
Blood vessels have a primary function
of nourishing
various organs and tissues of the body by supplying
them with blood.
Vascular diseases are manifested clinically through
three mechanisms that are reflected through the
diseases vessel (s) as:
Progressive narrowing of the lumen
associated with progressive ischemia of the
relevant tissues.
Thrombosis associated with partial or
complete luminal obstruction and/or
embolism.
Aneurysmal dilatation that may eventuate in
rupture with ischemic and destructive
consequences.
Definition
Variants
This generic term refers to a group of disorders
having in common
thickening and loss of elasticity
of arterial walls
and thus leading to
sclerosis
i.e.
hardening of the wall.

There are three morphologic
variants of
arteriosclerosis
that
come under this generic term,
what are they?
1.
Atherosclerosis (the most
frequent and important type)
2.
Medial calcific sclerosis
3.
Arteriolosclerosis
ATHEROSCLEROSIS
This disease is responsible for more deaths and serious
complications than any other disorder.
This is because its prime targets are vital arteries, namely
the
coronaries, cerebral arteries, & the aorta.
Accordingly the major consequences are
1.
Myocardial infarction
2.
Cerebral infarction
3.
Aortic aneurysm
Myocardial infarction alone is responsible for
about
25% of all deaths.
By definition atherosclerosis is “
a disease
primarily of large elastic arteries and medium sized
muscular arteries.
Its basic lesion is the atheroma (fibro-fatty plaque),
which is a raised patch within the intima having a
core of lipid (mainly cholesterol and its esters) and
a cap of fibrous tissue”.
Examples of large elastic arteries are
aorta, carotid,
and the iliac arteries,
& examples of medium-sized
muscular arteries are the
coronaries and popliteal
arteries.
Epidemiology and risk factors
Epidemiological data and that of the risk factors of
atherosclerosis are expressed largely in terms of the
incidence of deaths caused by
ischemic heart disease
(IHD).
This is because atherosclerosis does not by itself
produce signs and symptoms but its prevalence is
detected by its effects on the most commonly
involved arteries, namely the
coronaries.
Epidemiological findings include
A decline in the incidence of deaths from IHD that has started since
1975. This is due to the recognition and avoidance of the risk factors,
better recognition and better management.
Marked geographical variations in the incidence of atherosclerosis-
related IHD.
It is high in Europe and the USA but remarkably low in
Asia (for e.g. the mortality rate from IHD is six times higher in the USA
than that in Japan).
This is probably related to differences in the
life
style and dietary customs
.
The following increase the risk of atherosclerosis
a. Increasing age as death rates from IHD rise with each decade of life.
b. Male gender since myocardial infarction is particularly uncommon in
premenopausal
women.
c. Certain genetic defects:
certain families suffer increased frequency of
heart attacks at an early age. This familial predisposition appears to be
related to
hyperlipidemia
(due for e.g. to genetic defects in lipoprotein
metabolism),
hypertension,
and
diabetes mellitus
. It should be noted
that both hypertension and diabetes also tend to be
familial.
Risk factors that predispose to atherosclerosis
and the resultant IHD can be divided into two
main groups:
Major Risk factors of atherosclerosis
A. Potentially modifiable (controllable)
1.
Diet and hyperlipidemia
2.
Hypertension
3.
Cigarette smoking
4.
Diabetes mellitus
B. Nonmodifiable
1.
Increasing age
2.
Male gender
3.
Family history
4.
Genetic abnormalities
Minor (uncertain risks)
1.
Obesity
2.
Physical inactivity
3.
Stress (type A personality)
4.
High carbohydrate intake
5.
Lipoprotein (a)
6.
Hardened unsaturated fat intake
7.
Chlamydia pneumonia
8.
Hyperhomocystinemia
Diet and Hyperlipidemia
Hyperlipidemia (particularly hypercholesterolemia) and other abnormalities
in lipid metabolism are major risk factors in atherosclerosis
.
The evidences linking hypercholestrolemia to atherosclerosis
include the following:
1
.
Atherosclerotic plaques are rich in cholesterol and its esters. These are
largely derived from lipoproteins of the blood.
2. Atherosclerotic lesions can be induced in experimental animals by
feeding them diets that raise their plasma cholesterol levels.
3. Genetic disorders that cause severe hypercholesterolemia lead to
premature atherosclerosis, often fatal in childhood.
4. Acquired diseases associated with hypercholesterolemia (as part of their
manifestations) for e.g
. nephrotic syndrome and hypothyroidism
, are
associated with increasing risk of atherosclerosis
5. Populations having relatively high levels of serum cholesterol show
higher mortality from IHD.
6. Treatment with diet and cholesterol-lowering drugs reduces
cardiovascular mortality in patients with hypercholesterolemia
.
High dietary intake of cholesterol and saturated fats, e.g. those
present in egg yolk, animal fats, and butter, raises plasma
cholesterol level.
The higher the level of serum cholesterol the higher the risk
particularly, with levels exceeding 200 mg/dl.
The most striking association is with elevated levels of
low-
density lipoprotein (LDL).
This is the lipoprotein moiety richest
in cholesterol.
In fact the major component of the total serum cholesterol
associated with increased risk is LDL.
Hypertriglyceridemia also appears to increase the risk.
In contrast, serum levels of high-density lipoprotein (HDL) are
inversely related to the risk. It is believed that HDL mobilizes
cholesterol from developing atheromas and transports it to the
liver to be eventually excreted into the bile.
Exercise also raises the HDL level, whereas obesity and
smoking lower it.
Hypertension is a major risk factor at all ages.
Elevated blood pressure accelerates the process
of atherosclerosis and increases the incidence of
IHD and cerebrovascular diseases.
Men over the age of
45 years
with a blood
pressure exceeding
170/95 mm Hg
have more
than
five-fold greater risk of IHD than
normotensives.
Antihypertensive therapy reduces the incidence
of atherosclerosis-related diseases, particularly
IHD and CVA (cerebrovascular accidents;
strokes).
Cigarette smoking is a
well-established risk
factor.
It is the most important avoidable cause of IHD.
Cigarette smoking is the main cause responsible
for the relatively recent increase in the incidence
and severity of atherosclerosis in
women
.
In the context of IHD, two facts are related to
smoking
a. It increases the incidence of sudden death among
those with IHD
b. Cessation of smoking in high-risk individuals is
followed within a few years by a reduction in the
risk of dying from IHD.

Q1. Diabetics show more advanced
atherosclerotic lesions than age-matched
nondiabetics, why?
Q2. What is the minimum duration of
diabetes required for the development of
clinically significant atherosclerosis?
Diabetes mellitus
: diabetics are more susceptible, compared
with nondiabetics to atherosclerosis-related diseases and
in particular
IHD
,
cerebrovascular accidents (CVA) and
gangrene of lower extremities.
This is probably related to
1. Hyperlipidemia, which is seen in up to 50% of diabetics
2. Increased platelets adhesiveness; predisposing to
thrombotic episodes.
3. Some diabetics tend to be obese and hypertensive; thus
have increased tendency to develop severe atherosclerosis.
All diabetics who have had the disease for at least
ten years, irrespective of the age of onset, are likely
to develop clinically significant atherosclerosis.
d
Enumerate, in descending order of severity,
the most heavily involved arteries in the body
by atherosclerosis.

