1
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
OBSTETRICS
Lec: 17.5
1- Post-partum hemorrhage
2- Retained placenta
3- Uterine inversion
4- Ruptured uterus
5- Obstetric shock (collapse)
PRI MARY PPH:
¡ Postpartum hemorrhage, defined as the loss of more than 500 mL
of blood from the genital tract following, but within the first 24
hours of, the delivery of the baby.
¡ Occurs in up to 5 percent of all deliveries.
1,2
Blood loss exceeding
1,000 mL is considered physiologically significant and can result in
hemodynamic instability.
3
Even with appropriate management,
approximately 0,7percent of vaginal deliveries will result in severe
post- partum hemorrhage.
4
It is the most common maternal
morbidity in developed countries and a major cause of death
worldwide
Secondary PPH:
¡ Is more of a subjective diagnosis, as its definition is blood loss from
the genital tract of a volume greater than expected after the first 24
hours, but within the first 6 weeks of delivery.
2
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
¡ The major etiological factors associated with secondary pph are
retained placental fragments & endometritis.
Complications:
¡ Complications from postpartum hemorrhage include :
1- Maternal death
2- Acute renal
failure 3- Embolism
4- Anemia
5- Sheehan’
s syndrome
6- Sepsis
7- Failure of lactation
Aetiolog y:
¡ Causes of postpartum hemorrhage are
uterine atony
,
trauma
,
retained
placenta
, and
coagulopathy
, commonly referred to as the
"four Ts":
¡ T
one
:
uterine atony
is the inability of the uterus to contract and may
lead to continuous bleeding. Retained placental tissue and infection
may contribute to uterine atony.
¡ T
rauma
: trauma from the delivery may tear tissue and vessels leading
to significant postpartumbleeding.
¡ T
issue
: retention of tissue from the
placenta
or
fetus
may lead
to bleeding.
¡ T
hrombin
: a
bleeding disorder
occurs when there is a failure of
clotting
, such as with diseases known as
