Pathology
of the
Endocrine System
THE PITUITARY GLAND
The Pituitary gland

Q. The following are true of pituitary adenoma
EXCEPT
A.
Not always clinically functional
B.
Usually composed of a single cell type
C.
A microadenoma is by definition < 1 cm in
diameter
D.
May cause hypopituitarism
E.
Histologic appearance predicts functional
status

Correct answer is
E
A.
True
: Pituitary adenomas can be functional (associated
with hormone excess with their associated clinical
manifestations) or silent.
B.
True:
usually composed of a single cell type & produce a
single predominant hormone.
C.
True
: divided on basis of size ( microadenomas < 1 >
macroadenomas)
D.
True:
macroadenomas can cause hypopituitarism by
compressing adjacent non-neoplastic parenchyma.
E.
Wrong
: functional status of an adenoma cannot be
predicted from its histologic appearance.
This is a small, bean-shaped structure that lies at the
base of the brain within the confines of the sella turcica.
It is connected to the hypothalamus by a "stalk,"
composed of axons extending from the hypothalamus.
The pituitary is composed of two morphologically and
functionally distinct components: the anterior lobe
(adenohypophysis) and the posterior lobe
(neurohypophysis).
The adenohypophysis, in H&E stained sections, shows a
colorful collection of cells with basophilic, eosinophilic or
poorly staining ("chromophobic") cytoplasm.
The release of trophic hormones is under the control of
releasing or inhibiting factors produced in the
hypothalamus.
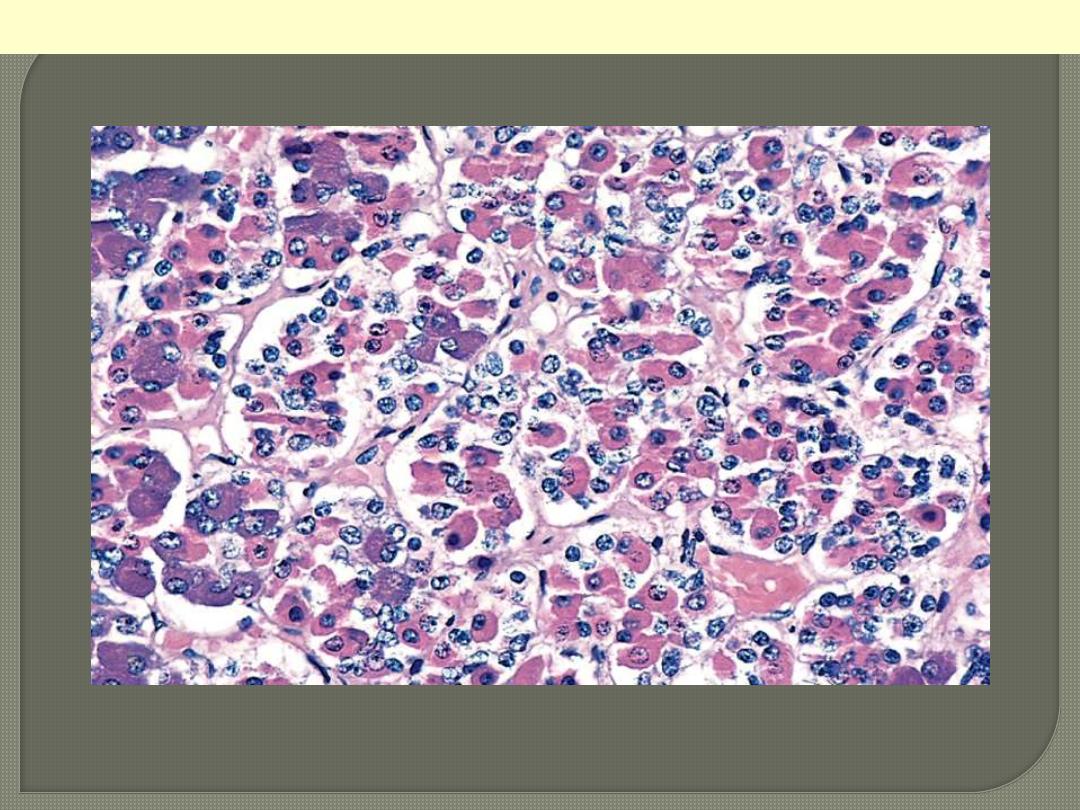
The gland is populated by several distinct cell populations containing a variety of stimulating (trophic)
hormones. Each of the hormones has different staining characteristics, resulting in a mixture of cell
types in routine histologic preparations.
Normal anterior pituitary
Hyperpituitarism
Causes
A. Pituitary; usually anterior lobe
1. Adenoma (the most common cause)
2. Hyperplasia
3. Carcinoma
B. Extra-pituitary causes
1. Hormone producing extra-pituitary
tumors (ectopic hormone production)
2. Certain hypothalamic disorders