1.
Abdominal aorta
2.
Coronaries
3.
Popliteal arteries
4.
Descending thoracic aorta
5.
Internal carotid arteries
6.
Arteries forming the circle of Willis at the
base of the brain.
•
Atheromatous plaques are patchy in distribution and
may involve the arterial wall in asymmetrical fashion
i.e. involve one portion of the wall circumference
more severely than elsewhere and as such produce
eccentric lesions.
Pathology of atherosclerosis
Gross features
The basic lesion in atherosclerosis is a focal intimal
thickening termed atheromatous plaque or fibro-fatty
plaque.
Each plaque is white to whitish yellow elevation up to 1.5
cm in diameter; adjacent plaques, however, may fuse to
form larger plaques.
The superficial portion of these lesions (i.e. facing the
lumen) tends to be firm and white; this is the fibrous cap,
whereas the deep portion is yellow and soft and
represents the lipid component
. It is from this yellow soft
debris, the term
atheroma is derived (Greek word for
gruel).
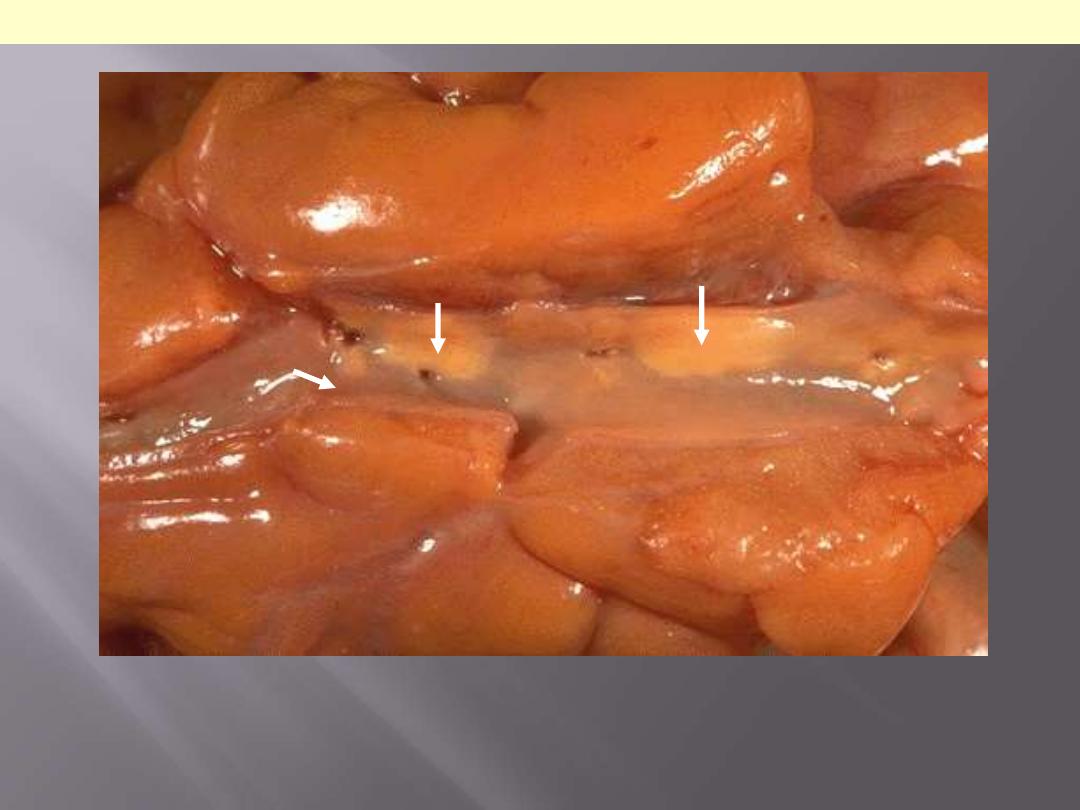
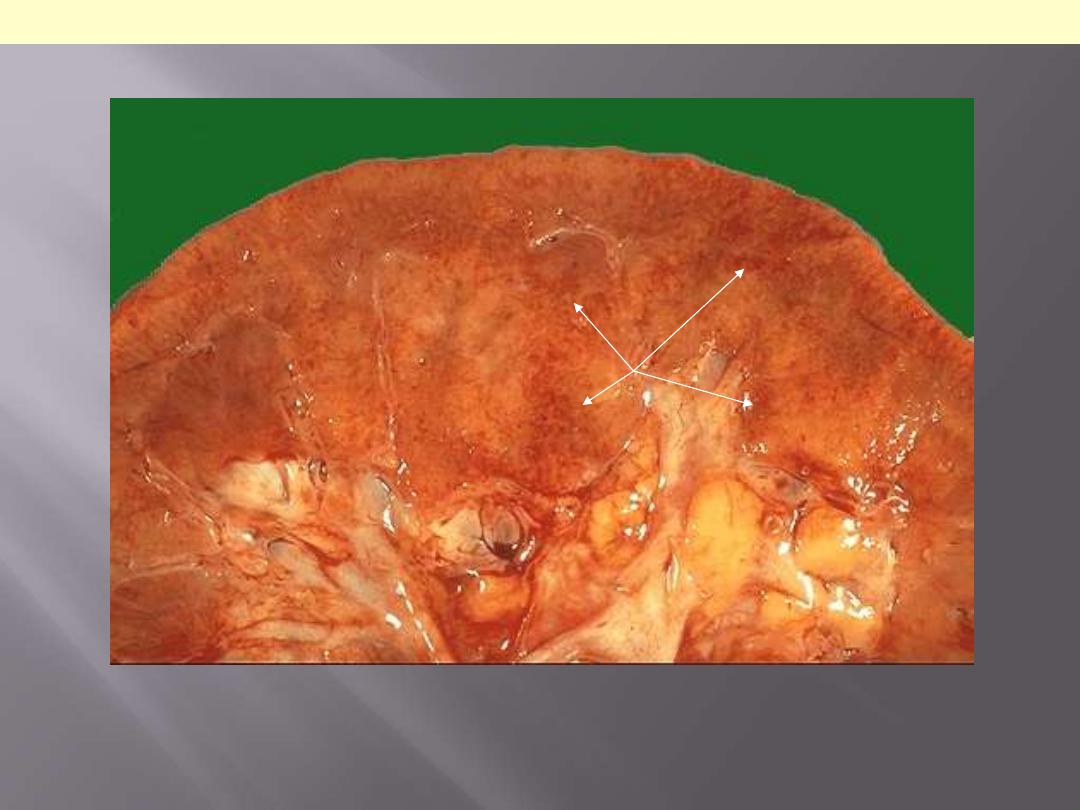
A coronary artery has been opened longitudinally. The coronary extends from left to right
across the middle of the picture and is surrounded by epicardial fat. This coronary shows
only mild atherosclerosis, with only an occasional yellow-tan lipid plaques (arrows) and no
narrowing.
Mild degree of coronary athersclerosis
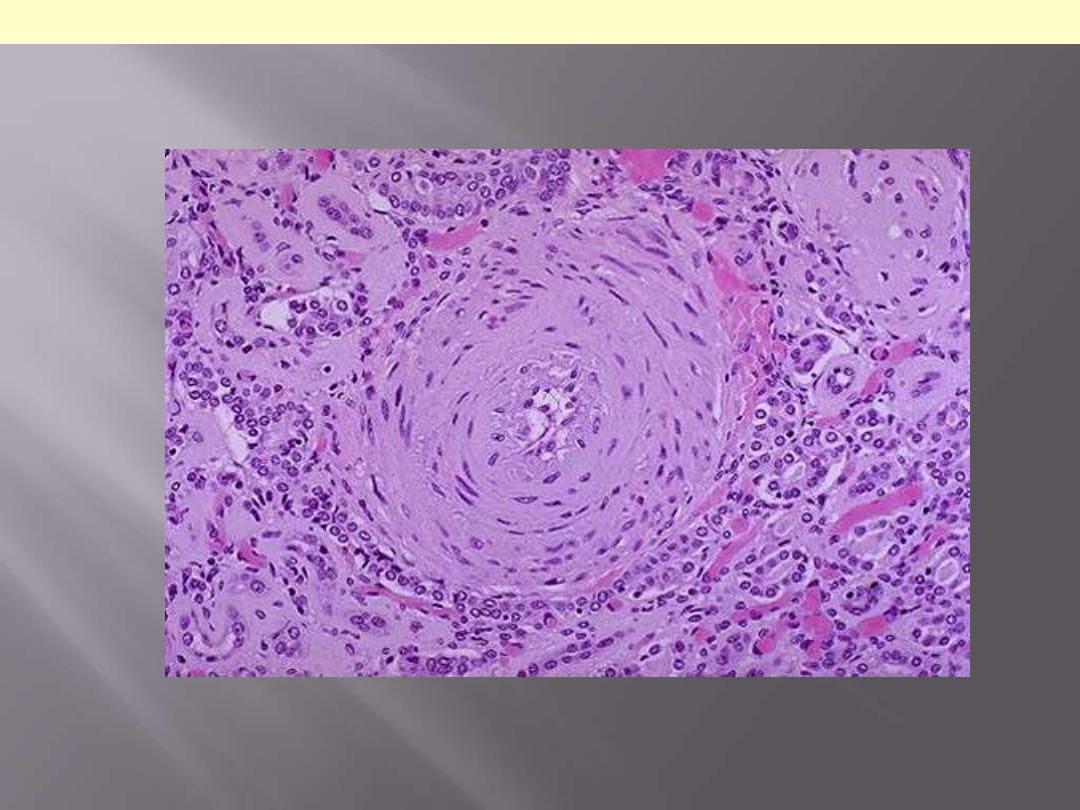
Microscopic features
The superficial cap is composed of smooth muscle cells and
relatively dense collagen fibers.
Just beneath and to the sides of the cap there is a cellular area
made up of variable mixture of macrophages, smooth muscle
cells and T-lymphocytes.
Foam cells. Deep to the cellular area is a necrotic core; consisting
of lipid material, cholesterol clefts, cellular debris and lipid-
laden cells
Finally, especially around the edges of the lesion there are
proliferating small, thin-walled blood vessels.
The above mentioned components may occur in varying
proportions in different plaques, for e.g. some plaques may be
composed mostly of smooth muscle cells and fibrous tissue
(fibrous plaques).
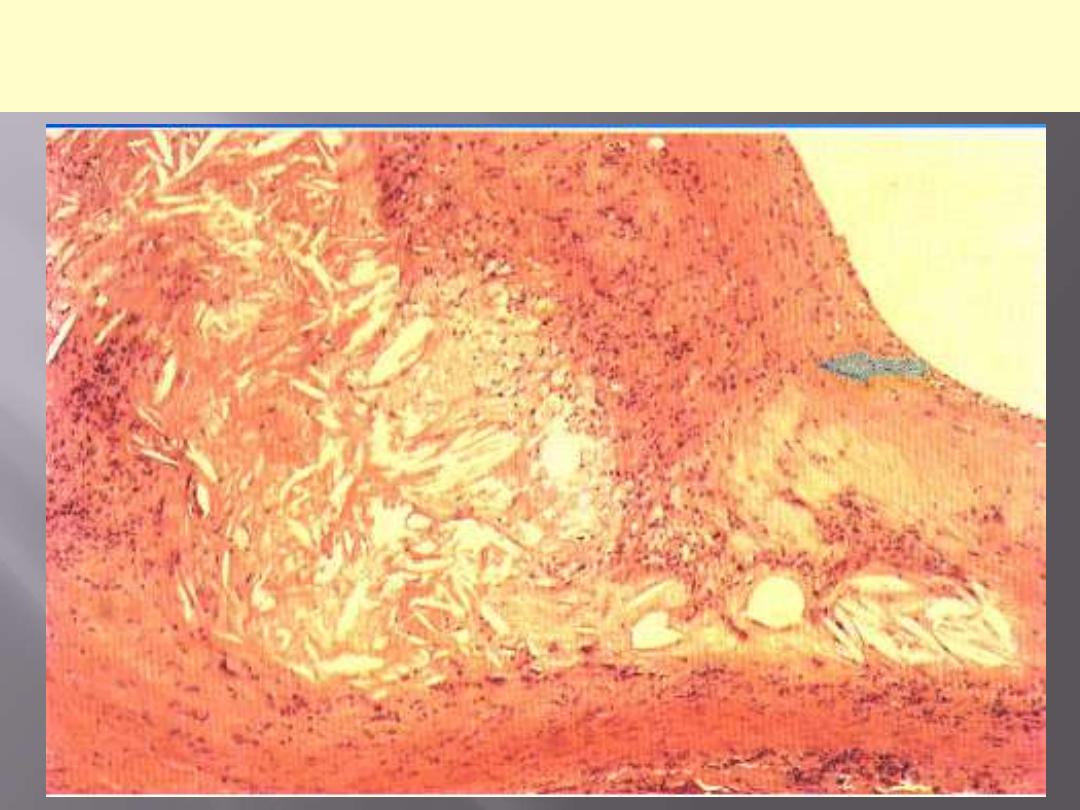
This is a microscopic section through an
atheromatous plaque. Describe.
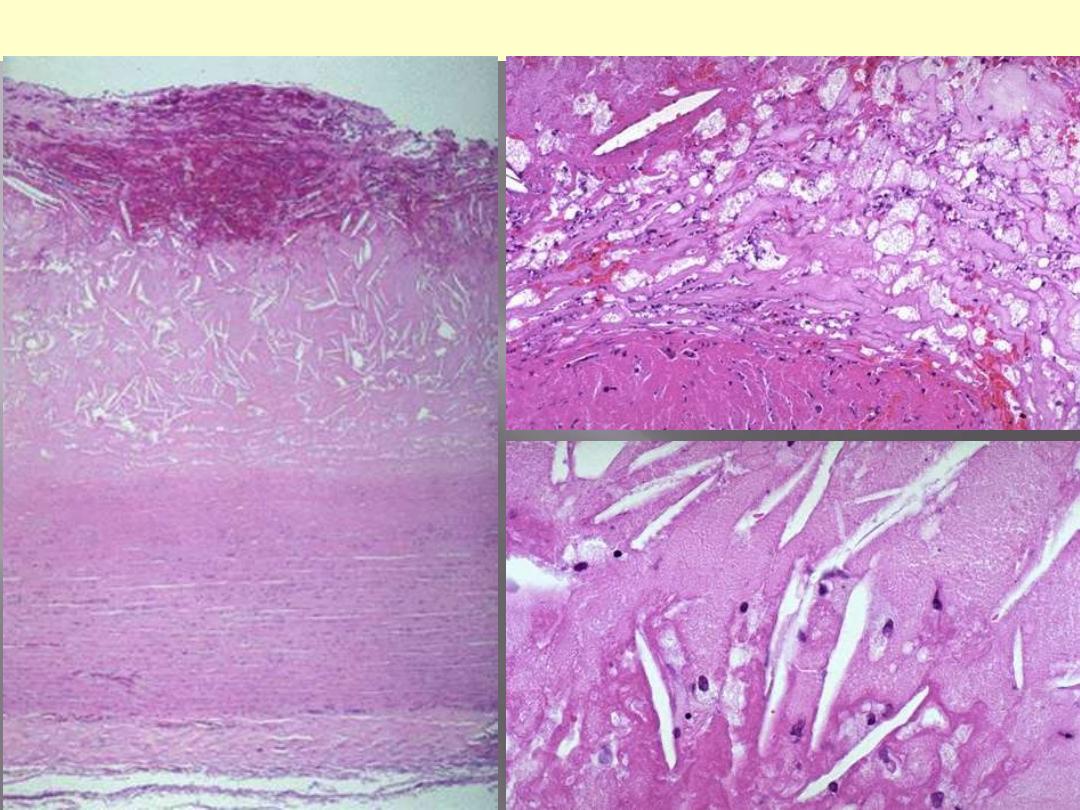
Three microscopic pictures LP, MP & HP. Describe
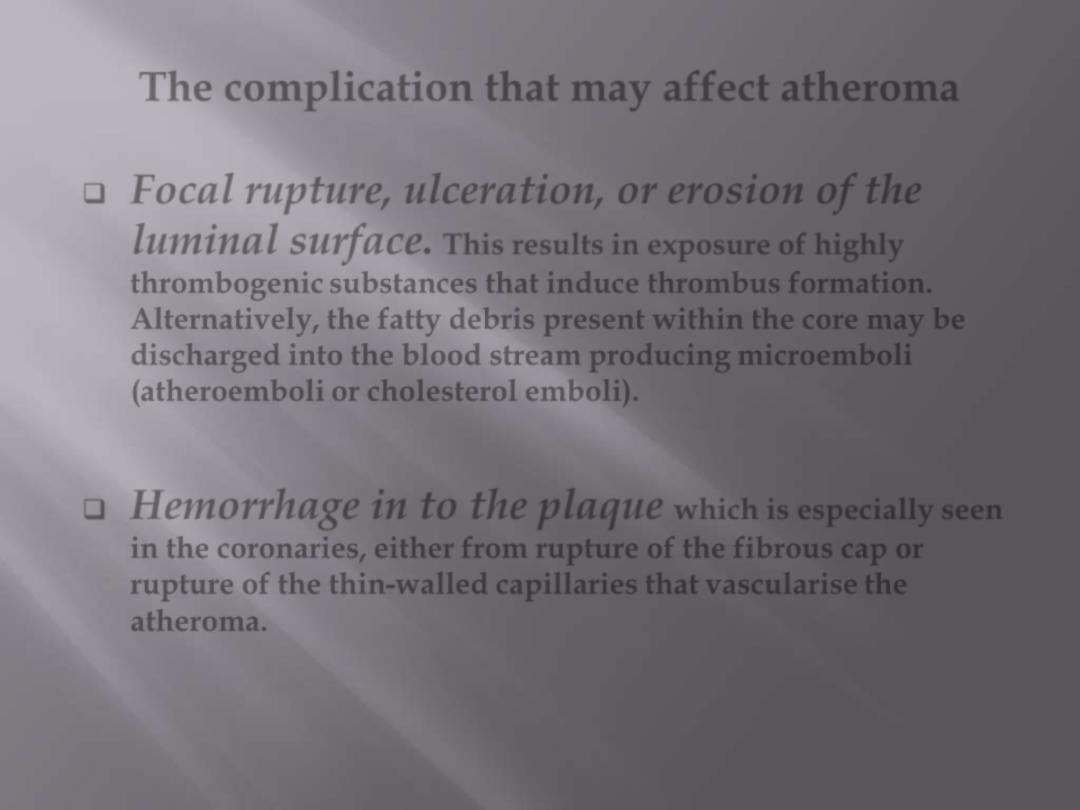
The complication that may affect atheroma
Focal rupture, ulceration, or erosion of the
luminal surface.
This results in exposure of highly
thrombogenic substances that induce thrombus formation.
Alternatively, the fatty debris present within the core may be
discharged into the blood stream producing microemboli
(atheroemboli or cholesterol emboli).
Hemorrhage in to the plaque
which is especially seen
in the coronaries, either from rupture of the fibrous cap or
rupture of the thin-walled capillaries that vascularise the
atheroma.
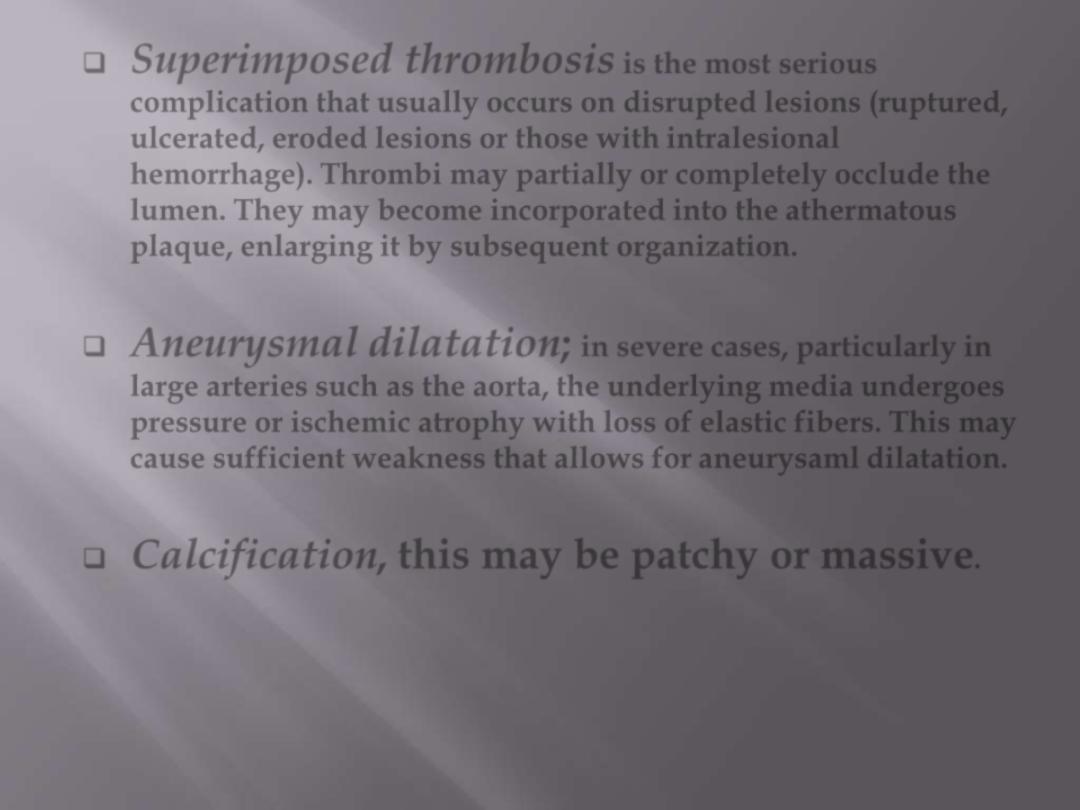
Superimposed thrombosis
is the most serious
complication that usually occurs on disrupted lesions (ruptured,
ulcerated, eroded lesions or those with intralesional
hemorrhage). Thrombi may partially or completely occlude the
lumen. They may become incorporated into the athermatous
plaque, enlarging it by subsequent organization.
Aneurysmal dilatation;
in severe cases, particularly in
large arteries such as the aorta, the underlying media undergoes
pressure or ischemic atrophy with loss of elastic fibers. This may
cause sufficient weakness that allows for aneurysaml dilatation.
Calcification, this may be patchy or massive
.