coagulopathies
.
¡ Causes of postpartum hemorrhage and their incidence Cause
Incidence Uterine atony 70% Trauma 20% Retained tissue 10%
Coagulopathy 1%
3
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
Risk factors:
¡ Factors relating to the preg nancy:
§
Antepartum hemorrhage
in this pregnancy
§
Placenta Previa
(15 x risk)
§
Multiple pregnancy
(5 x risk)
§
Pre-eclampsia
or pregnancy-induced
hypertension
(4 x risk)
§ Multiparity (3 x risk)
§ Previous PPH (3 x risk)
§ Asian ethnic origin (2 x risk)
§ Maternal obesity (2 x risk)
¡ Factors relating to delivery:
§ Emergency
Caesarean section
(CS) (9 x risk)
§ Elective CS (4 x risk) - especially if >3 repeat procedures
[6]
§ Retained placenta (5 x risk)
§ Mediolateral episiotomy (5 x risk)
§ Operative vaginal delivery (2x risk)
§ Labour of >12 hours (2 x risk)
§ >4 kg baby (2 x risk)
§ Maternal pyrexia in labour (2 x risk)
¡ Pre- existing maternal hemorrhag ic conditions:
§ Factor 8 deficiency -
Hemophilia A
carrier
§ Factor 9 deficiency -
Hemophilia B
carrier
§
Von Willebrand's disease

4
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
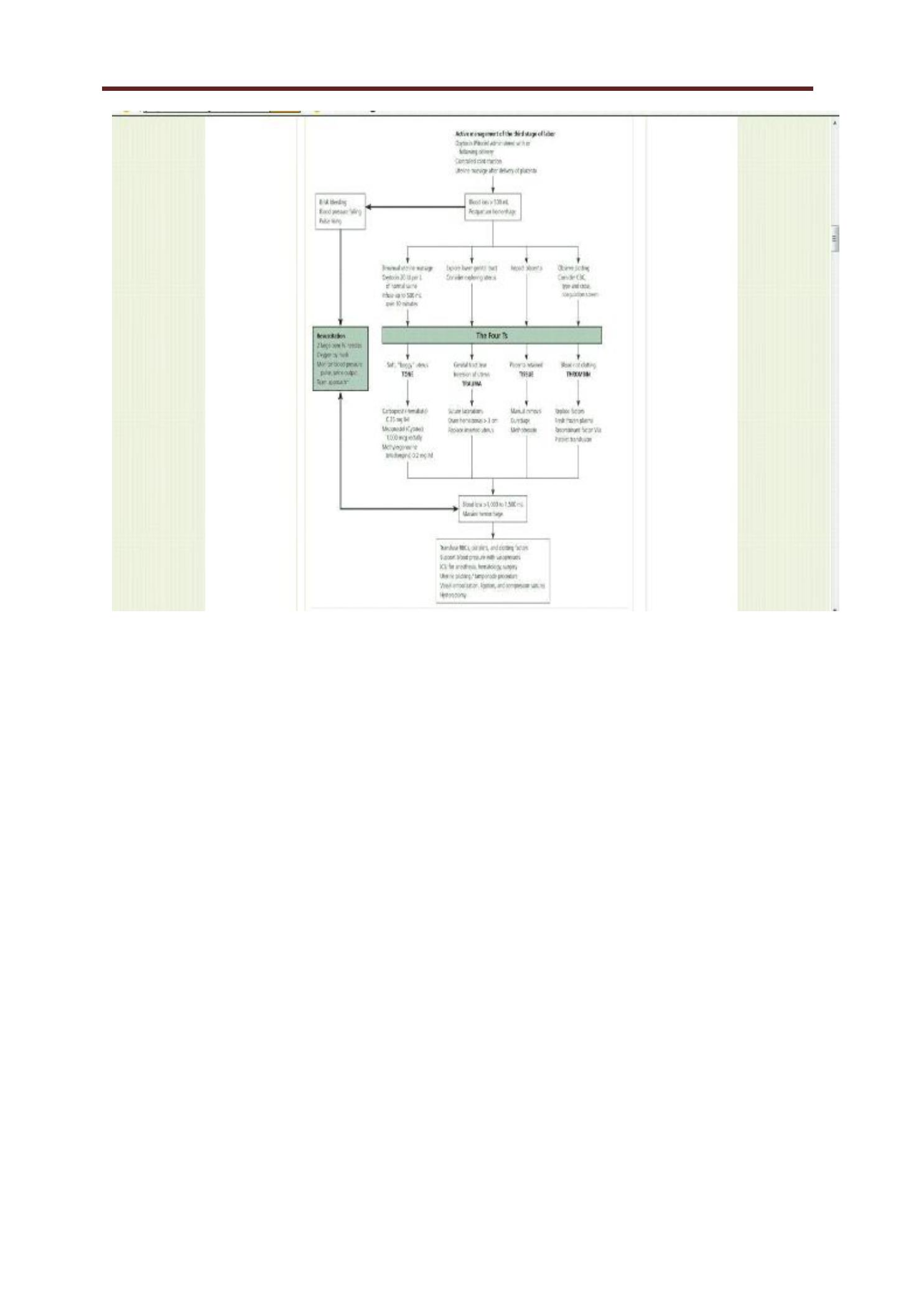
Manag ement: Prevention:
¡ The best preventive strategy is active management of the third stage
of labor. Hospital guidelines encouraging this practice have resulted in
significant reductions in the incidence of massive hemorrhage.
19
Active management, which involves administering a uterotonic drug
with or soon after the delivery of the anterior shoulder, controlled
cord traction, and, usually, early cord clamping and cutting, decreases
the risk of postpartum hemorrhage and shortens the third stage of
labor with no significant increase in the risk of retained placenta.
Compared with expectant management, in which the placenta is
allowed to separate spontaneously aided only by gravity or nipple
stimulation,active management decreases the incidence of
postpartum hemorrhage by 68 percent.