Q. Fill the blanks in the following statements
with the appropriate words or phrases
Pituitary adenomas are responsible for
…% of intracranial neoplasms
….. is the most common type of
hyperfunctioning pituitary adenoma
C.
Functional corticotroph cell adenoma is
associated with
….disease

D. Ischemic necrosis of the anterior pituitary
is an important cause of pituitary
insufficiency. This requires destruction of
…% of the ant. lobe. A recognized cause of
the above is referred to as
…..Syndrome.
Explain

Answer for fill the blanks
A.
10%
B.
Prolactinomas
C.
Cushing disease
D.
75%
Sheehan syndrome:
postpartum necrosis of anterior pituitary
During pregnancy anterior pit. enlarges due ↑
size/number of prolactin-secreting cells, not \\
↑ B. supply
enlarged gland vulnerable to ischemic damage during
peripartum period especially in women with significant
Hge

are classified according to the hormone(s) produced by the
neoplastic cells;
Pituitary adenomas can be functional (associated with hormone
excess with their related clinical manifestations) or silent.
Adenomas are usually composed of a single cell type and
produce a single predominant hormone. However, some
adenomas can secrete two hormones (e.g. growth hormone and
prolactin).
Other adenomas are hormone negative.
Adenomas are divided on the basis of whether the size is less or
exceeds 1 cm. (microadenomas and macroademomas
respectively). Macroadenomas can cause hypopituitarism by
compressing the adjacent non-neoplastic parenchyma.

Adenomas are usually soft & well-
circumscribed
Larger lesions extend superiorly through
the sellar diaphragm compressing the
optic chiasm and adjacent structures .
Invasive adenomas refer to
nonencapsulated tumors that infiltrate
adjacent bone, dura, and even brain.

This massive, nonfunctional adenoma has grown far beyond the confines of the sella turcica and has
distorted the overlying brain. Nonfunctional adenomas tend to be larger at the time of diagnosis than
those that secrete a hormone.
Pituitary adenoma gross

Adenomas are composed of
monomorphic, polygonal cells displayed
in sheets, cords, or papillae. Their nuclei
may be uniform or pleomorphic but the
mitotic activity is scanty. The cytoplasm
of the constituent cells may be
acidophilic, basophilic, or chromophobic.
The connective tissue is scanty that is
why many lesions are soft & even
gelatinous in consistency.

The monomorphism of these cells contrasts markedly to the mixture of cells seen in the normal
anterior pituitary. Note also the absence of connective tissues.
Pituitary adenoma

The functional status of an adenoma cannot be
predicted from its histologic appearance.
Pituitary adenomas are responsible for 10% of
intracranial neoplasms.
High-resolution CT or MRI suggests that 20% of
"normal" adult pituitary glands contain an
incidental usually silent adenoma measuring 3 mm
or more in diameter.
The peak incidence of pituitary adenomas is from
30 to 50 years.

