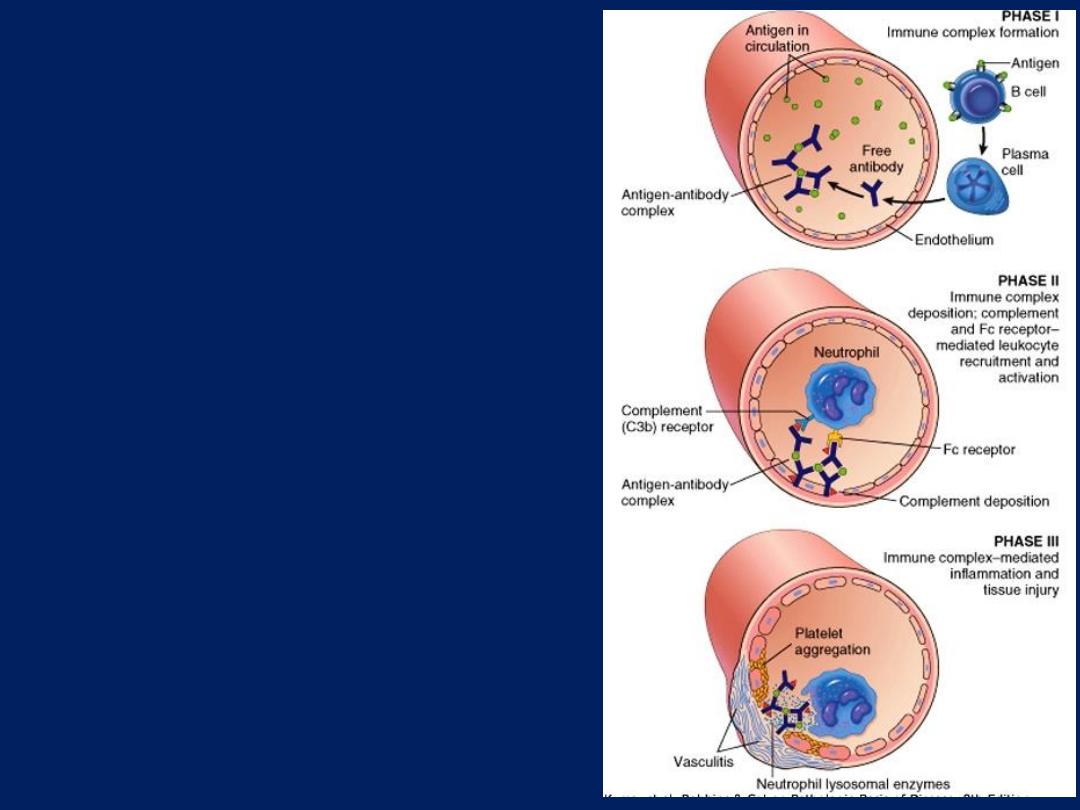
Immune Complex–Mediated
(Type III) Hypersensitivity
Pathogenesis of systemic
immune complex–mediated
disease
(type III hypersensitivity).
The three sequential phases in
the development of immune
complex diseases are shown.
