Epidemiology & control of tropical disease
Dr. Nadia AzizC.A.B.C.M.
Department of community medicine
Baghdad medical college
MALARIA ICD-10 B50-B54
Objectives1- Identify Malaria & its different types
2- Describe its occurrence
3- Identify signs & symptoms of the clinical disease
4- Identify the diagnostic methods
5- Describe the methods of control
MALARIA
A parasitic disease infections with the 4 human types of malaria.The fever pattern of the first few days of infection resembles early stages of many other
illnesses.
MALARIA
The most serious malarial infection, falciparum malaria presents a clinical picture including
fever, chills, sweats, anorexia, nausea, lassitude, headache, muscle and joint pain, cough and diarrhea.
Anaemia and/or splenomegaly.
Complications
Acute encephalopathy (cerebral malaria),severe anemia, icterus, renal failure (black-water fever), hypoglycaemia, respiratory distress, lactic acidosis and more rarely coagulation defects and shock. Severe malaria is a possible cause of coma and other CNS symptoms.
Blackwater fever
Also called malarial hemoglobinuria , one of the less common yet most dangerous complications of malaria. It occurs almost exclusively with infection from the parasite Plasmodium falciparum. Blackwater fever has a high mortality.The passage of urine that is black or dark red in colour
The distinctive colour of the urine is due to the presence of large amounts of hemoglobin, released during the extensive destruction of the patient’s red blood cells by malarial parasites.
High Risk population
Pregnant women and young children when infected are highly susceptible to development of severe and complicated malaria.Malaria in a pregnant woman increases the risk of maternal death, miscarriage, stillbirth and neonatal death.
Case-fatality
Among untreated children and adults can reach 10%–40% or higher.Types of Malaria
The other human malarias:
Vivax
malariae
and ovale
Are not usually life-threatening.
MALARIA
After a fever-free interval, the cycle of chills, fever and sweating recurs daily, every other day or every third day.MALARIA
True relapses with no parasitaemia (in vivax and ovale infections) may occur at irregular intervals for up to 5 years.Infections with P. malariae may persist for life with or without recurrent febrile episodes.
Diagnosis
1- Demonstration of malaria parasites inblood films. Repeated microscopic examinations every 12–24 hours may
be necessary because the blood density of parasites varies.
Diagnosis
Both thick & thin blood films should be done.
Thick film find parasites that may be present in small numbers.
Thin film for species identification and determination of degree of parasitemia( the percentage of erythrocytes harboring parasites)
Diagnosis
2- Rapid diagnostic tests that detect plasmodial antigens in the blood.3- PCR is the most sensitive method.
4- Antibodies, demonstrable by IFA (not helpful for diagnosis of current illness)
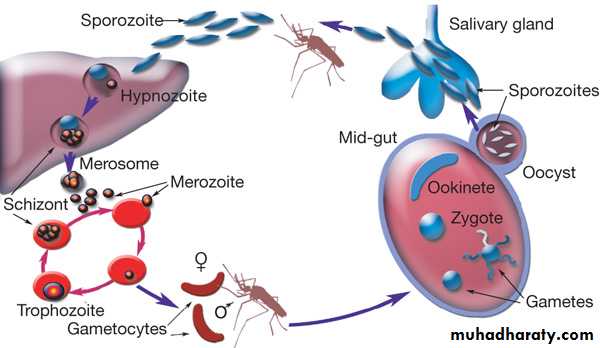
Infectious agents
Plasmodium falciparum, P. vivax, P. ovaleand P. malariae,
protozoan parasites with asexual and sexual phases.
Occurrence
The disease causes over 1 million deaths per year in the world, most of these in young children in Africa.Reservoir
Humans are the only important reservoir of human malaria.For P. malariae, which is common to man, the
African apes and probably some South American monkeys.
Mode of transmission
1- Bite of an infective female Anopheles
mosquito.
Most species feed at night,
some important vectors
also bite at dusk or in the early
morning.
Mode of transmission
2- Injection or transfusion of infected blood3- Use of contaminated needles and syringes (e.g. injecting drug users).
4- Congenital transmission occurs rarely.
Incubation period
The period between an infective bite and detection of the parasite in a thick blood smear is the “prepatent period,” which is typically 6–12 days for P. falciparum, 8–12 days for P. vivax and P. ovale and 12–16 days for P. malariae, But may range up to about 2 monthspregnant women are more vulnerable to falciparum malaria (and possibly other Plasmodium species) that infect the placenta and cause low birth-weight ,anemia, abortion and premature delivery.
Period of communicability
Humans may infect mosquitoes as long as infective gametocytes are present in the blood; this varies with parasite species and with response to therapy.The mosquito remains infective for life.
Methods of control
A. Preventive measures:I. Local community measures
1) Insecticide-treated mosquito nets (ITNs) are the most universally useful measure for the prevention of malaria. (pyrethrinoids should be repeated once or twice a year)
Preventive measures
2) Indoor residual spraying with insecticides (IRS) targeting adult mosquitoes, where they rest indoors on sprayablesurfaces.
Preventive measures
3) In epidemic-prone areas, malaria surveillance should be based on weekly reporting and monitoring important factors environmental conditions and human population movements.
Preventive measures
4) protection from biting mosquitoes is of paramount importance.5) prophylaxis with antimalarial drugs for travellers to malarious areas, and “standby” or emergency self-treatment is recommended
when a febrile illness occurs in a falciparum malaria area.
Malaria prophylaxis
Chloroquine (5 mg base/kg/week) plusProguanil (3 mg/kg/day) may be safely given to infants.
Standby treatment
The most important factors that determine the survival of patients with falciparum malaria are early diagnosis and immediate treatment.Prophylaxis
1- Chloroquine Minor side-effects2- Hydroxychloroquine less side – effects
3- Mefloquine It is not recommended for women in first trimester of pregnancy(serious side-effects with long-term use)
4- Doxycycline alone (100 mg once daily)
Prophylaxis
5-Primaquine 0.5 mg base/kg/day for adults
(do not have G6PD deficiency).
With the exception of primaquine, chemosuppressive drugs do not eliminate intrahepatic parasites, so clinical relapses of vivax or ovale malaria may occur after the drug is discontinued.
B. Control of patient, contacts and the immediate environment
1) Isolation: For hospitalized patients, blood precautions. patients should be in mosquito-proof areas from dusk to dawn.B. Control of patient, contacts and the immediate environment
2) Investigation of contacts and source of infection:Determine history of previous infection or of possible exposure e.g. sharing needles or transfusion-induced malaria.
Treatment
3) Specific treatment for all forms of malaria:1- Chloroquine- sensitive P. falciparum, P. vivax, P. Malariae and P. ovale is the oral administration of a total of 25 mg of chloroquine base/kg administered
Plasmodium falciparum is nowadays resistant to chloroquine and to sulfadoxine-pyrimethamine
Treatment
2) Quinine dihydrochloride, for emergency treatment of adults with severe or complicated infections or unable to retain orally medication, 20 mg salt/kg ,diluted in 10 ml/kg of isotonic fluid, by slow IVTreatment
3) Primaquine, is the drug of choice for prevention of relapses of P. vivax and P. ovale infections.Thank you