Hypopituitarism
is caused by
1
.
Loss of the anterior pituitary parenchyma
a. congenital
b. acquired
2. Disorders of the hypothalamus e.g. tumors; these
interfere with the delivery of pituitary hormone-releasing
factors from the hypothalamus.
Most cases of anterior pituitary hypofunction are
caused by the following:
1. Nonfunctioning pituitary adenomas
2. Ischemic necrosis of the anterior pituitary is an
important cause of pituitary insufficiency. This requires
destruction of 75% of
the
anterior pituitary.
The first endocrine target organ affected is the OVARY

a. Sheehan syndrome
b. Disseminated intravascular coagulation
c. Sickle cell anemia
d. Elevated intracranial pressure
e. Traumatic injury
f. Shock states
3. Iatrogenic i.e. surgical removal or radiation-induced destruction
4. Inflammatory lesions such as sarcoidosis or tuberculosis
5. Metastatic neoplasms involving the pituitary.
6. Mutations affecting the pituitary transcription factor Pit-1

The posterior pituitary, or
neurohypophysis, is composed of
modified glial cells (termed pituicytes)
and axonal processes extending from
nerve cell bodies in the hypothalamus.
The hypothalamic neurons produce two
peptides: antidiuretic hormone (ADH)
and oxytocin that are stored in axon
terminals in the neurohypophysis.

The clinically important posterior
pituitary syndromes involve ADH
production and include:
1. Diabetes insipidus and
2. Inappropriate secretion of high levels
of ADH.


is “a hypermetabolic state caused by elevated
circulating levels of free T
3
and T
4
”.
This may primary (Graves disease) or rarely,
secondary (due to pituitary or hypothalamic
diseases).
The measurement of serum TSH concentration
provides the most useful single screening test for
hyperthyroidism, because TSH levels are decreased
in primary cases, even when the disease is still be
subclinical.
In secondary cases TSH levels are either normal or
raised. A low TSH value is usually associated with
increased levels of free T
4
. Occasionally,
hyperthyroidism results from increased levels of T
3
(T
3
toxicosis).

It is sometimes divided into primary and secondary
categories, depending on whether the condition
arises from diseases affecting the thyroid or
hypothalamic/pituitary disease.
Cretinism
Myxedema,
Measurement of the serum TSH is the most sensitive
screening test for this disorder. The serum TSH is
increased in primary hypothyroidism. The TSH
concentration is not increased in hypothyroidism
caused by hypothalamic or pituitary disease. Serum
T
4
is decreased in individuals with hypothyroidism of
any origin.

The more common and clinically
significant thyroidites are:
1. Hashimoto thyroiditis
2. Subacute granulomatous thyroiditis
3. Subacute lymphocytic thyroiditis

Choose the most appropriate statement:
Hashimoto thyroiditis
A.
It is a rare cause of hypothyroidism
B.
Mostly encountered in males
C.
It has an infectious etiology
D.
The role of genetics is insignificant in its
etiology
E.
There is an increased risk for
development of B-cell non-Hodgkin
lymphomas.

The correct answer is
E
A.
Wrong
: it is the most common cause of hypothyroidism.
B.
Wrong
: there is striking female predominance (10: 1 to
20:1)
C.
Wrong
: it is an autoimmune disease resulting from
sensitization of CD4+ (T-helper) cells to thyroid Ags
Reaction of the above two
interferon γ
inflammation + activation
macrophages
Injury to the thyroid
D.
Wrong
: there is a significant genetic component to disease
pathogenesis
E.
True
: patients are at increased risk for the development of
B-cell non-Hodgkin lymphomas.
CD8+ (cytotoxic T)
Natural killer cells



Answer:
Gross features
•
The thyroid shows moderate, diffuse, and symmetric
enlargement.
•
The cut surface is pale, gray-tan, firm, and nodular
(Eventually there is thyroid atrophy)

Below are two microscopic sections from the previous thyroid. Describe

Microscopic features:
Diffuse infiltration of the parenchyma by small
lymphocytes, plasma cells.
Lymphocytes form follicles some with germinal centers
•
Thyroid follicles are atrophic and lined by Hürthle cells
(having abundant eosinophilic, granular cytoplasm.
•
Interstitial connective tissue is increased and may be
abundant.

