
COPD

Asthma
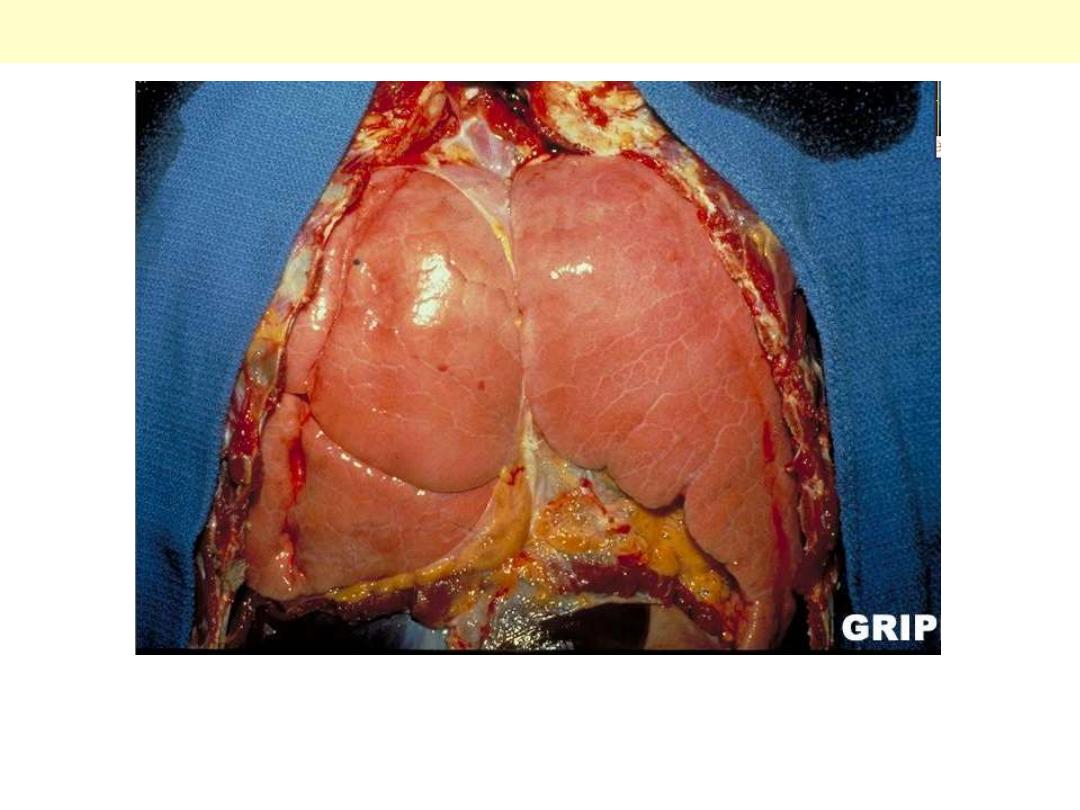
Bronchial asthma: overinflation of the lungs
Status asthmaticus: Note the overinflated lungs secondary to airway obstruction.
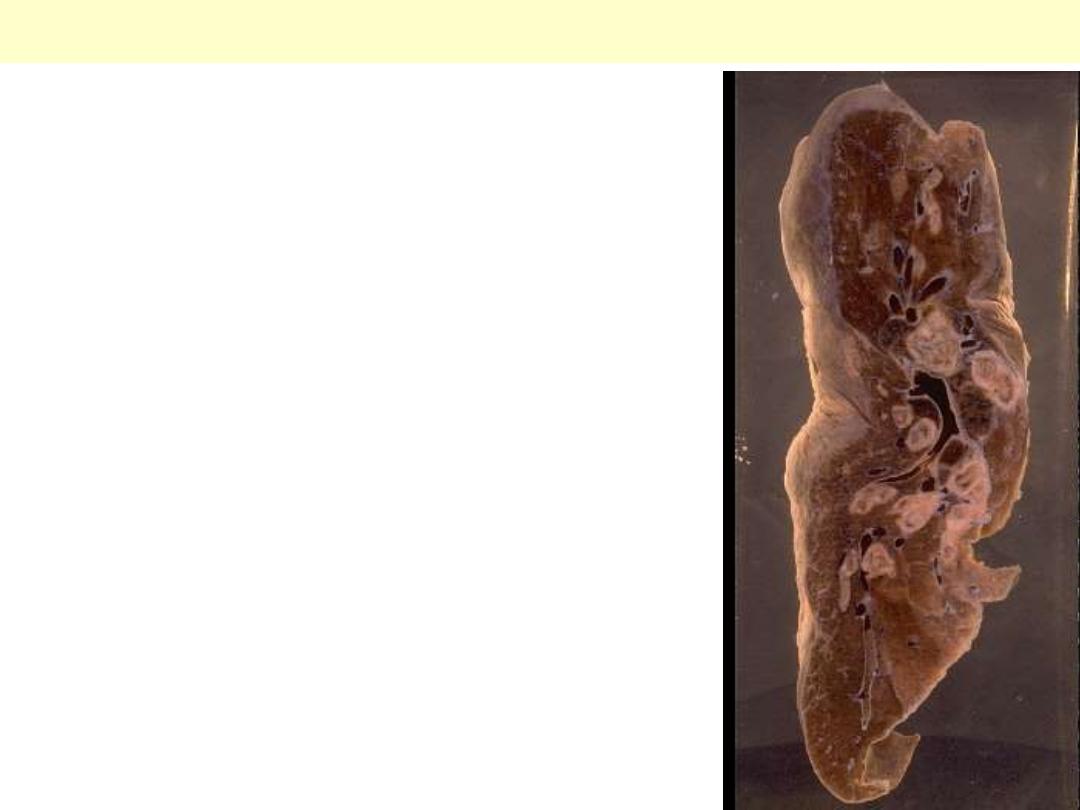
Bronchial asthma
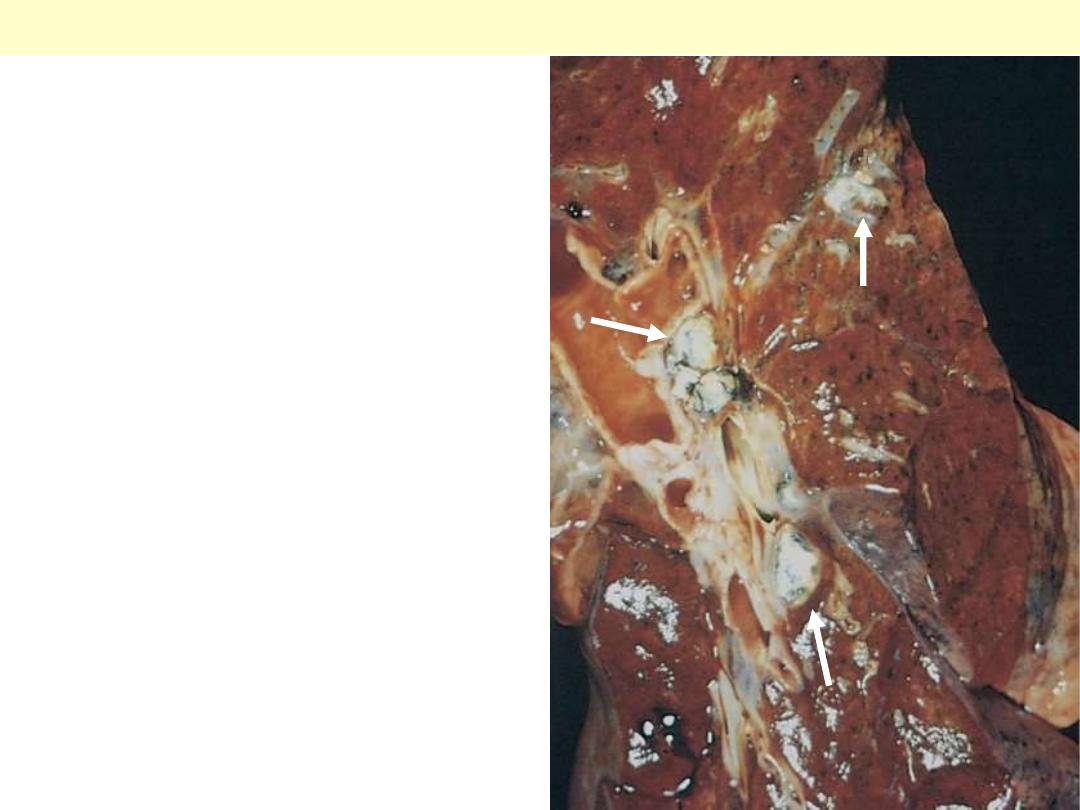
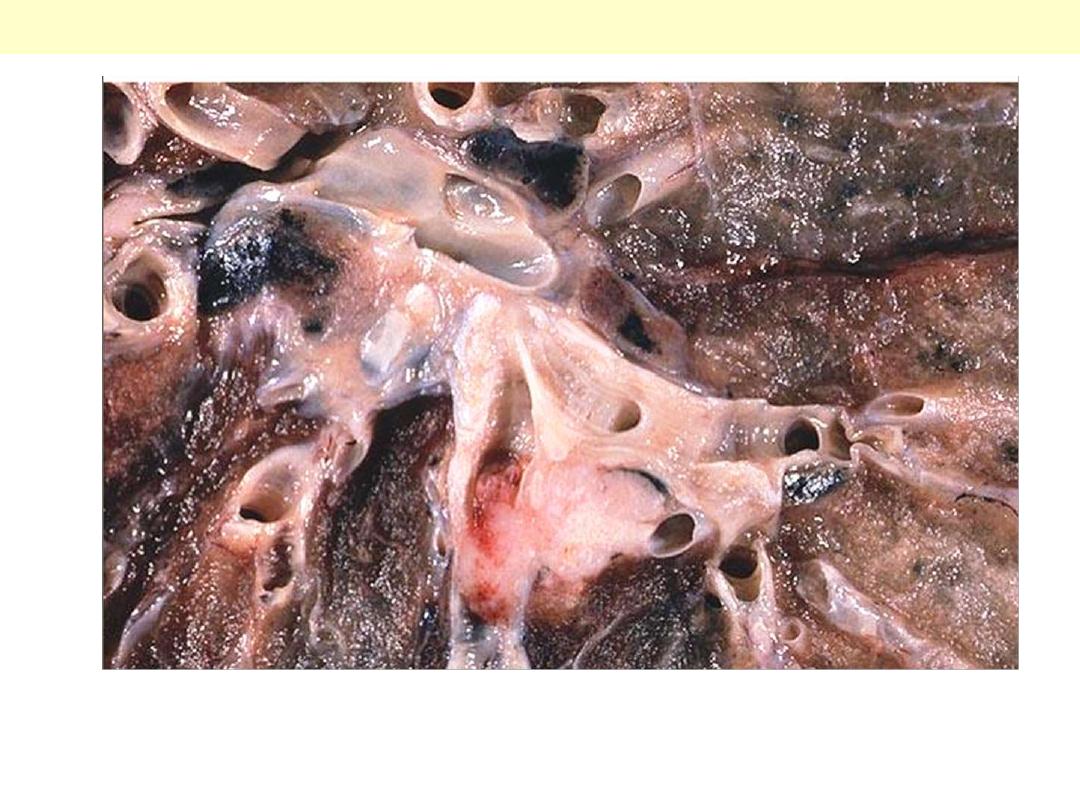
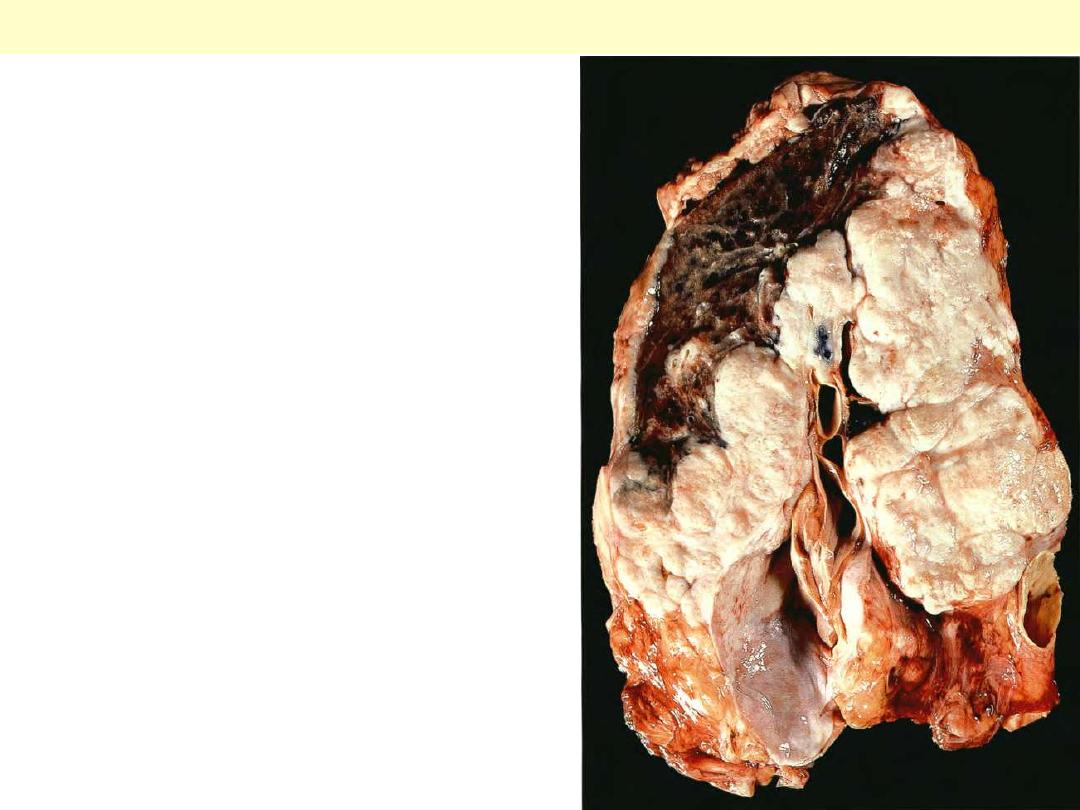
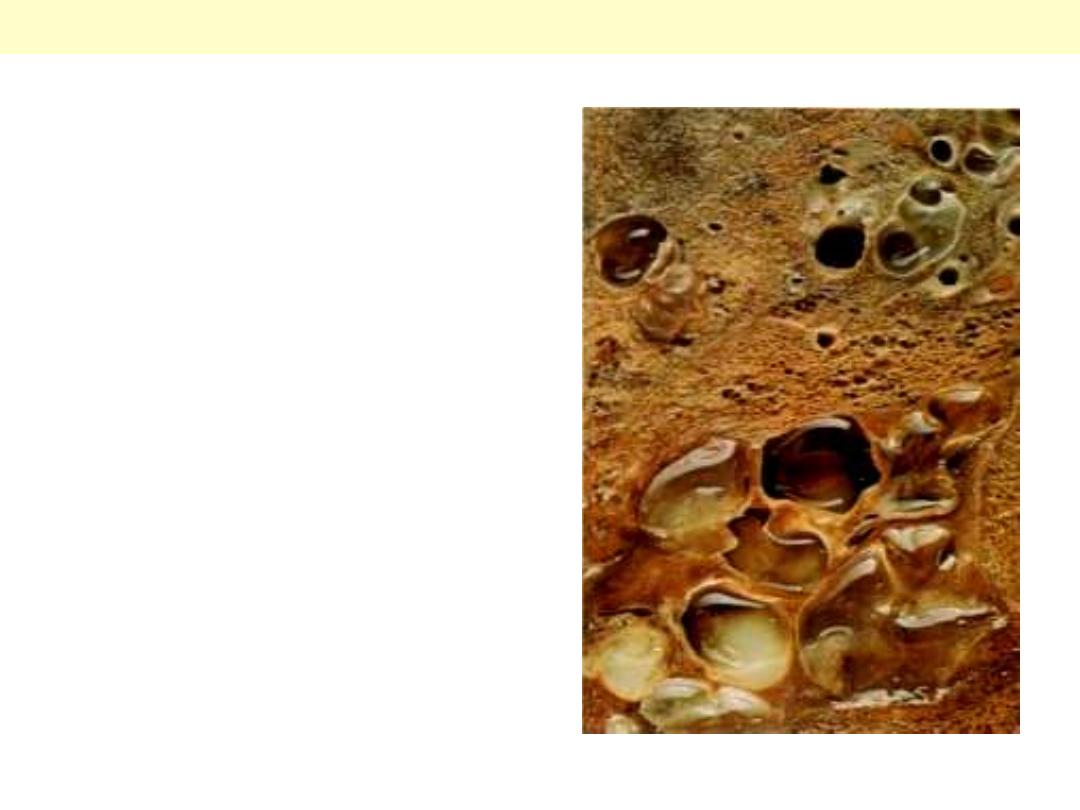
This specimen shows a cross section of a lung from an asthmatic
with obstruction of major airways (bronchi). The lung is collapsed,
due to absorption of air trapped by obstruction of airways (bronchi
and bronchioles). The large and medium-sized bronchioles are
thick-walled and they are filled with greyish-white, jelly-like mucus
plugs. It is these plugs, rather than spasm of airway muscle, that
have caused the partial collapse of the lung, low arterial oxygen and
high carbon dioxide.
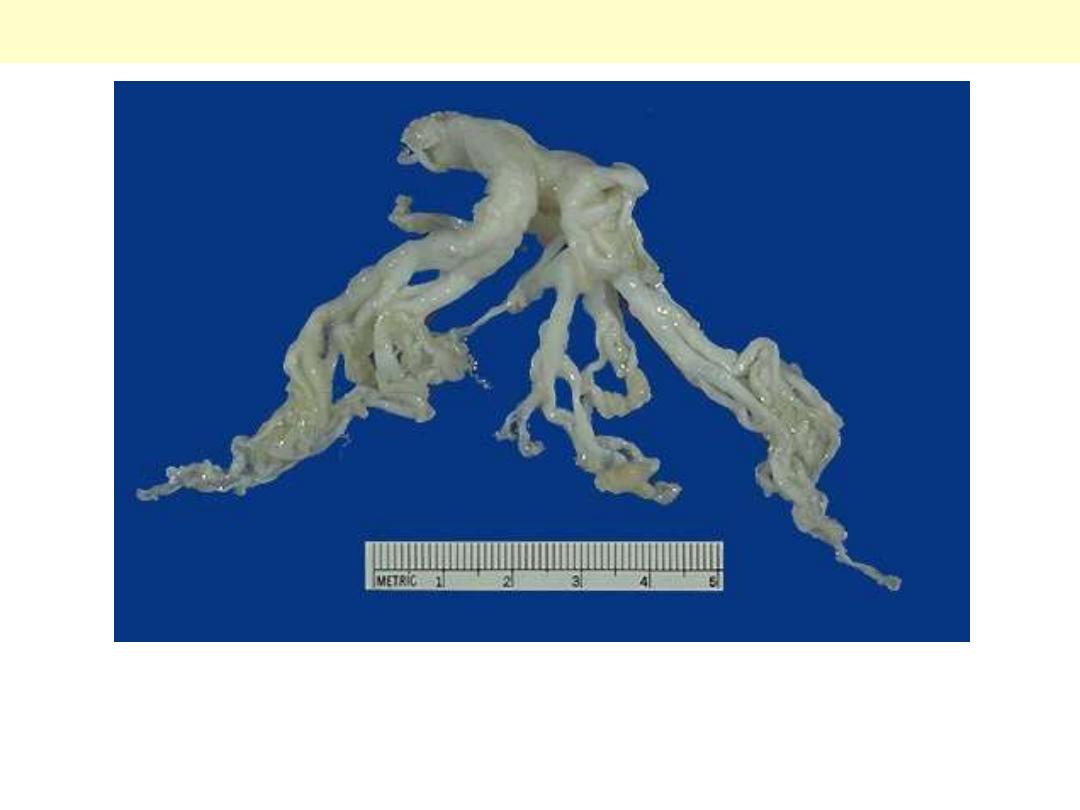
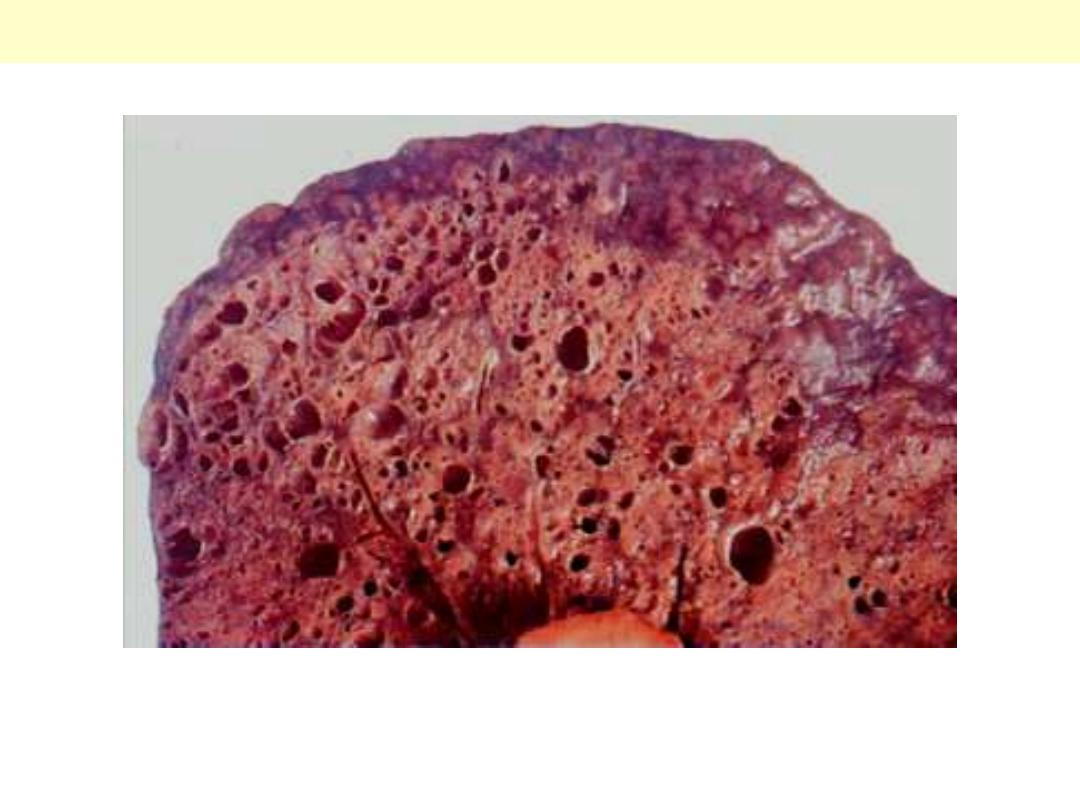
Bronchial asthma
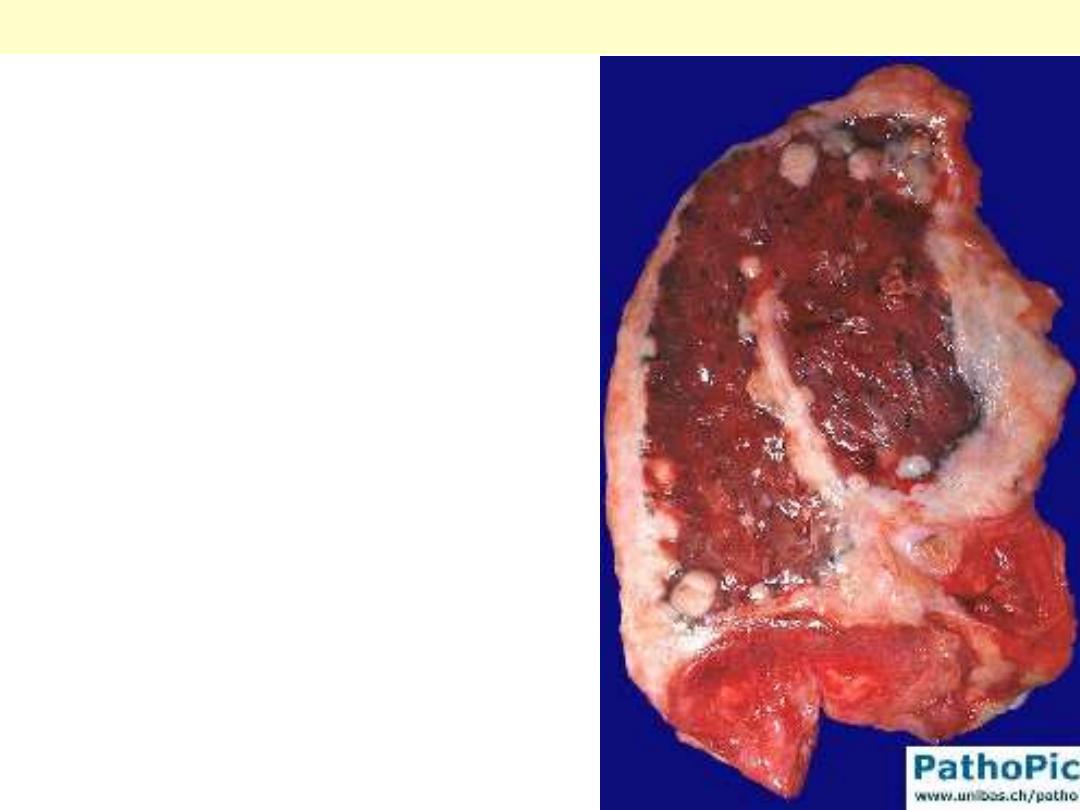
This cast of the bronchial tree is formed of inspissated mucus and was coughed up by a patient during
an asthmatic attack. The outpouring of mucus from hypertrophied bronchial submucosal glands, the
bronchoconstriction, and dehydration all contribute to the formation of mucus plugs that can block
airways in asthmatic patients.
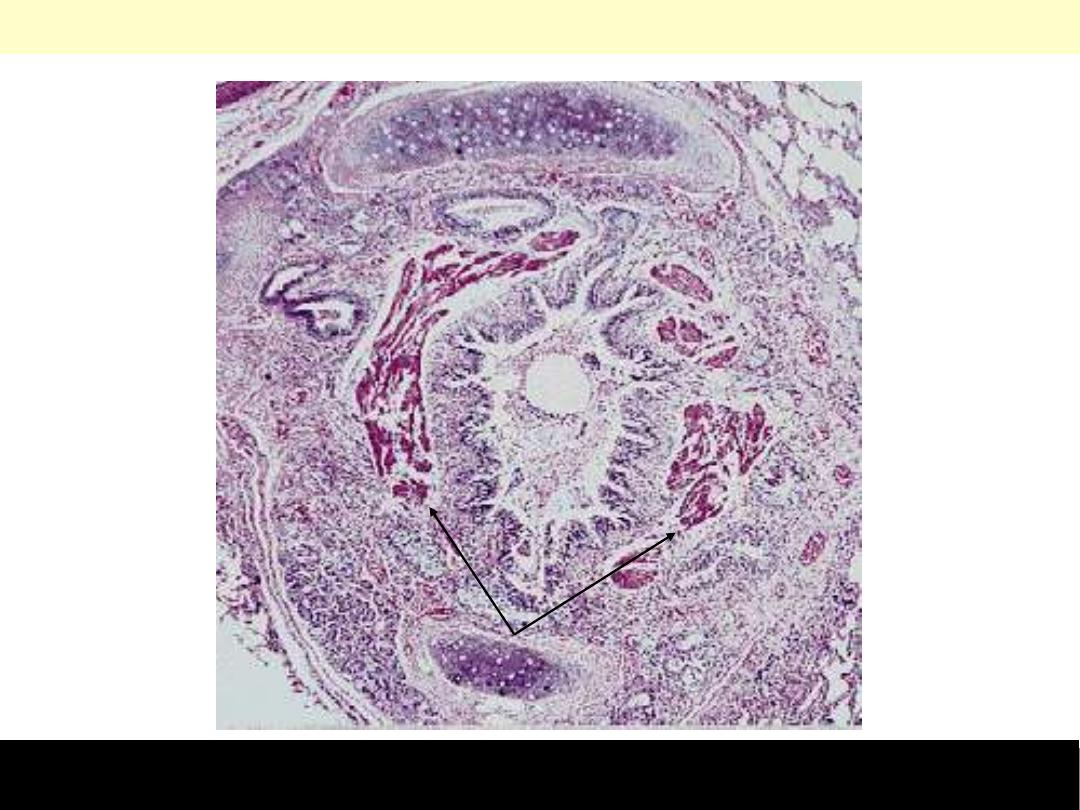
Bronchial asthma
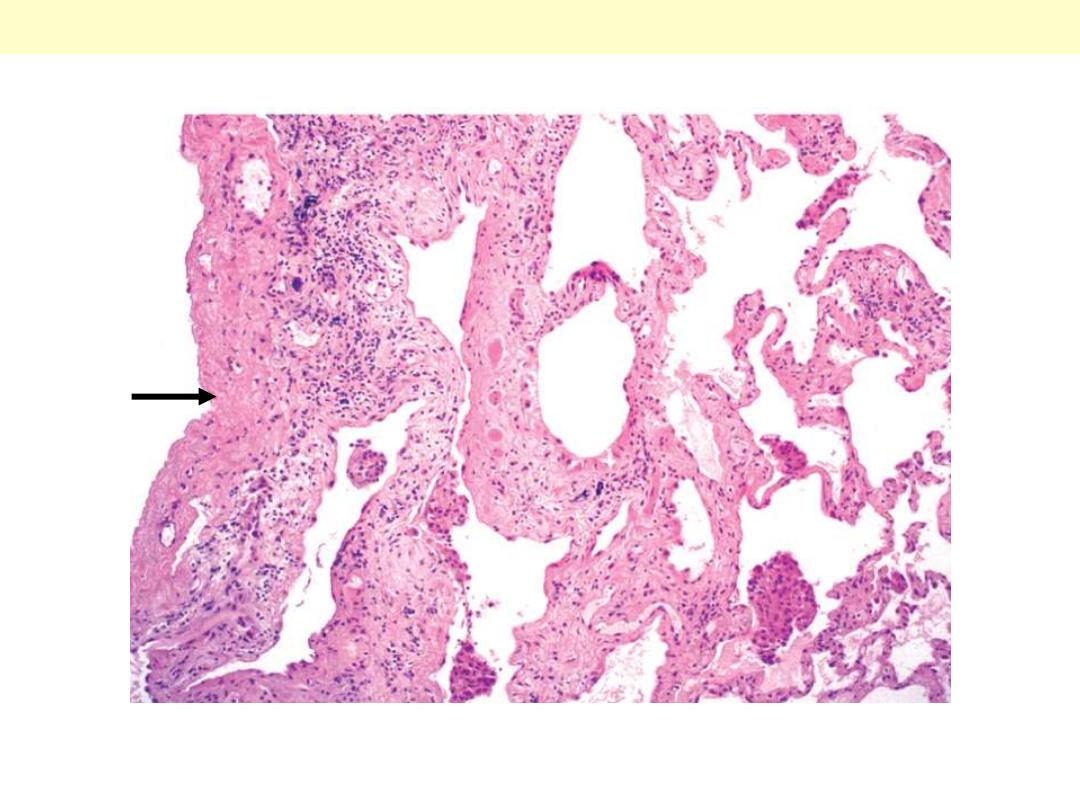
Asthma is characterized by reversible airways obstruction in small airways. The latter is due to a
combination of bronchospasm and mucus plugging. Note mucus plugging of the lumen, smooth muscle
cell prominence (arrow), and the intense inflammatory cell infiltration.
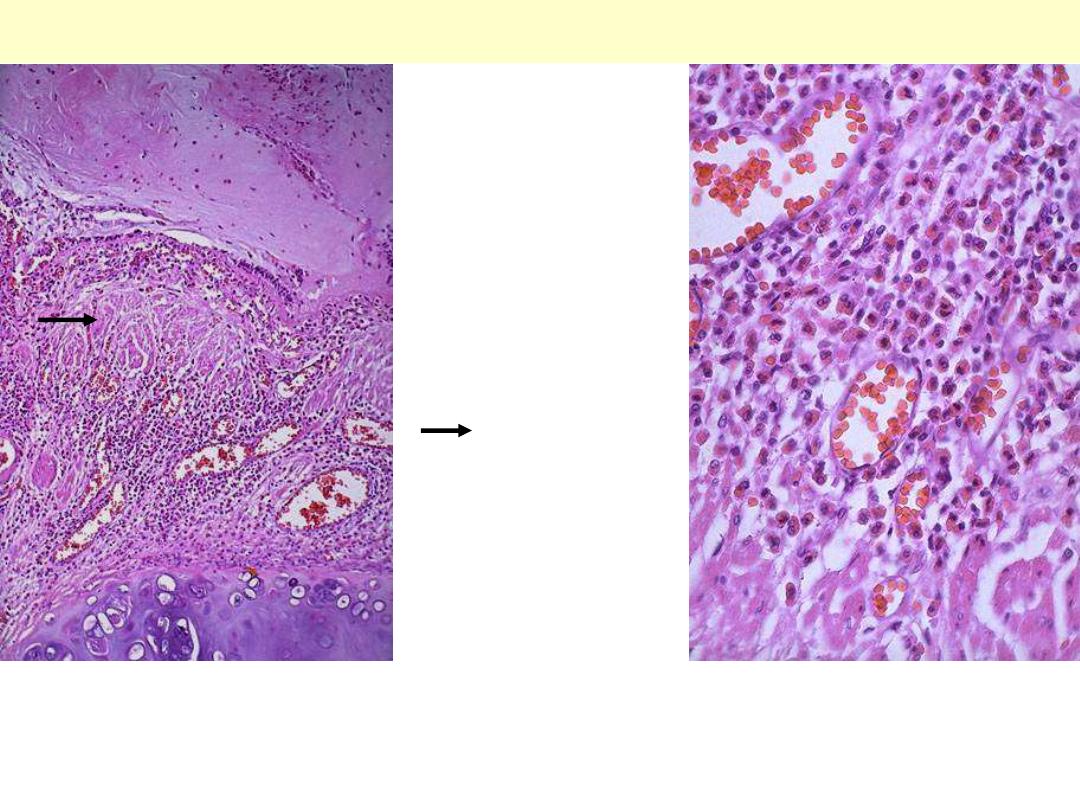
Bronchial asthma
Lt. Between the bronchial cartilage below and the bronchial lumen filled with mucus at the top is a
submucosa widened by smooth muscle hypertrophy (arrow), edema, and inflammation (mainly
eosinophils).
Rt. At high magnification, the numerous eosinophils are prominent from their bright red cytoplasmic
granules.