This is severe atherosclerosis of the aorta in which the atheromatous plaques have
undergone ulceration along with formation of overlying mural thrombus (arrows).
Atherosclerosis aorta: ulcerations with superadded thrombosis

This is coronary atherosclerosis with the complication of hemorrhage into atheromatous
plaque (arrow). Such hemorrhage acutely may narrow the arterial lumen.
Coronary atherosclerosis: plaque hemorrhage

There is a severe degree of narrowing in this coronary artery. It is "complex" in that there is
a large area of calcification on the lower right, which appears bluish on this H&E stain.
Complex atheroma have calcification, thrombosis, or hemorrhage. Such calcification would
make coronary angioplasty difficult.
Stenosing coronary atheroma with calcification
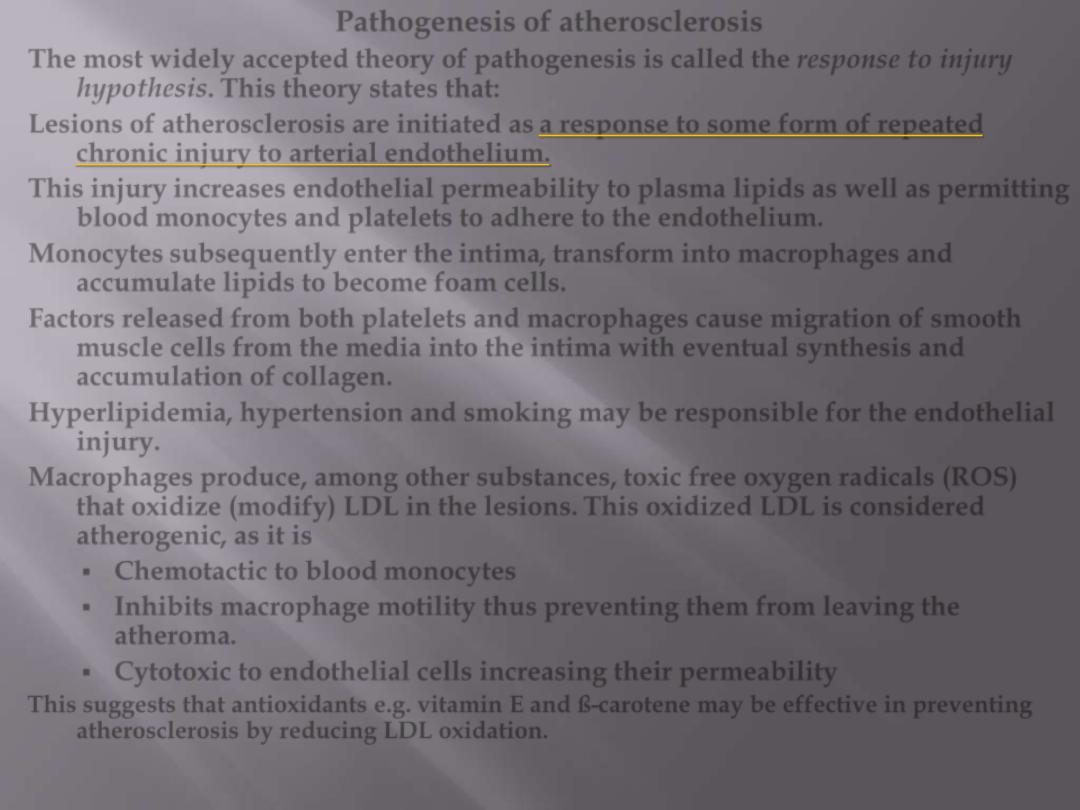
Pathogenesis of atherosclerosis
The most widely accepted theory of pathogenesis is called the
response to injury
hypothesis.
This theory states that:
Lesions of atherosclerosis are initiated as
a response to some form of repeated
chronic injury to arterial endothelium.
This injury
increases endothelial permeability to plasma lipids as well as permitting
blood monocytes and platelets to adhere to the endothelium.
Monocytes subsequently enter the intima, transform into macrophages and
accumulate lipids to become foam cells.
Factors released from both platelets and macrophages cause migration of smooth
muscle cells from the media into the intima with eventual synthesis and
accumulation of collagen.
Hyperlipidemia, hypertension and smoking may be responsible for the endothelial
injury.
Macrophages produce, among other substances, toxic free oxygen radicals (ROS)
that oxidize (modify) LDL in the lesions.
This oxidized LDL is considered
atherogenic, as it is
Chemotactic to blood monocytes
Inhibits macrophage motility thus preventing them from leaving the
atheroma.
Cytotoxic to endothelial cells increasing their permeability
This suggests that antioxidants e.g. vitamin E and ß-carotene may be effective in preventing
atherosclerosis by reducing LDL oxidation.
Clinical significance of atherosclerosis
Atherosclerosis cause clinical disease through the
following
1. Slow, progressive narrowing of the arterial lumen that
result in chronic ischemia of the relevant tissues.
2. Sudden occlusion of the lumen by superimposed
thrombosis or hemorrhage into the atheroma.
This may produce severe ischemia that if prolonged may
terminate in infarction.
3. Providing a site for thrombosis and then embolism.
4. Weakening of the wall of an artery, causing
aneurysmal dilatation with subsequent rupture.
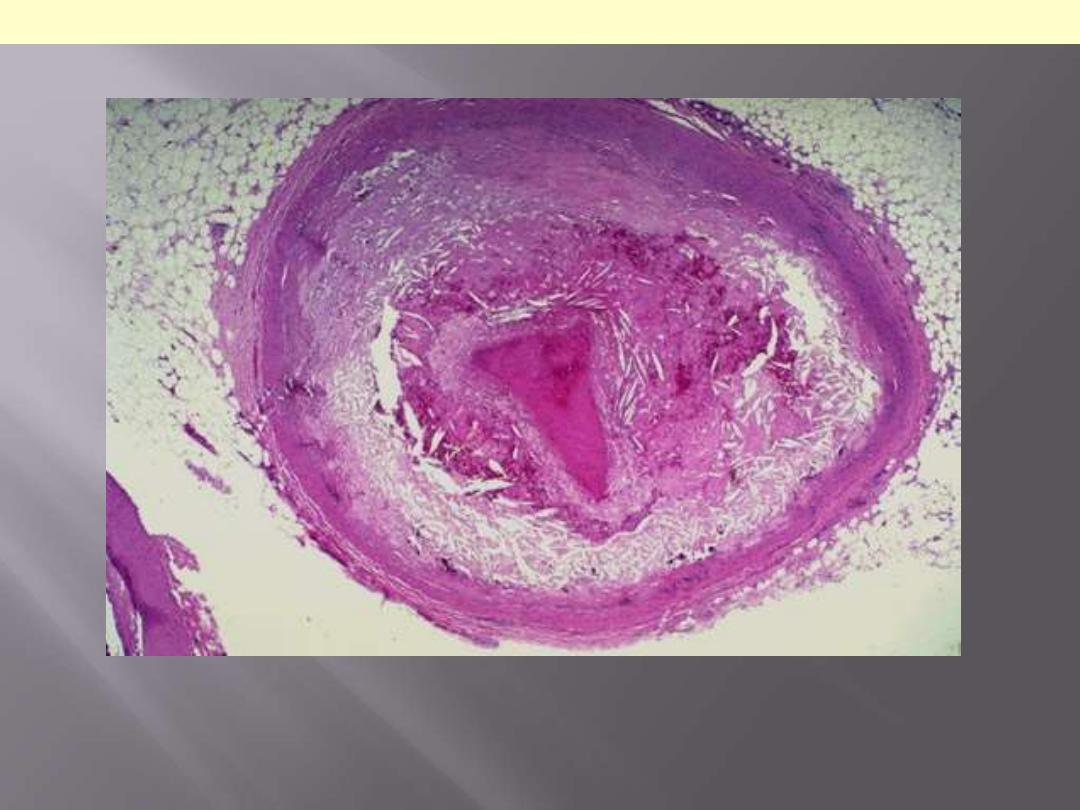
There is a pink to red recent thrombosis in this narrowed coronary artery. The open, needle-
like spaces in the atheromatous plaque are cholesterol clefts.
Coronary atherosclerosis with superimposed occlusive thrombosis

Atherosclerotic involvement of medium
sized arteries produces a set of clinical
features that differ from those arising
from involvement of large arteries.
Explain
In large arteries
Large mural thrombi
peripheral emboli.
Aneurysmal dilatation
rupture
Rupture of the atheroma cholesterol emboli.
In smaller arteries
Narrowing of the lumen
chronic ischemia
Superadded thrombosis or plaque hemorrhage
occlusion of the vessel

What effects does hypertension have on
blood vessels?
(Hypertensive vascular disease)
Hypertension is the most important cause of this group of vascular
diseases. Hypertension has the following effects on blood
vessels
1. It accelerates the process of atherosclerosis.
2. Causes structural changes in the blood vessel wall that
predisposes to
Aortic dissection.
Cerebrovascular hemorrhage.
3. Induce changes in arterioles referred to as arteriolosclerosis.
There are two forms of arteriolosclerosis;
hyaline &
hyperplastic

Arteriolosclerosis is typically seen in the kidneys. One form, called hyaline
arteriolosclerosis, is demonstrated by the markedly thickened arteriole to the lower right of
this glomerulus with PAS stain. Hyaline arteriolosclerosis is seen in the elderly, but more
advanced lesions are seen in persons with diabetes mellitus and/or with hypertension.
Hyaline arterioloscelrosis Kidney