The following are true of Graves disease EXCEPT
A.
It is the most common cause of
hyperthyroidism
B.
It is characterized by diffusely enlarged
thyroid, exophthalmos, and pretibial
myxedema
C.
The peak incidence is between 40 and 50
years
D.
The F/M is 7:1
E.
Auto-Abs to TSH receptors are central to
disease pathogenesis

The correct answer is
C
A.
True
: Graves disease is the most common cause of
hyperthyroidism
B.
True:
characterized by the a triad of
1.
Thyrotoxicosis
, caused by a diffusely enlarged, hyperfunctioning
thyroid
2.
Exophthalmos
, a form of infiltrative ophthalmopathy (40% of
patients)
3.
Pretibial myxedema
(minority of cases)
C.
Wrong
(the exception): the peak incidence is between
20
and 40 years
D.
True:
the F/M: 7/1
E.
True:
Graves disease is an autoimmune disorder with a variety of serum
Abs
Autoantibodies to the TSH receptor are central to disease
pathogenesis;
the most important of these is TSI is the most important; it binds to
the TSH receptor of follicular cells. It mimics the action of TSH with
resultant increased release of thyroid hormones. This antibody is
present in most patients and is relatively specific for Graves disease.


Answer:
The photo on your left shows the external
aspect of diffusely & moderately enlarged,
hyperemic thyroid gland.
The photo on your right shows the cut
surface of thyroid gland showing a
hyperemic "juicy" appearance.

Below are histological sections from the previous gland. Describe.
What is your diagnosis?

Microscopic features
The follicular epithelial cells are tall, columnar, and more
crowded than usual. This crowding often results in the
formation of small pseudopapillae, which project into the
follicular lumen
•
The colloid within the follicle lumens is pale, with
scalloped margins.
•
Lymphoid infiltrates and mature plasma cells are present
throughout the interstitium; germinal centers are
common.
•
The above features are consistent with involvement of
the gland by Graves disease


The following are true of multinodular goiter
EXCEPT
A.
Most often caused by dietary iodine
deficiency
B.
There is a euthyroid metabolic state
C.
The degree of thyroid enlargement is not
related to the level and duration of thyroid
hormone deficiency.
D.
It includes endemic goiter
E.
It is a recognized cause of thyrotoxicosis

The correct choice is
C
True
as the enlargement reflects impaired synthesis of
thyroid hormones, most often caused by dietary iodine
deficiency.
True
: the thyroid cell hyperplasia & hypertrophy are able
to overcome the hormone deficiency resulting in
euthyroid metabolic state.
Wrong
: the degree of thyroid enlargement is proportional
to the level and duration of thyroid hormone deficiency.
True
: occurs in geographic areas (typically mountainous)
where the soil, water, and food supply contain little
iodine. The term endemic is used when goiters are
present in > 10% of the population in a given region.
True
: a hyperfunctioning ("toxic") nodule may develop
within a long-standing goiter, resulting in
hyperthyroidism. This condition is not accompanied by
the infiltrative ophthalmopathy and dermopathy

This is the external appearance of a thyroidectomy specimen.
DESCRIBE

This diffusely enlarged thyroid gland is somewhat nodular. This patient was euthyroid. This represents
the most common cause for an enlarged thyroid gland and the most common disease of the thyroid--a
nodular goiter.
Nodular colloid goiter

The gland is coarsely nodular and contains areas of fibrosis and cystic change. Note the brown
gelatinous colloid characteristic of this condition ("colloid goiter").
Multinodular
goiter

These are microscopic sections from the previous thyroid.
DESCRIBE

LP appearance of nodular goiter. The
hyperplastic nodules lack a capsule
Nodular colloid goiter
Nodular goiter showing markedly distended,
colloid-filled follicles


Q1. What is the DD of a solitary
thyroid nodule?
Q2. How you determine the nature of
the nodule?

Answer1: causes of a solitary thyroid nodule
include
1. Non-neoplastic conditions
a. A dominant nodule of otherwise multinodular goiter
b. Simple cysts
c. Foci of thyroiditis
2. Neoplastic conditions
a. Follicular adenomas
b. Carcinomas
Answer 2
: through microscopic evaluation of the nodule. This
is done by FNAB &/or histologic study of surgically
resected thyroid tissue, that provides the most definitive
information about its nature.