Chronic bronchitis
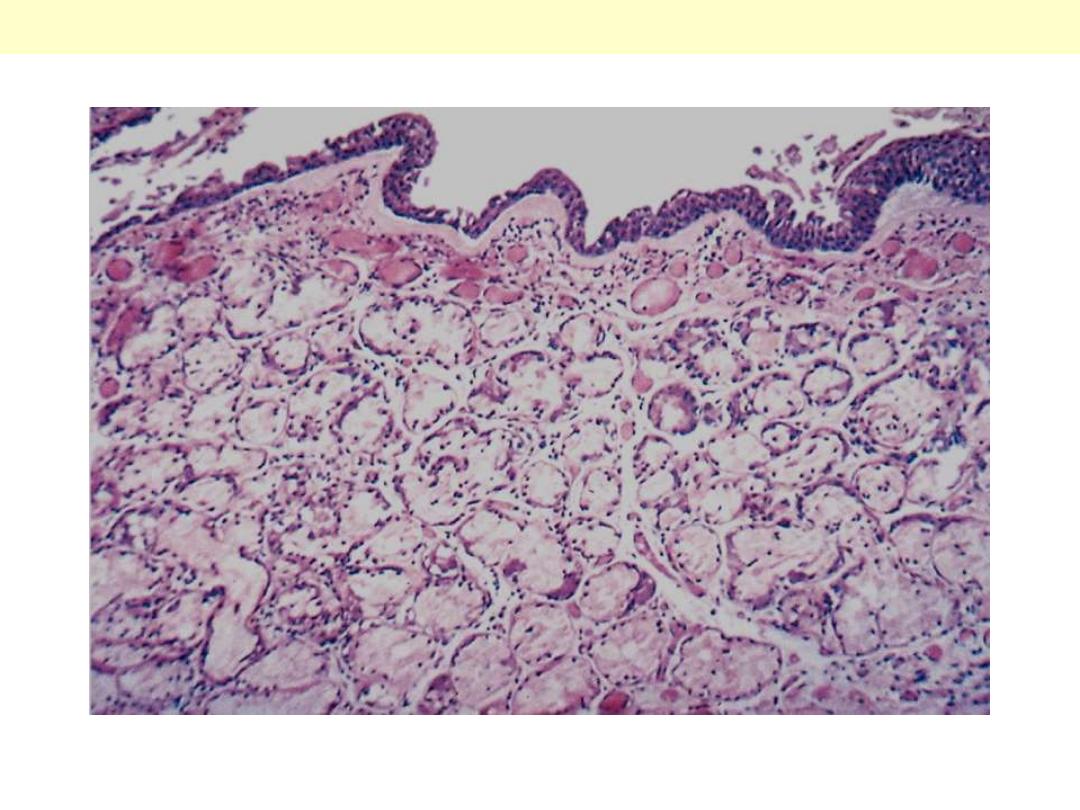
The lumen of the bronchus is above. Note the marked thickening of the mucous gland layer
(approximately twice normal) and squamous metaplasia of lung epithelium.
Chronic bronchitis

Emphysema
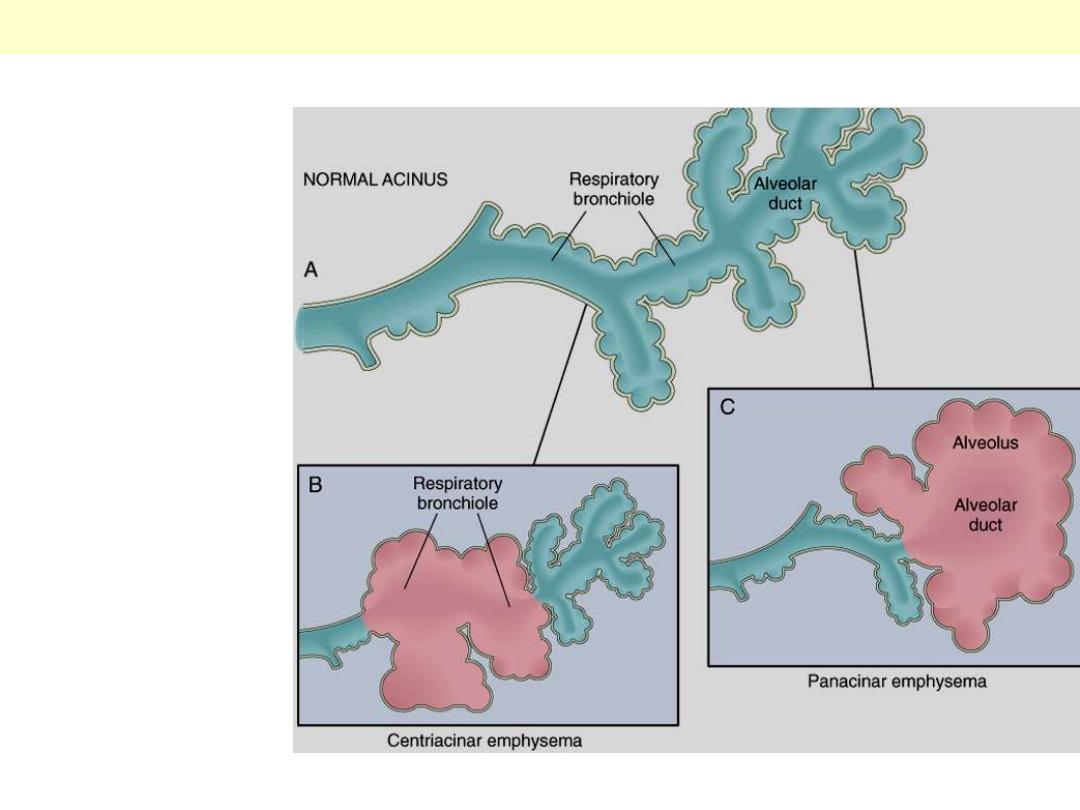
A, Diagram of normal
structures within the
acinus, the fundamental
unit of the lung. A
terminal bronchiole (not
shown) is immediately
proximal to the
respiratory bronchiole.
B, Centrilobular
emphysema with dilation
that initially affects the
respiratory bronchioles.
C, Panacinar emphysema
with initial distention of
the peripheral structures
(i.e., the alveolus and
alveolar duct); the
disease later extends to
affect the respiratory
bronchioles.
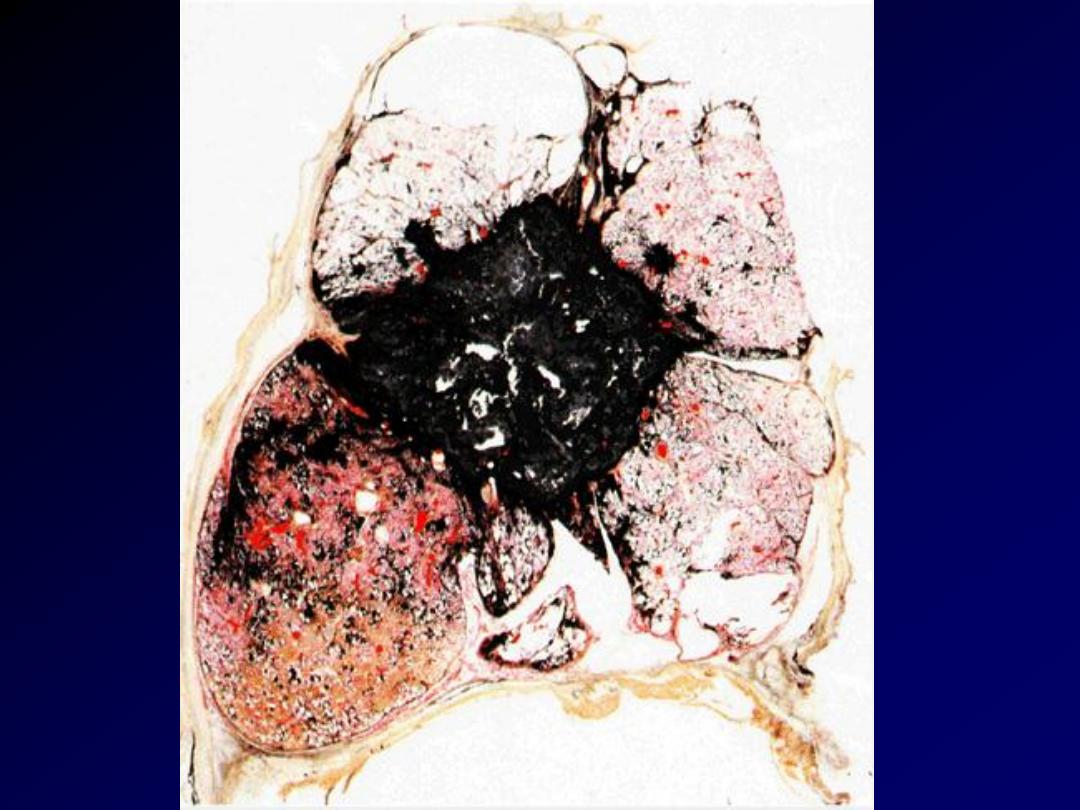
Emphysema Centriacinar Vs Panacinar

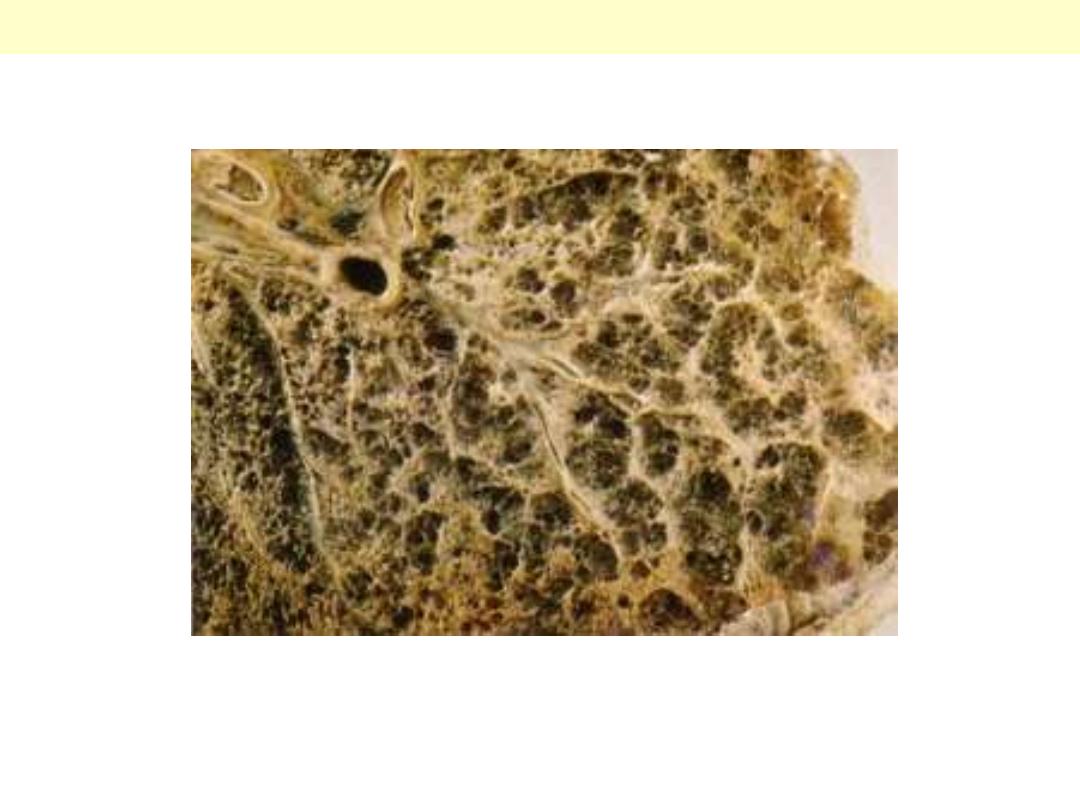
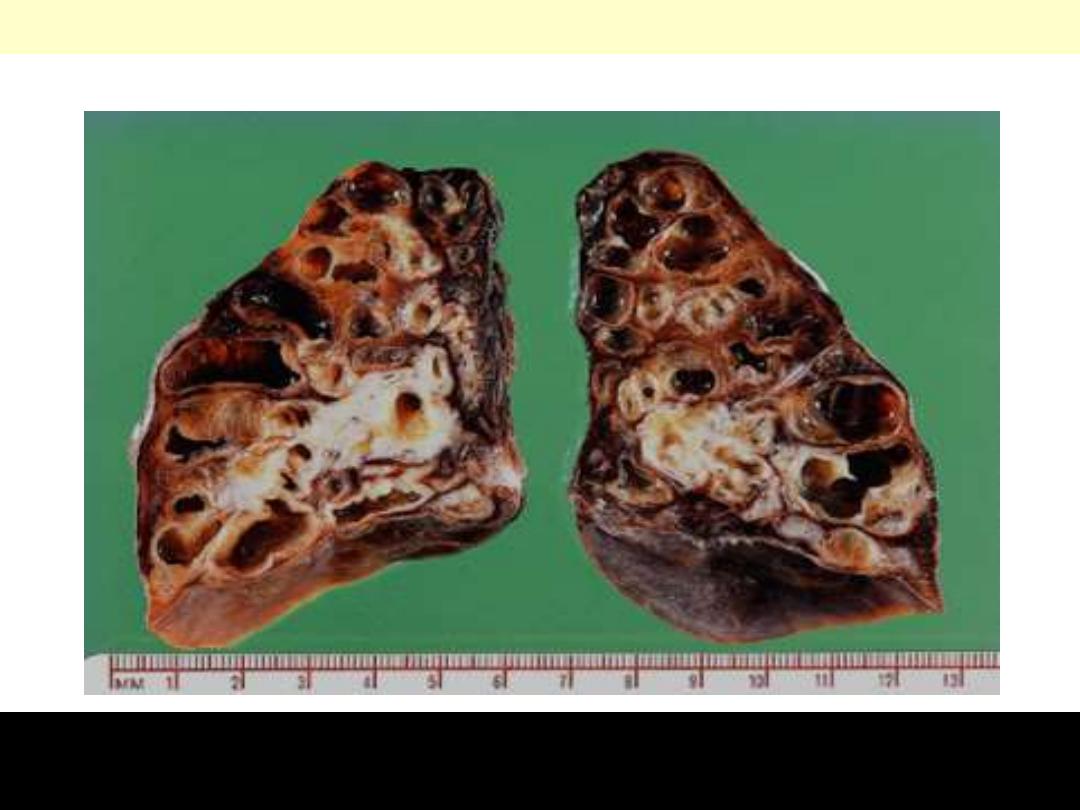
Centrilobular emphysema occurs with loss of the
respiratory bronchioles in the proximal portion
of the acinus, with sparing of distal alveoli. This
pattern is most typical for
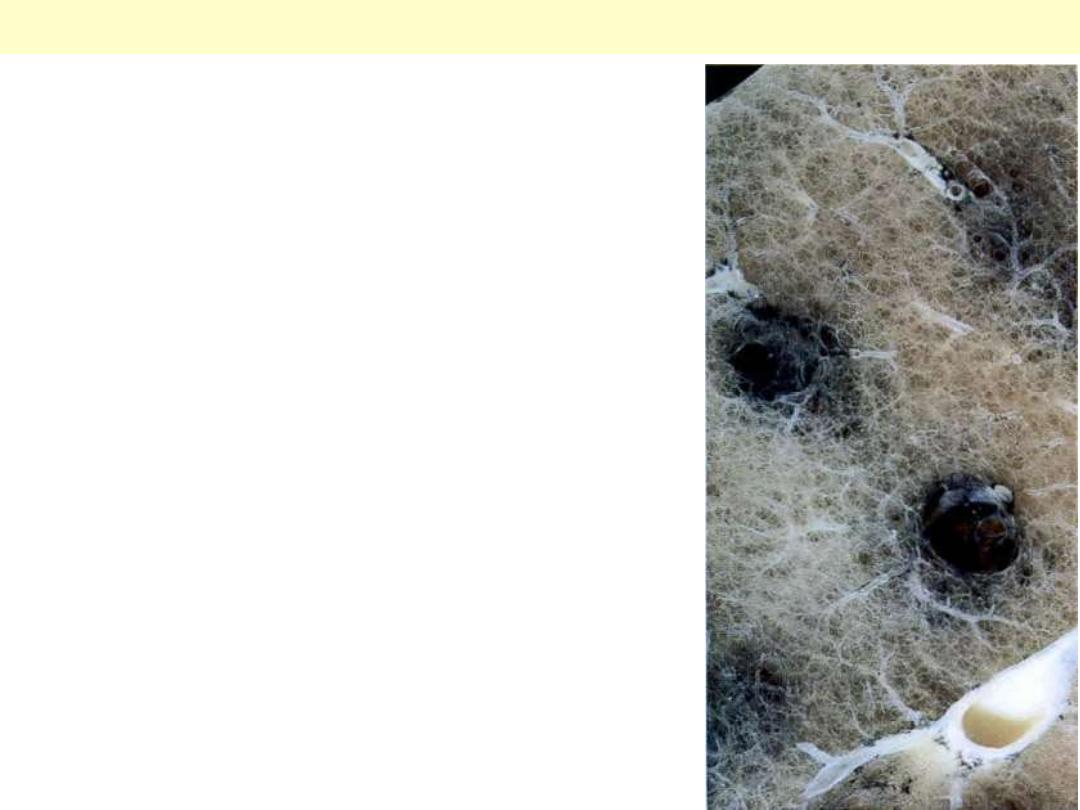
The respiratory bronchioles and some of the alveolar ducts in the
middle of the pulmonary lobules are destroyed. This results in
holes being formed – emphysematous spaces. These areas are
black because of the accumulation of carbon pigment in the
peribronchial lymphatics.
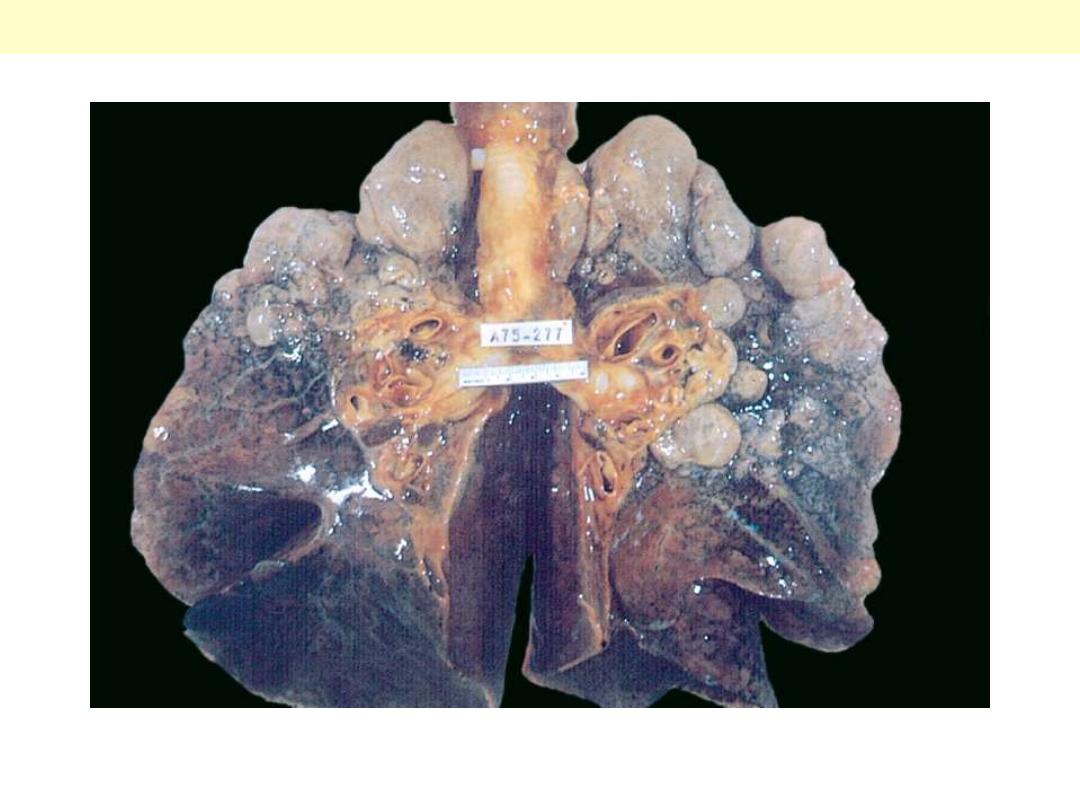
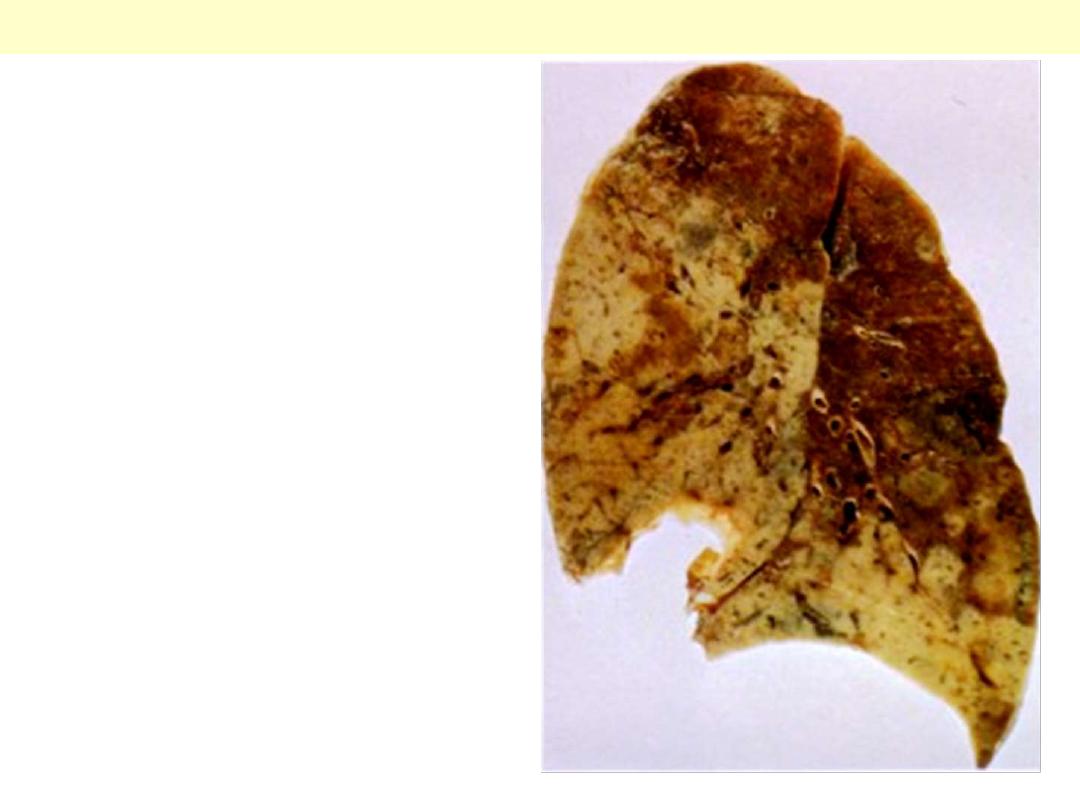
Centrilobular emphysema
There is severe diffuse involvement of the acini; the whole acinus is markedly dilated.
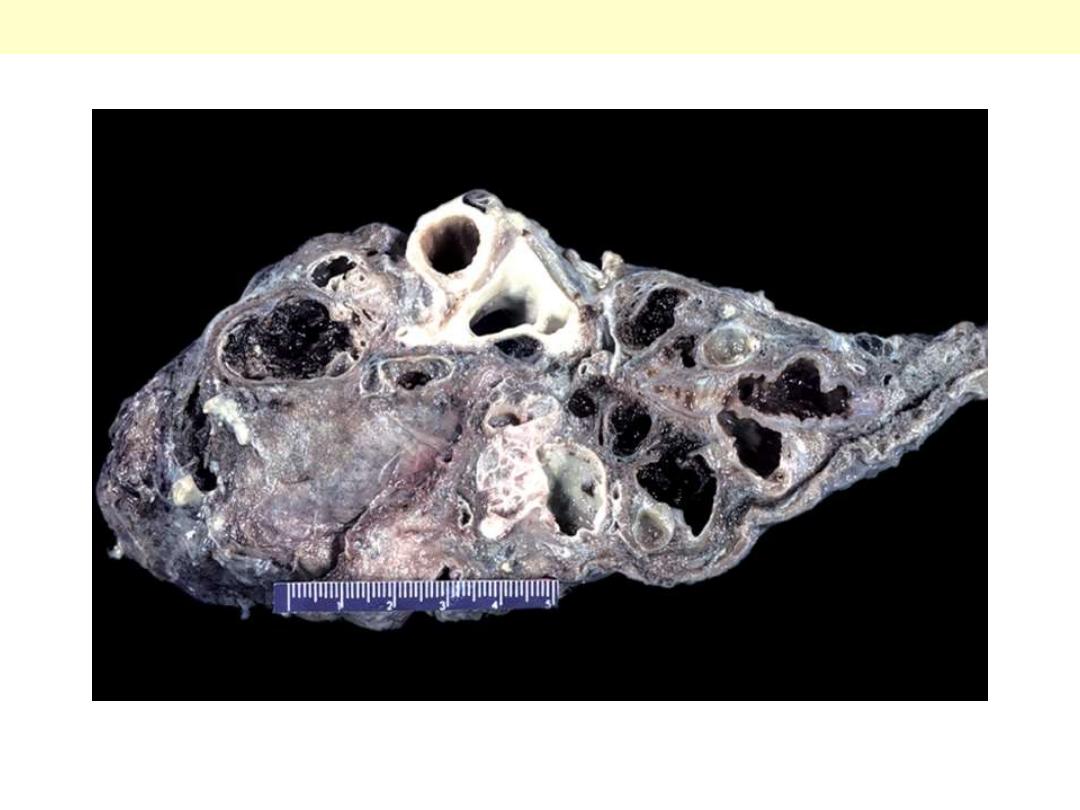
Panacinar emphysema
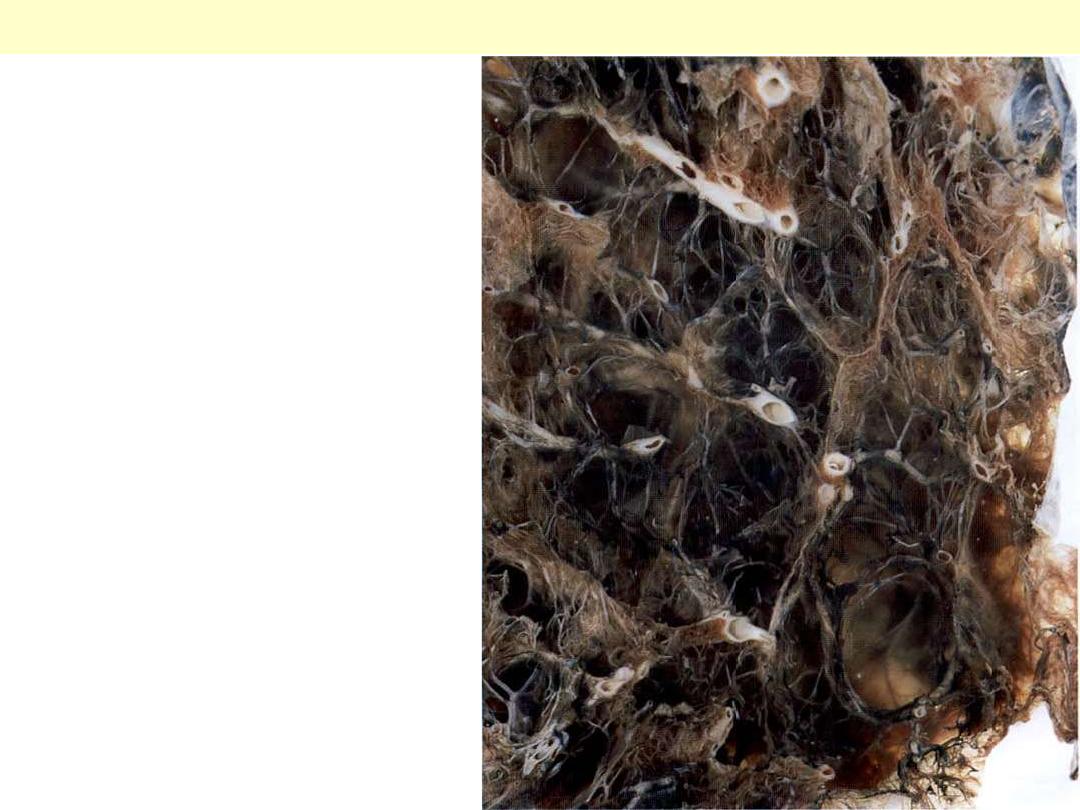
The 'substance' of the lung has been almost
completely lost. When such lungs are
removed from the body they are soft and
can often be squeezed into a small ball. The
pathology can be demonstrated by inflating
the intact lung by running formalin into the
main bronchus, allowing it to float in
formalin for 48 hours for fixation, then
slicing it with a long, sharp knife. As the
lung is cut, the formalin runs out of the
emphysematous spaces but the holey organ
can be examined by immersing the slices in
water, as was done for this photograph.
Pan-acinar destructive emphysema – severe emphysema.
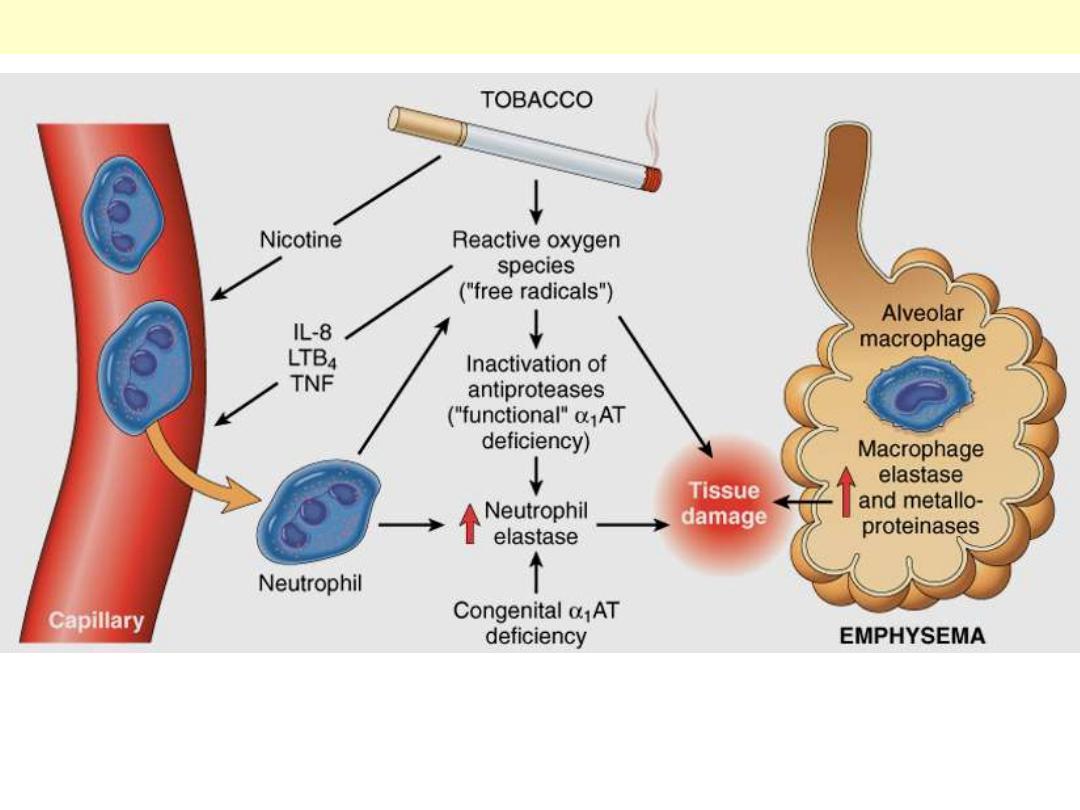
The protease-antiprotease imbalance and oxidant-antioxidant imbalance are additive in their effects
and contribute to tissue damage. α1-Antitrypsin (α1AT) deficiency can be either congenital or
"functional" as a result of oxidative inactivation. See text for details. IL-8, interleukin 8; LTB4,
leukotriene B4; TNF, tumor necrosis factor.
Pathogenesis of emphysema
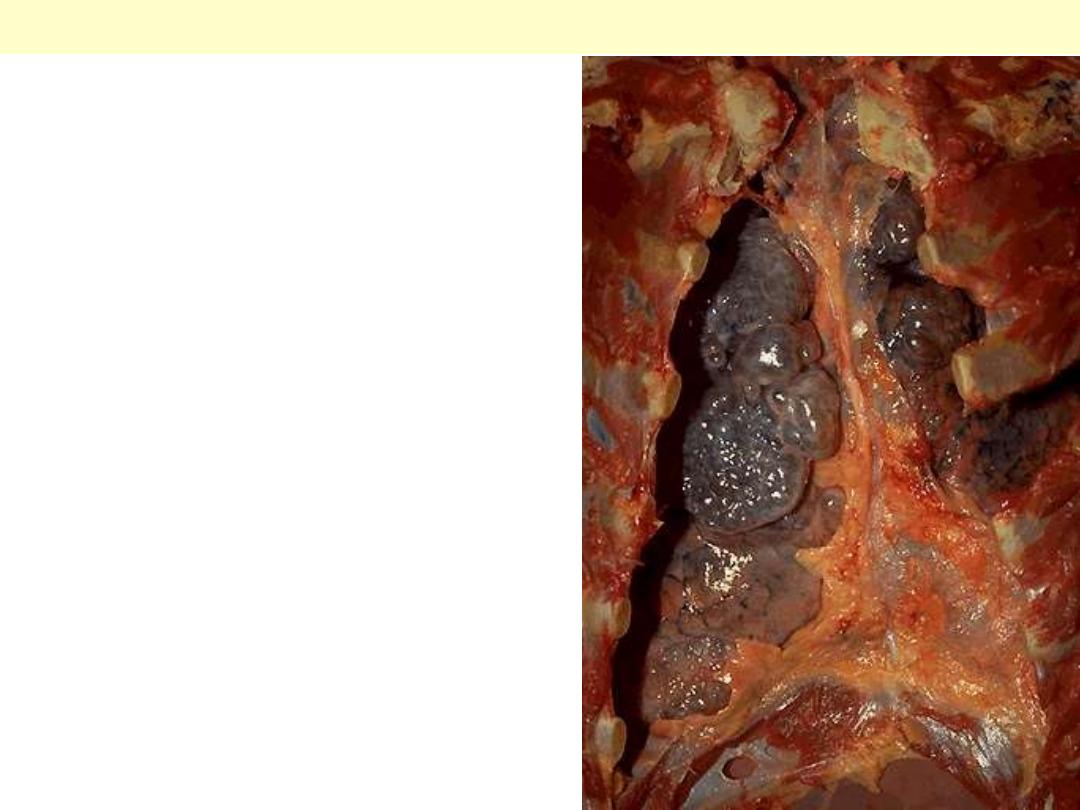
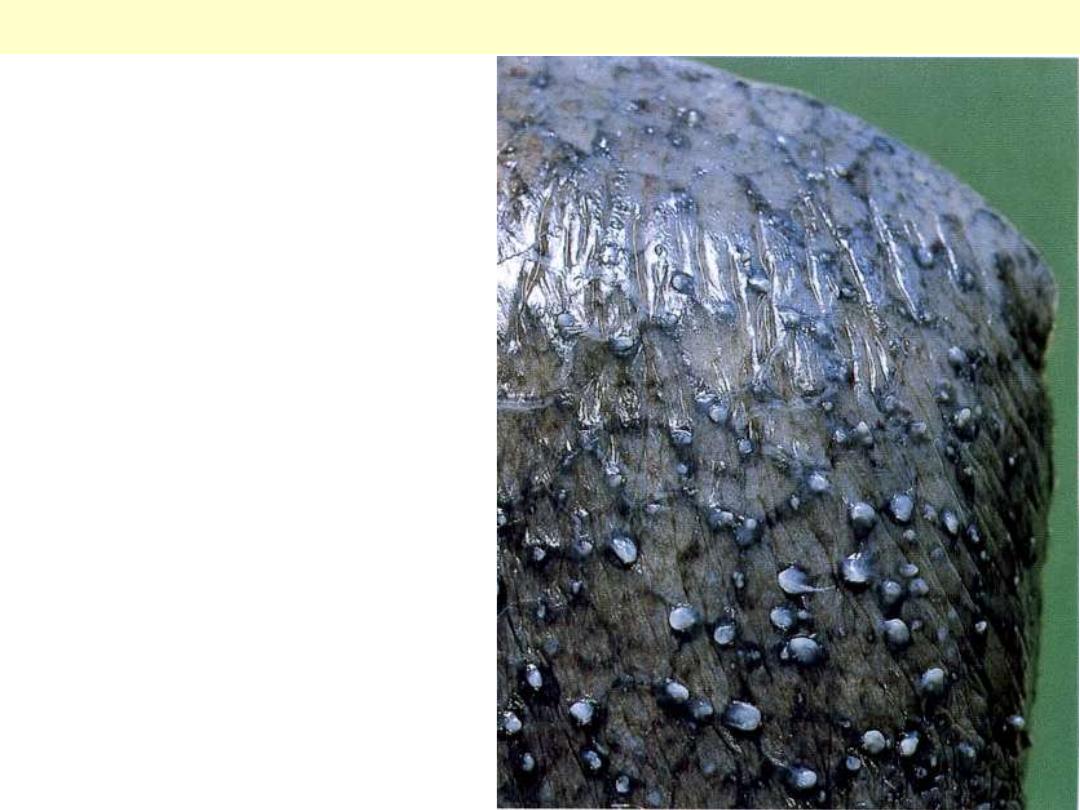
The chest cavity is opened at autopsy to reveal
numerous large bullae apparent on the surface of the
lungs in a patient dying with emphysema. Bullae are
large dilated airspaces that bulge out from beneath
the pleura. Emphysema is characterized by a loss of
lung parenchyma by destruction of alveoli so that
there is permanent dilation of airspaces.
Advanced emphysema
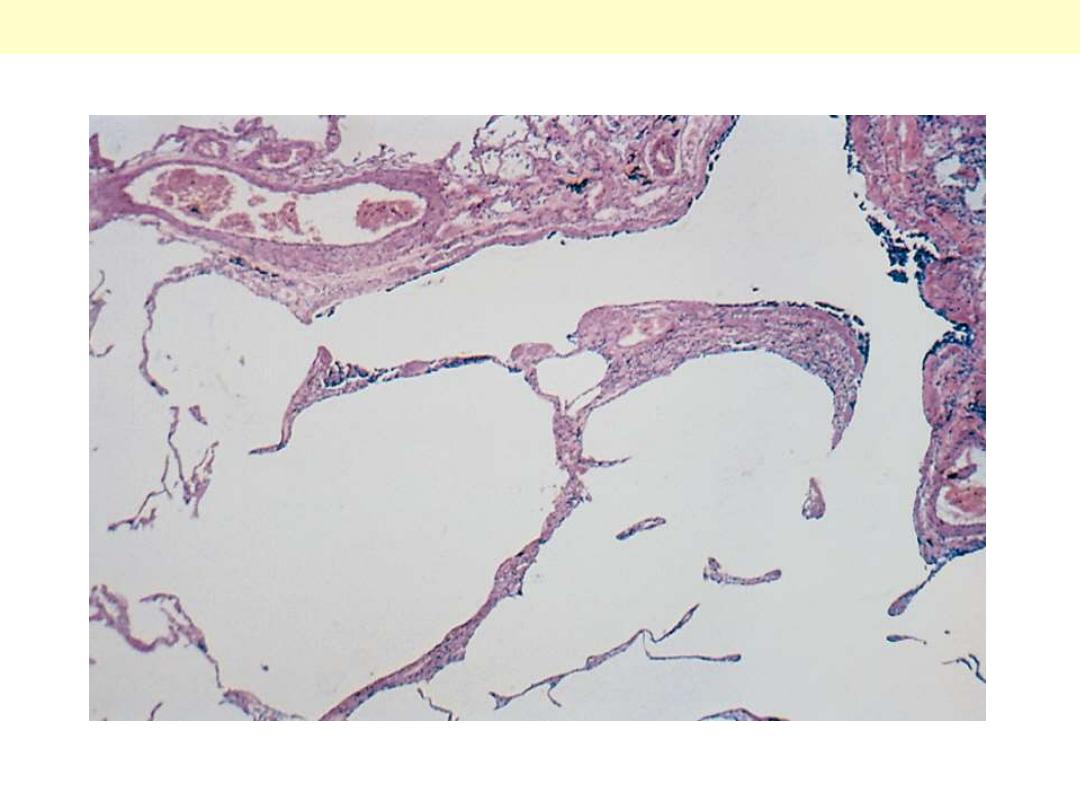
There is marked enlargement of airspaces, with thinning and destruction of alveolar septa. (
Pulmonary emphysema
There are large apical and subpleural bullae
Bullous emphysema