The smaller arterioles in the kidney have
become thickened and narrowed. This leads to
patchy ischemic atrophy with focal loss of
parenchyma that gives the surface of the
kidney the characteristic granular appearance
as seen here.
Benign nephrosclerosis
In malignant nephrosclerosis, the kidney demonstrates focal small hemorrhages. This is
due to an accelerated phase of hypertension in which blood pressures are very high (such
as 300/150 mm Hg).
Malignant neophrosclerosis
Onion-skin concentric, laminated thickening of the arteriolar wall with progressive
narrowing of the lumen.
Hyperplastic arterilosclerosis
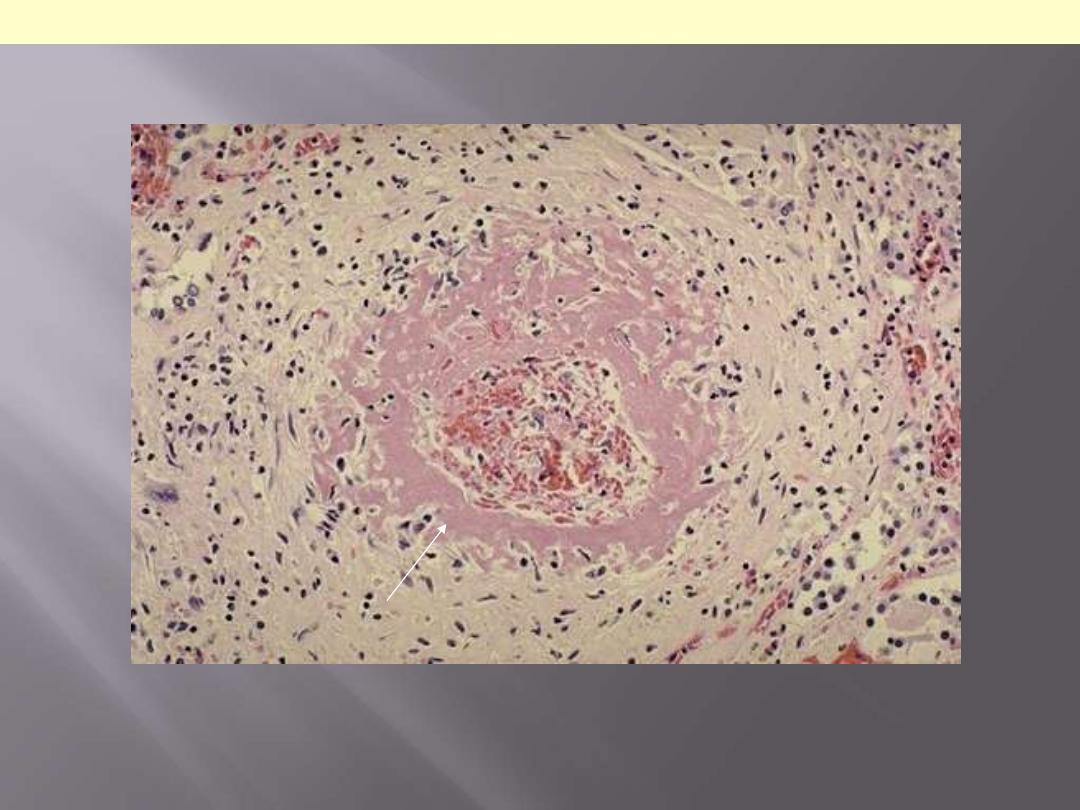
One complication of hyperplastic arteriolosclerosis with malignant hypertension is fibrinoid
necrosis, as seen here in a renal arteriole. Rupture of the affected arterioles lead to grossly
visible minute hemorrhages.
Hyperplastic arterilosclerosis with fibrinoid necrosis
Morphological classification
Berry
Saccular
Fusiform
Etiological classification
Atherosclerosis
Cystic medial degeneration
Syphilis
Vasculitides
Trauma
Congenital defects
Infections
The two most important causes of aortic aneurysms are
1.
atherosclerosis
2.
cystic medial degeneration
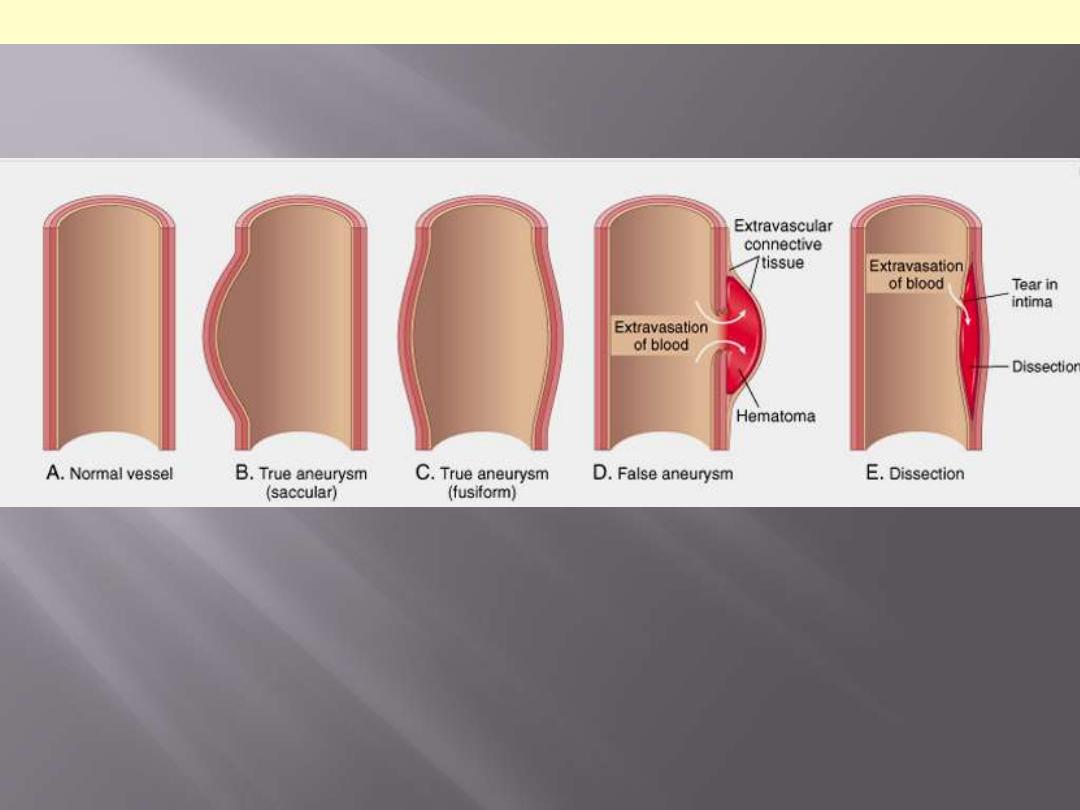
A. Normal vessel. B, True aneurysm, saccular type. The wall focally bulges outward and
may be attenuated but is otherwise intact. C, True aneurysm, fusiform type. There is
circumferential dilation of the vessel, without rupture. D, False aneurysm. The wall is
ruptured, and there is a collection of blood (hematoma) that is bounded externally by
adherent extravascular tissues. E, Dissection. Blood has entered (dissected) the wall of the
vessel and separated the layers. Although this is shown as occurring through a tear in the
lumen, dissections can also occur by rupture of the vessels of the vaso vasorum within the
media.
Morphological types of aneurysms
Most frequent of intracranial aneurysms
Most frequent cause of subarachnoid hemorrhage
2% of general population have them
Thin-walled bright red out-pouching
Occur at arterial branch points along the circle of
Willis
Pathogenesis: congenital defect of the media
Rupture most frequent in age group of 40-50 yr
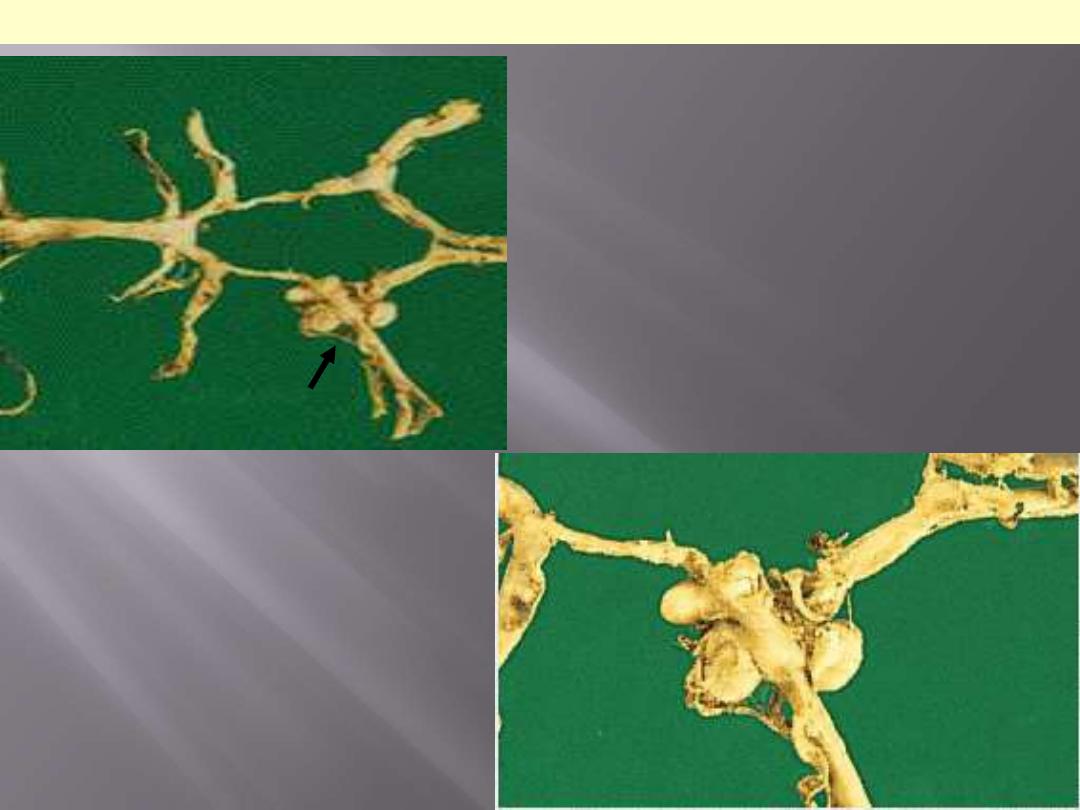
Circle of Willis with anterior, middle and
posterior cerebral arteries linked by
communicating vessels. Berry aneurysms are
