
EPIDEMIOLOGY OF
HYPERTENSION (HT)
Dr Faris Al Lami
MB,ChB MSc PhD FFPH

HYPERTENSION
•
Commonest CVD
•
A major PH problem at global level because of:
High prevalence
Association with increased risk of CVDs.
•
A major RF for CV mortality, CHD, CVA, CHF,
and CRF
HYPERTENSION
•
The relationship between BP and risk of CVD
events is:
o
Continuous
o
Consistent
o
Independent of other RFs
•
The higher the BP the greater the chance of
heart attack, HF, stroke, and kidney diseases.

Hypertension
Advances in the diagnosis and treatment of
hypertension lead to dramatic declines in CHD
and stroke mortality in industrialized countries.
It is estimated that
1.2 billion
people
suffering HT worldwide

Hypertension
•
In EMR it affects about
26%
of adult
population
and it affects
125
million individuals
•
About
75%
of HT individuals are unaware of
being diseased
•
About
50%
of hypertensive patients who knew
they are diseased are either not on treatment
or taking treatment but not controlled.
Hypertension
Of greater concern is that CV complications of high
BP are on the increase, including the incidence of
stroke, ESRD and HF.
These alarming data support a need for:
Greater emphasis on public awareness
Aggressive approach to anti HT treatment.

HYPERTENSION
•
Definition of hypertension is arbitrary
The level of blood pressure at which treatment
does more good than harm
•
BP follows normal distribution curve
•
BP has a high intra-individual variation
•
CV risk associated with HT is strongly correlated
with both SBP and DBP, correlation is higher
with SBP

Population with HT constituted a risk
pyramid:
•
No. of individuals with mild HT at the base of
the pyramid is high, but the RR is small
•
No. of individuals with sever HT at the tip of
the pyramid is small, but the RR is high
•
Absolute no. of complications attributable to
HT is more at base than the tip of the pyramid

To achieve community control of HT
related CV complications it is important to
control mild HT
A
2
mm decrease in the entire distribution
will decrease mortality from:
•
Stroke by 6%,
•
CHD by 4%
•
All causes by 3%

•
Beginning at 115/75mmHg, CVD risk (IHD and
Stroke) doubles for each increment of 20/10
mmHg
•
BP values between 130-139/85-89mmHg are
associated with a more than two folds
increase in relative risk from CVD as compared
with those with BP levels below 120/80 mmHg

•
DHT predominates before age 50, either alone
or in combination with SBP elevation
•
The prevalence of SHT increases with age and
above 50 SHT represents the most common
form of HT
•
DBP is a more potent CV RF than SBP until the
age 50, thereafter SBP is more important.

CLASSIFICATION OF HT
The severity of HT depends on:
•
BP level
•
Concomitant CV RFs
•
End-organ damage

For practical reasons, HT can be classified
into
1.HT with NO other CV RFs and NO target organ
damage
2.HT with other CV RFs
3.HT with evidence of target organ damage
4.HT with other CV RFs AND evidence of other
organ damage