A 45-year-old lady with solitary thyroid nodule
surgical removal done. Thyroidectomy performed
The photo below depict the gross appearance & microscopic sections
from the nodule. Describe. What is your diagnosis

Answer
A.
A tan-colored rounded solid mass surrounded by a thin
white capsule.
B.
The lesion consists of closely packed variably sized
follicles (acini)
C.
Higher power examination shows follicles lined by
cuboidal benign-looking epithelium & are filled with
colloid.
Diagnosis
Follicular adenoma of the thyroid
.
How you differentiate this lesion from well-differentiated,
minimally invasive follicular ca.?


What are the types of thyroid carcinomas that
you know of?
•
Papillary carcinoma
80%
• Follicular carcinoma
15%
• Medullary carcinoma 4%
• Anaplastic carcinomas
1%


Is the most common thyroid cancer.
although it can present in any age
group, the mean age at the time of initial
diagnosis is 40 years.
Papillary carcinomas present most often
as a painless mass in the neck.
Metastases to adjacent cervical lymph
nodes occur in 50% of cases.
Papillary carcinomas are indolent
lesions, with 10-year survival rates in
excess of 95%.


Papillary thyroid carcinomas:
two major types of genetic
alteration:
a. Chromosomal rearrangements involving the tyrosine kinase
receptor gene RET . Such rearrangements result in the
formation of fusion genes, known as ret/PTC (receptor of
tyrosine kinase/papillary thyroid carcinoma),
b. Point mutations in the BRAF oncogene
Both these genetic changes independently activate the
carcinogenic MAP kinase signaling pathway.
Follicular thyroid carcinomas:
approximately 50% of such tumors
harbor mutations in the RAS family of oncogenes.
Medullary carcinomas:
familial medullary thyroid carcinomas
occur in MEN 2, and are associated with germ-line RET proto-
oncogene mutations. RET mutations are also seen in nonfamilial
(sporadic) medullary thyroid cancers.
Anaplastic carcinomas:
inactivating point mutations in the p53
tumor suppressor gene are common in anaplastic tumors

a.
Exposure to ionizing radiation
, particularly
during the first 2 decades of life,
The incidence of carcinoma of the thyroid
is substantially higher among atomic bomb
survivors in Japan and in those exposed to
ionizing radiation after the Chernobyl
nuclear plant disaster. The overwhelming
majority of cancers arising in this setting
are papillary thyroid cancers, and most
have RET gene rearrangements.
b.
Long-standing multinodular goiter
has
been suggested as a predisposing factor.

The following are true of papillary carcinoma
EXCEPT
A.
May be quite small & measure < 1 cm in
diameter
B.
The diagnosis depends on the nuclear
features of the constituent cells
C.
The presence of papillary architecture is not
essential for the diagnosis
D.
Metastasis to adjacent cervical lymph nodes
is a rare event.
E.
Psammoma bodies are a recognized feature

The correct answer is D
A.
True
: the size of papillary carcinomas ranges from
microscopic to huge. A very high proportion of thyroid
cancers measuring < 1 cm in diameter are of papillary
type.
B.
True
: the diagnosis of papillary carcinoma is based on
nuclear features even in the absence of a papillary
architecture.
C.
True:
some papillary ca are composed predominantly or
exclusively of follicles (follicular variant)
D.
Wrong
: Metastases to adjacent cervical lymph nodes
occur in 50% of cases
E.
True
: psammoma bodies are often present within the
tumor

Q 1. What are psammoma bodies?
Q 2. What are the nuclear features of papillary carcinoma
cells?
Q1. Concentrically calcified structures
Q2. A. Optically clear nuclei referred to as "ground-glass"
nuclei.
B. intranuclear pseudo-inclusions due to invaginations of
the cytoplasm.
C. Nuclear clefting

The size of the primary tumor ranges
from microscopic to huge. A very high
proportion of thyroid cancers measuring
< 1 cm in diameter are of papillary type.
The tumor may be solitary or multifocal
It is either well circumscribed
encapsulated or ill-defined with
infiltrative margins.
Most cases are solid, whitish, firm, and
clearly invasive; sometimes papillary
formations are evident.