seen arising where the internal carotid
bifurcates into middle and anterior cerebral
arteries (arrow).
Berry aneurysms
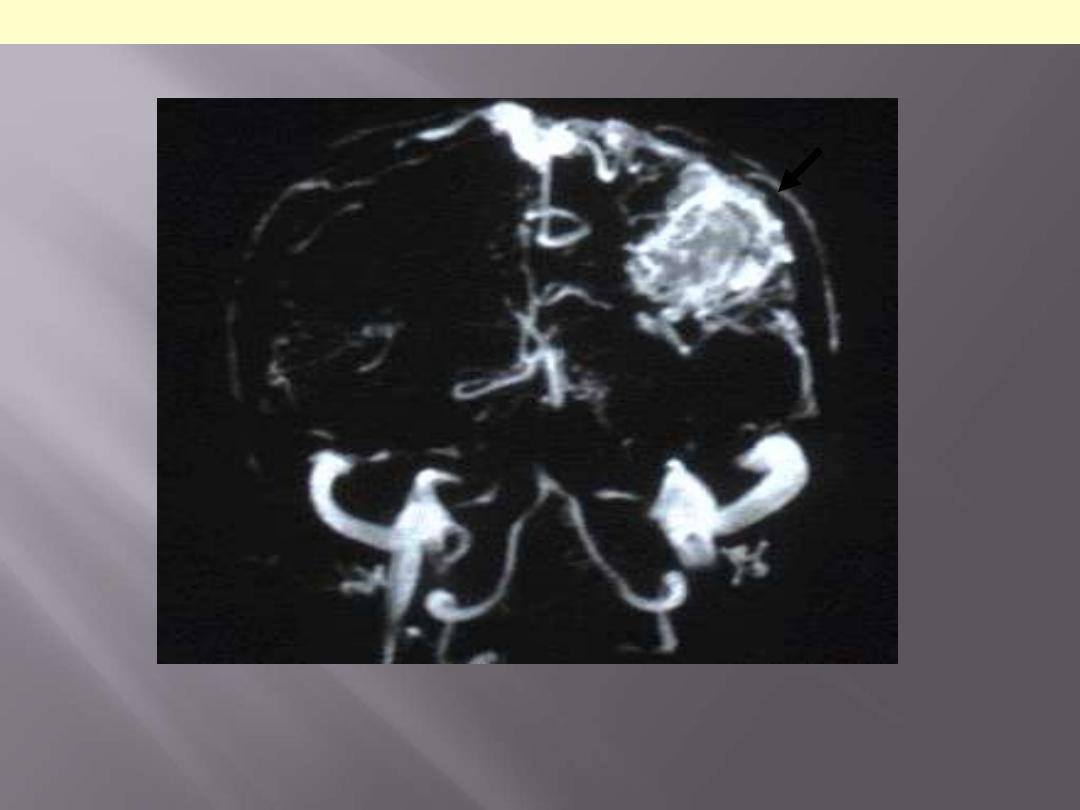
There is a large abnormal mass of vessels in the parietal lobe (arrow). Such abnormal
vessels are prone to bleeding.
AVM (MRI of brain)
There is a mass of irregular, tortuous vessels over the left posterior parietal region. This is
one cause for hemorrhage, particularly in persons aged 10 to 30 years.
AVM Brain
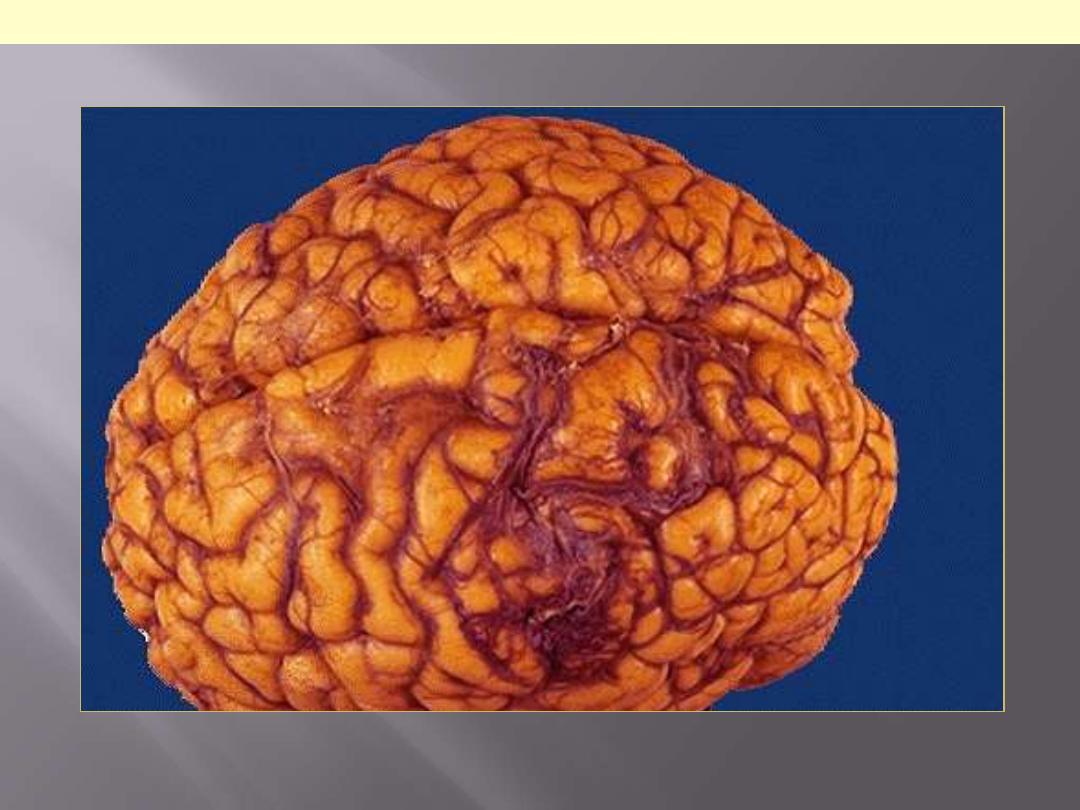
Blood is present in the sub-arachnoid space over the cerebellum. in this case the aneurysm
was arising at the tip of the basilar artery.
Ruptured Berry aneurysm with subarachnoid Hge
most frequent
arterial wall thinning
abdominal aorta
usually fusiform
contains atheromatous ulcers covered by mural thrombi
emboli
Kidney
lower limbs
Mycotic AAA
- infected atherosclerotic aneurysm that has become infected
- bacteremia complicating salmonella gastroenteritis
- rapid course
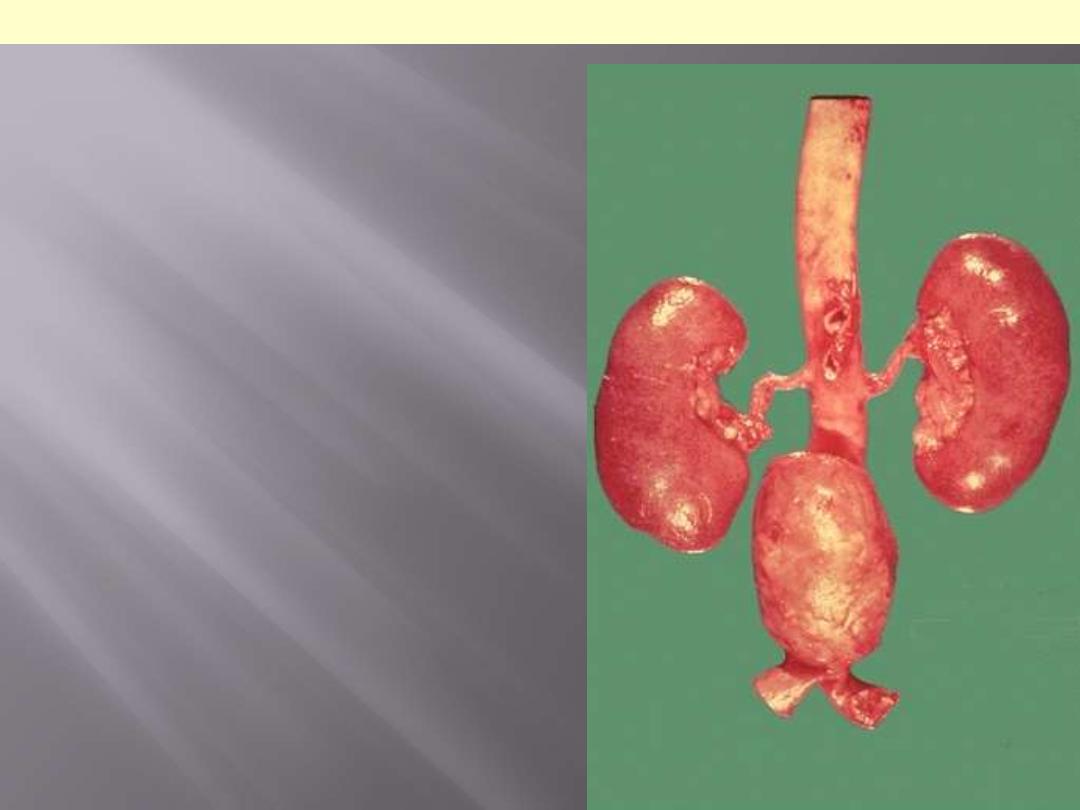
A large "bulge" appears just above the aortic
bifurcation. Such aneurysms are prone to
rupture when they reach about 6 to 7 cm in size.
They may be felt on physical examination as a
pulsatile mass in the abdomen. Most such
aneurysms are located below the renal arteries
so that surgical resection can be performed
with placement of a dacron graft.
Atherosclerotic aneurysm of the abdominal aorta
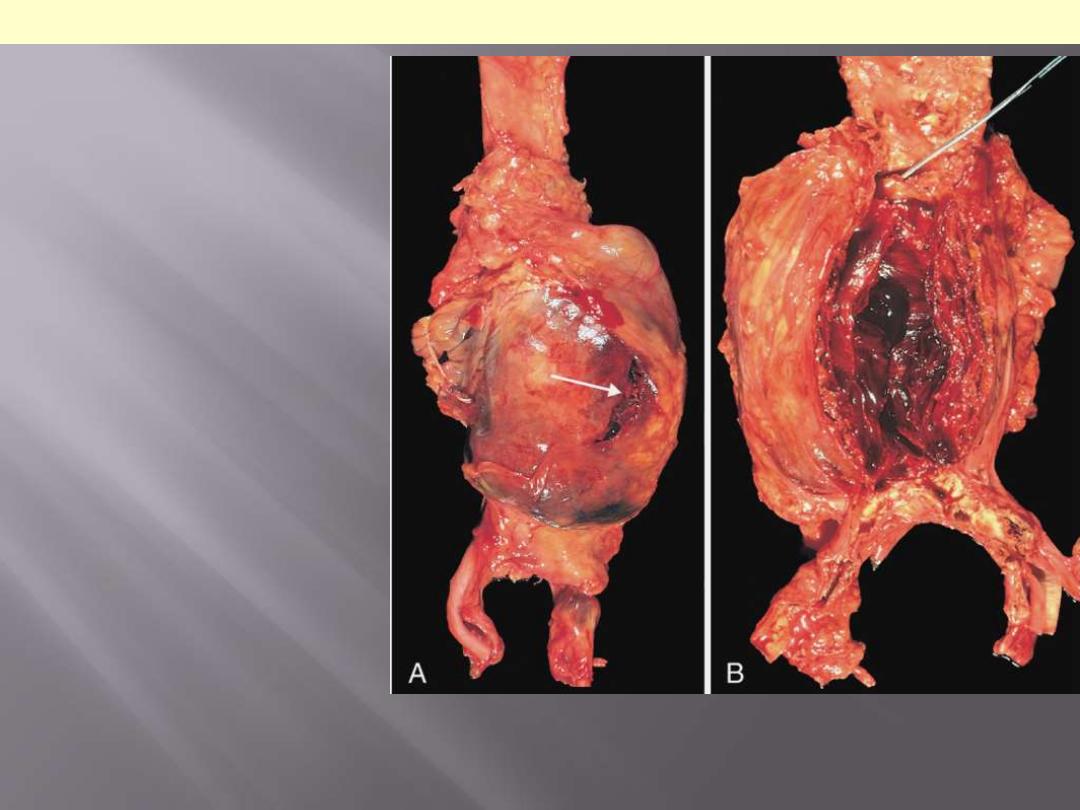
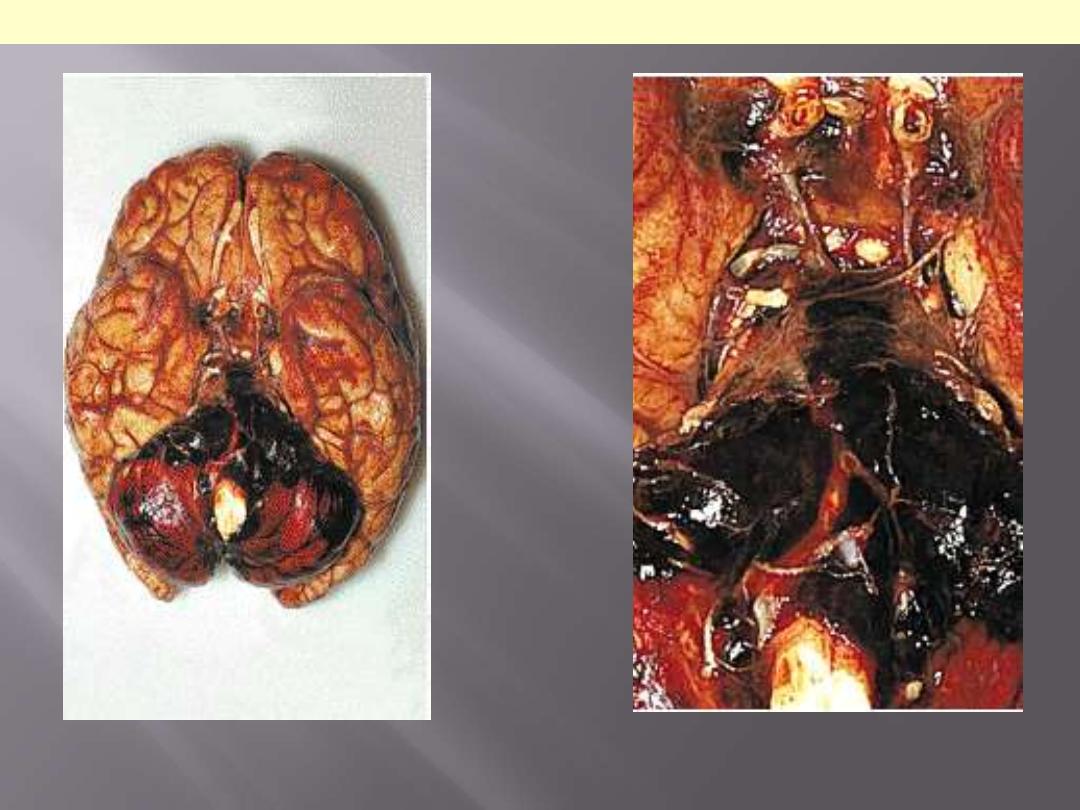
A, External view, gross
photograph of a large aortic
aneurysm that ruptured
(arrow). B, Opened view, with
the location of the rupture
tract indicated by a probe.
The wall of the aneurysm is
exceedingly thin, and the
lumen is filled by a large
quantity of layered but largely
unorganized thrombus.
Abdominal aortic aneurysm
The clinical effects of aortic aneurysm include
Rupture in to the peritoneal cavity
or retroperitoneum with massive
or fatal hemorrhage.
Pressure on adjacent structures
leading for e.g. obstruction of a
ureter or erosion of vertebrae.
Occlusion of a vessel
either by direct pressure or through intramural
thrombus formation e.g. vertebral branches supplying spinal cord.
Embolism from the atheroma or mural thrombus.
Creation of abdominal mass
that may be confused with a tumor.
Prosthetic grafts should replace large aneurysms (> 5 cm in diameter)
to avoid the possibility of rupture.

