
LEISHMANIASIS ICD-10 B55
Dr. Nadia Aziz Nasir
C.A.B.C.M.
Department of community medicine
Baghdad medical college
Community
1

Objectives
1- Define LEISHMANIASIS, its types, visceral &
cutaneous.
2- identify sign & symptoms & its occurrence
3- identify the mode of transmission
4- identify the incubation period & methods of
controlling the disease.
2

I. CUTANEOUS AND MUCOSAL
LEISHMANIASIS ICD-10 B55.1, B55.2
A polymorphic
protozoan
disease of
skin
and
mucous membranes
caused by several species
of the genus Leishmania.
These protozoa exist as obligate
intracellular
parasites in humans and other mammalian
hosts.
3

CUTANEOUS AND MUCOSAL
LEISHMANIASIS
The disease starts with a
macule
then a
papule
that enlarges and typically becomes an
indolent
ulcer
Lesions may be single or multiple, occasionally non
ulcerative and diffuse.
Lesions may
heal spontaneously within weeks to
months
, or last for a year or more.
4

5

CUTANEOUS AND MUCOSAL
LEISHMANIASIS
In some individuals, certain strains can
disseminate to cause
mucosal lesions (espundia)
These sequelae, which involve
nasopharyngeal
tissues, are characterized by
progressive tissue
destruction
and often scanty presence of
parasites and can be severely disfiguring.
6

Diagnosis
1-
Microscope
identification
of the nonmotile,
intracellular form (amastigote) in stained
specimens from lesions.
2-
Culture
of the motile, extracellular form
(promastigote) on suitable media.
7

Diagnosis
3-
Intradermal (Montenegro)
test with antigen
derived from the promastigotes, it is
negative
in
very
early lesions
or
immunosuppressed
patients.
4-
Serological (IFA or ELISA)
testing for mucosal
leishmaniasis
8

Infectious agents
Eastern hemisphere: Leishmania tropica,
L. major, L. aethiopica
western hemisphere: L. braziliensis and
L. mexicana complexes.
9

Infectious agents
Members of
L. donovani
complex usually cause
visceral disease in the eastern hemisphere,
in the western hemisphere the responsible
organism is
L.
infantum/chagasi
10

Occurrence
2 million new cases per year
In the eastern hemisphere,
urban
population
groups, including children, are at risk for
anthroponotic
cutaneous leishmaniasis
due to
L. tropica
.
In
rural
areas, people are at risk for
zoonotic
cutaneous leishmaniasis due to
L. major
.
11

Reservoir
Humans
(in anthroponotic cutaneous
leishmaniasis),
wild rodents
(gerbils), hyraxes,
marsupials and
domestic dogs
12
13

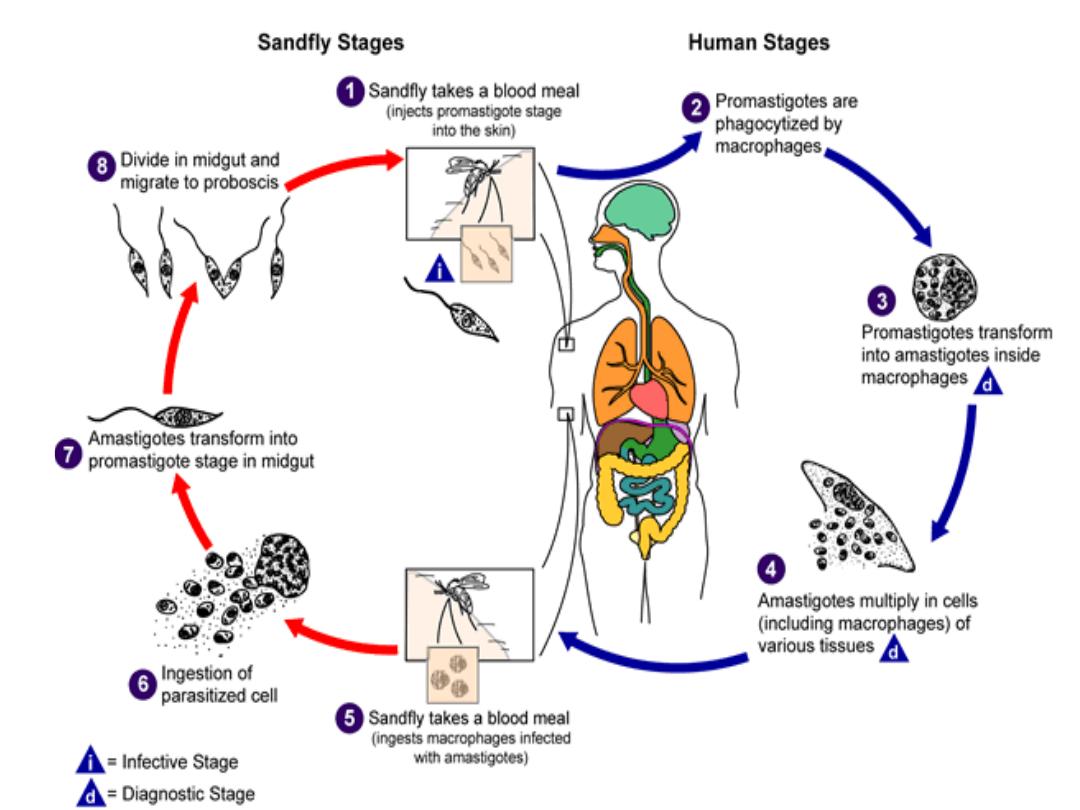
Mode of transmission
From the animal reservoir through
the bite of
infective female phlebotomines (sandflies).
Motile promastigotes develop and multiply in
the gut of the sandfly after it has fed on an
infected mammalian host
In
8–20
days, infective parasites develop and are
injected during biting.
14