The diagnosis of papillary carcinoma is based
on nuclear features even in the absence of a
papillary architecture.
The nuclei of papillary carcinoma cells contain
very finely dispersed chromatin, which imparts
an optically clear appearance referred to as
"ground-glass" nuclei.
In addition, invaginations of the cytoplasm
may give the appearance of intranuclear
pseudo-inclusions.
Nuclear clefting is another feature of
papillary carcinoma cells.

are composed of fairly uniform cells forming small follicles,
Similar to follicular adenomas, Hürthle cell variants of follicular
carcinomas may be seen.
Follicular carcinomas may be frankly infiltrative or minimally
invasive. The latter are sharply demarcated lesions that may be
impossible to distinguish from follicular adenomas on gross
examination. This distinction requires extensive histological
sampling of the tumor-capsule-thyroid interface, to exclude of
confirm the presence of capsular and/or vascular invasion.
Follicular lesions in which the nuclear features are typical of
papillary carcinomas should be regarded as papillary cancers.
Follicular carcinomas present most frequently as solitary "cold"
thyroid nodules. These neoplasms tend to metastasize through
the bloodstream to the lungs, bone, and liver. Regional nodal
metastases are uncommon, in contrast to papillary carcinomas.


Fill the blanks with the correct word or phrase
Medullary Carcinoma is derived from the
….cells
Medullary carcinoma secretes the
hormone
….
A distinctive feature of medullary
carcinomas is the presence of
…deposits
…. is among the most aggressive,
uniformly fatal human neoplasms that
presents as a bulky cervical mass
Osteitis fibrosa cystica, nephrolithiasis ,
pathological fractures & metastatic
calcification are recognized feature of
…..

Answers
Parafollicular C cells
Calcitonin
Amyloid deposits
Anaplastic thyroid ca
Primary hyperparathyroidism

This is either primary or secondary, and, less
commonly, tertiary. The primary form represents an
autonomous overproduction of PTH, while the latter
two conditions occur as secondary phenomena in
individuals with chronic renal failure.
Primary hyperparathyroidism is an important cause of
hypercalcemia. It is caused by parathyroid
1. Adenoma (80%)
2. Primary hyperplasia (15%)
3. Parathyroid carcinoma (5%).


The following are true regarding pancreatic
endocrine cell tumors EXCEPT
A.
Their behavior cannot be predicted from light
microscopic criteria
B.
Insulinomas may be associated with
hypoglycemia
C.
Gastrinomas may be associated with
Zollinger-Ellison syndrome
D.
Gastrinomas tend to behave in a malignant
fashion
E.
Glucagonomas are as frequent as
insulinomas

Answers: the correct choice is E
A.
True
: it is difficult to predict their behavior purely on their light
microscopic criteria. Features of importance in this regard include
size & cell type in that tumors < 2 cm in size tend to be behave in a
benign & the vast majority of insulinomas are benign, while the vast
majority of other pancreatic endocrine neoplasms tend to be
malignant.
B.
True:
Insulinomas (β-cell tumors), the most common type pancreatic
endocrine neoplasms, may produce sufficient insulin to induce
hypoglycemia.
C.
True:
Zollinger and Ellison were the first to report the association of
pancreatic islet cell lesions (gastrinomas) with hypersecretion of
gastric acid and severe peptic ulceration (Zollinger-Ellison
syndrome). In ZE syndrome, hypergastrinemia stimulates extreme
gastric acid secretion, which in turn leads to multiple duodenal and
gastric ulcers.
D.
True:
> 50% of gastrinomas are locally invasive or have already
metastasized at the time of diagnosis.
E.
Wrong:
α-Cell tumors (glucagonomas) is relatively rare pancreatic
endocrine cell tumor & are characterized by extremely high plasma
glucagon levels.