This aorta has been opened longitudinally to reveal an area of fairly limited dissection that is
organizing. The red-brown hematoma can be seen in on both sides of the section as it
extends around the aorta. The dissection creates a "double lumen" to the aorta. This aorta
shows in addition severe atherosclerosis.
Aortic dissection
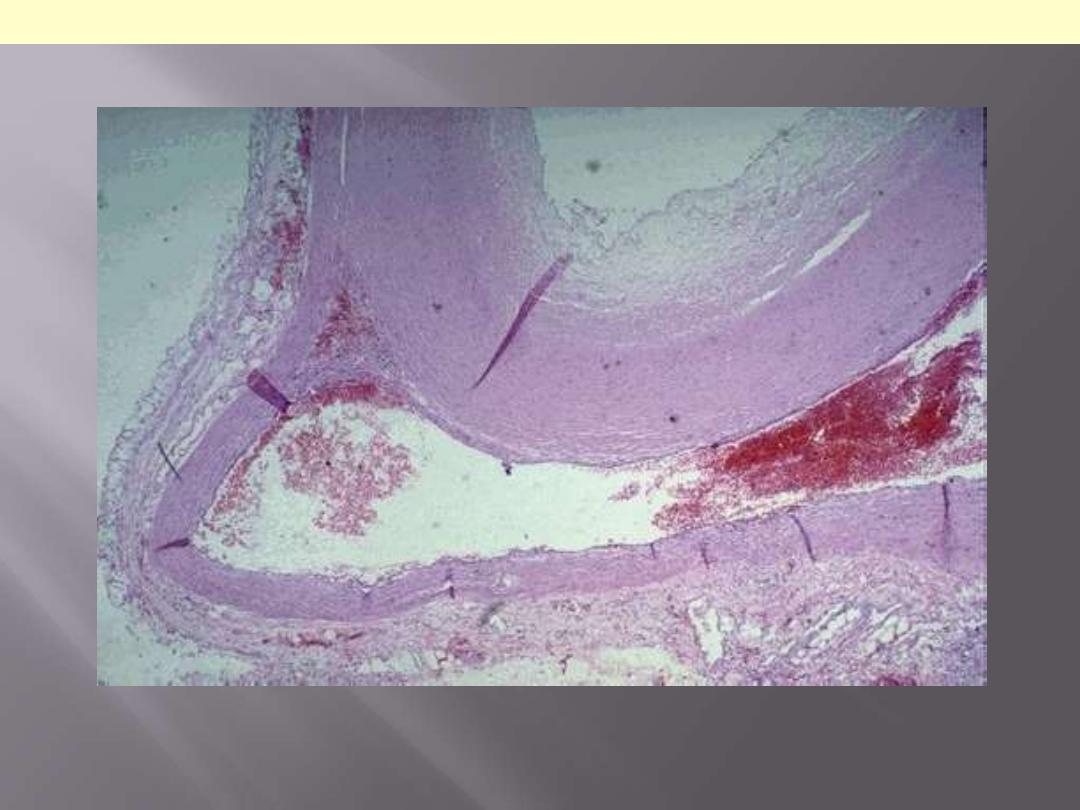
The dissection goes into the muscular wall creating an aorta with double lumina.
Aortic dissection
Original lumen
Dissection