Infections

Pneumonia

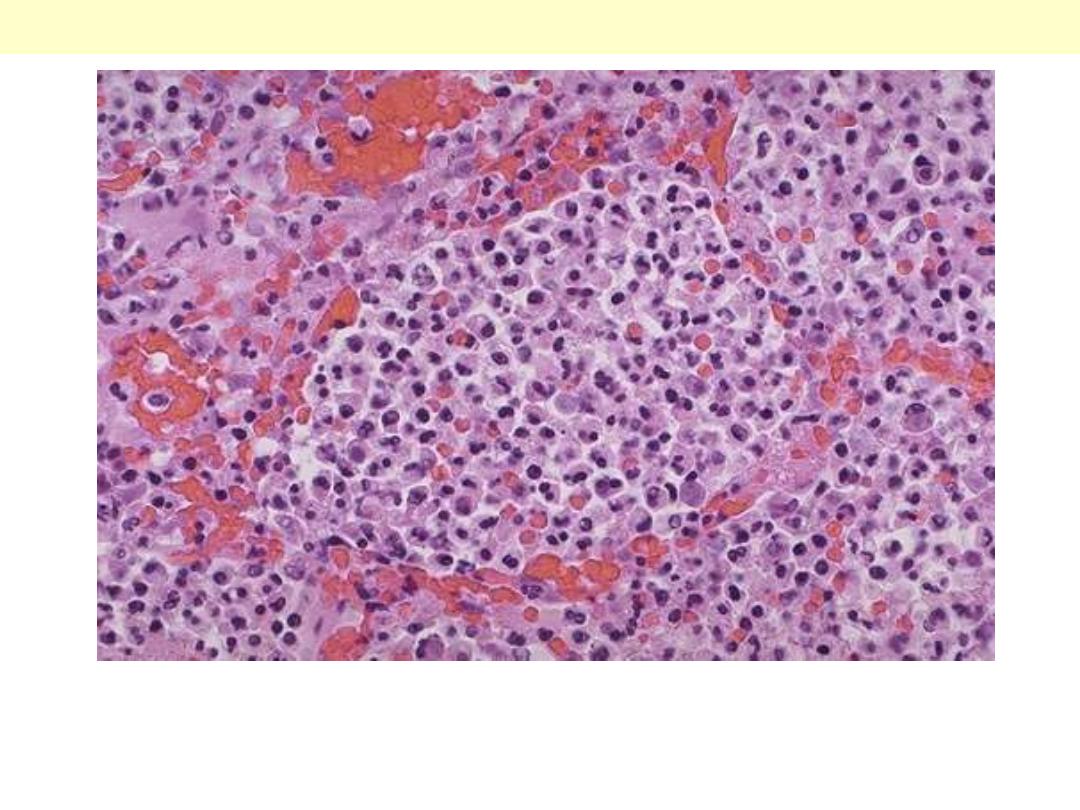
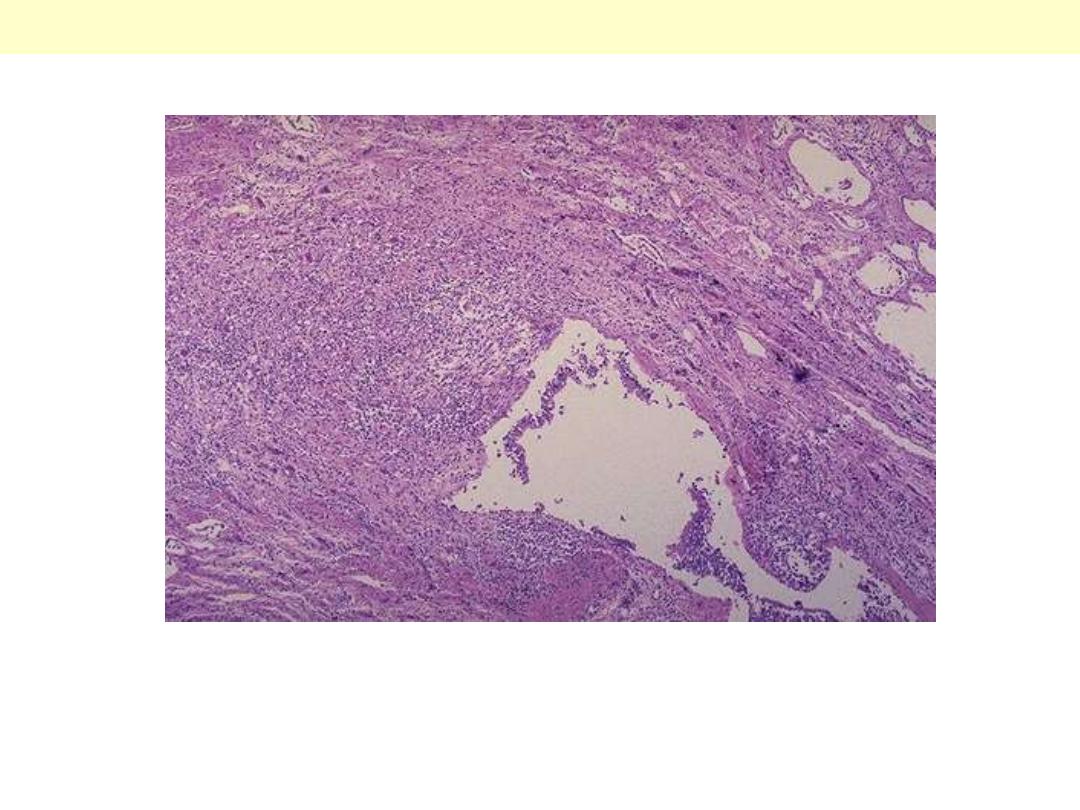
Pneumonia – Atypical
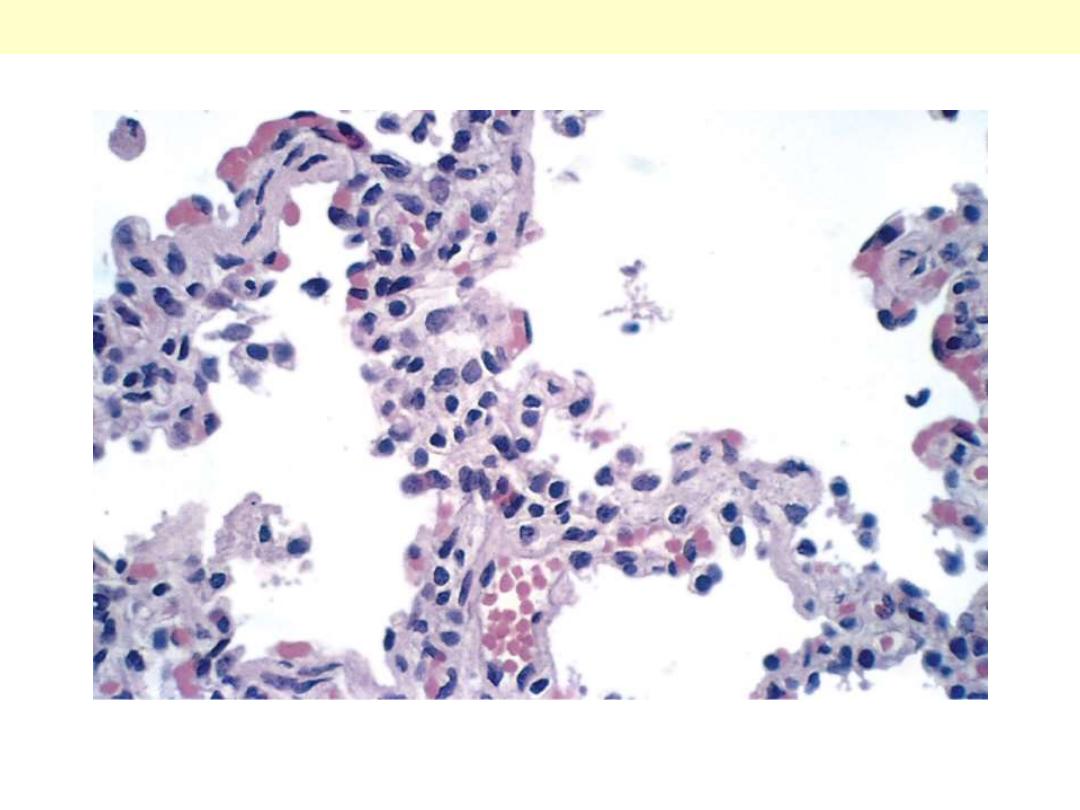
The thickened alveolar walls are heavily infiltrated with mononuclear leukocytes.
Atypical pneumonia