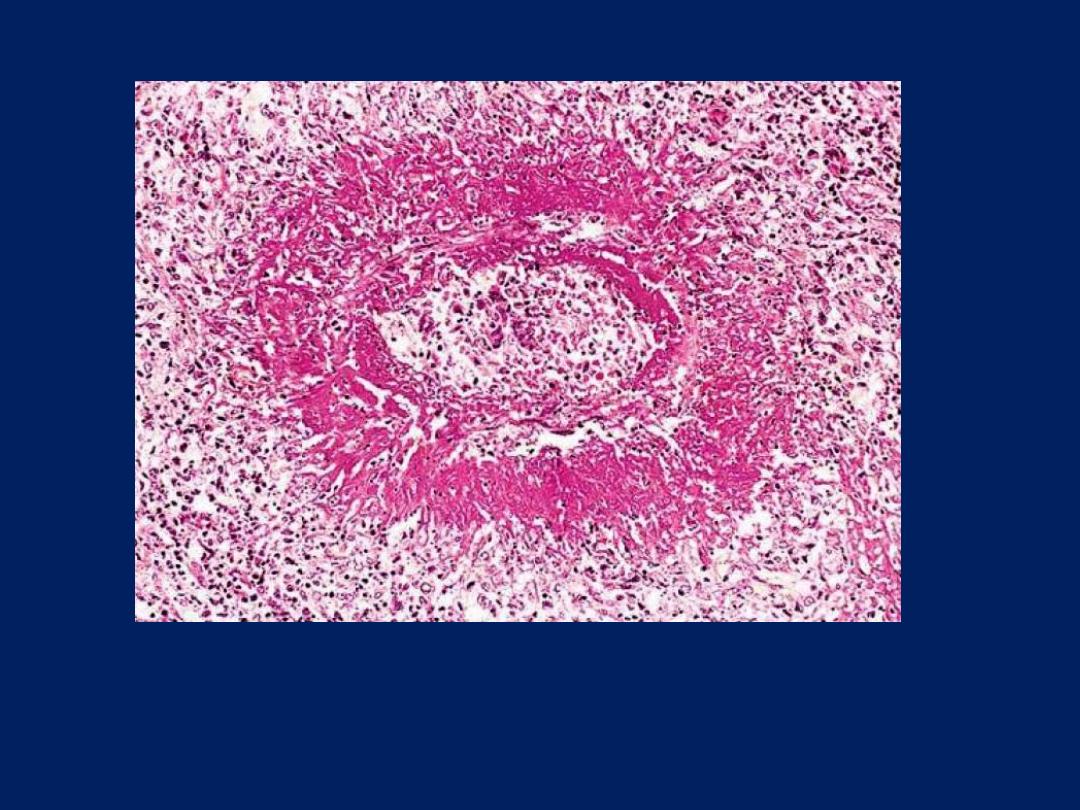
The principal morphologic manifestation of immune complex injury is acute necrotizing
vasculitis, with necrosis of the vessel wall and intense neutrophilic infiltration. The
necrotic tissue and deposits of immune complexes, complement, and plasma protein
produce a smudgy eosinophilic deposit that obscures the underlying cellular detail, an
appearance termed fibrinoid necrosis
Immune Complex–Mediated (Type III) Hypersensitivity:
Vasculitis
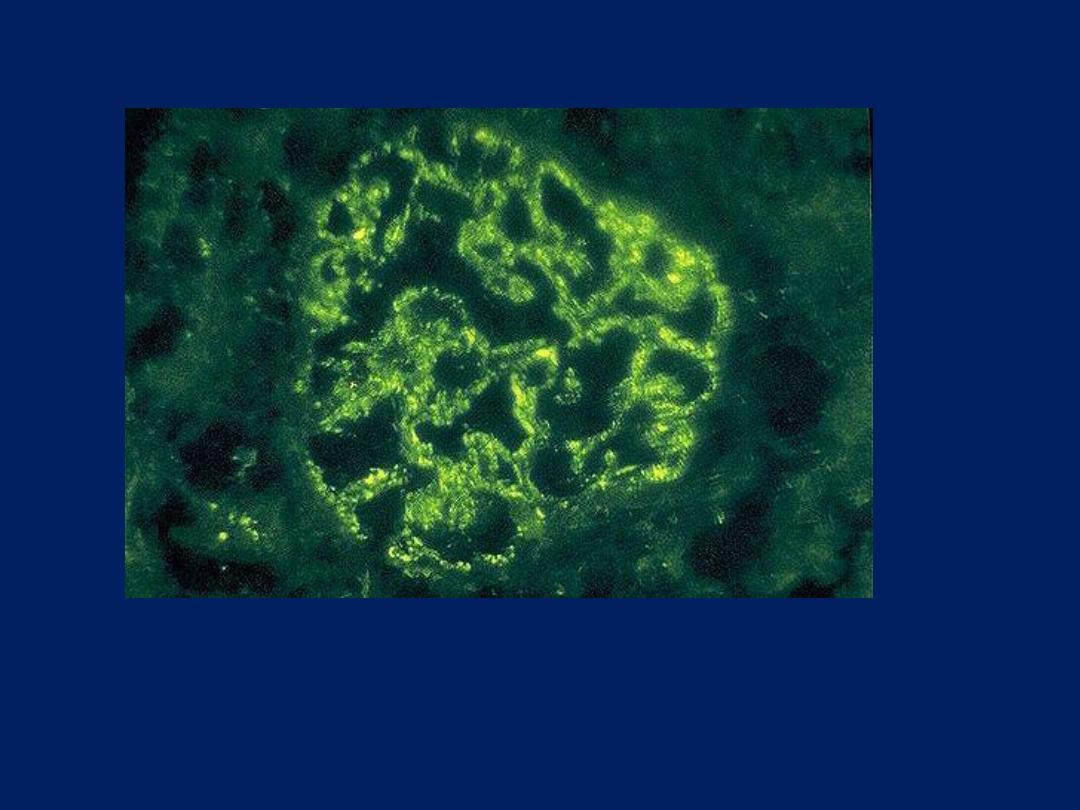
Post-streptococcal glomerulonephritis is immunologically
mediated, and the immune deposits are distributed in the capillary