Aortic dissection may have the
following consequences
Rupture into any of the three body
cavities
Extension of dissection
Retrograde dissection
Rupture in the lumen of the aorta
through a second distal tear
Varicose veins +
phlebothrombosis =
90% of venous diseases.

Note the prominently dilated &
tortuous veins below & above the
knee
Varicose veins of the leg
Disabling complications include
Persistent edema
Stasis dermatitis
Varicose ulcers.
Benign tumors and tumor-like conditions
Intermediate
Malignant
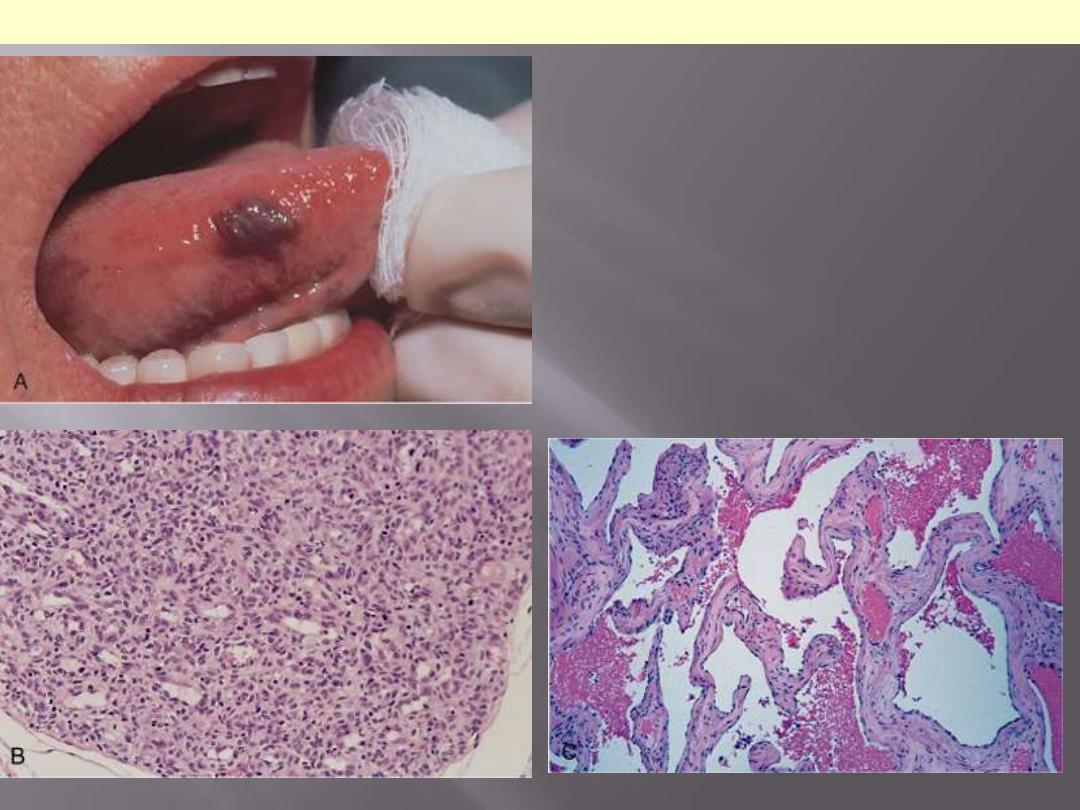
A, Hemangioma of the tongue. B, Histology
of juvenile capillary hemangioma. C,
Histology of cavernous hemangioma
Hemangioma