Penumonia - Broncho
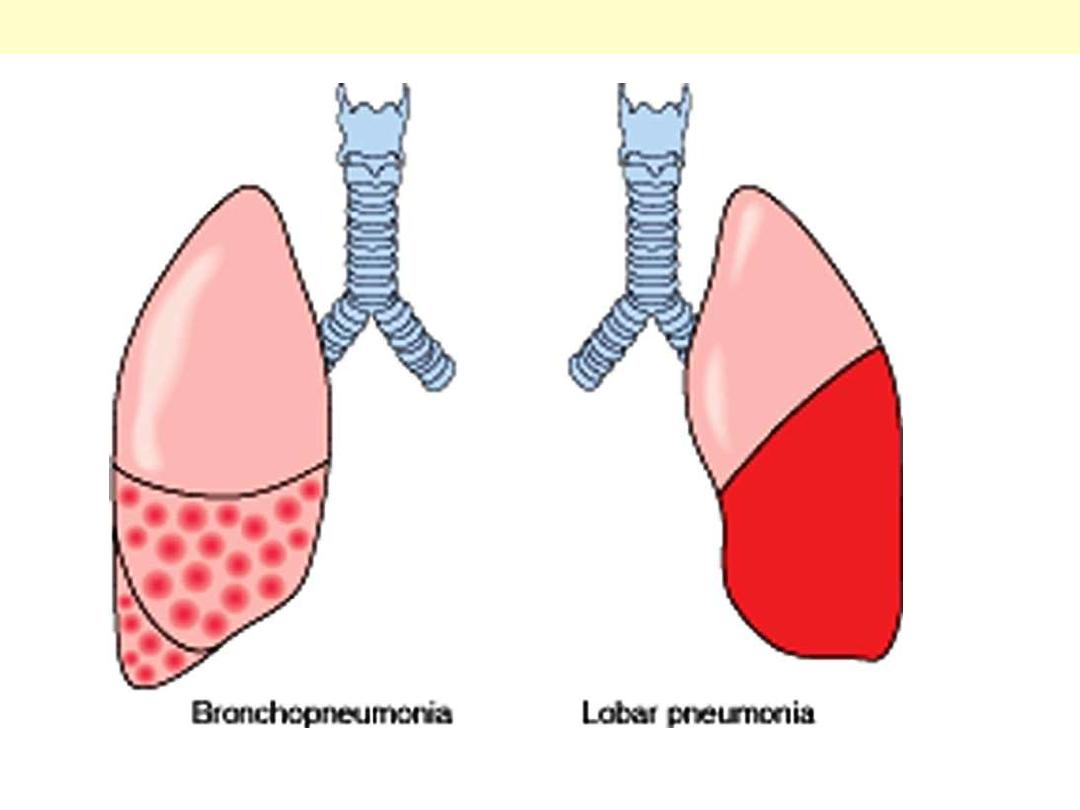
The anatomic distribution of bronchopneumonia and lobar pneumonia.
Bronchopneumonia Vs lobar pneumonia
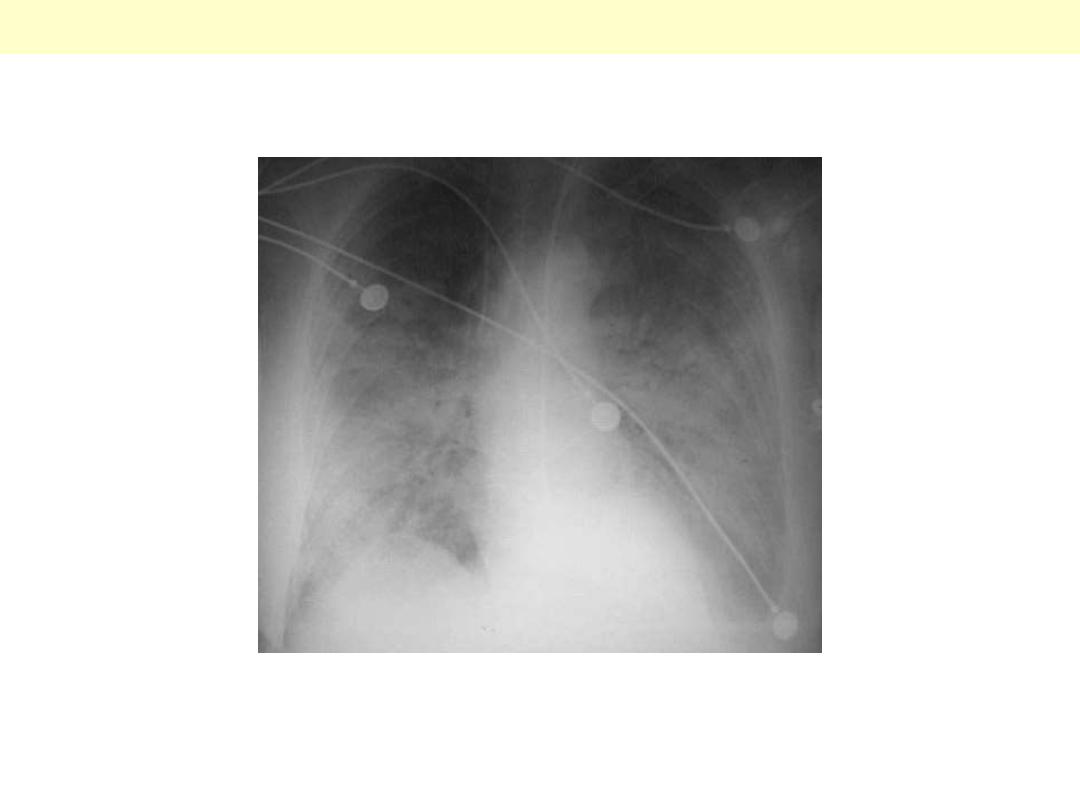
Patchy infiltrates consistent with a bronchopneumonia from a bacterial infection. Typical organisms
include Streptococcus pneumoniae, Staphylococcus aureus, Pseudomonas aeruginosa, Hemophilus
influenzae, Klebsiella pneumoniae, among others.
CXR: bronchopneumonia
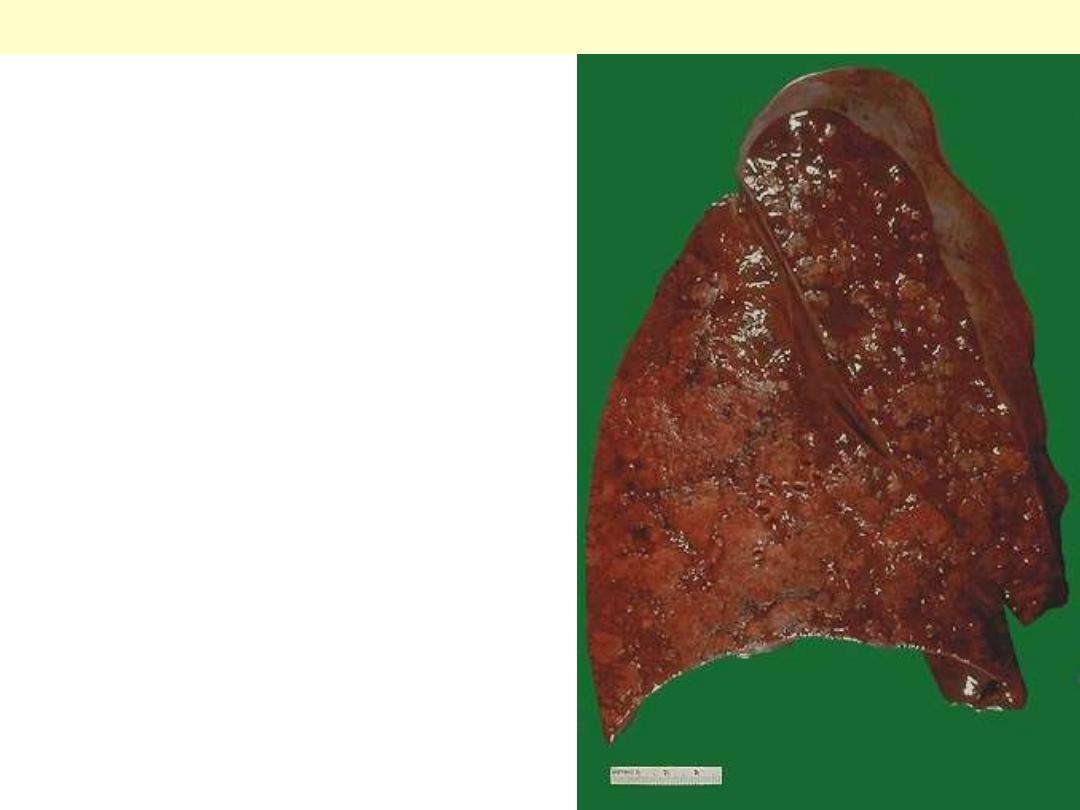
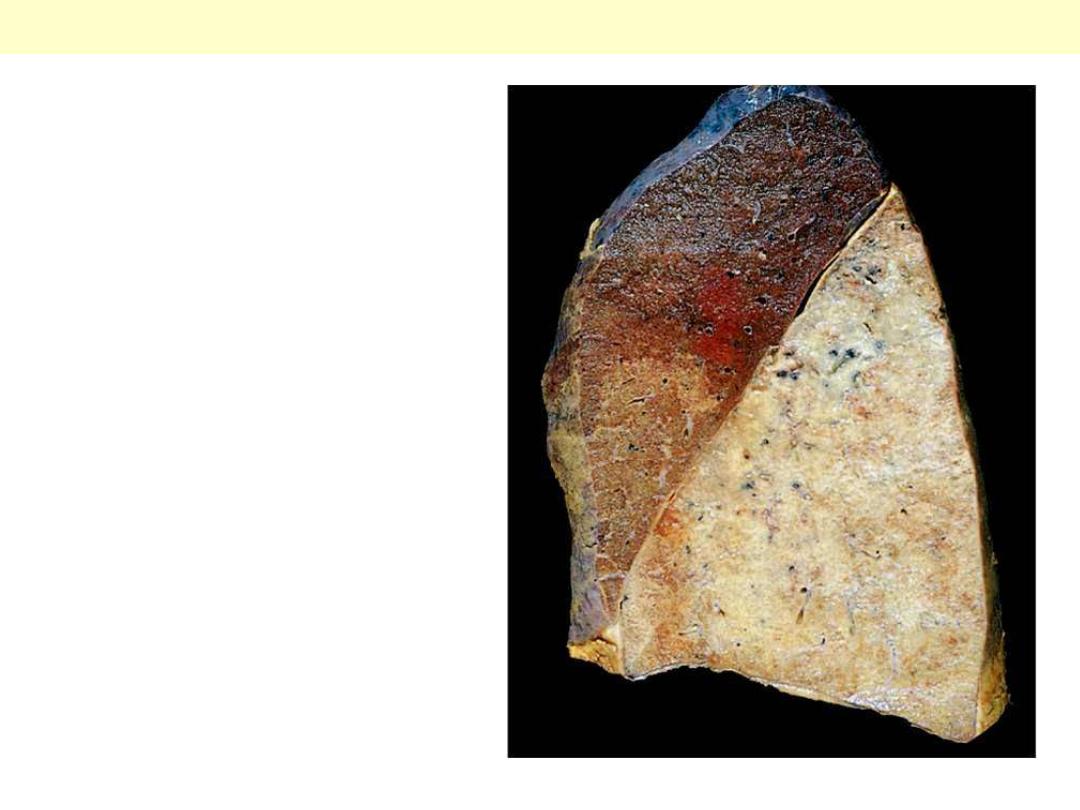
The cut surface of this lung demonstrates the typical
appearance of a bronchopneumonia with areas of
tan-yellow consolidation. Remaining lung is dark red
because of marked pulmonary congestion.
Bronchopneumonia (lobular pneumonia) is
characterized by patchy areas of pulmonary
consolidation. These areas become almost confluent
in the left lower lobe on the bottom left of the
photograph. The areas of consolidation are firmer
than the surrounding lung.
Bronchopneumonia
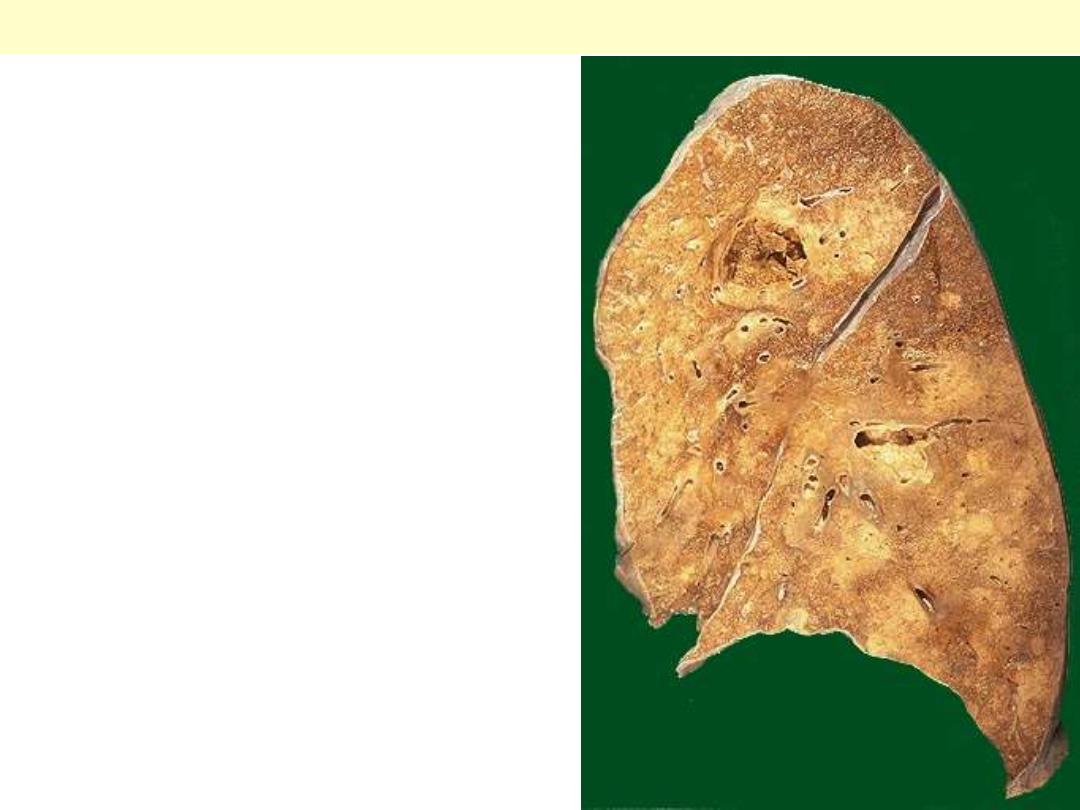
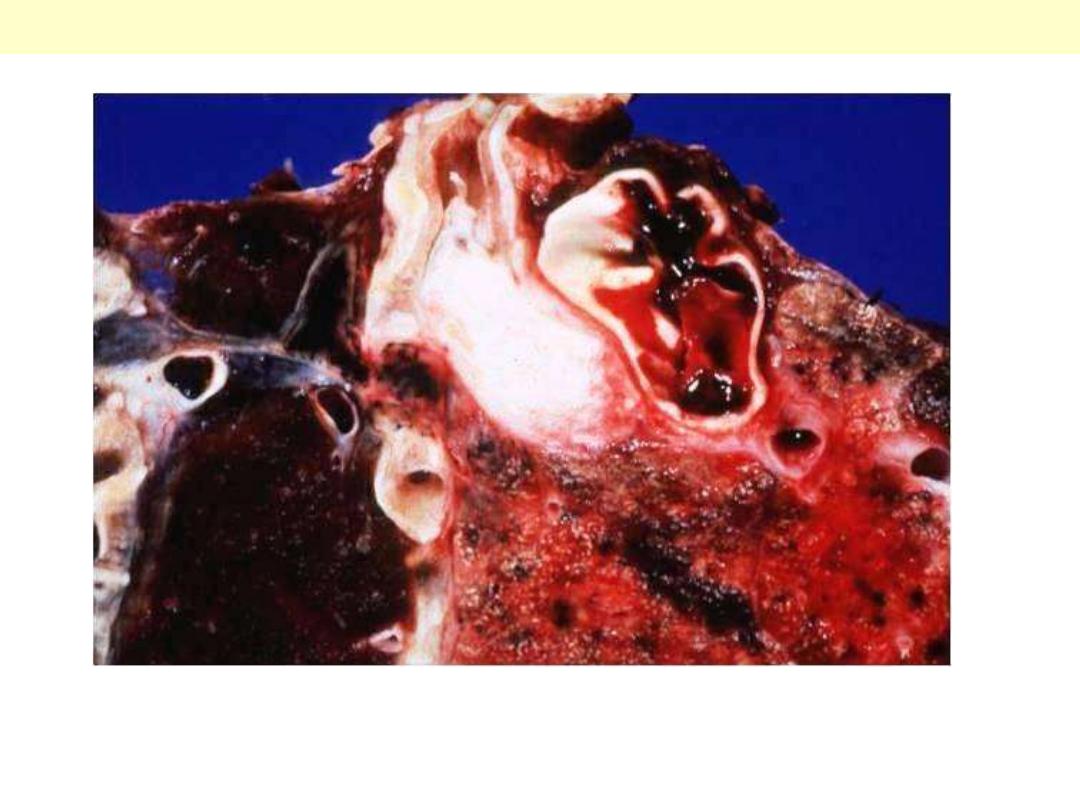
Two lung abscesses, one in the upper lobe and one in
the lower lobe of this left lung. An abscess is a
complication of severe pneumonia, most typically
from virulent organisms such as S. aureus.
Abscesses complicating bronchopneumonia
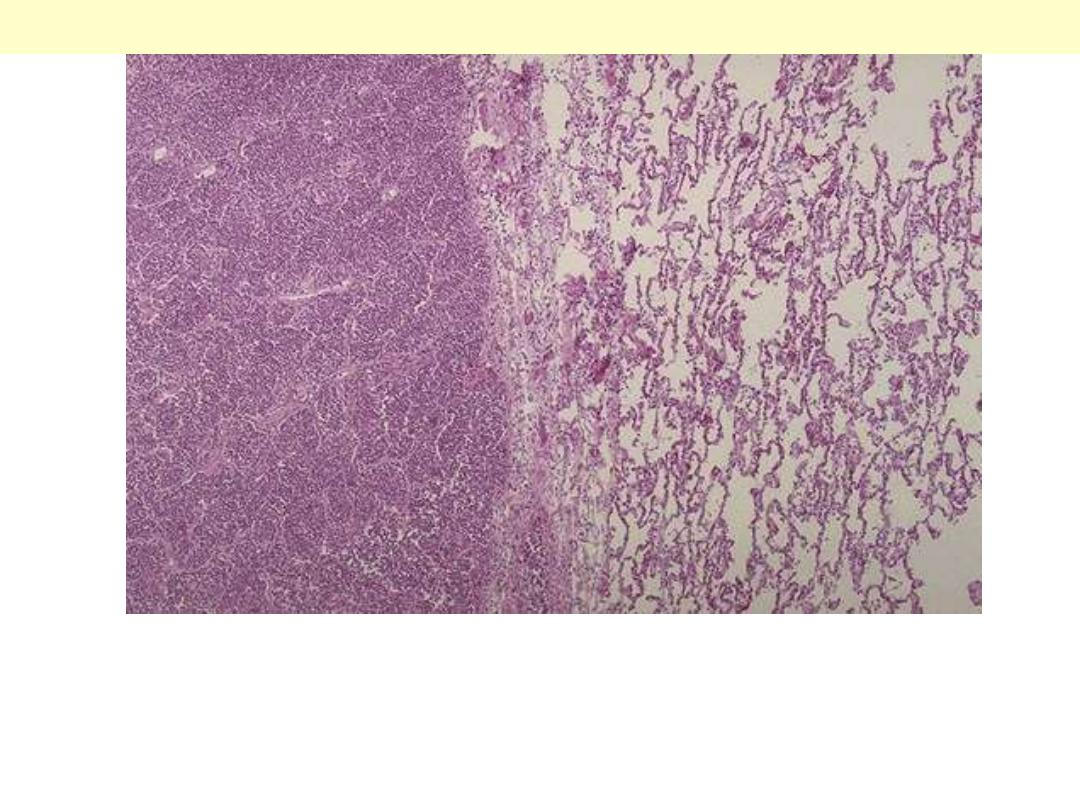
At the left the alveoli are filled with a neutrophilic exudate that corresponds to the areas of consolidation
seen grossly with the bronchopneumonia. This contrasts with the aerated lung on the right of this
photomicrograph.
Bronchopneumonia
At high magnification, the alveolar exudate of mainly neutrophils is seen. The surrounding alveolar walls
have capillaries that are dilated and filled with RBC's. Such an exudative process is typical for bacterial
infection. This exudate gives rise to the productive cough of purulent yellow sputum seen with bacterial
pneumonias.
Bronchopneumonia

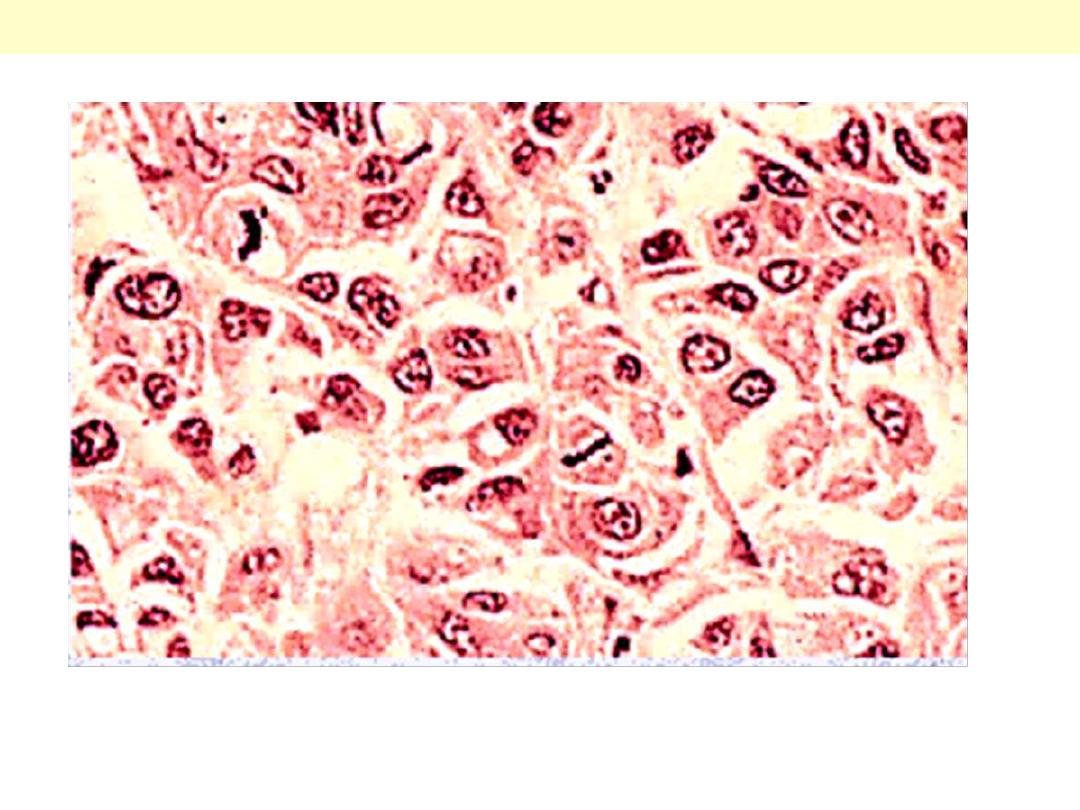
Pneumonia - CMV
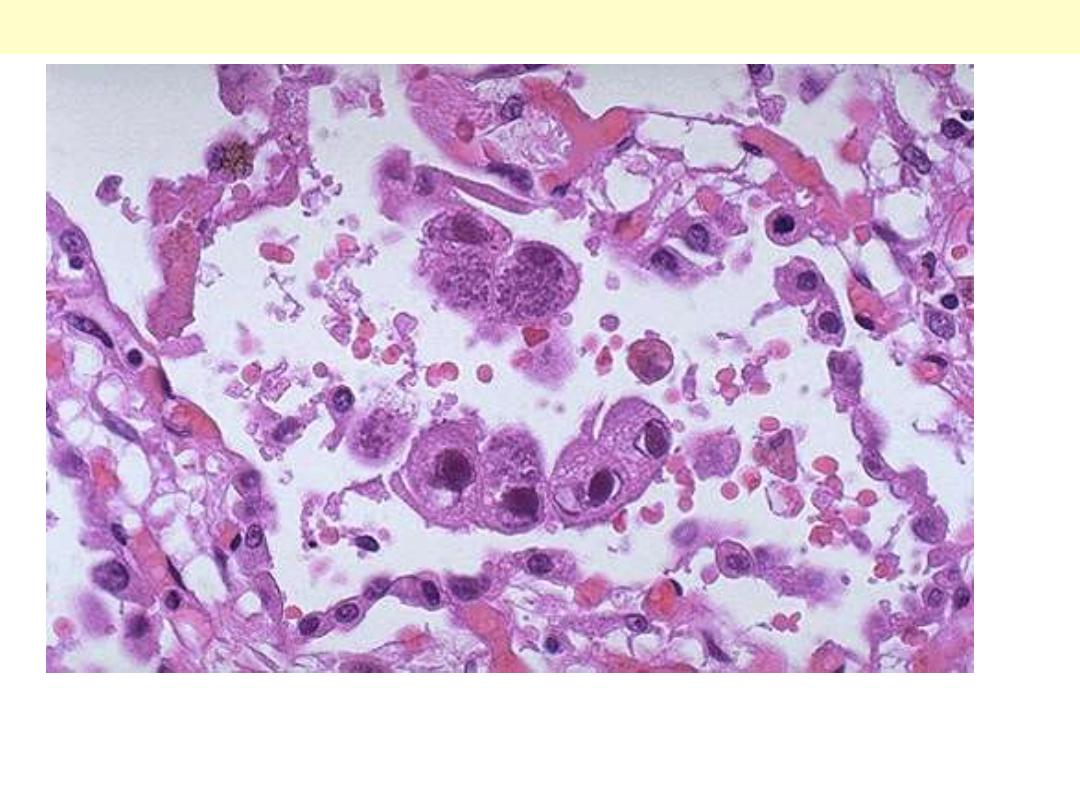
This is cytomegalovirus (CMV) infection in the lung. Note the very large cells that have large violet
intranuclear inclusions with a small clear halo. Basophilic stippling can be seen in the cytoplasm.
Pulmonary CMV infection

Pneumonia - Lobar
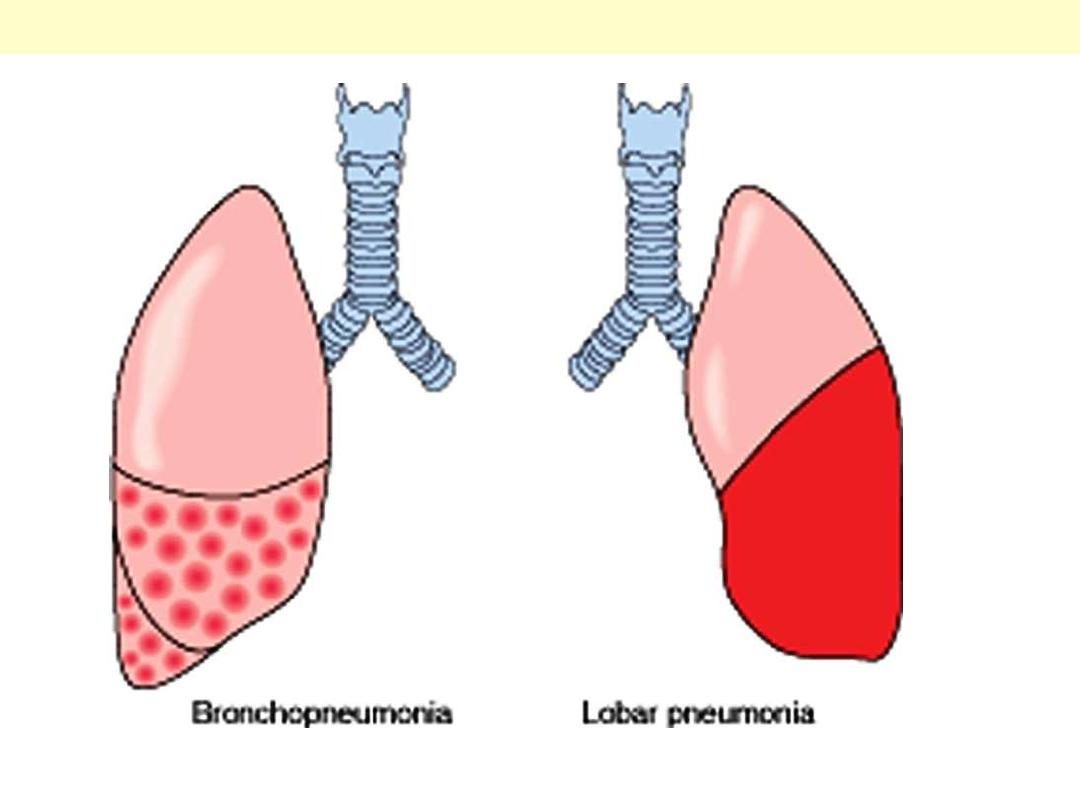
The anatomic distribution of bronchopneumonia and lobar pneumonia.
Bronchopneumonia Vs lobar pneumonia
Gross view of lobar pneumonia with gray
hepatization. The lower lobe is uniformly
consolidated
Lobar pneumonia
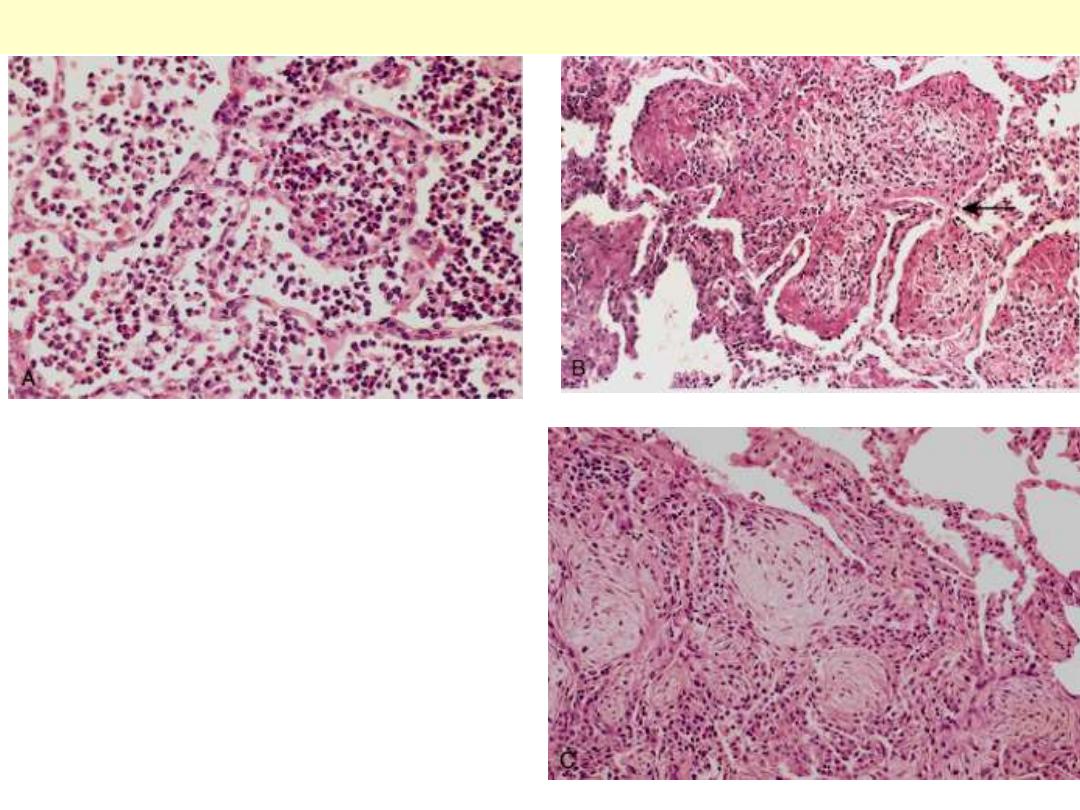
A, Acute pneumonia. The congested septal
capillaries and extensive neutrophil exudation
into alveoli corresponds to early red
hepatization. Fibrin nets have not yet formed. B,
Early organization of intra-alveolar exudates,
seen in areas to be streaming through the pores
of Kohn (arrow). C, Advanced organizing
pneumonia, featuring transformation of
exudates to fibromyxoid masses richly
infiltrated by macrophages and fibroblasts.
Stages of Streptococcus (Pneumococcal) pneumoniae

Pneumonia – Necrotizing +
Abscess
Lung Abscess complicating aspiration pneumonia
Bronchopneumonia (solid grey-yellow area) with abscess formation (cystic ragged area) in 2-year-old
boy secondary to aspiration of foreign body.
Lung Abscess
Early abscess; the alveolar walls are not clearly seen, only sheets of neutrophils are present.