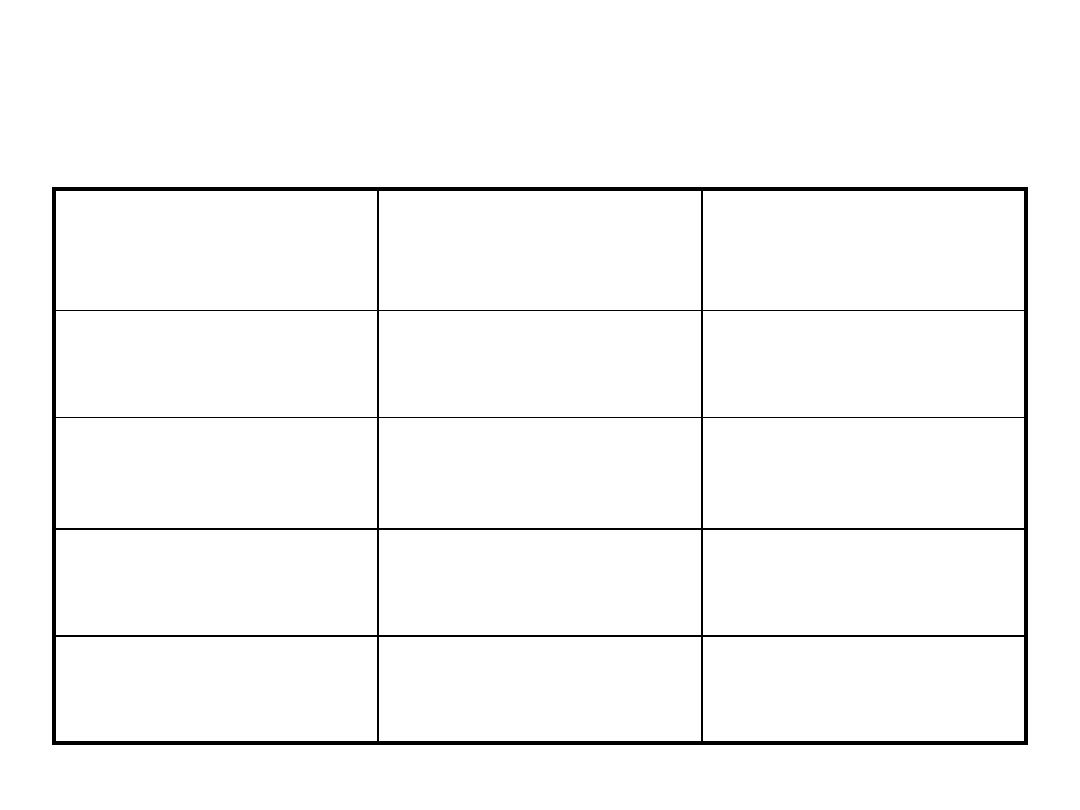
Classification of HT by BP level:
TYPE
SBP (mmHg) DBP (mmHg
)
•
Normotensive <140 and <90
•
Mild HT 140-180 or 90-105
•
Subgroup, Borderline HT 140-160 or 90-95
•
Mod. And Severe HT >180 or >105
•
Isolated SHT >140 and <90
•
Borderline SHT 140-160 and
<90

Classification of HT by Target Organ
Damage:
•
Stage I: No Manifestation
•
Stage II: At least one of the following:
1.LVH
2.Gen. or Focal narrowing of retinal arteries
3.Microalbuminuria; proteinuria: and /or slight increase
in serum creatinin level (1.2-2 mg/dl)
4.U/S or radiology evidence of plaque in aorta, carotid,
iliac, or femoral arteries
Stage III: Appearance of symptoms or
signs
•
Heart:
AP
MI
HF
•
Brain:
Stroke
TIA
HT encephalopathy
Vascular dementia
•
Optic fundi
Retinal Hmg. And exudates
+/- papilloedema
•
Kidney:
S.creatinin level > 2 mg/dl
RF
•
Vessels:
Dissecting aneurysm
Symptomatic occlusive
disease

Classification of HT by Causes
I. Primary (essential) HT
II. Secondary HT:
•
Renal: renal parenchyma dis., Reno vascular dis. , rennin
producing tumor
•
Drugs: OC, Corticosteroids , Liquorices< carbenoxolone,
sympathomometics , NSAIDs
•
Endocrin: Acromegaly, Cushing Syndrome, Primary
hyperaldosteronism, Congenital adrenal hyperplasia,
Pheochromocytoma, Carcinoid tumors
•
Coarctation of Aorta and Aoartitis
•
Pregnancy induced HT