Mention the conditions in which
cavernous hemangiomas are of clinical
significance.
In most cases, the tumors are of little clinical
significance; however,
1. There can be a cosmetic disturbance.
2. Visceral hemagiomas detected by imaging
studies may need to be distinguished from more
ominous malignant tumors.
3. Brain hemangiomas can cause pressure
symptoms or rupture.
4 Cavernous hemangiomas are component of von
Hippel-Lindau disease; they involve the
cerebellum or brain stem and eye grounds, along
with similar lesions in the pancreas and liver.
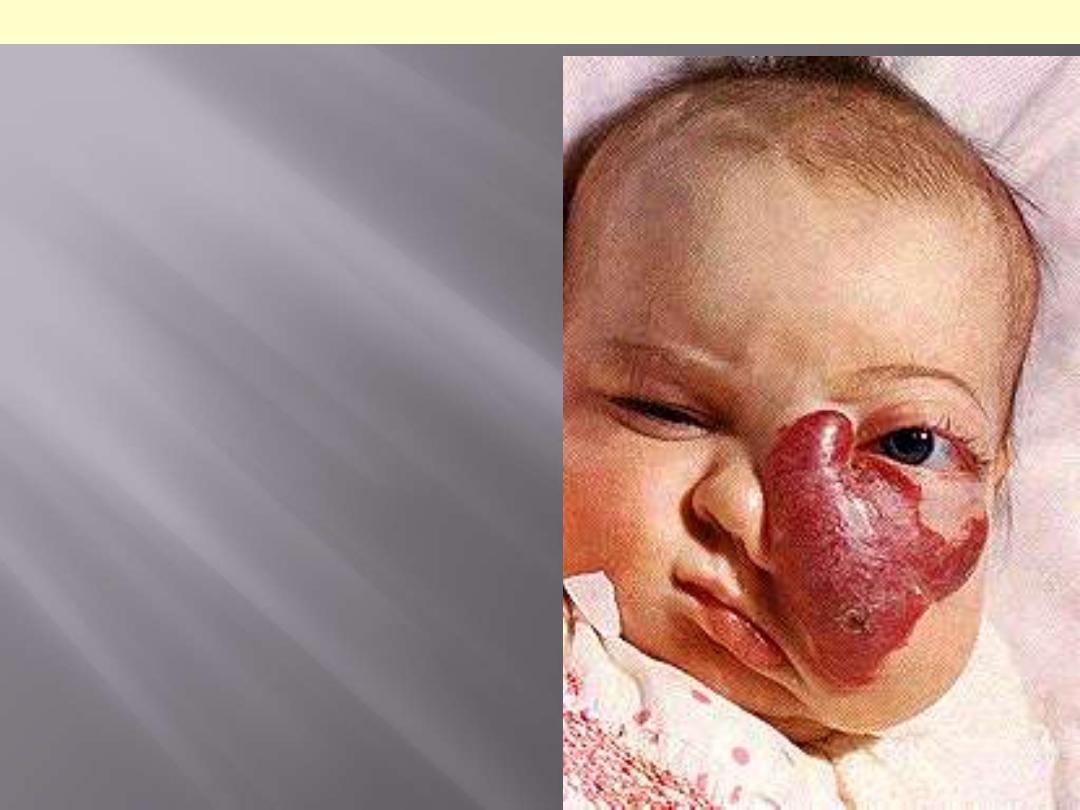
Female infant shows a massive lesion
distorting the nose and cheek.
Disfiguring hemangioma of the face
II. Intermediate-
Grade (Low-Grade
Malignant) Tumors
A. Kaposi Sarcoma
is used to be fairly common in patients with AIDS prior to the advent of
effective antiretroviral therapy, and its presence is used as a criterion for
diagnosing AIDS.
Four forms of the disease are recognized, all of these share the same
underlying viral pathogenesis:
1.
Chronic KS (classic KS)
characteristically occurs in older men.
It is not associated with HIV.
There multiple red to purple skin plaques or nodules, usually in the distal
lower extremities.
2. Lymphadenopathic KS (African, endemic KS)
is
particularly prevalent among South African Bantu children; it is also not
associated with HIV. Skin lesions are sparse, and patients present instead
with lymphadenopathy due to KS involvement; the tumor occasionally
involves the viscera and is extremely aggressive.
3. Transplant-associated KS :
Occurs in the setting of solid-organ transplantation with its attendant
long-term immunosuppression.
It tends to be aggressive (even fatal) with
nodal, mucosal, and
visceral involvement; cutaneous lesions may be absent.
4. AIDS-associated KS (epidemicKS) :
was found in a third of AIDS patients, particularly male
homosexuals.
However, with current regimens of intensive antiretroviral therapy,
KS incidence is now less than 1% (although it is still the most
prevalent malignancy in AIDS patients in the United States).
AIDS-associated KS can involve
lymph nodes and viscera
, with
wide dissemination early in the course of disease.
Most patients eventually die of opportunistic infectious rather than
from KS.

Rt. Gross photograph, illustrating coalescent red-purple patches and plaques of the skin of
foot.
Lt. in the nodular stage, the lesions become nodular, larger, and more numerous.
Kaposi sarcoma
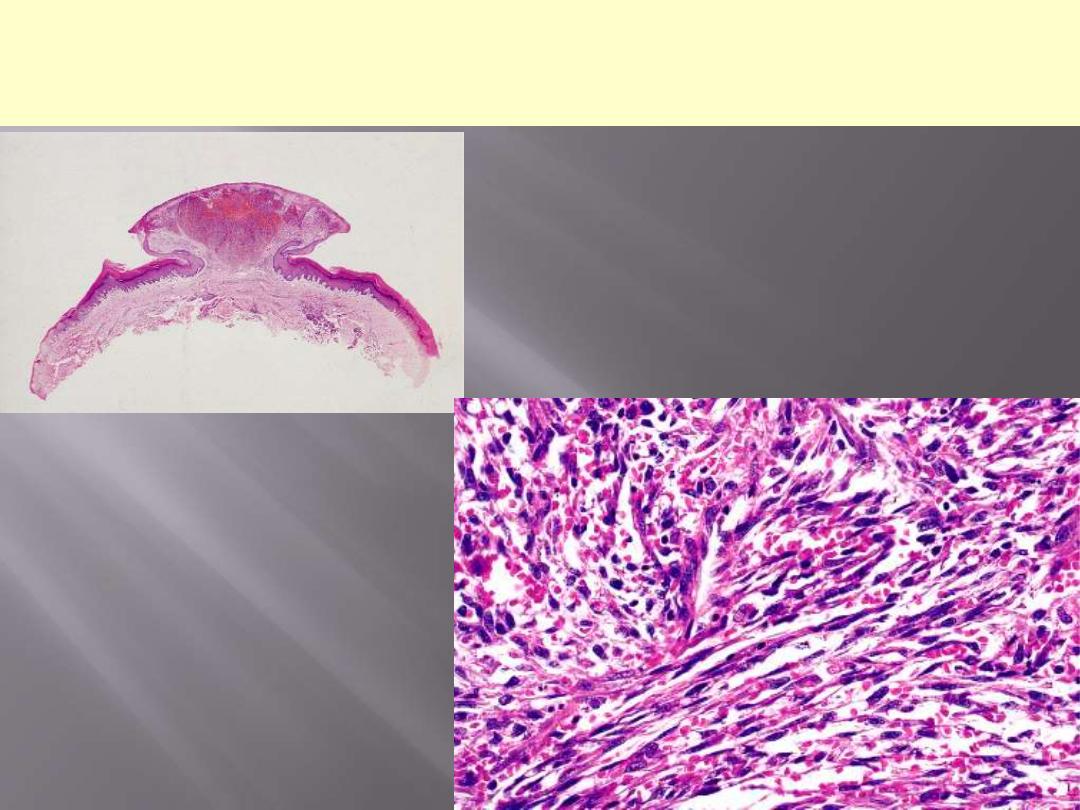
Describe the salient microscopic features of
Kaposi sarcoma in the nodular stage.
Low-power view of a lesion of Kaposi's
sarcoma having a prominent nodular
shape.
Microscopic appearance of
Kaposi’s sarcoma. Elongated
spindle cells showing minimal
atypia are separated by slits
containing red blood cells.
Pathogenesis
Regardless of the clinical subtype
(described above),
95%
of KS
lesions have been shown to be
due to
human herpesvirus 8
[HHV-8]
infection.
The virus is transmitted sexually
and by poorly understood
nonsexual routes.
III. Malignant Tumors
A.
Angiosarcomas
are malignant endothelial neoplasms with histology varying from
highly differentiated tumors that resemble hemangiomas to anaplastic
lesions.
Older adults are commonly affected.
They occur at any site but most often involve
skin, soft tissue, breast,
and liver.
Hepatic angiosarcomas
are associated with carcinogenic
exposures, including
arsenic (
arsenical pesticides),
Thorotrast (
a
radioactive contrast agent formerly used for radiologic imaging), and
polyvinyl chloride (PVC; a widely used plastic).
The increased frequency of angiosarcomas among PVC workers is one
of the truly well-documented instances of human chemical
carcinogenesis.
Angiosarcomas can also arise in the setting of
lymphedema
, classically
in the ipsilateral upper extremity several years after radical mastectomy
for breast cancer; the tumor presumably arises from lymphatic vessels
(lymphangiosarcoma)
. Angiosarcomas can also be induced by
radiation.
Clinically, angiosarcomas are locally invasive and can
metastasize readily. The current 5-year survival rates approach 30%.
B. Hemangiopericytomas
Are rare tumors derived from
pericytes-myofibroblast-
like cells
that are normally arranged around capillaries
and venules.
They are most common on the
lower extremities
(especially the thigh)
and in
the retroperitoneum.
They consist of numerous branching capillary channels
and gaping sinusoidal spaces enclosed within nests of
spindle-shaped to round cells.
The tumors may
recur after excision
, and roughly
half
metastasize
, usually
hematogenously to lungs, bone, or
liver.