loops in a granular, bumpy pattern because of the focal nature of
the deposition process.
Immune Complex–Mediated (Type III) Hypersensitivity:
Post-streptococcal glomerulonephritis
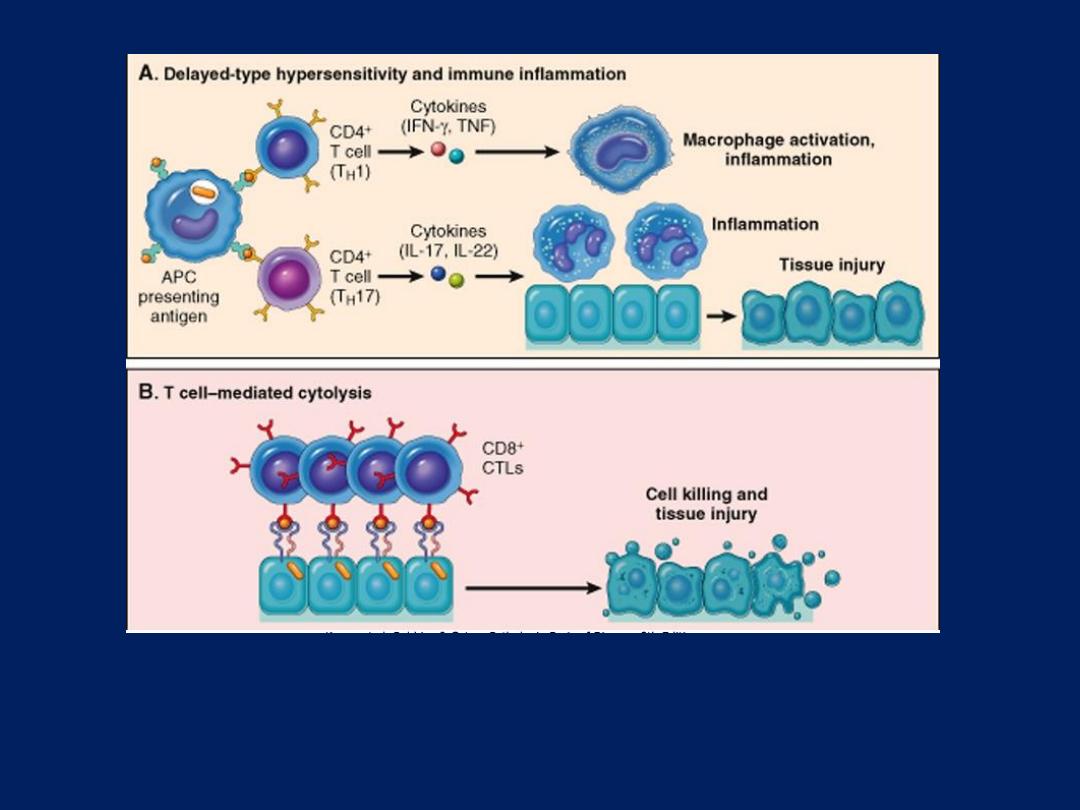
T Cell–Mediated (Type IV) Hypersensitivity
A: In delayed-type hypersensitivity reactions, CD4+ TH1 cells (and sometimes CD8+ T cells respond
to tissue antigens by secreting cytokines that stimulate inflammation and activate phagocytes,
leading to tissue injury. CD4+ TH17 cells contribute to inflammation by recruiting neutrophils (and,
to a lesser extent, monocytes). B: In some diseases, CD8+ cytotoxic T lymphocytes (CTLs) directly
kill tissue cells. APC, antigen-presenting cell.