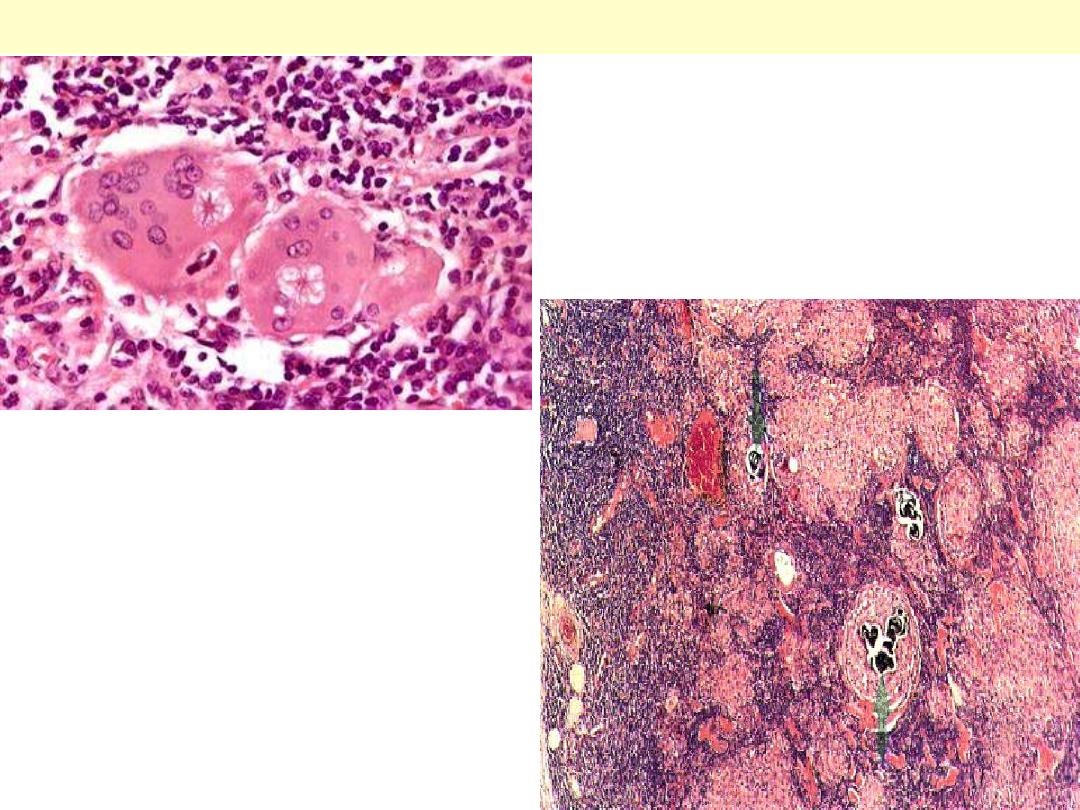
Pneumonia - Pneumocystits
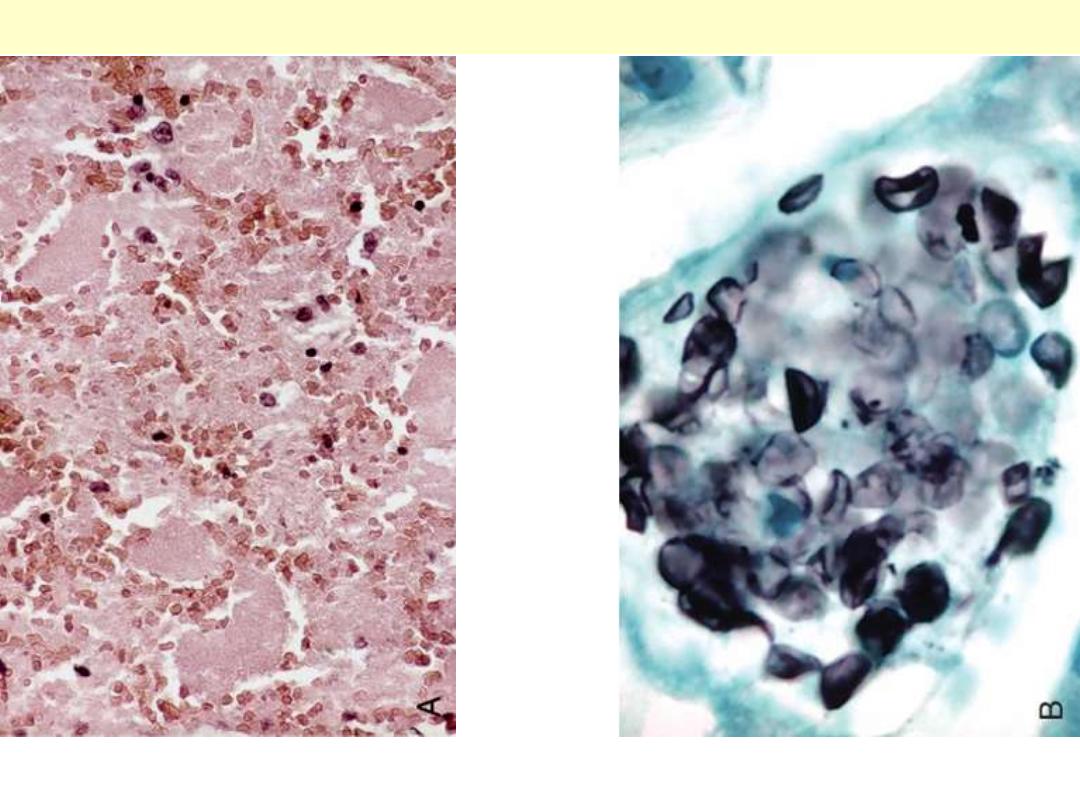
A, The alveoli are filled with a characteristic foamy "cotton candy" exudate. B, Silver stain
demonstrates cup-shaped cysts (5-8 μm in diameter) within the exudate.
Pneumocystis pneumonia

Candidiasis
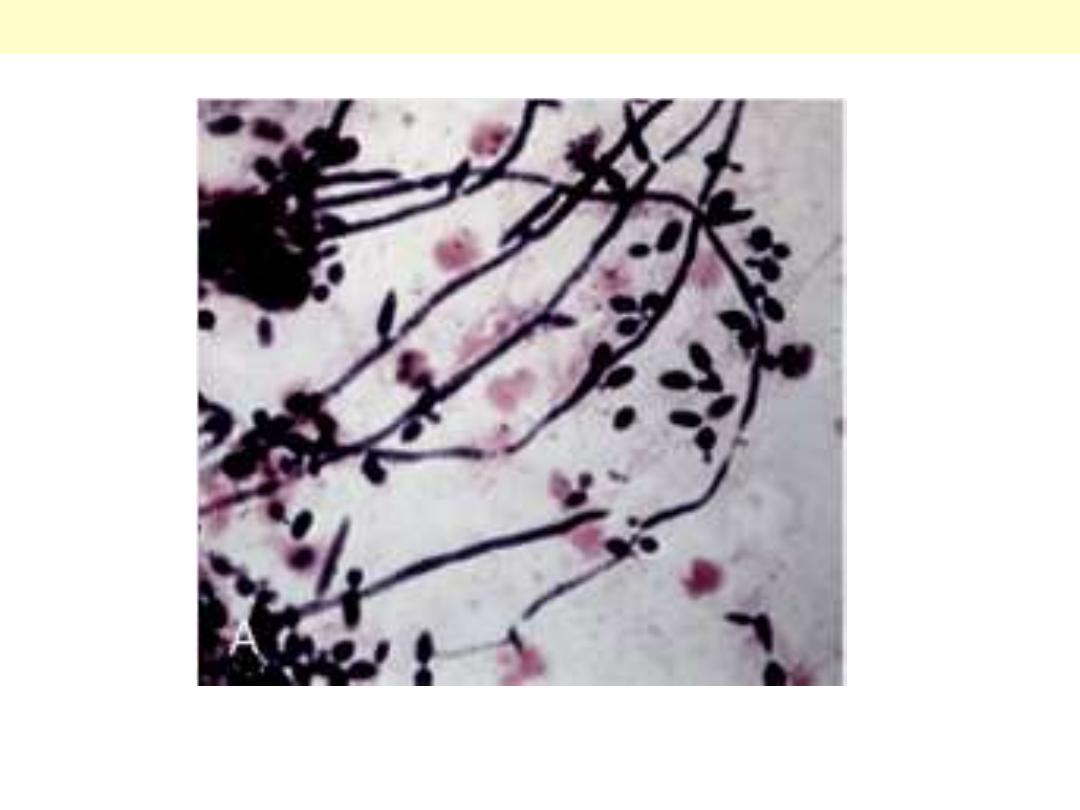
The diagnosis of candidiasis is made by observing the characteristic pseudohyphae and budding yeasts
in tissue sections or exudates. (silver stain)
Candidiasis

Cryptococcosis
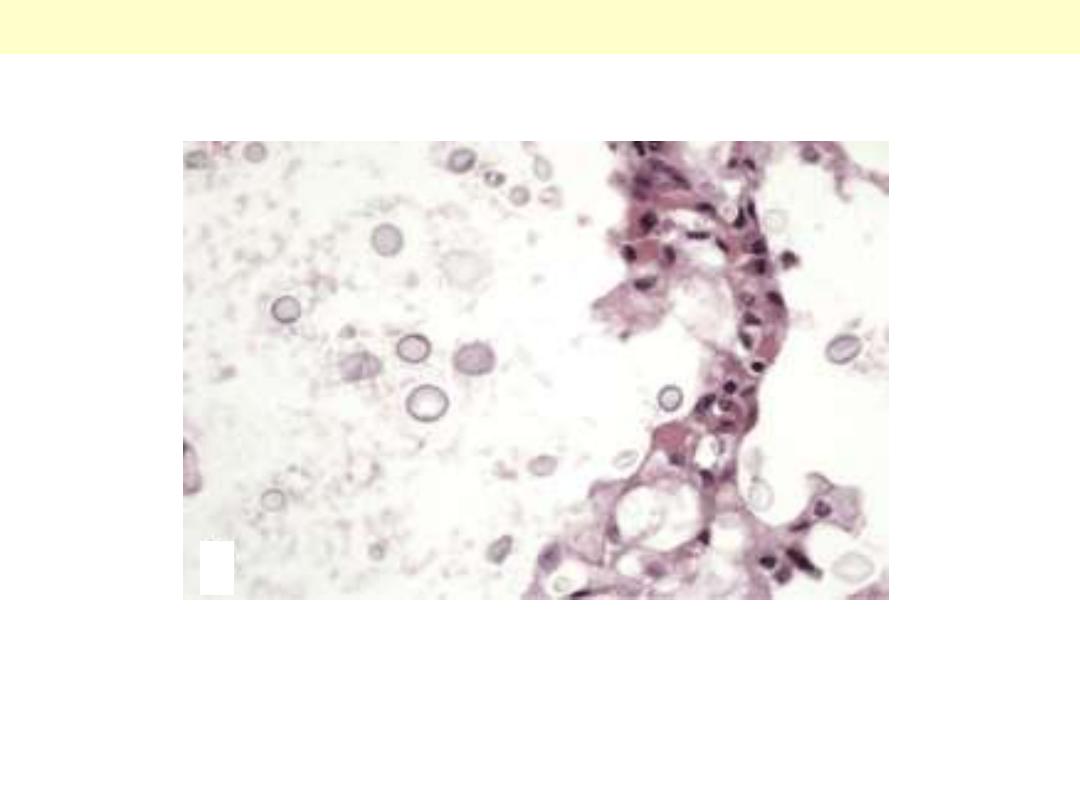
Cryptococcosis of the lung in a patient with AIDS. The yeast forms are somewhat variable in size;
unlike in Candida, pseudohyphae are not seen.
Cryptococcosis

Fungul infection
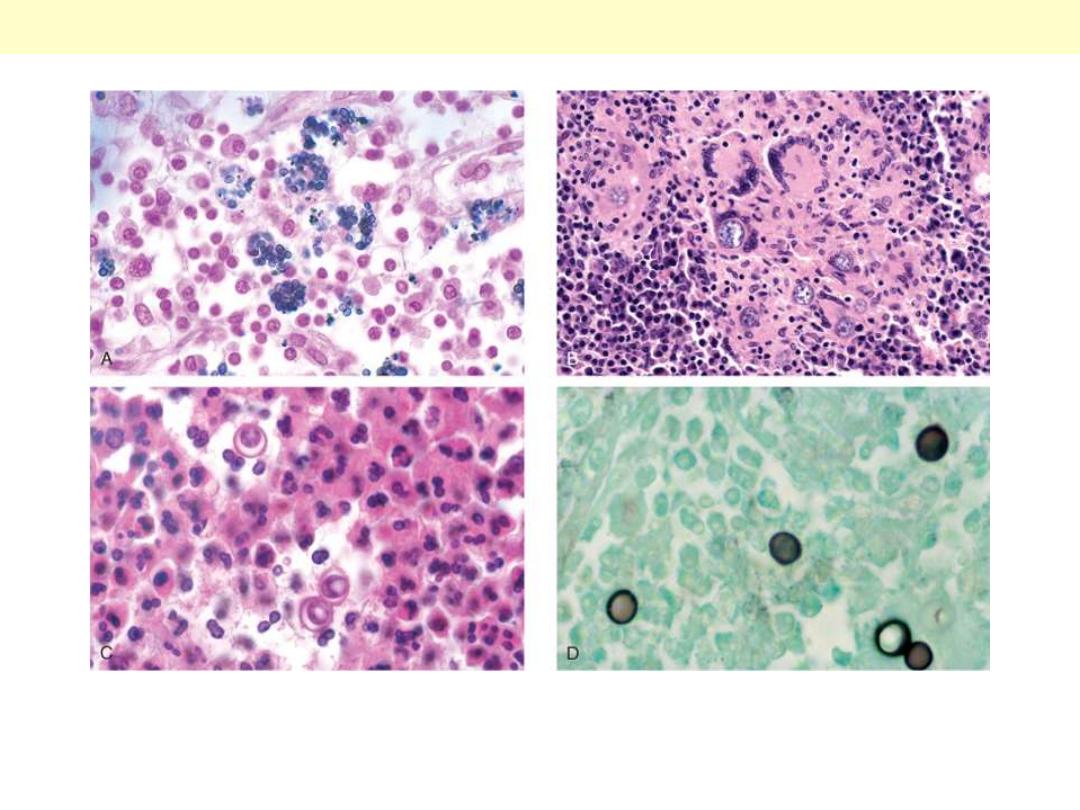
A, Histoplasma capsulatum yeast forms fill phagocytes in a lymph node of a person with disseminated
histoplasmosis. B, Coccidioidomycosis with intact spherules within multinucleated giant cells. C,
Blastomycosis, with rounded budding yeasts, larger than neutrophils. Note the characteristic thick wall
and nuclei (not seen in other fungi). D, Silver stain highlighting broad-based budding.
Fungal infections lung

Molds – Oppurtunistic
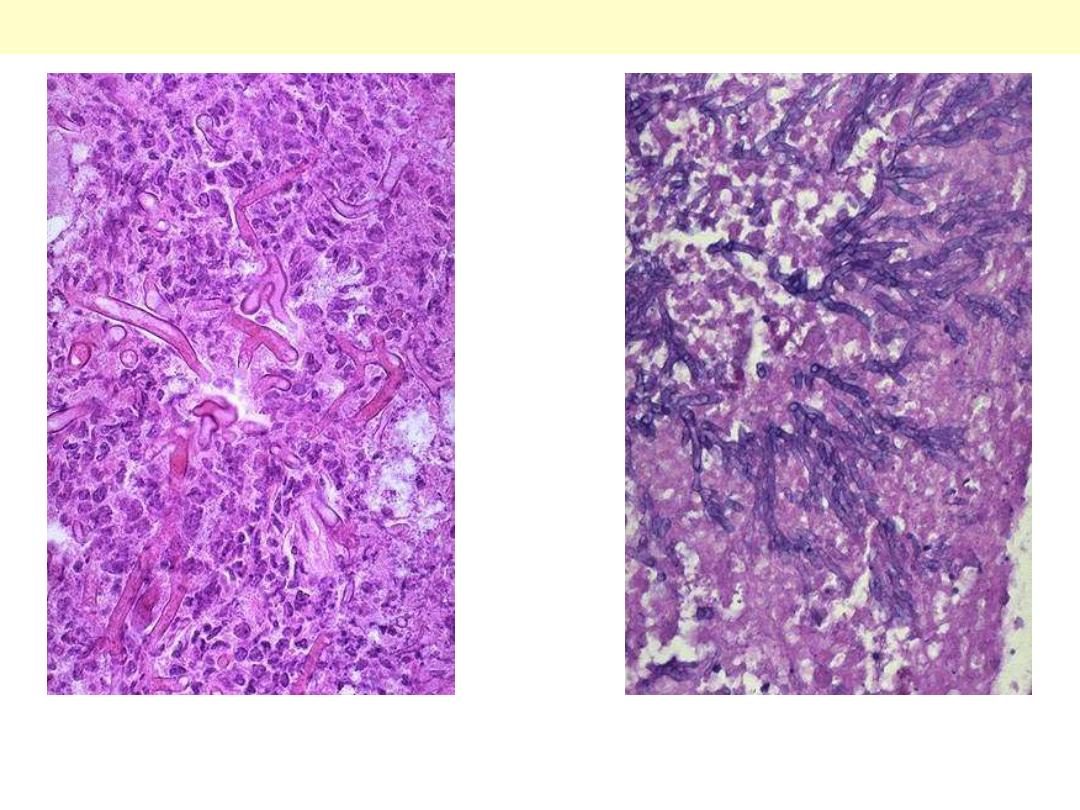
Rt. Mucor produces broad, short, non-septate hyphae that branch at right angles.
Lt. The hyphae of Aspergillus are septate and branch at more acute angles
Mucormycosis Vs Aspergillosis

TB
The gray-white parenchymal focus
is under the pleura in the lower
part of the upper lobe. Hilar
lymph nodes with caseation are
seen on the left.
Primary pulmonary tuberculosis (Ghon complex)
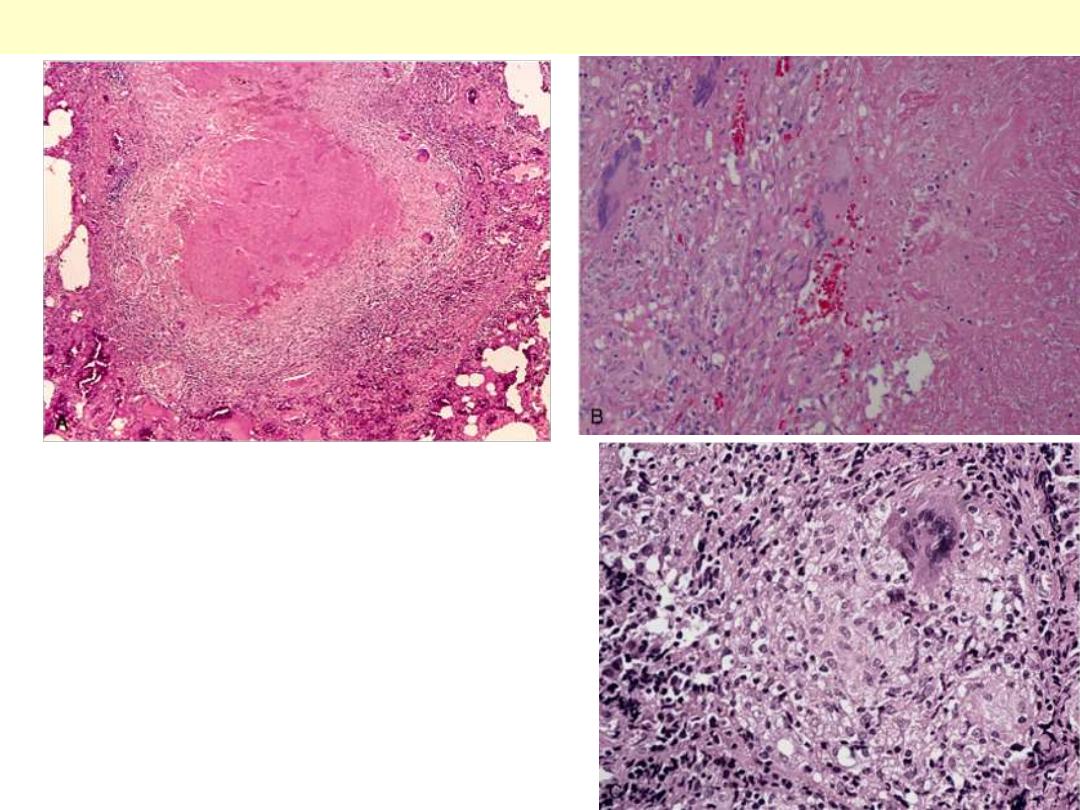
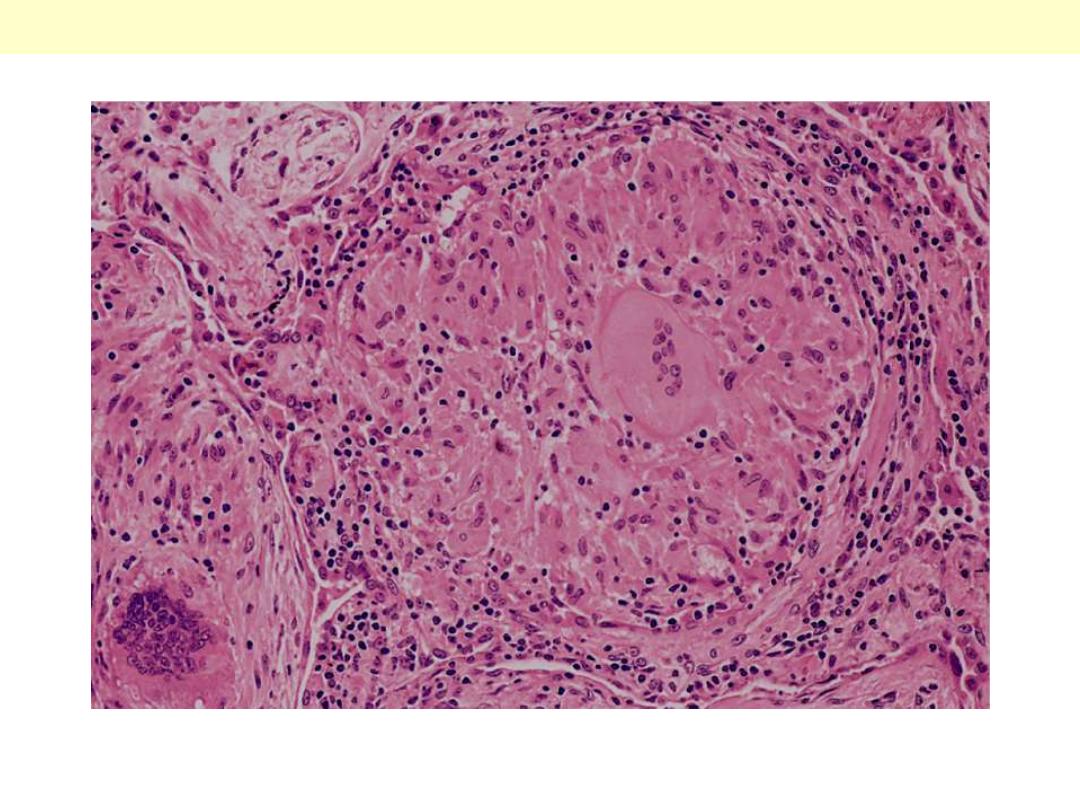
A characteristic tubercle at low magnification (A) and
in detail (B) illustrates central granular caseation
(right) that is surrounded by epithelioid and
multinucleated giant cells (left). This is the usual
response seen in individuals who have developed cell-
mediated immunity to the organism. C, Occasionally,
even in immunocompetent individuals, tubercular
granulomas may not show central caseation; hence,
irrespective of the presence or absence of caseous
necrosis, special stains for acid-fast organisms must
be performed when granulomas are present in
histologic sections.
The morphologic spectrum of tuberculosis
Multiple noncaseating epithelioid granuloma of TB
Note that the granulomas are enclosed within a fibroblastic rim with lymphocytes.
Microscopically, caseous necrosis is characterized by acellular pink areas of necrosis, as seen here at
the upper right, surrounded by a granulomatous inflammatory process.
Caseating epithelioid granuloma of TB
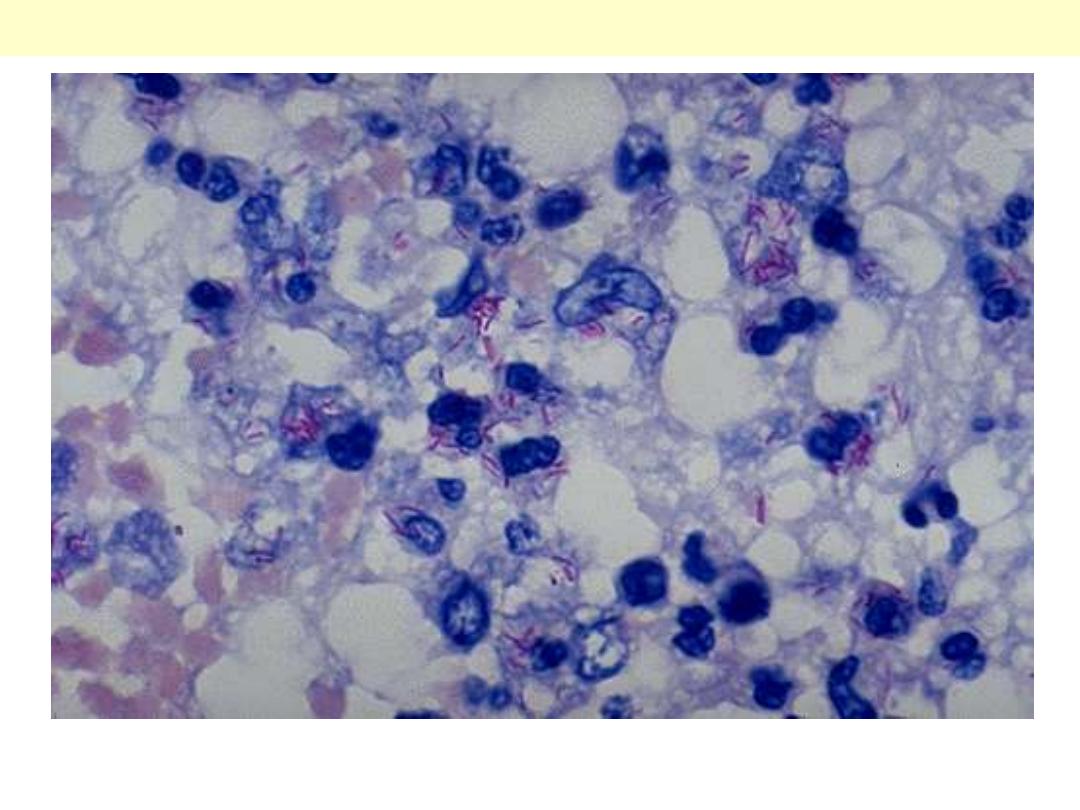
Mycobacterium tuberculosis: acid-fast stain
Note the red rods--hence the terminology acid fast bacilli (AFB)
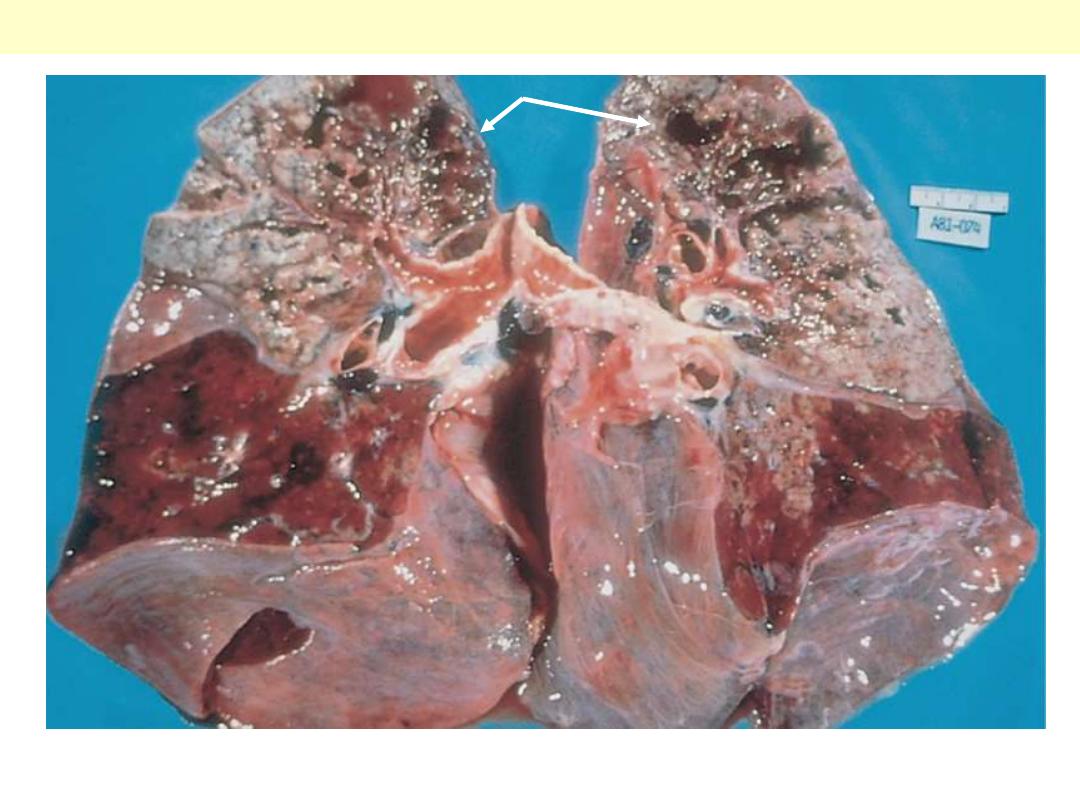
The upper parts of both lungs show multiple areas of softening and cavitation (arrows)
Secondary pulmonary tuberculosis
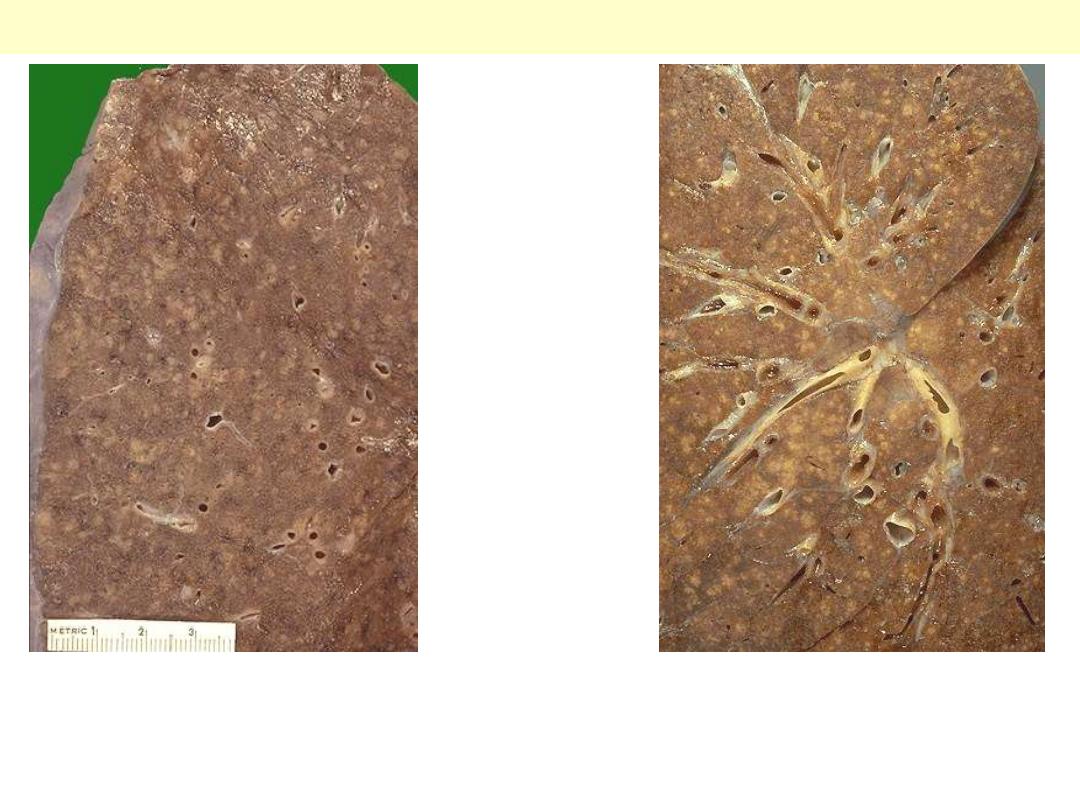
Lt. multitude of small (2 to 4 mm), yellow-white foci ; these scatter diffusely through the lungs. The
miliary pattern gets its name from the resemblance of the granulomas to millet seeds.
Rt. A zoom in appearance; the miliary pattern is seen throughout the lung.
Miliary pulmonary TB
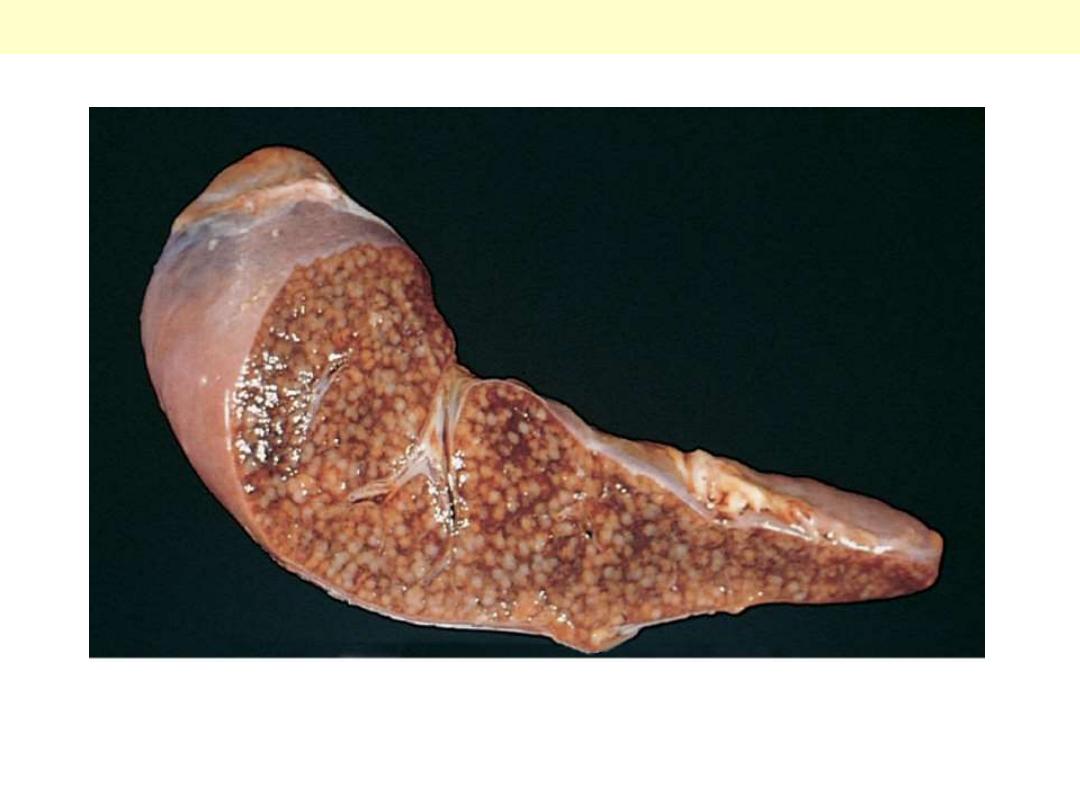
The cut surface shows numerous gray-white granulomas.
Miliary tuberculosis of the spleen