¡ Prophylactic administration of oxytocin (Pitocin) reduces rates of
postpartum hemorrhage by 40 percent; this reduction also occurs if
oxytocin is given after placental delivery. Oxytocin is the drug of
choice for preventing postpartum hemorrhage because it is at least
as effective as ergot alkaloids or prostaglandins and has fewer side
effects. Misoprostol (Cytotec) has a role in the prevention of
postpartum hemorrhage (NNT = 18); this agent has more side effects
but is inexpensive, heat- and light-stable, and requires no syringes.
Diag nosis and Manag ement
¡ The diagnosis of postpartum hemorrhage begins with recognition of
excessive bleeding and methodic examination to determine its
cause. The “
Four Ts”mnemonic (Tone, Trauma, Tissue, and
Thrombin) can be used to detect specific causes (
Table 1
).
5
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
Resuscitation:
¡ Two large-bore intravenous cannulae (16G).
¡ Fluid administration (studies failed to show any benefit of colloids
over crystalloids).
¡ Application of facial oxygen.
¡ Examination to determine the etiology of the hemorrhage,
often performing uterine massage.
¡ Obtain blood for a full blood count, clotting studies & group &
cross- matching.
Disseminated intravascular coag ulation:
¡ Is a life threatening complication of massive PPH.

6
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
¡ Regardless the etiology, the management should aim to follow four
basic principles:
1- To maintain the intravascular volume.
2- To administer fresh frozen plasma at a rate to keep the APTT:
control ratio less than 1,5.
3- To administer platelets to maintain their count more than 75000.
4- To administer cryoprecipitate to keep fibrinogen level more
than 1
gm/dl.
TONE
¡ Uterine atony is the most common cause of postpartum hemorrhage.
Because hemostasis associated with placental separation depends on
myometrial contraction, atony is treated initially by pharmacological or
a combination of pharmacological & surgical intervention(
ergometrine administration followed by a syntocinoninfusion).
¡ Should these efforts fail to control bleeding, examination of the
genital tract need to be performed in an operating theatre . This
include examination of vagina, cervix &, in case of continued
bleeding, exploration of the uterine cavity digitally to identify &
removed any retained fragments of placenta.
At this time, if no other cause for the hemorrhage, administration
of prostaglandin analogues.
¡ Syntocinone i.v bolus dose of 5 i.u followed if necessary by an infusion
of 40 i.u .
¡ Ergometrine i.v/i.m 250-500 ug