These are most common in adults, may be single or
multiple, and benign or malignant.
The latter metastasize to lymph nodes and liver.
They tend to be functional.
Like other endocrine neoplasms, it is difficult to
predict their behavior purely on their light microscopic
criteria.
In general, tumors less than 2 cm in size tend to
behave in an indolent manner. The vast majority of
insulinomas (the most common subtype) are benign,
while the vast majority of other pancreatic endocrine
neoplasms tend to be malignant.
Insulinomas (β-cell tumors) are the most common
of pancreatic endocrine neoplasms; they are
generally benign but may produce sufficient
insulin to induce hypoglycemia.


Hypercortisolism (Cushing Syndrome) is
caused by any condition that produces an
elevation in glucocorticoid levels. The
causes of this syndrome are
A. Exogenous through administration of
exogenous glucocorticoids; the most common
cause.
B. Endogenous
1. Hypothalamic-pituitary diseases causing
hypersecretion of ACTH (Cushing disease)
2. Adrenocortical hyperplasia or neoplasia
3. Ectopic ACTH secretion by nonendocrine
neoplasms (paraneoplastic)

The following are true of Cushing syndrome
EXCEPT
A.
Encompasses any condition that produces an
elevation in serum glucocorticoid levels.
B.
Administration of exogenous glucocorticoids
is a relatively rare cause
C.
Excessive secretion of ACTH is a recognized
cause
D.
It may be associated with pulmonary small
(oat) cell carcinoma
E.
The cortex of adrenal glands may be atrophic

The EXCEPTION IS
B
True
: hypercortisolism (Cushing Syndrome) is caused by
any condition that produces an elevation in
glucocorticoid levels.
Wrong
: exogenous administration of glucocorticoids is
the most common cause.
True
: hypothalamic-pituitary diseases can cause
hypersecretion of ACTH (Cushing disease)
True
: ectopic secretion of ACTH by nonendocrine tumors
is commonly due to a small-cell carcinoma of the lung.
True
: there is one of four changes in the adrenal glands,
which depends on the cause.
1. Cortical atrophy
2. Diffuse hyperplasia
3. Nodular hyperplasia
4. Adenoma, rarely a carcinoma

Describe the three pair of adrenals in the photo below & predict the
possible clinical correlation with each pair

Normal
-looking adrenals
Adrenal
atrophy
(due either
Addison's disease or long-
term corticosteroid
therapy).
Bilateral adrenocortical
hyperplasia
. This could be
due to a pituitary adenoma
secreting ACTH (Cushing's
disease), or Cushing's
syndrome from ectopic
ACTH production, or
idiopathic adrenal
hyperplasia.

Metastatic cancer is more common than
primary tumors.
Functional adenomas are commonly
associated with hyperaldosteronism and with
Cushing syndrome.
In other words, functional and
nonfunctional adrenocortical neoplasms
cannot be distinguished on the basis of
morphologic features.

Identify the organ, describe the abnormality. What is your diagnosis

Adrenocortical
adenoma
The adenoma is
distinguished from
nodular hyperplasia by
its solitary,
circumscribed nature.
The functional status of
an adrenocortical
adenoma cannot be
predicted from its gross
or microscopic
appearance.
Do you think that this
tumor has been
clinically functioning?

Enumerate three conditions associated with
acute adrenocortical insufficiency
1.
Massive adrenal
hemorrhage
including
Waterhouse-Friderichsen syndrome
2.
Sudden withdrawal of long-term
corticosteroid therapy
3.
Stress
in those with chronic adrenal
insufficiency

Pheochromocytoma
are neoplasms composed of chromaffin cells, which as their
normal counterparts synthesize and release catecholamines.
The "rule of 10s" is conviently applied to this tumor: 10% of
pheochromocytomas
1. Arise in association with one of several familial syndromes such
as MEN syndromes, type 1 neurofibromatosis, von Hippel-
Lindau disease, and Sturge-Weber syndrome.
2. Are extra-adrenal, occurring in sites such as the organ of
Zuckerkandl and the carotid body, where they are usually called
paragangliomas rather than pheochromocytomas.
3. Are bilateral; but in association with familial syndromes, this
figure may rise to 50%.
4. Are malignant; frank malignancy, however, is more common in
extra-adrenal tumors.