Pneumoconiosis

Coal Workers’ pneumoconiosis


Asbestosis
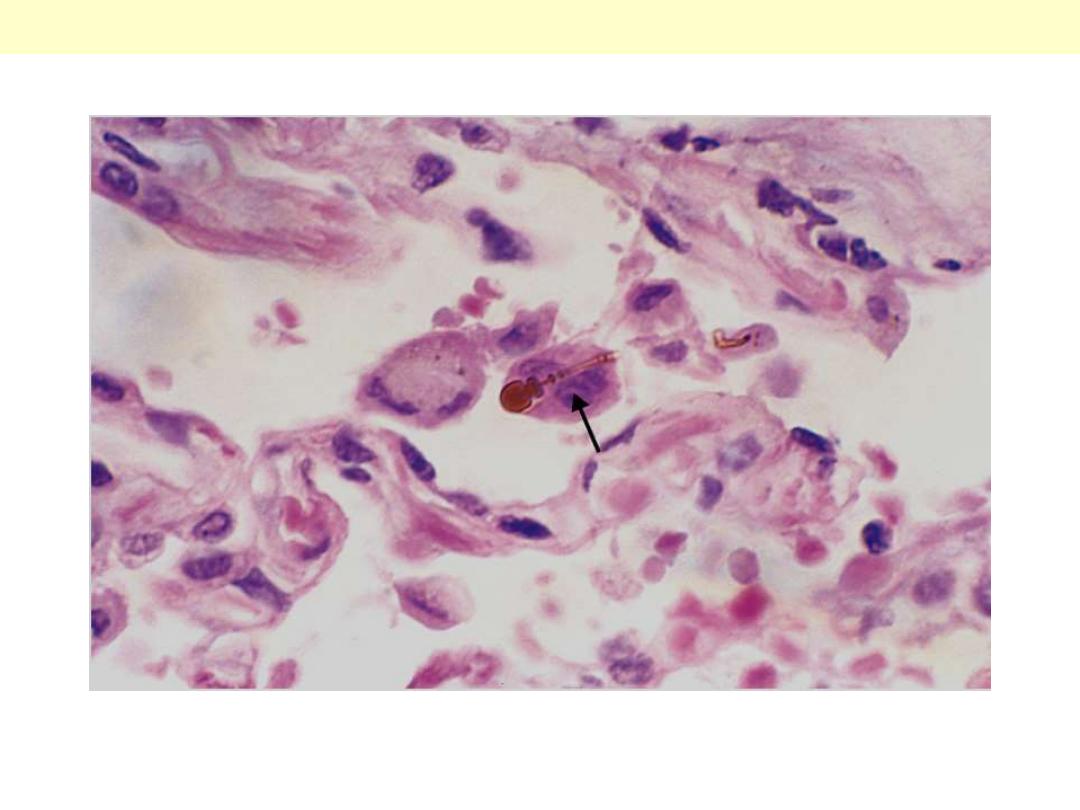
High-power detail of an asbestos body, revealing the typical beading and knobbed ends (arrow).
Asbestos body

Asbestos –related disease
Localized fibrous pleural plaque

Silicosis
M/69. Multiple silicotic nodules can be seen
under the pleura. This man had worked as a
miner for most of his life.
Silicosis lung
Several coalescent collagenous silicotic nodules.
Silicosis lung

Tumors
Lung - Tumors

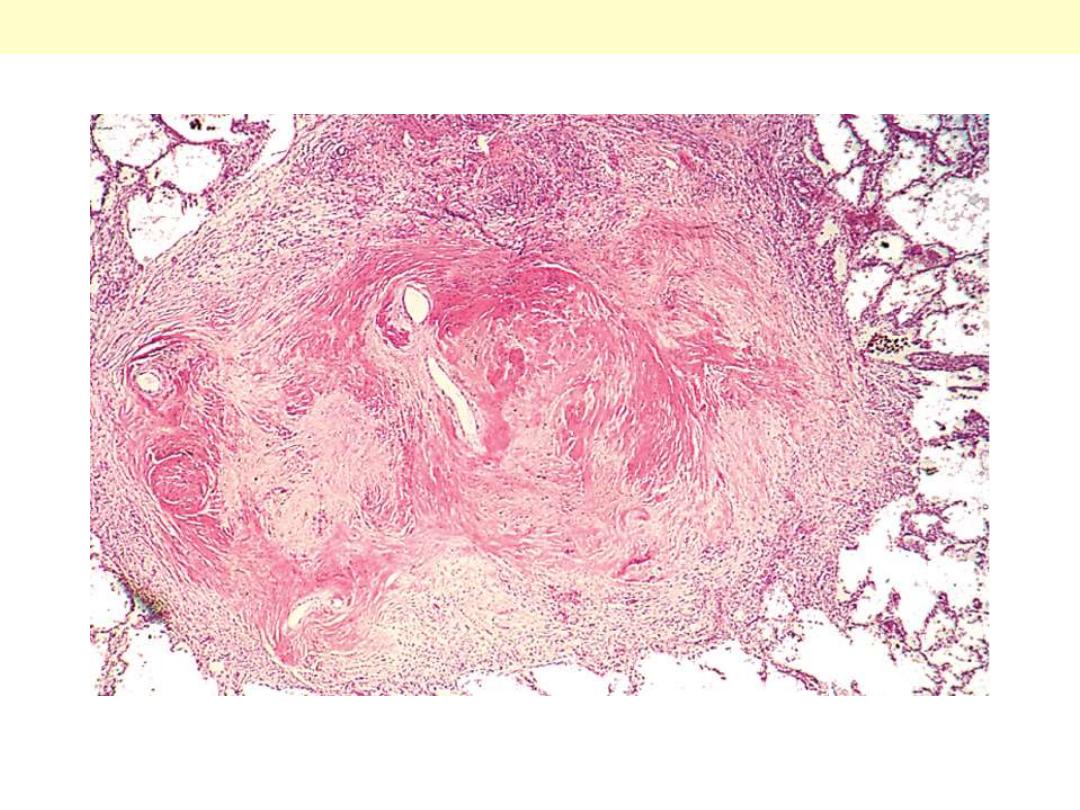
Here are two examples of a benign lung neoplasm known as a pulmonary hamartoma. These
uncommon lesions appear on chest radiograph as a "coin lesion" that has a differential diagnosis of
granuloma and localized malignant neoplasm. They are firm and discreet and often have calcifications
in them that also appear on radiography. Most are small (less than 2 cm).
Pulmonary hamartoma
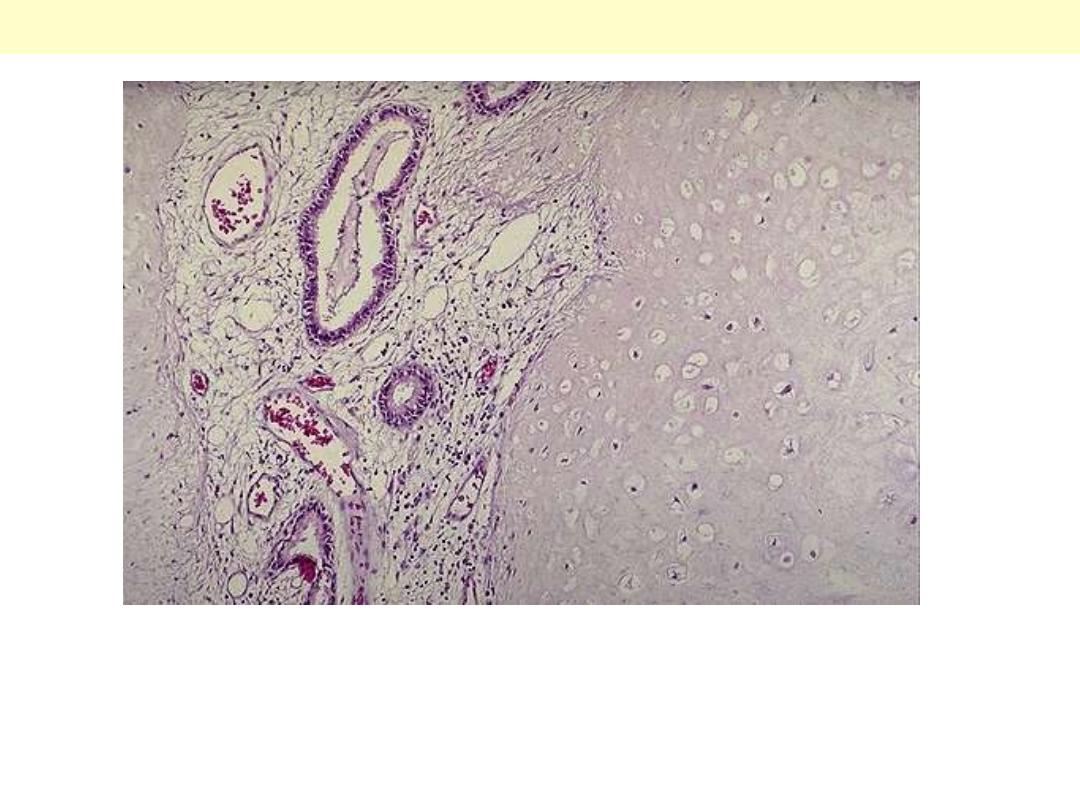
The pulmonary hamartoma is seen microscopically to be composed mostly of benign cartilage on the
right that is jumbled with a fibrovascular stroma and scattered bronchial glands on the left. A
hamartoma is a neoplasm in an organ that is composed of tissue elements normally found at that site,
but growing in a haphazard mass.
Pulmonary hamartoma
Squamous cell carcinoma: Note whitish endobronchial obstructive mass.
Early bronchial carcinoma
This is a fairly small carcinoma which has arisen in a bronchus blue (arrow), and then invaded into
surrounding lung tissue; tumor obstructing bronchus
Early bronchial carcinoma

Irregular pale growth which obstructs the lower lobe
bronchus producing collapse of the lung distal to the
growth and bronchiectasis.
Bronchiectasis complicating bronchial carcinoma