¡ Misoprostol p.r 800-1000 ug
¡ Bimanual compression of the uterus , put the uterine arteries
under tension.
7
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
¡ In addition to uterotonics, drugs that promote coagulation can be
administered, such as tranexamic acid & recombinant active factor
7.
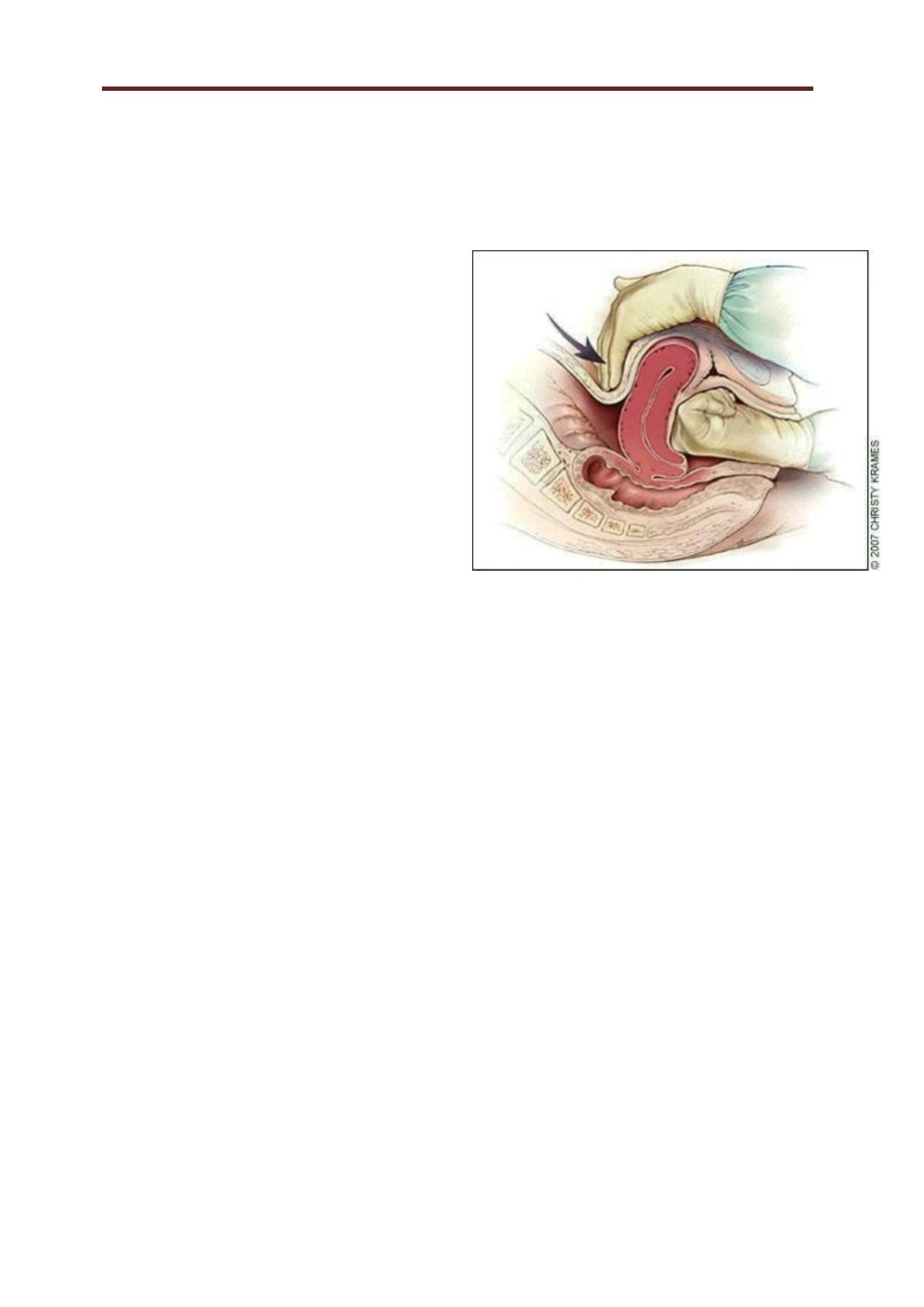
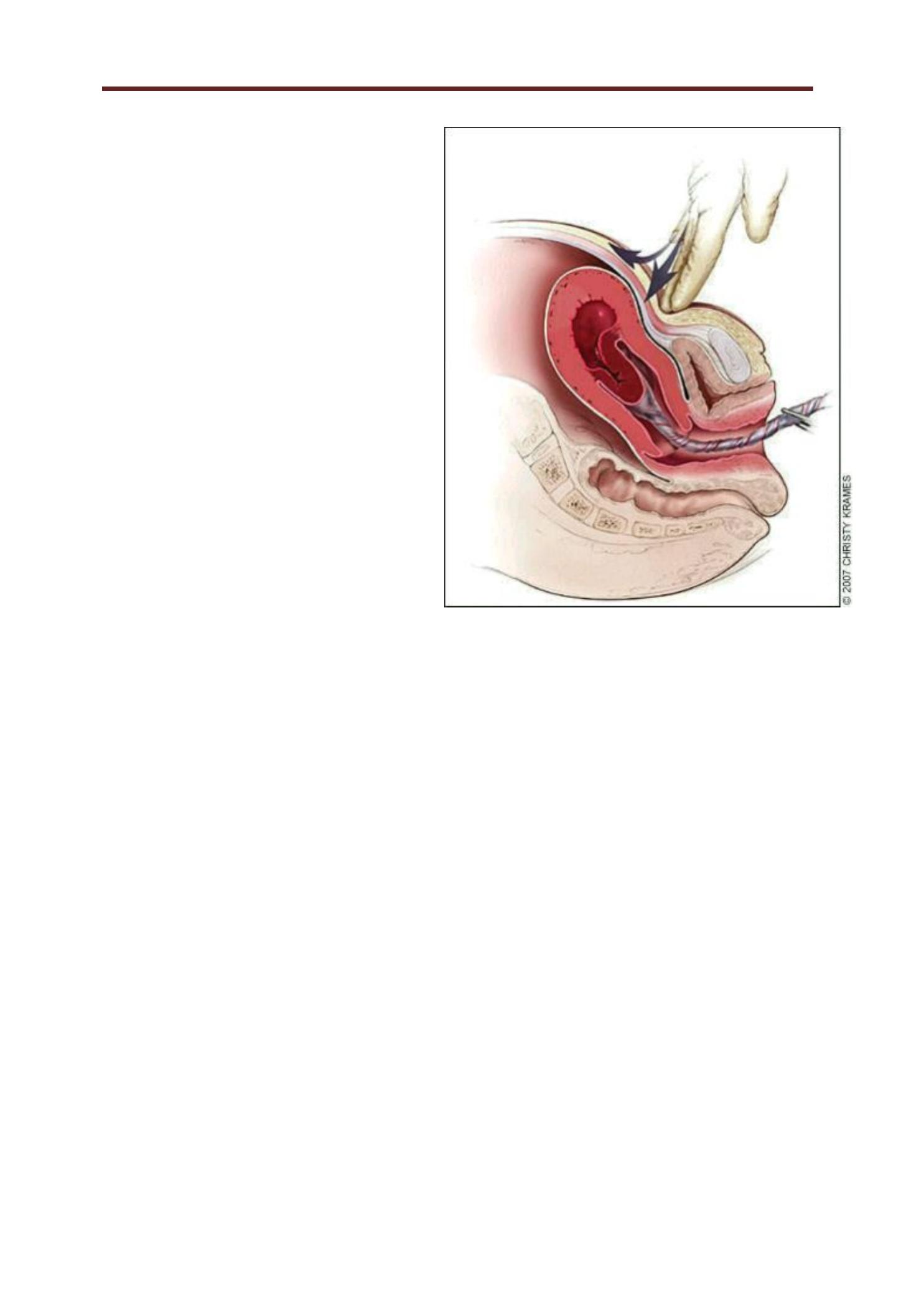
¡ Fig ure 1.
¡ Technique of bimanual
massage for uterine atony.
Bimanual uterine compression
massage is performed by
placing one hand in the vagina
and pushing against the body
of the uterus while the other
hand compresses the fundus
from above through the
abdominal
wall. The posterior aspect of the uterus is massaged with the
abdominal hand and the anterior aspect with the vaginal hand.
¡ Redrawn with permission from Anderson J, Etches D, Smith D.
Postpartum hemorrhage. In: Baxley E. Advanced Life Support in
Obstetrics course syllabus. 4th ed. Leawood, K an.: American
Academy of Family Physicians,2001.
¡ If these measures failed, the uterus can be packed (gauze,
balloon insufflation).
¡ L aparotomy: unilateral or bilateral uterine artery ligation with
success rate of more than 90 percent.
¡ Five steps: unilateral ligation of the uterine artery at the level of
the lower uterine segment.
¡ Bilateral ligation.