RECLASSIFICATION OF BP
•
New data of lifetime risk of HT and the increase of CV
complications associated with levels of BP previously
considered to be normal
•
JNC 7 introduced “ prehypertension”
•
The aim is to:
identify those in whom early intervention by
adoption of healthy lifestyle could reduce BP,
decrease the rate of progression of BP to
hypertensive levels with age, or
prevent hypertension entirely.
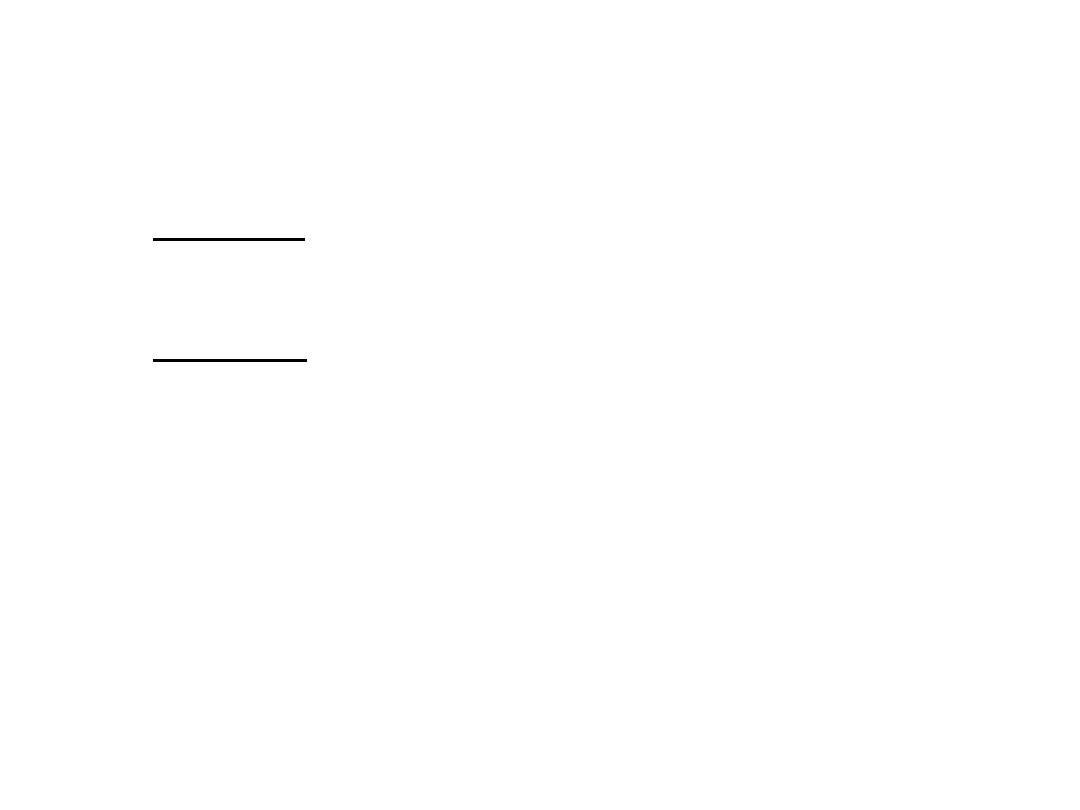
JNC7 category
SBP/DBP
JNC6 category
Normal
<120/80
Optimal
Prehypertension
120-129/80-84
130-139/85-89
Normal
Borderline
Hypertension
≥140/90
Hypertension
Stage 1
Stage 2
Stage 2
140-159/90-99
160-179/100-109
≥180/110
Stage 1
Stage 2
Stage 3
CLASSIFICATION OF BP FOR ADULTS
DBP
mmHg
SBP
mmHg
BP
classification
And <80
<120
NORMAL
Or 80-89
120-139
PREHYPERTE
NSION
Or 90-99
140-159
STAGE 1 HT
Or ≥100
≥160
STAGE 2 HT

Prehypertension
•
Prehypertension is not a disease category.
•
They are not intended to have drug therapy, but
should be advised to practice lifestyle modification to
reduce risk of developing HT
•
Individuals with prehypertension who also have DM
or kidney diseases should be considered candidates
for appropriate drug therapy if a trial of lifestyle
modification fails to reduce their BP to 130/80
mmHg or less.