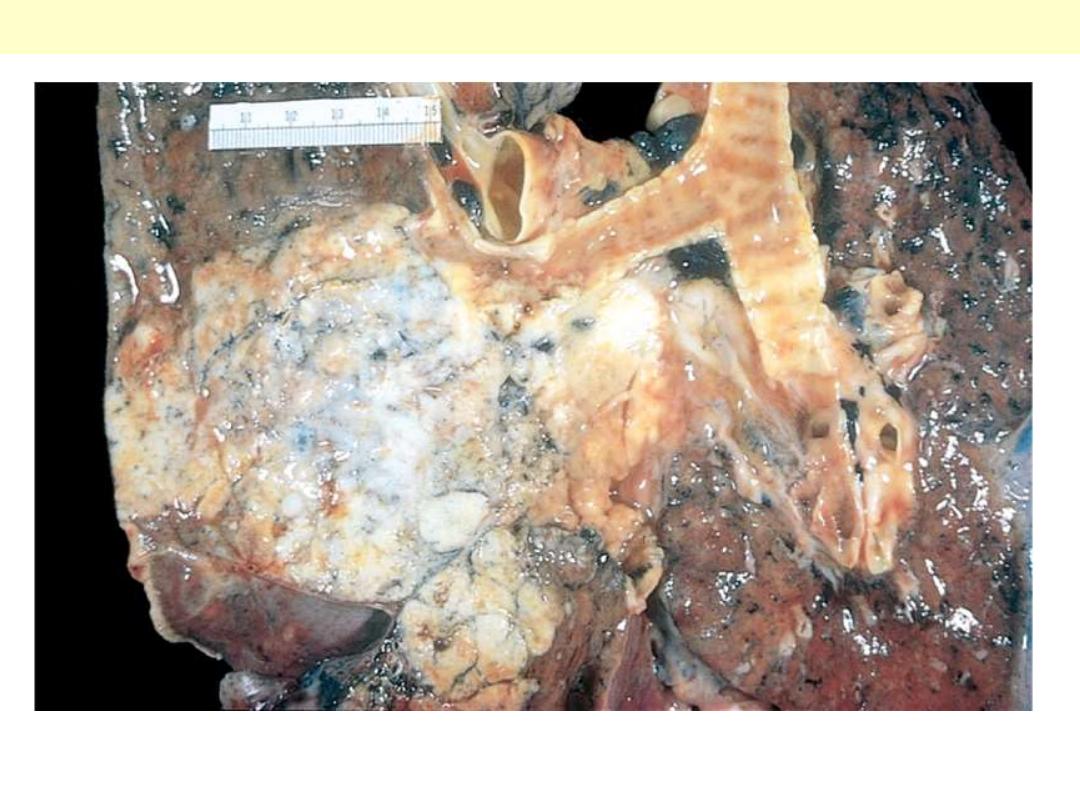
Centrally located carcinoma
This pale white tumor is obstructing the right main
bronchus. a squamous cell carcinoma of the lung that is
arising centrally in the lung (as most squamous cell
carcinomas do). Microscopy shows squamous cell
carcinoma.
Peripheral carcinoma
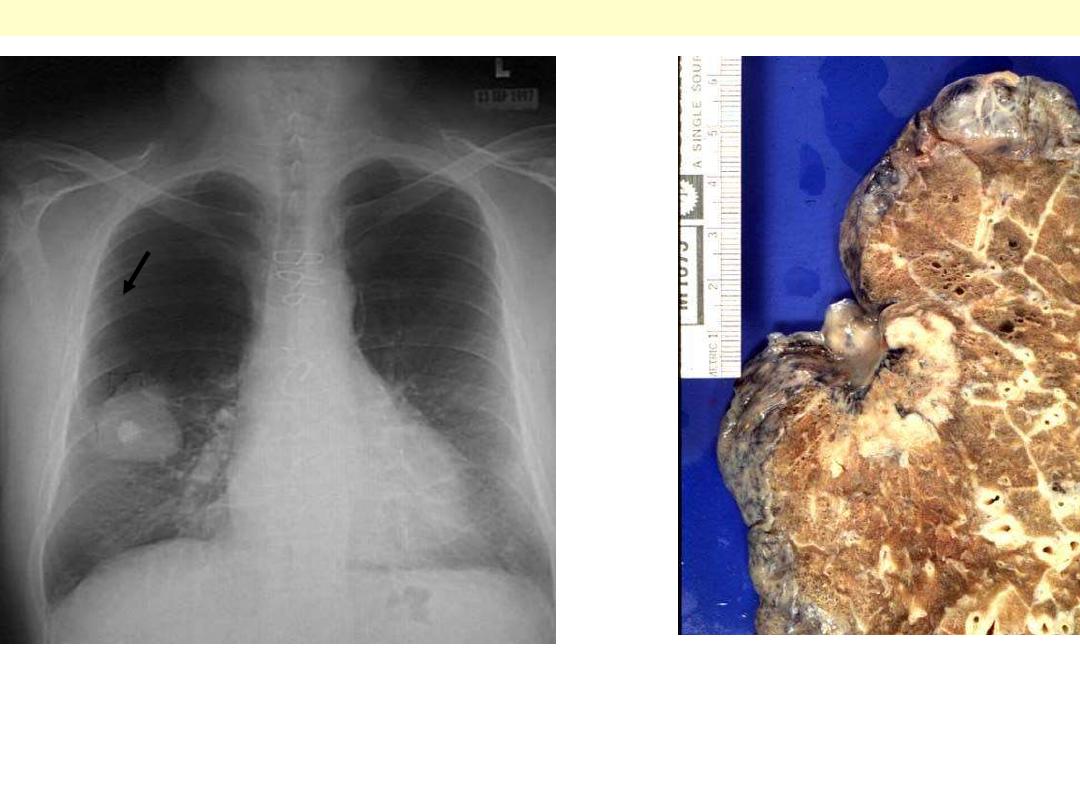
Rt. This chest radiograph demonstrates a large 5 cm diameter adenocarcinoma of the right lower lobe. The
bright opacity in the middle of the mass is a calcified granuloma.
Lt. Adenocarcinoma: Peripheral mass located immediately under visceral pleura, with pleural retraction.
Adenocarcinoma. The tumor is peripherally located and
has extended to the pleura.
Peripheral carcinoma
Squamous cell carcinoma G
This is a large squamous cell carcinoma in
which a portion of the tumor demonstrates
central cavitation (arrow), probably because
the tumor outgrew its blood supply.
The tumor usually begin as central (hilar) masses and grow contiguously into the peripheral
parenchyma and adjacent pleura
Squamous cell carcinomas
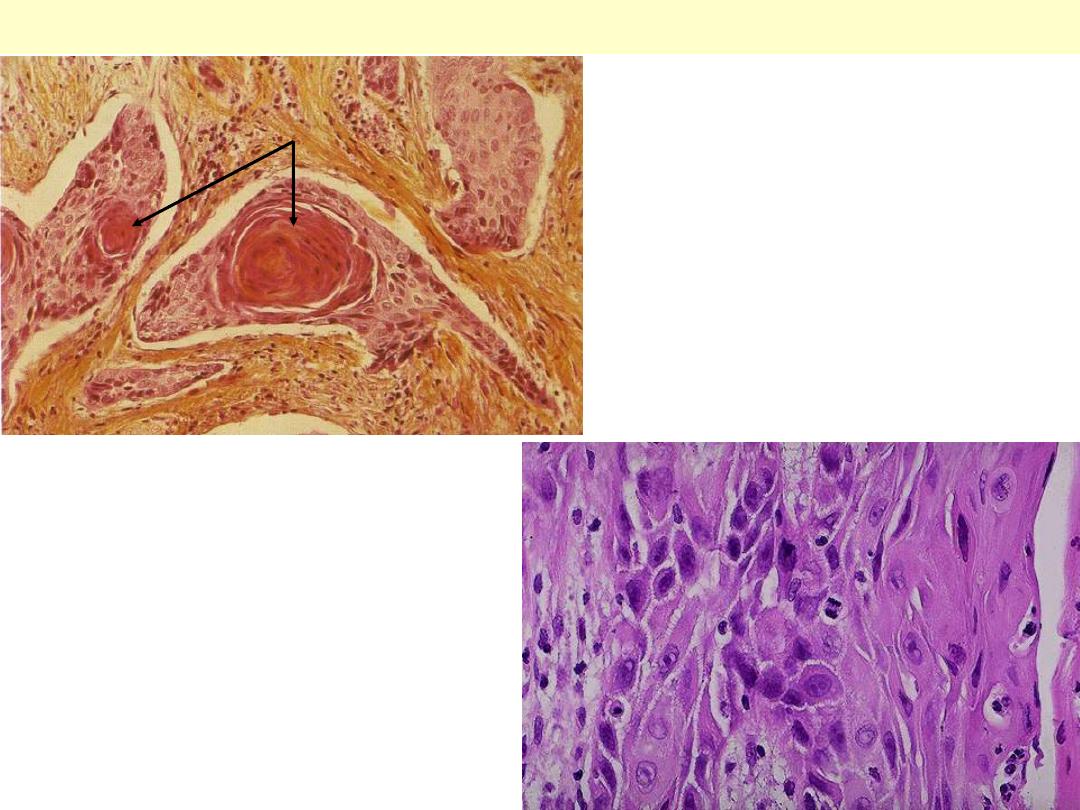
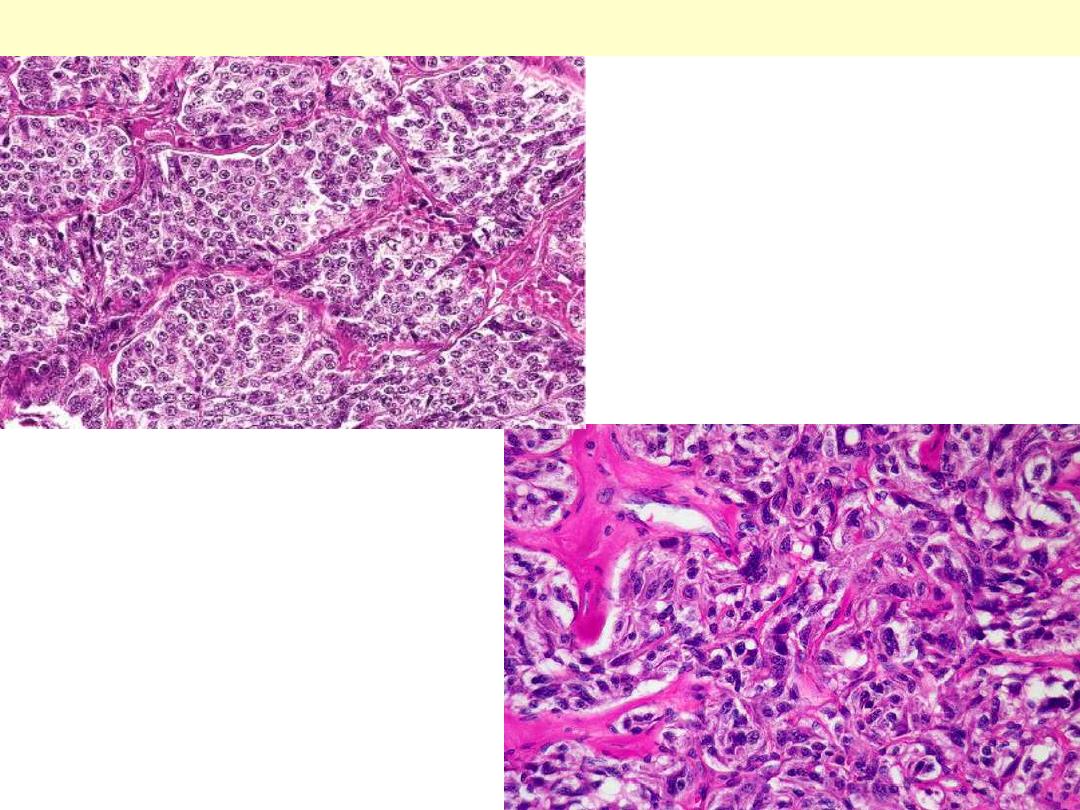
Well differentiated squamous cell ca WD
Above: nests of squamous cells with keratin
production (arrow).
Below: the pink cytoplasm with distinct cell
borders and intercellular bridges
characteristic for a squamous cell
carcinoma are seen here at high
magnification. Such features are seen in
well-differentiated tumors (those that more
closely mimic the cell of origin).
Malignant epithelial cells forming glandular
structures with mucin secretion.
Pulmonary adenocarcinoma
papillary and micropapillary structures
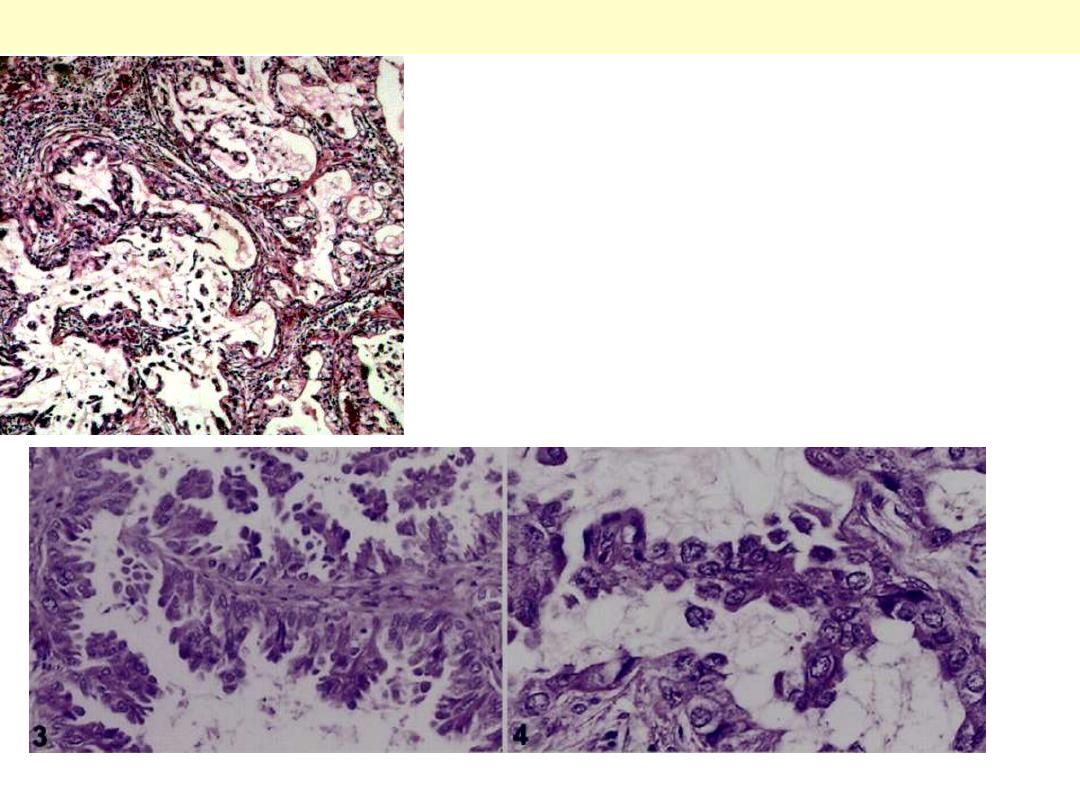
Bronchioloalveolar ca G
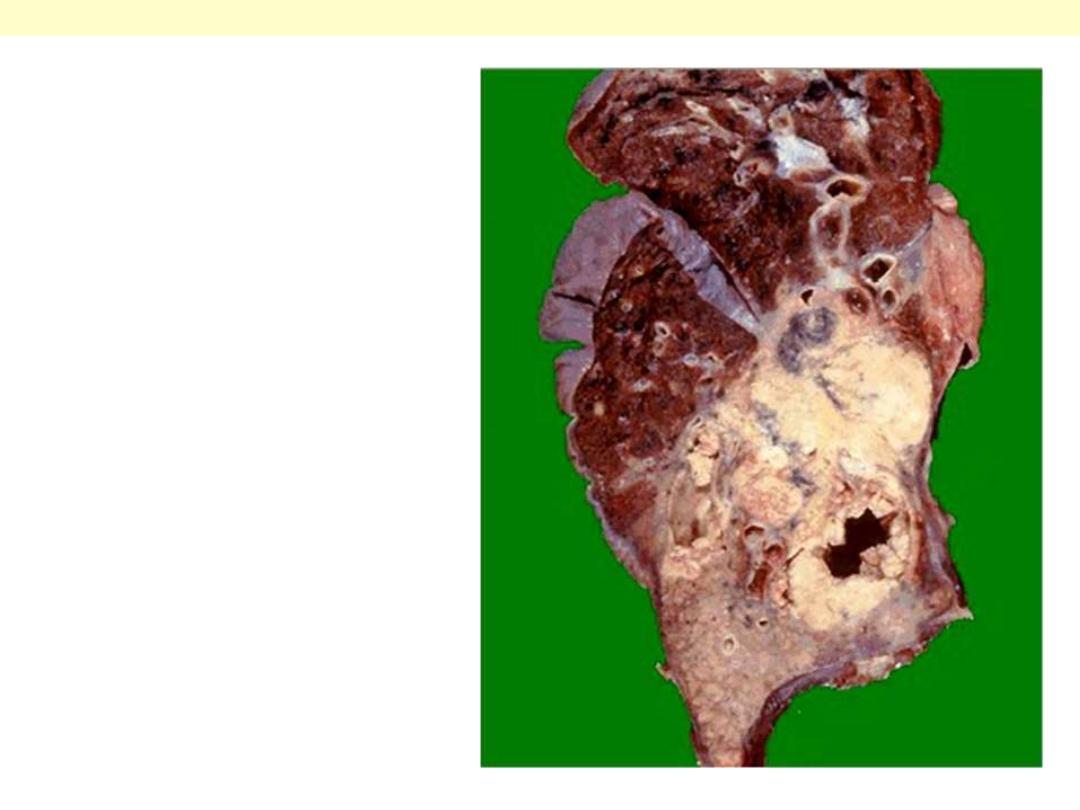
Greyish-white tumor involves 2/3 of left upper
lobe and 1/3 of the lower lobe. The color and
distribution suggest pneumonic consolidation.
Secondary tumors can peoduce the same
appearance.
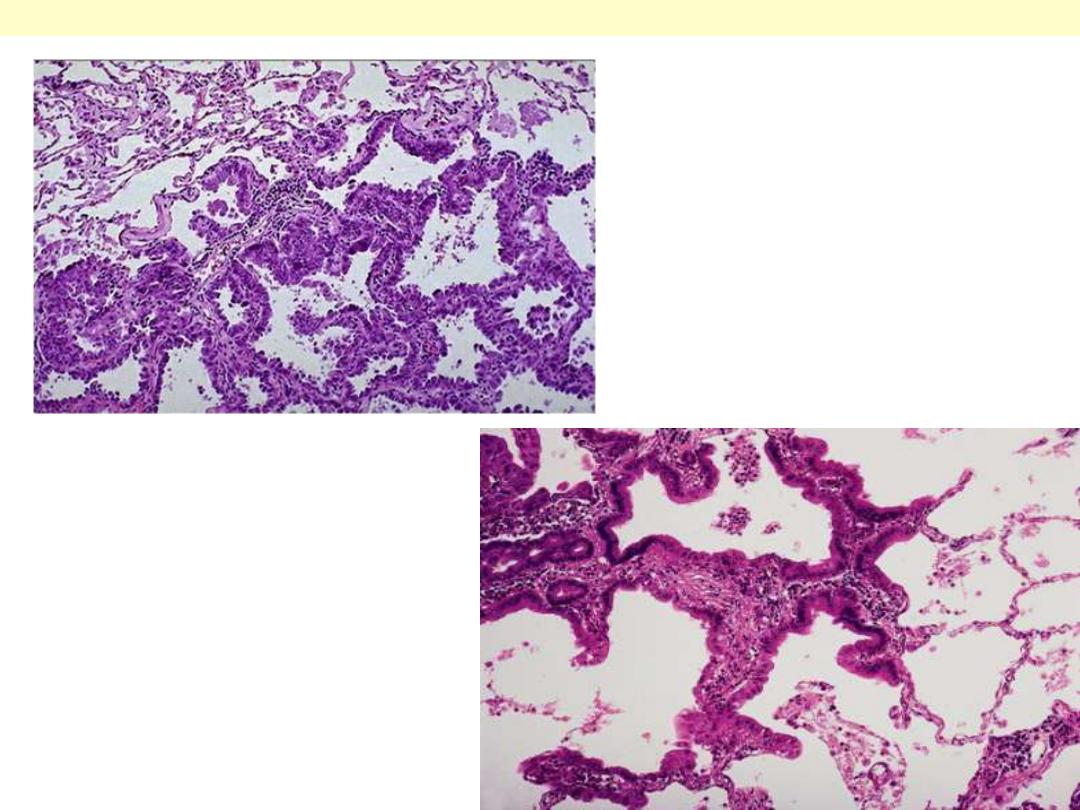
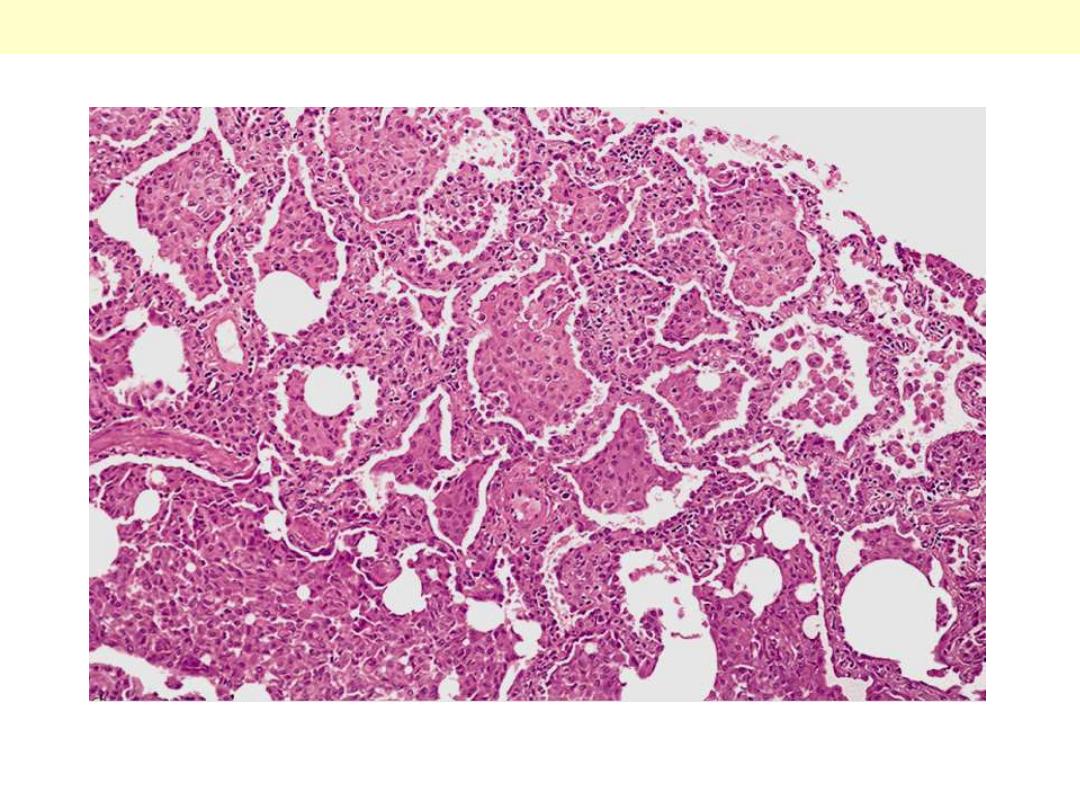
Bronchioloalveolar ca mic
The tumor is composed of columnar cells
that proliferate along the framework of
alveolar septae. The cells are well-
differentiated.
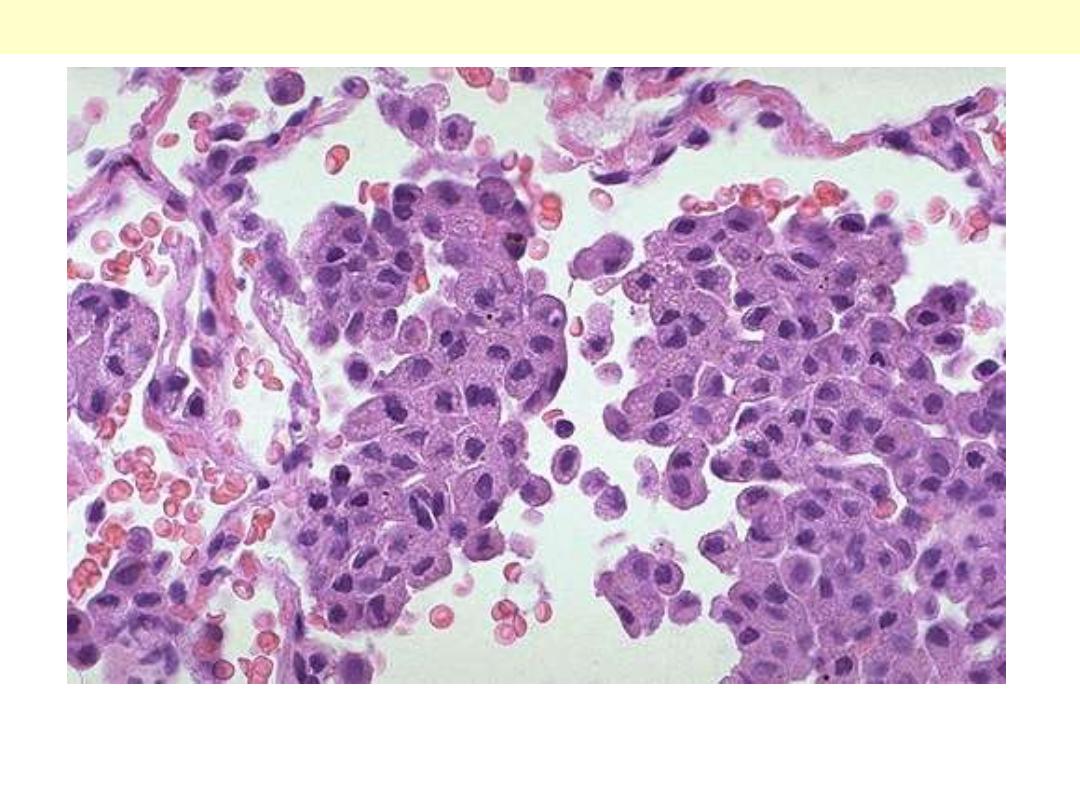
Large cell undifferentiated ca
Undifferentiated large cell carcinoma. Tumor is formed by large cells growing in solid nests without
evidence of glandular or squamous differentiation.
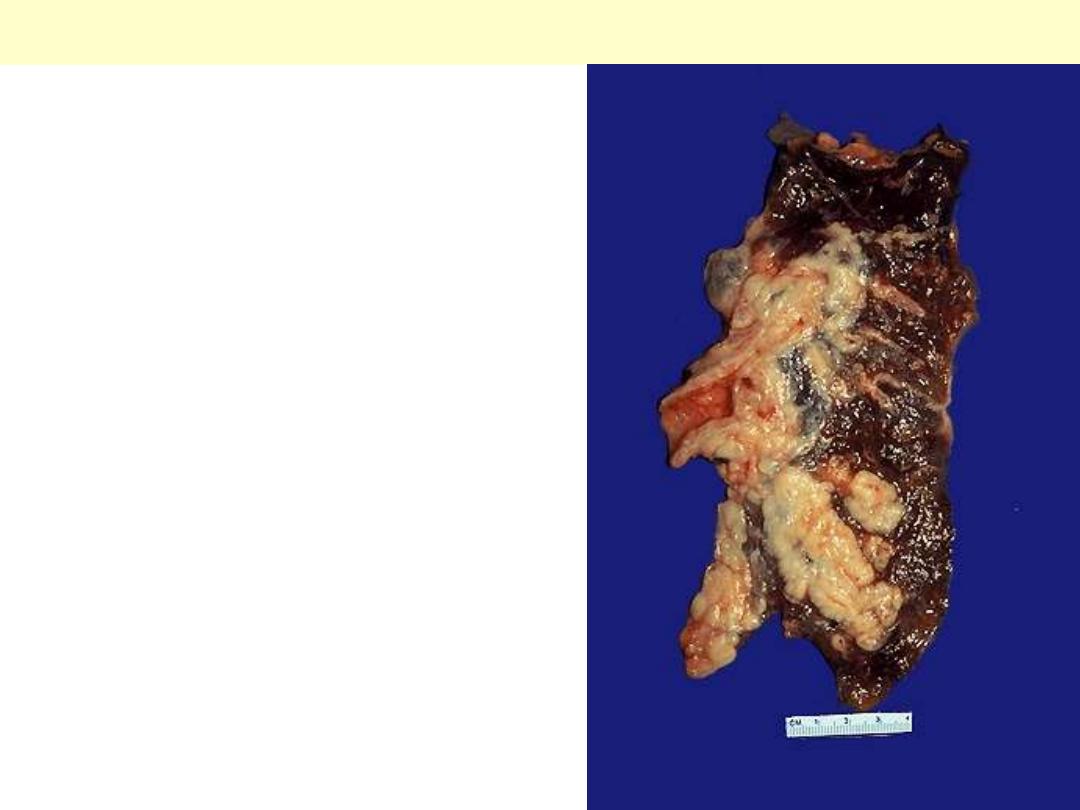
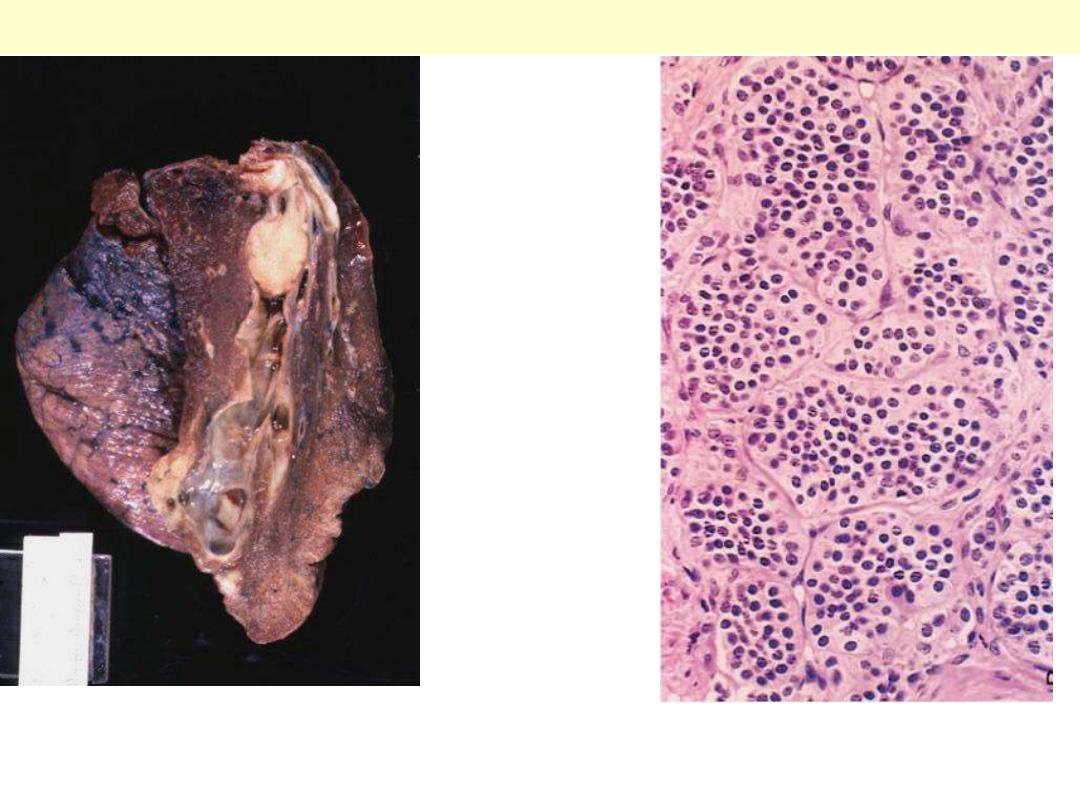
Small cell carcinoma lung
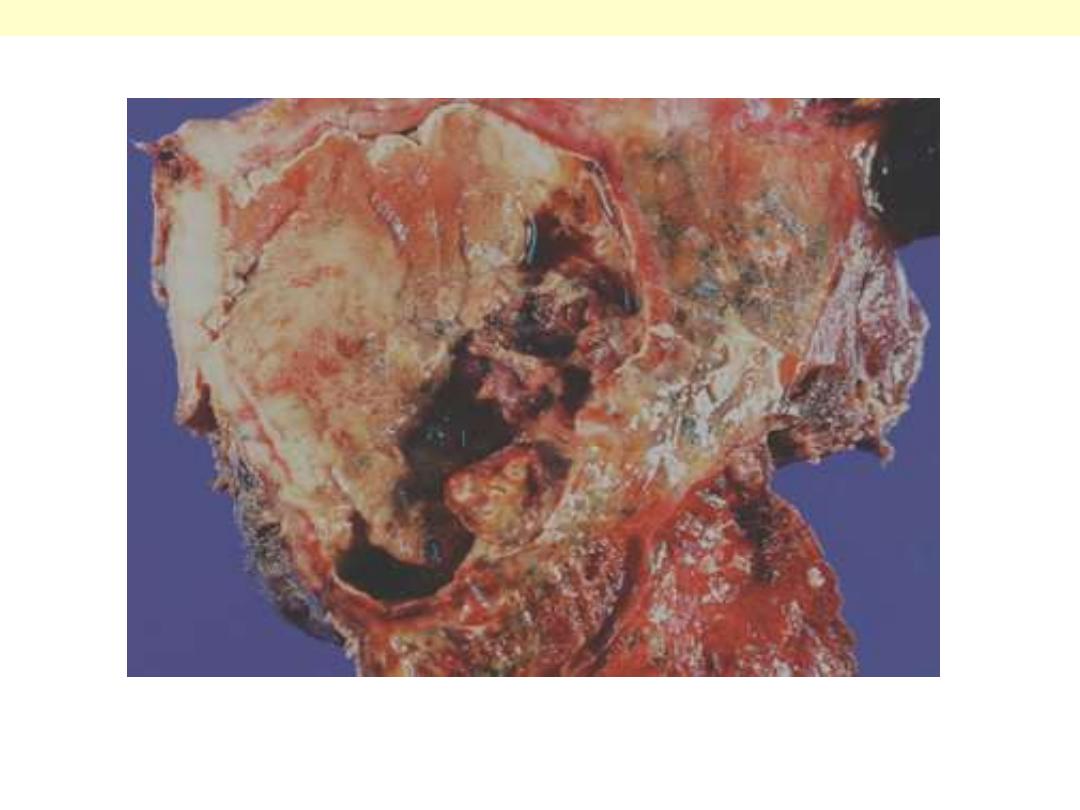
Arising centrally in this lung and spreading
extensively is a small cell anaplastic (oat cell)
carcinoma. The cut surface of this tumor has a
soft, lobulated, white to tan appearance. The
tumor seen here has caused obstruction of the
main bronchus to left lung so that the distal lung
is collapsed. Oat cell carcinomas are very
aggressive and often metastasize widely before
the primary tumor mass in the lung reaches a
large size.
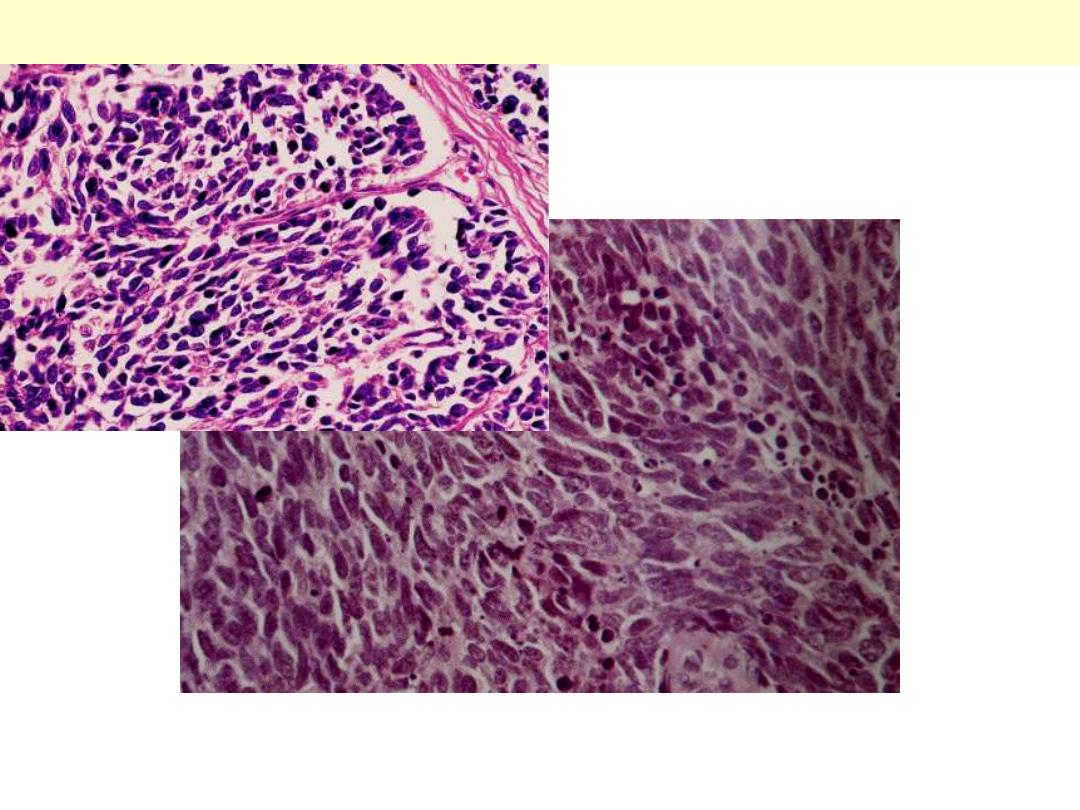
Small cell carcinoma lung
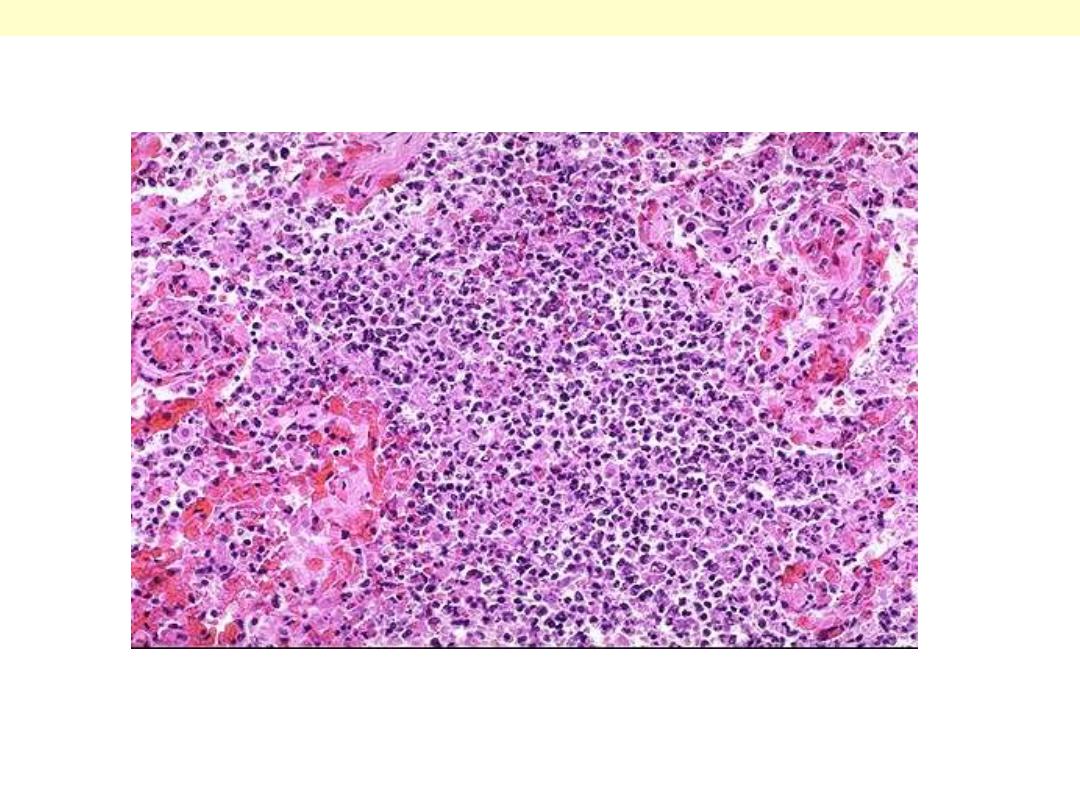
The tumor is composed of small cells with darkly
staining oval to spindle nuclei and extremely scanty
cytoplasm.
A, Bronchial Carcinoid Tumor: Yellow intrabronchial mass (lower) has resulted in obstructive
bronchiectasis
B, Histologic appearance demonstrating trabecular arrangement of small, rounded, uniform cells
.
Bronchial carcinoid
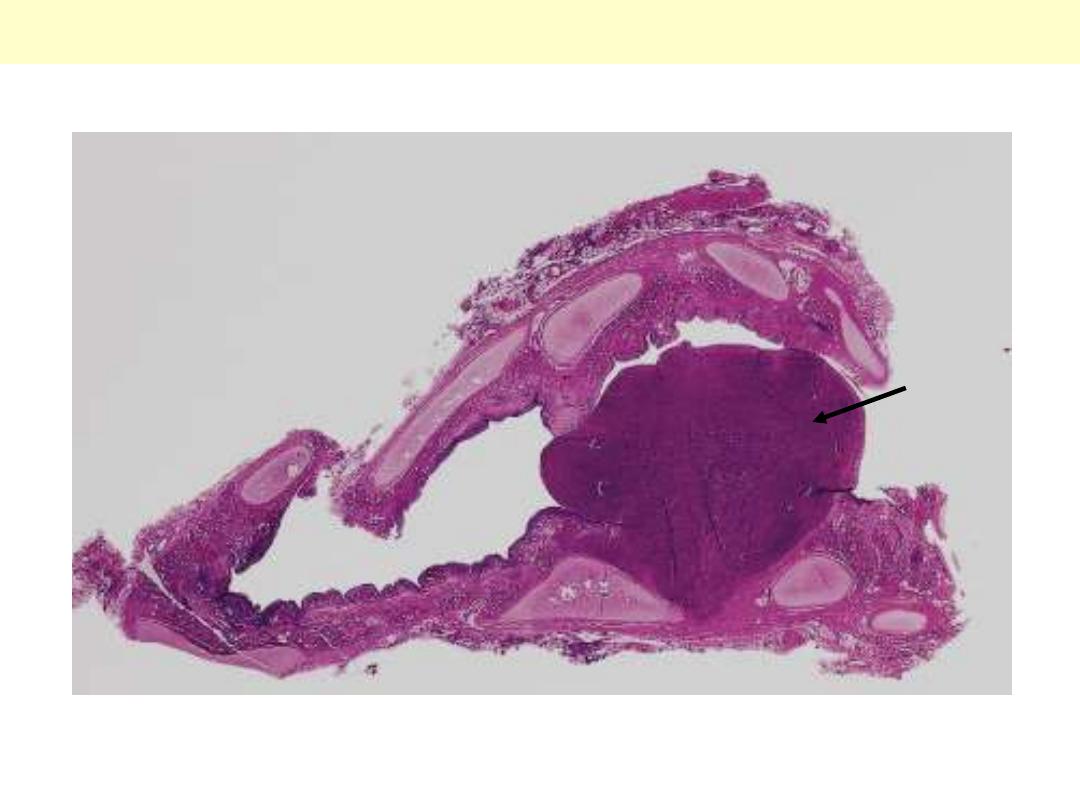
Carcinoid Central
Whole mount of carcinoid tumor showing polypoid endobronchial growth.
Carcinoid lung
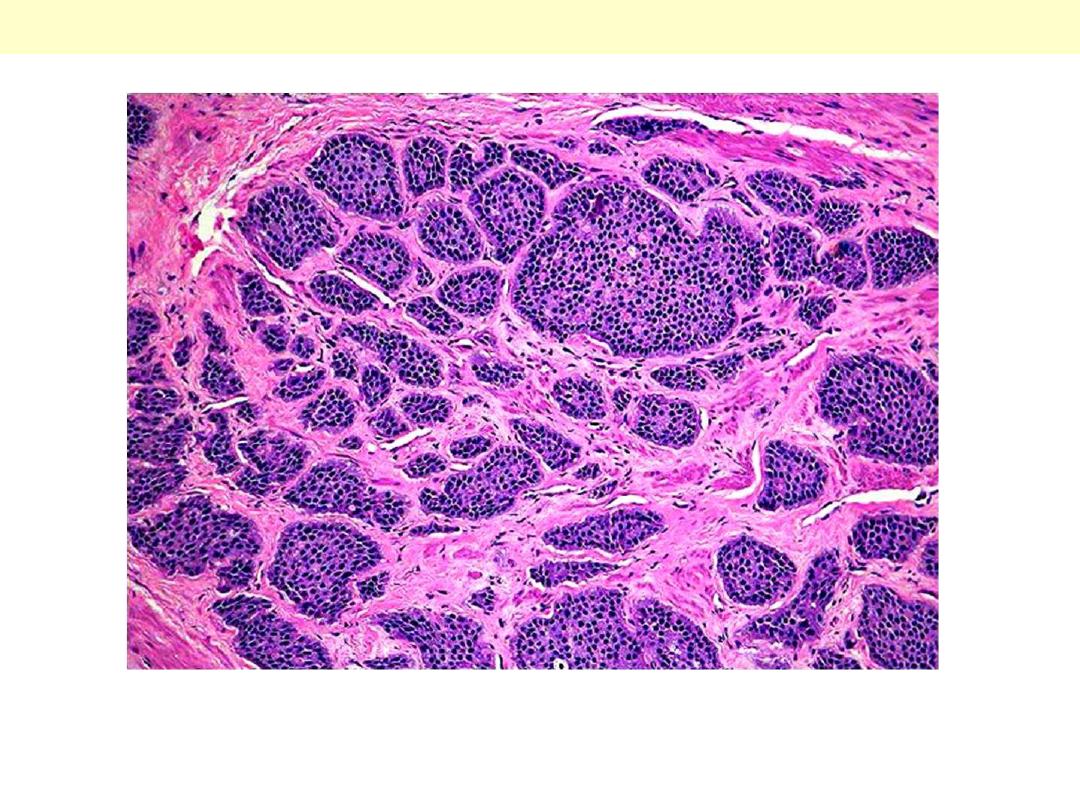
The tumor is composed of nests of uniform cells that have regular round nuclei & absent or rare
mitoses
Atypical Carcinoid
There is typical nesting of marked
pleomorphic cells. mitotic activity, and
necrosis are also present elsewhere.