15
16

Incubation period
At least a
week
, up to
many months
.
17

Period of communicability
Not directly transmitted from person to person,
but
infectious to sandflies
as long as parasites
remain in lesions in untreated cases, usually a
few months to 2 years.
Eventual
spontaneous healing
occurs in most
cases.
18

Susceptibility
Is probably general.
Lifelong
immunity may be present after lesions
due to L. tropica or L. major heal
19

Methods of control
A. Preventive measures:
Currently no vaccine available.
1) Case management:
Detect
cases systematically
and
treat
rapidly. This applies to all forms of
leishmaniasis and is one of the important
measures to prevent development of destructive
mucosal lesions
20

Preventive measures
2) Vector control:
Apply
residual insecticides
periodically.
Phlebotomine sandflies have a relatively
short flight
range and are highly susceptible to control by systematic
spraying with residual insecticides.
Possible breeding places of sandflies, such as stone
walls, animal houses and rubbish heaps, must be
sprayed.
21

Preventive measures
Insecticide-treated
bednets
are a good vector
control alternative, especially in anthroponotic
foci.
22

Preventive measures
3) Destroy gerbils (and their burrows)
implicated as reservoirs in local areas by deep
ploughing and removal of plants they feed on.
23

B. Control of patient, contacts and the
immediate environment
Specific treatment:
1- Mainly
pentavalent antimonials
, either
sodium stibogluconate, or meglumine
antimonate
24

B. Control of patient, contacts and the
immediate environment
2-
Pentamidine
is used as a second line drug for
cutaneous leishmaniasis.
3-
Imidazoles
, ketoconazole and itraconazole
4-
Amphotericin B
for mucosal disease if this
does not respond to antimonial therapy.
25

II. VISCERAL LEISHMANIASIS
(Kala-azar) ICD-10 B55.0
A chronic systemic disease caused by
intracellular
protozoa
of the genus Leishmania.
The disease is characterized by
fever
,
hepatosplenomegaly, lymphadenopathy, anemia,
leukopenia, thrombocytopenia
and progressive
emaciation and weakness.
Untreated clinically evident disease
is usually fatal.
26

VISCERAL LEISHMANIASIS
Fever
is of
gradual
or
sudden
onset,
persistent
and
irregular
, often with
two daily
peaks
, alternating periods of
apyrexia and low-grade fever.
Post-kala-azar
dermal
lesions
may occur after
apparent cure of systemic disease.
27

VISCERAL LEISHMANIASIS
Leishmania/HIV co-infection
is a well-known
entity in southern Europe, and in eastern Africa
and in Asia.
28

Diagnosis
1-
Culture
of the organism from a biopsy
specimen or aspirated material
2-
Demonstration of intracellular amastigotes
in
stained smears from bone marrow, spleen, liver,
lymph nodes or blood
3-
PCR
technique is the most sensitive but
expensive.
29

Diagnosis
4- Serological diagnosis is based on
IFA
and
ELISA
, tests that are expensive
5- Freeze-dried antigen (
DAT
) and
dipsticks
(k39/k26) are inexpensive, easy to use and
reliable
30

Infectious agents
Typically Leishmania donovani, L. infantum
and L. infantum/chagasi.
31

Occurrence
Visceral leishmaniasis occurs with a yearly
incidence of 500 000 cases
the disease occurs as scattered cases among
infants
,
children
and
adolescents
but
occasionally in epidemic waves.
Incidence is modified by the use of antimalarial
insecticides.
32

Reservoir
Include
humans
,
wild
Canidae
(foxes and
jackals) and
domestic dogs
.
33

Mode of transmission
Through bite of infected phlebotomine sandflies.
In anthroponotic visceral leishmaniasis,
humans
are the only reservoir and transmission occurs
through the sandfly bite.
In zoonotic visceral leishmaniasis,
dogs
, constitute
the main source of infection for sandflies.
Person-to-person
transmission has been reported
in intravenous drug users
34

Incubation period
Generally
2–6 months
, range is 10 days to
years.
35

Susceptibility
Kala-azar induces
lasting homologous
immunity.
Asymptomatic
and
subclinical
infections
are
common.
Malnutrition
&
AIDS
predisposes to
reactivation of latent infections
.
36

Treatment
Pentavalent antimonials
is the first-line drugs.
Sodium stibogluconate, and meglumine
antimonate are effective.
Amphotericin B
or
pentamidine
for cases not
responding to antimony (not used routinely
because of
toxicity
& its price restricts use to
industrialized countries).
37

Treatment
Aminosidine
(paramomycin), a good for
combination therapy with antimonials therapy.
38