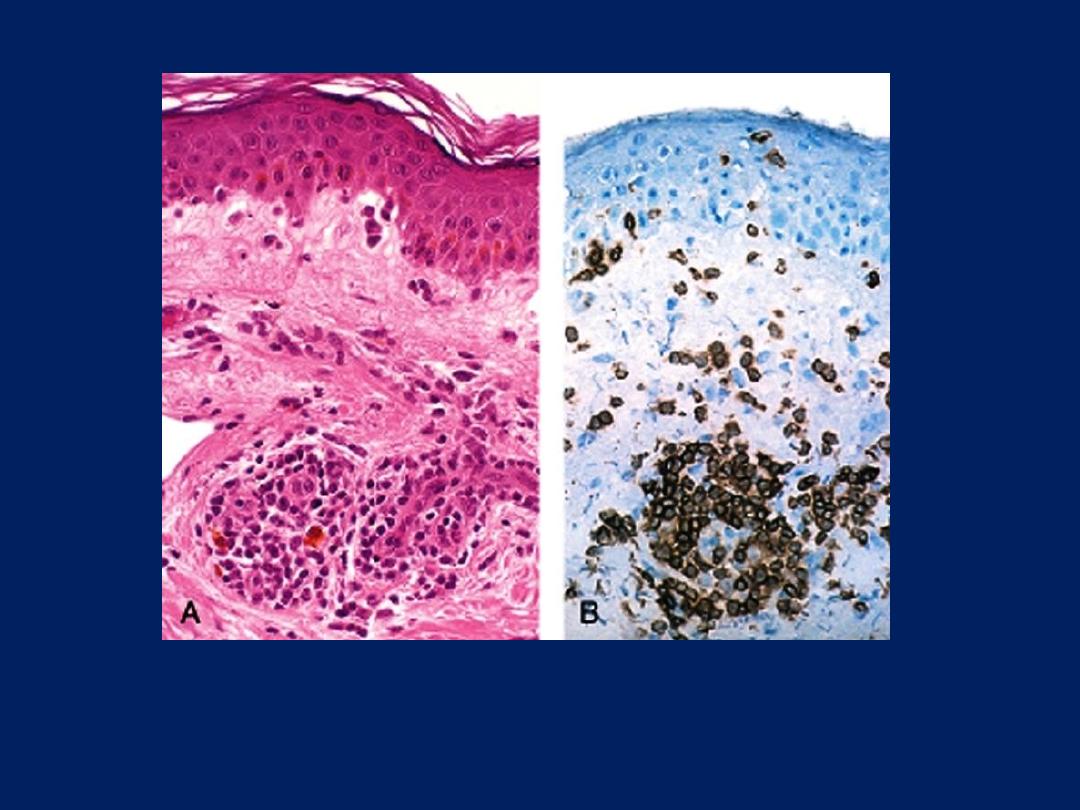
Delayed hypersensitivity reaction in the skin. A: Perivascular infiltration by T
cells and mononuclear phagocytes. B: Immunoperoxidase staining reveals a
predominantly perivascular cellular infiltrate that marks positively with
antibodies specific to CD4.
T Cell–Mediated (Type IV) Hypersensitivity:
Contact dermatitis