Pleura – Malignant
mesothelioma
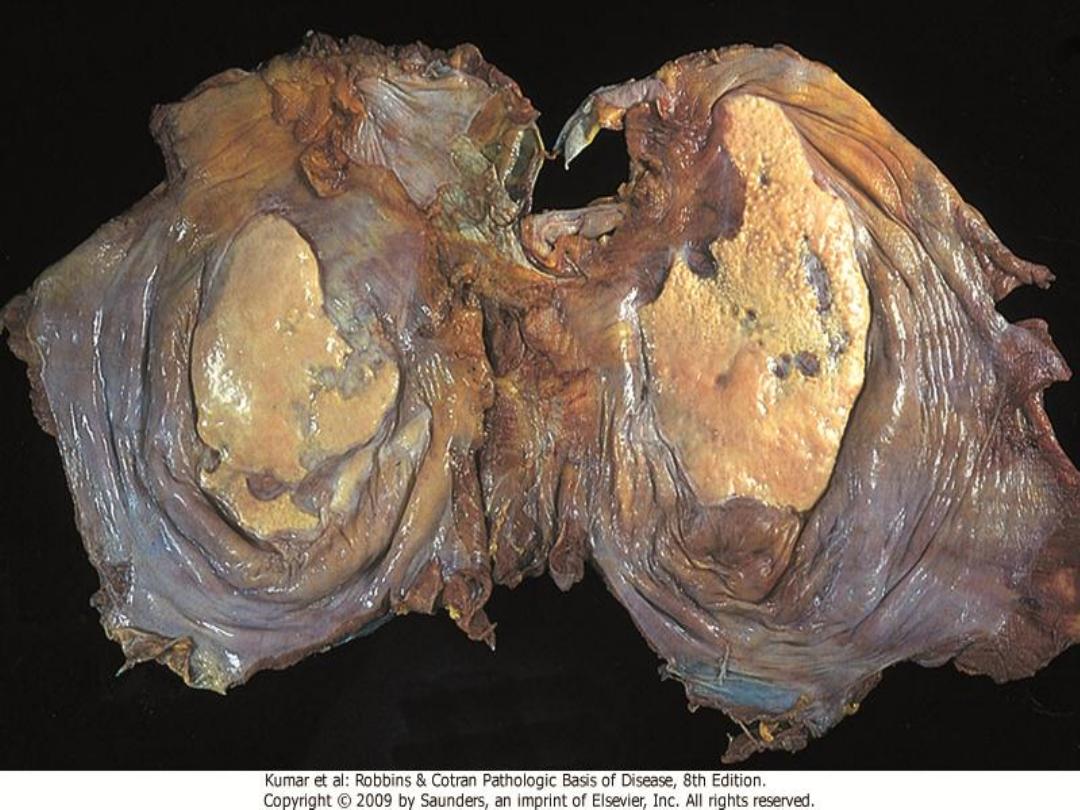
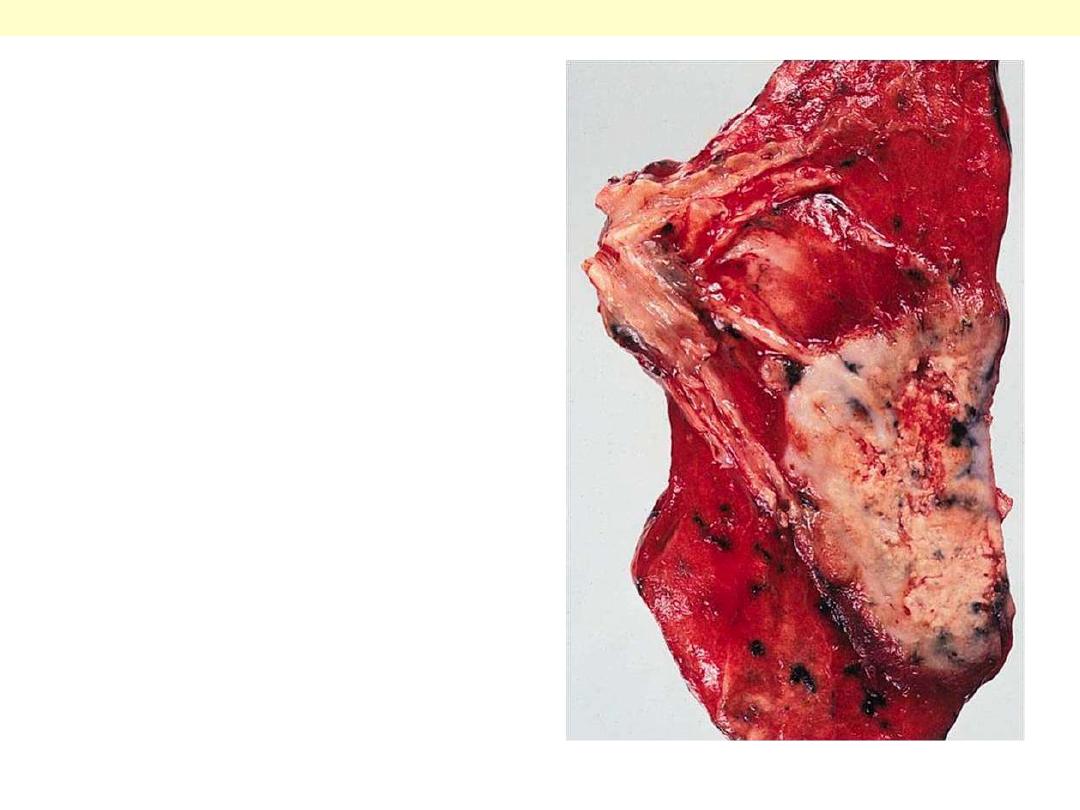
M/67. This vertical slice of the right lung shows the
manner in which a pleural mesothelioma causes
thickening of the pleura and encases the whole
lung and mediastinum.
Malignant mesothelioma pleura
Malignant mesothelioma
Thick, firm, white, pleural tumor that ensheaths the
lung. Nodular invasion into the lung parenchyma is also
evident.
Note the thick, firm, white, pleural tumor that ensheaths this bisected lung.
Malignant mesothelioma
Malignant mesothelioma
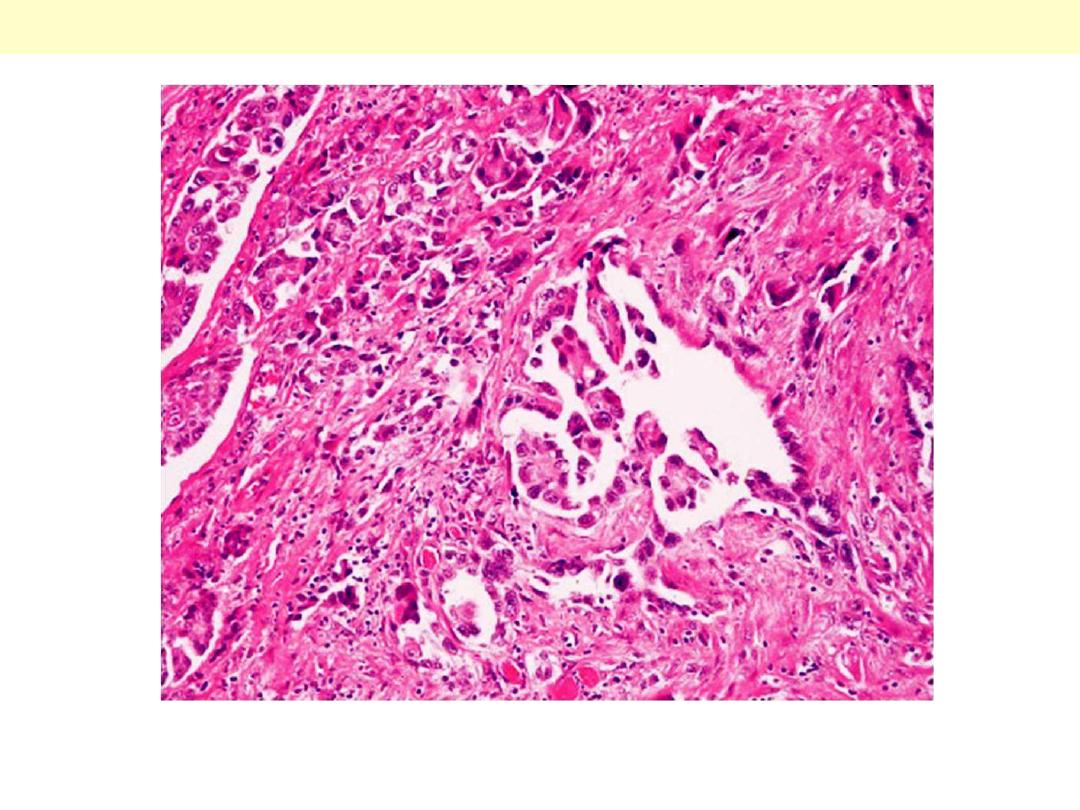
Malignant mesothelioma with papillary formations and desmoplastic stromal reaction.

ARDS
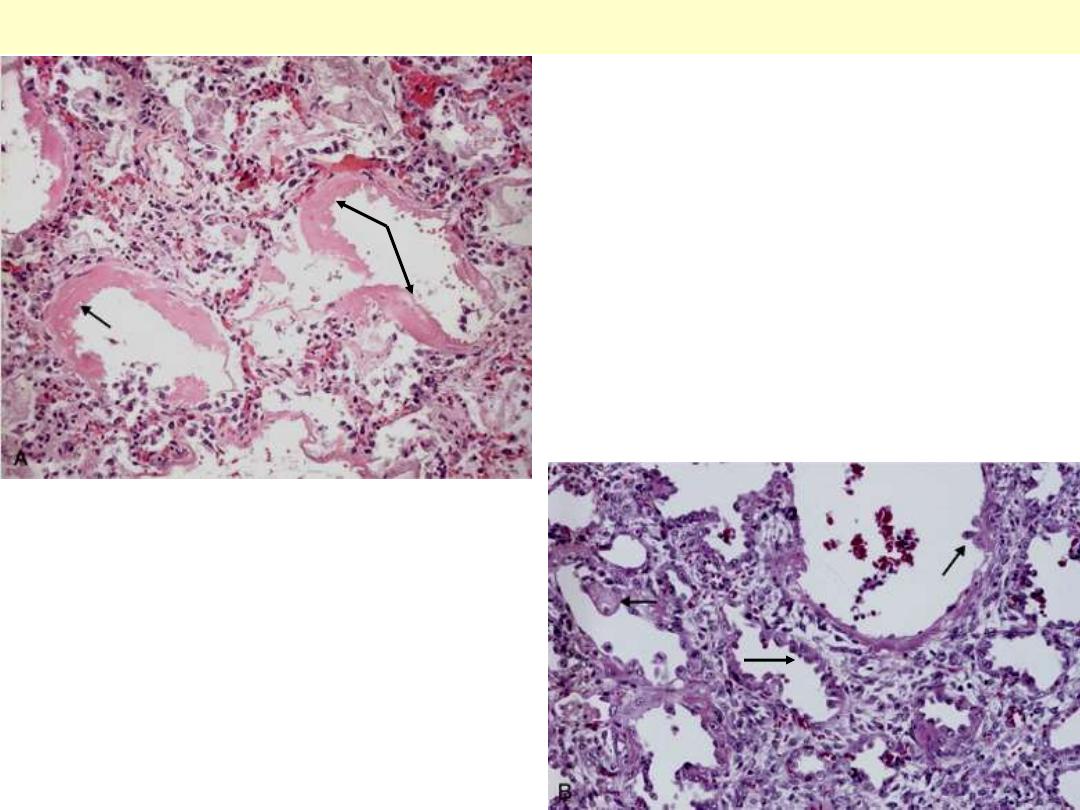
B, In the healing stage there is resorption of
hyaline membranes with thickened alveolar septa
containing inflammatory cells, fibroblasts, and
collagen. Numerous regenerating type II
pneumocytes are seen at this stage (arrows).
ARDS
A, Diffuse alveolar damage in ARDS. Some
alveoli are collapsed; others are distended. Many
are lined by bright pink hyaline membranes
(arrows).

Atelectasis
d
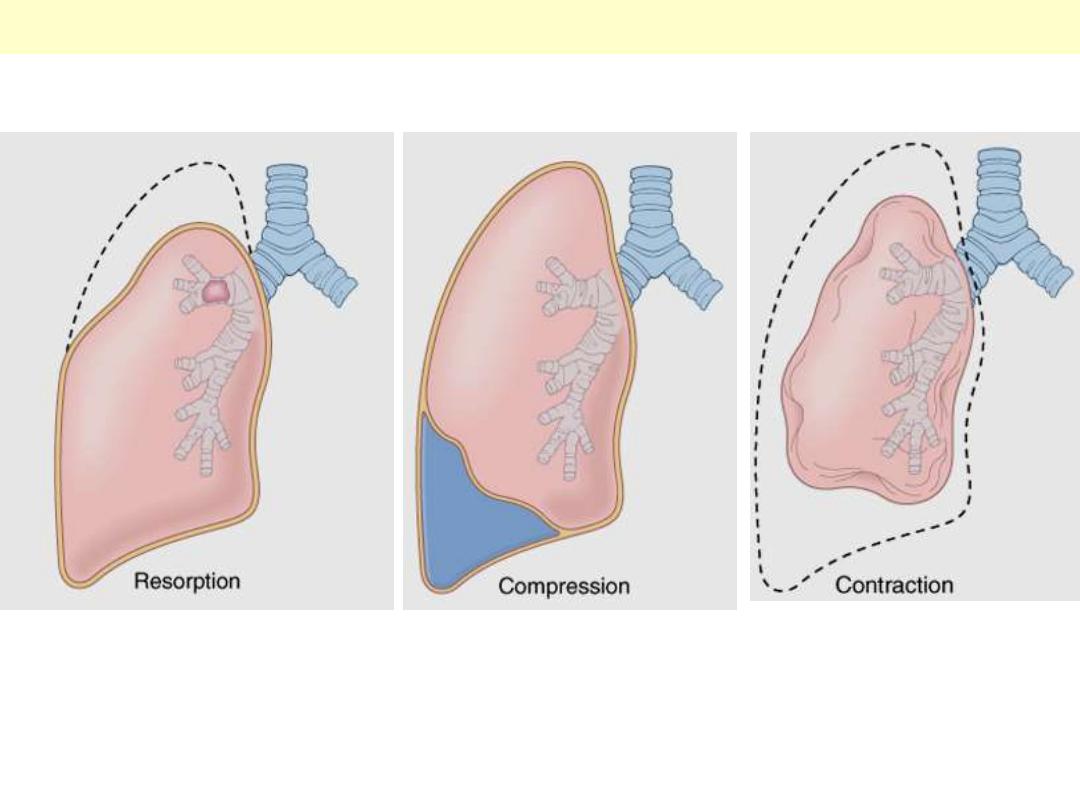
Atelectasis: pathogenetic types

Bronchiectesis
Bronchiectasis
Extensive bilateral bronchiectasis; the massively dilated bronchi extend almost to the pleura.
Widespread bronchiectasis is typical for patients with cystic fibrosis who have recurrent infections and
obstruction of airways by mucus throughout the lungs.
Cross-section of lung demonstrating dilated bronchi extending almost to the pleura.
Bronchiectasis

A closer view demonstrates the focal area of dilated bronchi with bronchiectasis. Bronchiectasis tends to
be localized with disease processes such as neoplasms and aspirated foreign bodies that block a
portion of the airways. Note that the dilated bronchi can be traced down to the pleura.
Segmental Bronchiectasis
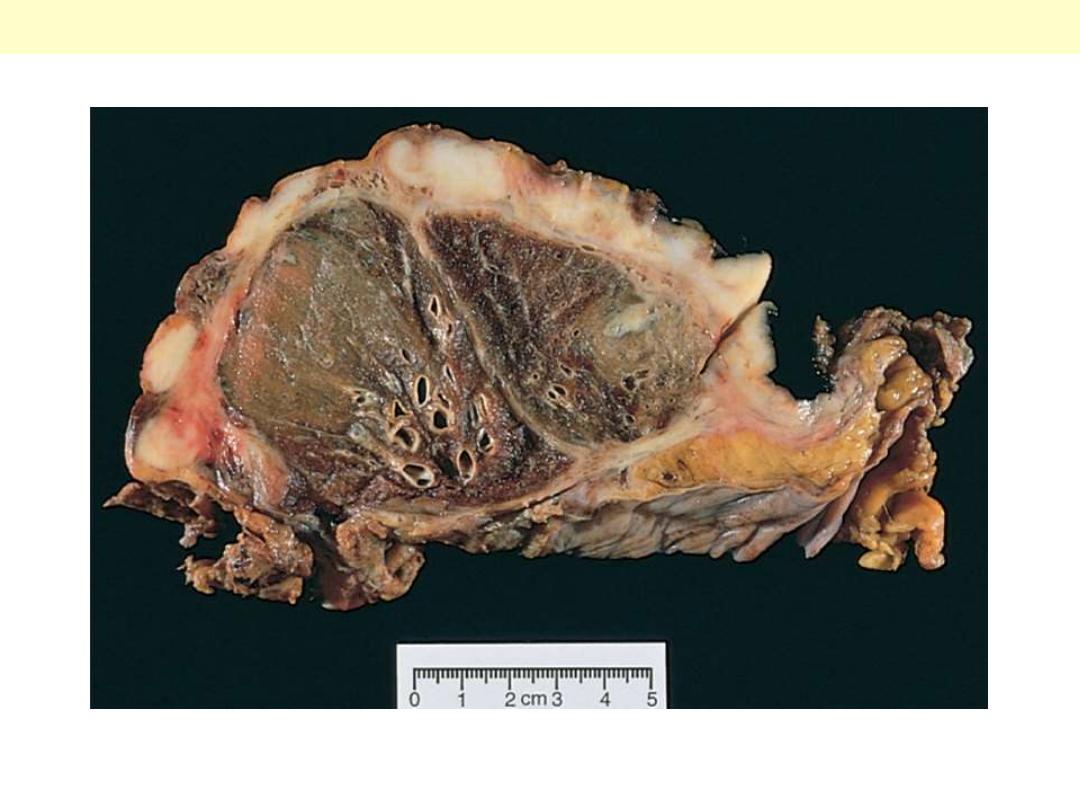
Segmental distribution of bronchiectasis. The bronchi are
dilated into cavities. The dilated bronchi are filled with
gelatinous inspissated mucus.
Segmental Bronchiectasis
The mid lower portion of this photomicrograph demonstrates a dilated bronchus in which the mucosa
and wall is not clearly seen because of the necrotizing inflammation with destruction.
Bronchiectasis

Desquamative interstitial
pneumonia
Medium-power detail of lung to demonstrate the accumulation of large numbers of mononuclear cells
within the alveolar spaces with only mild fibrous thickening of the alveolar walls.
Desquamative interstitial pneumonia (DIP)
Desquamative interstitial pneumonia (DIP)
Accumulation of large numbers of mononuclear cells within the alveolar spaces
with only mild fibrous thickening of the alveolar walls.

Diffuse interstitial lung
disaese
The fibrosis, which varies in intensity, is more pronounced in the subpleural region (arrow)
Idiopathic pulmonary fibrosis
HONEYCOMB LUNG
The lung has a honeycomb appearance grossly. There is prominent interstitial fibrosis. Etiologies
include DIP, UIP, interstitial pneumonitis associated with collagen vascular diseases, asbestosis,
berylliosis, sarcoidosis, LIP, DAD, recurrent aspiration, allergic alveolitis, and idiopathic.

Pulmonary hypertension
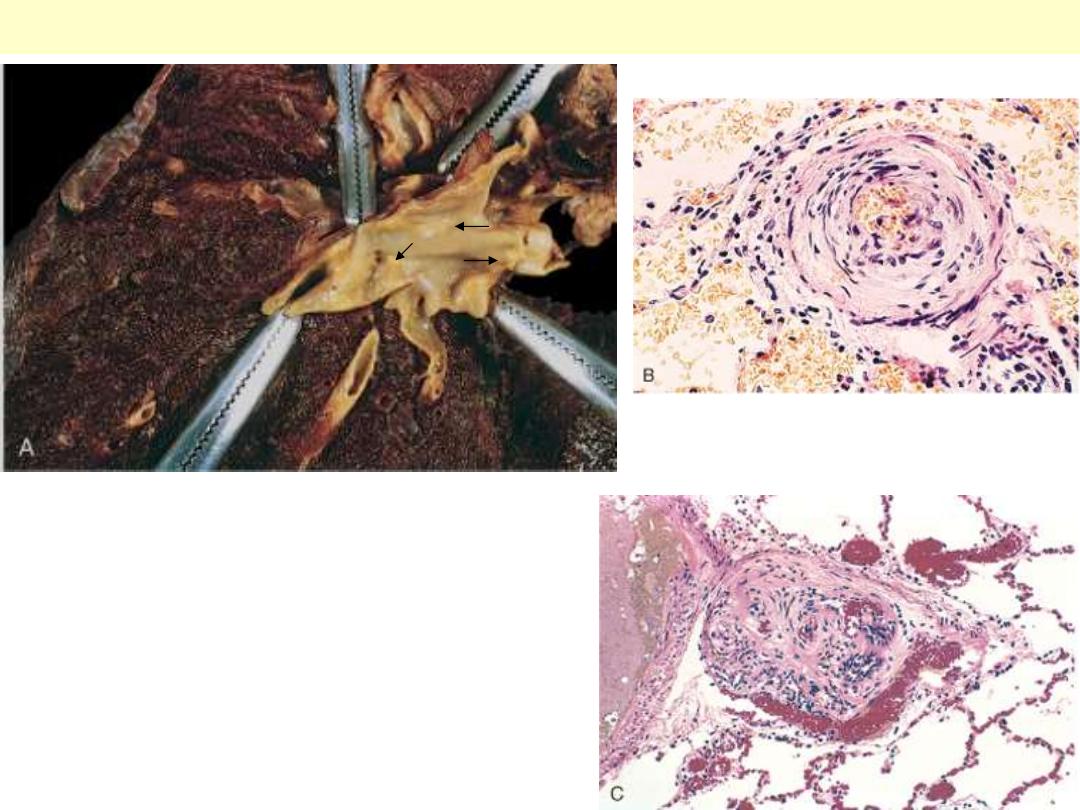
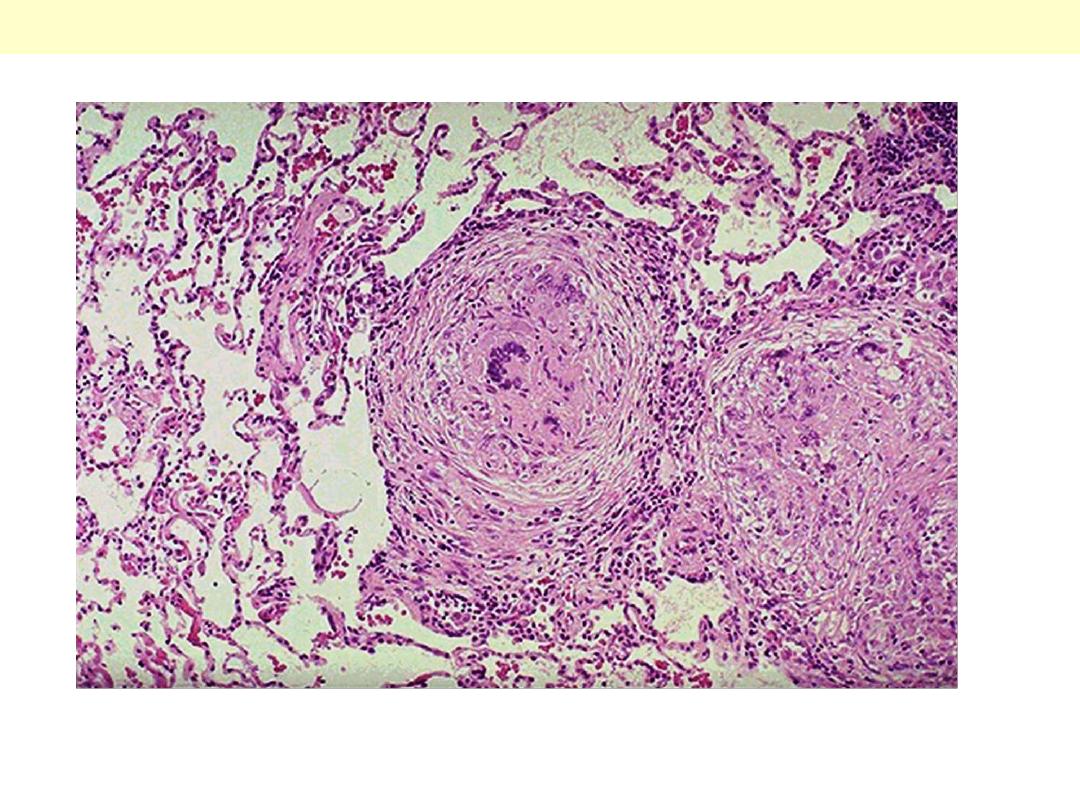
Vascular changes in pulmonary hypertension. A, Gross
photograph of atheroma formation, a finding usually
limited to large vessels. B, Marked medial hypertrophy.
C, Plexogenic lesion characteristic of advanced
pulmonary hypertension seen in small arteries.
Pulmonary hypertension

Sarcoidosis
Sarcoidosis lung
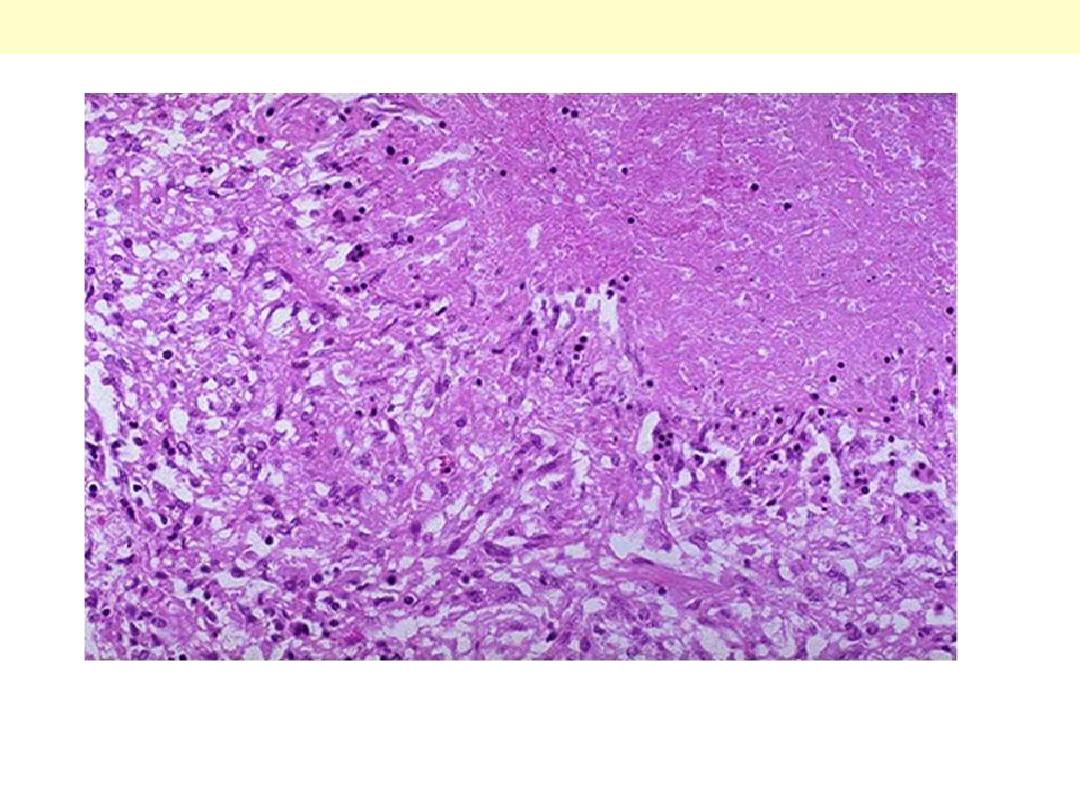
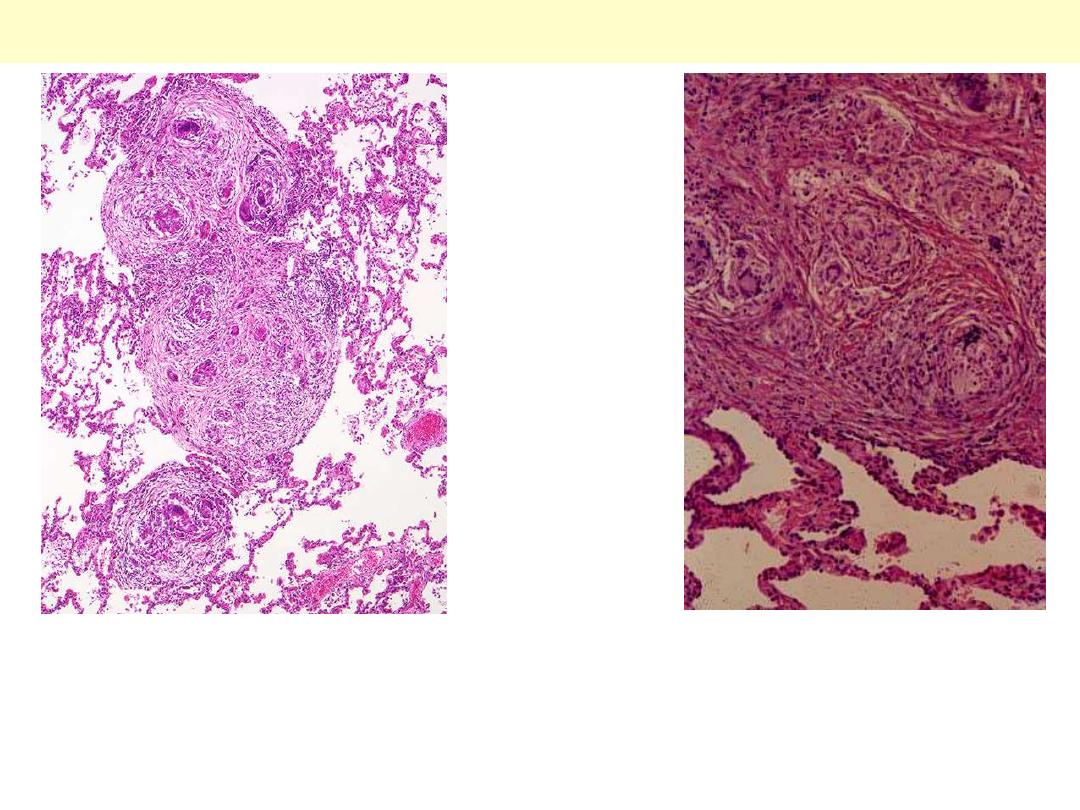
Rt. Low power: non caseating granulomas are present in the lung parenchyma. The inciting agent for
this granulomatous disease is unknown - speculation ranges from an unidentified microorganism to
tree pollen!. Sarcoidosis typically presents with non-caseating granulomas.
Lt. Medium power: there is interstitial non-caseating granulomatous inflammation. Giant cells and
histiocytes form nodular aggregates without necrosis
High power: characteristic sarcoid noncaseating granulomas in lung with many giant cells.
Sarcoidosis
Each of the two multinucleated giant cells shown
here has an asteroid body with surrounding
vacuoles in the cytoplasm. The basophilic body in
the giant cell to the left may be an early, small
Schaumann body.
Sarcoidosis lymph node
Multiple noncaseating epithelioid granulomas
There is no caseation, but some contain
calcified laminated Schaumann bodies
(arrows).