The following are true of Pheochromocytomas
EXCEPT
A.
Are neoplasms composed of chromaffin cells
B.
Are malignant or bilateral in 50% of the cases
C.
May be associated with extra-adrenal
paraganglioma
D.
Incubation of fresh tumor tissue with
potassium dichromate imparts the tumor a
dark brown color
E.
There is increased urinary excretion of
vanillylmandelic acid (VMA)& metanephrines.

Correct choice is
B
A.
True
: pheochromocytomas are neoplasms composed of
chromaffin cells, which as their normal counterparts
synthesize and release catecholamines.
B.
Wrong (the exception):
10% of these tumors are bilateral
& 10% are malignant. (The "rule of 10s")
C.
True:
these tumors are extra-adrenal in 10% of the cases,
occurring in sites such as the organ of Zuckerkandl and
the carotid body, where they are usually called
paragangliomas rather than pheochromocytomas.
D.
True: incubation of the fresh tissue with potassium
dichromate solutions converts the tumor a dark brown
color. See next photo
E.
True: the laboratory diagnosis of pheochromocytoma is
based on demonstration of increased urinary excretion of
free catecholamines and their metabolites, such as
vanillylmandelic acid (VMA)& metanephrines.

The section of tumor at the bottom has been placed into a dichromate fixative which turns the tissue
brown as the catecholamines are oxidized. Compare to the section of pink to yellow tumor at the top
which has not been placed in dichromate fixative
*
.
Pheochromocytoma Chromaffin reaction

The clinical course of
pheochromocytoma is dominated by
hypertension that may be episodic,
which is associated with tachycardia,
palpitations, headache, sweating and
tremor.
Sudden cardiac death may occur,
probably secondary to catecholamine-
induced myocardial irritability and
ventricular arrhythmias.


Choose the most appropriate statement
Regarding neuroblastoma
A.
It is the most common malignancy of
childhood
B.
A unique feature is spontaneous
regression of the tumor
C.
The adrenal cortex is the commonest site
D.
Therapy may induce maturation into
neuroma
E.
The age of the patient does not influence
prognosis

The correct choice is
B
A.
Wrong
: NB is the 2
nd
most common solid malignancy of
childhood after brain tumors
B.
True (the correct choice):
spontaneous regression is a
unique feature of NB
C.
Wrong
: adrenal medulla is the commonest site. The
remainder occur along the sympathetic chain, mostly in
the paravertebral region of the abdomen and posterior
mediastinum.
D.
Wrong
: Some neoplasms show signs of maturation,
either spontaneous or therapy-induced, into
ganglioneuroblastoma. Further maturation leads to
ganglioneuroma.
E.
Wrong:
age of the patient & the stage of the tumor are the
two most important prognostic factors. Children < 1 year
of age have a much more favorable outlook than do older
children at a comparable stage of disease.

The tumor shows the typical
location above the upper
pole of the kidney, which is
uninvolved.
Neuroblastoma adrenal G
The tumor exhibits a variegated
appearance resulting from hemorrhage
and necrosis.
neuroblastoma showing a variegated
appearance with extensive areas of
necrosis. The tumor shown is almost
entirely necrotic and hemorrhagic.

A, the tumor is composed of small cells embedded in a finely fibrillar matrix. A Homer-Wright pseudo-
rosette is seen (arrow) . B, Ganglioneuromas, arising from spontaneous or therapy-induced maturation
of neuroblastomas, are characterized by clusters of large cells with vesicular nuclei and abundant
eosinophilic cytoplasm (arrow), representing neoplastic ganglion cells. Spindle-shaped Schwann cells
are present in the background stroma.
Neuroblastoma & ganglioneuroma