•
The goal for individuals with prehypertension
with no compelling conditions is to lower BP
to normal levels with lifestyle changes, and
prevent the progressive rise in BP using the
recommended lifestyle modifications.
Factors influencing BP level:
–
Age: a positive association between BP level and
age in most populations of different geographical,
cultural, and SE characteristics.
The rise in SBP continue throughout life in contrast
to DBP which rises until the age 50, tends to level
off over the next decade, and may remain the
same or fall later in life.
Factors influencing BP level:
–
Sex: early in life, there is no difference between
males and females in BP level, but after puberty
males tend to have higher BP level than females.
After menopause the difference gets narrower.
Factors influencing BP level:
–
Ethnicity: Blacks have higher BP level than others
–
SE status: in post-transitional populations –inverse
relation
In pre and transitional populations – positive
association

Risk Factors of HT
1.Hereditary factors : positive family history
2.Genetic factors: certain genes as ACE gene
3.Early life exposure to certain events: as LBW
4.Certain childhood predictors: as BP response
to exercise, weight gain, LV mass…
Risk Factors of HT
5.Body weight: overweight individual has 2-6 times
higher risk having HT compared to a normal weight
individual.
6.Central Obesity and Metabolic Syndrome: high
waist/hip ratio is positively associated with HT
7.Nutritional factors: positive association between Nacl
intake and HT, negative association between
potassium intake and HT, and no relation with
other nutrients.

Risk Factors of HT
8.Alcohol intake : causes acute and chronic increase in
BP level
9.Physical Inactivity : Sedentary unfit individual has 20-
50% excess risk to have HT
10.Heart rate : HT patients have higher HR than
normotensive individuals
11.Psychological factors: acute mental stress causes
increase in BP level
12.Environmental factors: noise, air pollution

Prevention of HT
•
Community Approach
Primary prevention of HT in the whole population
•
High risk Approach ( individual case management)
Identification of individuals with high BP who are at
increased risk of complications
The two approaches are complementary

Community Approach
Aim: Primary Prevention of HT through:
1.Elimination of modifiable RFs
2.Promotion of protective factors maintaining
reasonable BP
3.Reduction of risks of complications by altering
the norms and behavior of population

It is useful to:
–
Avoid risky life-style that increase BP
–
Adoption of healthy life-style
–
Encourage industrial and agricultural activities to
provide healthier food
Population approach is highly effective in
decreasing HT and its complications in the
community, but it offers little direct individual
effect, making it of less motivation to people
and physicians.

Lifestyle measures for prevention of
HT
In the whole population (primary prevention)
they help in:
•
Decrease risk of development of HT
•
Decrease risk of development of other life-
style related disorders (DM, CHDs,)
Lifestyle measures for prevention of
HT
In individual patient, they help in:
•
Decrease BP
•
Avoid or decrease need for anti-HT treatment
•
Control associated RFs

FOUR life-style measures
proved effective in clinical
trials:
1.Weight Reduction
•
Decreases BP in HT patients with >10%
overweight
•
Decreases insulin resistance
•
Improves lipid profile
Obese patients with mild or borderline HT
should try weight reduction for 3-6 months
before starting anti-HT treatment

2.Reduction of alcohol intake:
•
Decreases SBP/DBP by 4.8/3.3 mmHg
•
When combined with 10 Kg weight loss , BP
will decrease by 10.2/7.5 mmHg

3.Increased physical activity
•
Effective for prevention and treatment of HT
•
Dynamic , isotonic exercises ( walking) is more
effective than static , isometric exercises (
weight lifting)
•
Brisk walking for 30-60 minutes /day for 5
times / week is better than strenuous
exercises.
4.Reduction of Sodium intake
•
Recommended intake is < 6 gm /day
•
Elderly people and blacks demonstrate more
sensitivity to sodium restriction

Life style measures to control other CV
RF
1.Tobacco smoking
•
Smoker hypertensive has 2-3 folds excess risk
of stroke and CHD.
•
Cessation of smoking is the most effective
single step to decrease CV risk among
hypertensive.

Life style measures to control other CV
RF
2.Dyslipidemia
Increased physical activity is most appropriate
in HT patients with dyslipidemia

Life style measures to control other CV
RF
3.Diabetes Mellitus
Regular exercise, weight reduction, and low fat
high fiber diet can improve insulin sensitivity,
and decrease contribution of insulin resistance
to high BP.