8
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
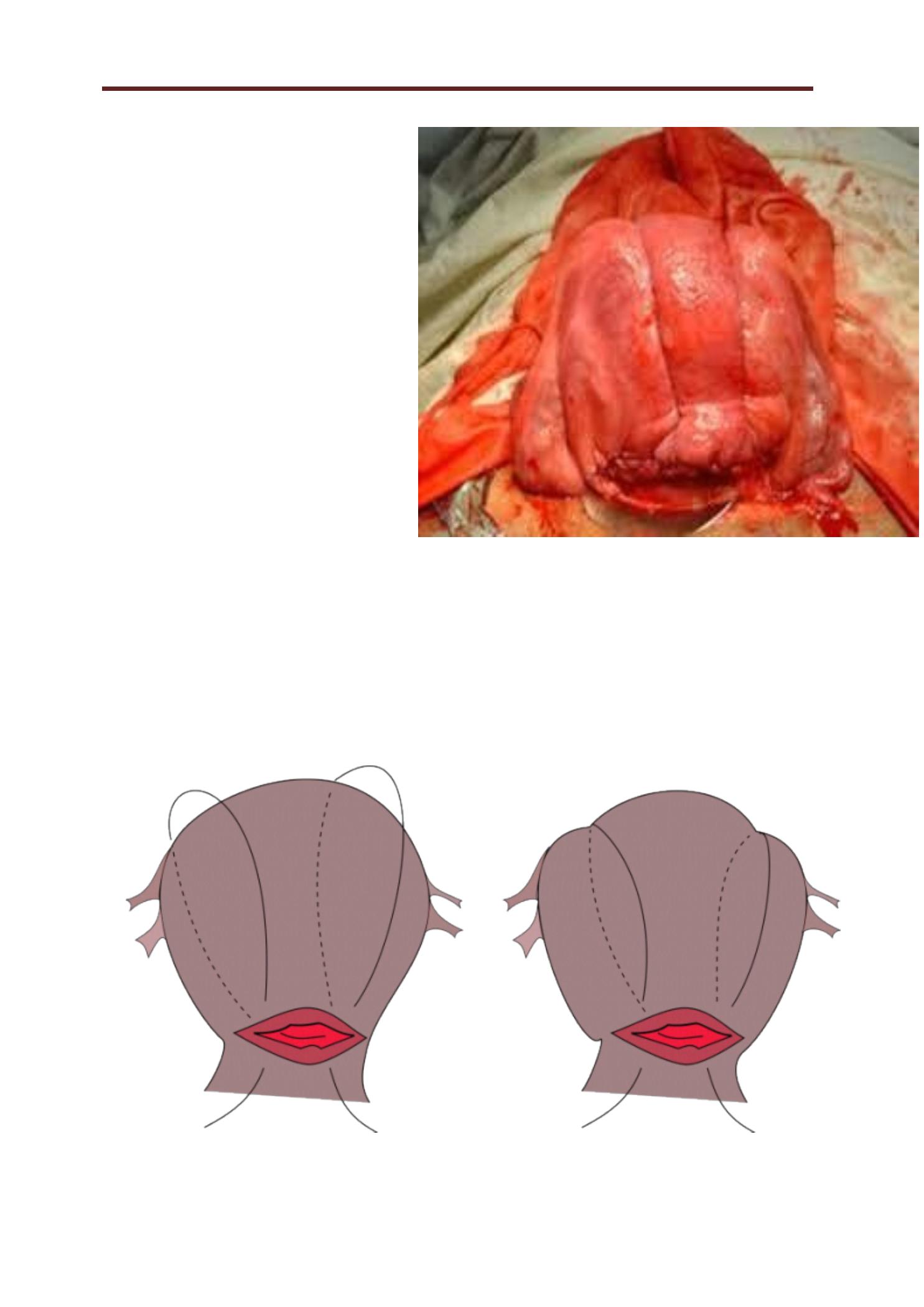
¡ L ow ligation of the
uterine artery after
mobilization of the
bladder.
¡ Unilateral ovarian
vessel ligation.
¡ Bilateral ovarian
vessel ligation.
¡ Internal iliac
arteries ligation.
¡ Compression sutures:
B- lynch sutures.
¡ Arterial embolization.
¡ Hysterectomy with ovarian conservation may be required as a
lifesaving procedure.
¡ Post-operative management:
¡ ICU, CVP, professionalcounseling.
¡ Prostaglandins enhance uterine contractility and cause
vasoconstriction. The prostaglandin most commonly used is 15-methyl

9
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
prostaglandinF
2a
,

10
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
or carboprost (Hemabate). Carboprost can be administered
intramyometrially or intramuscularly in a dose of 0.25 mg; this dose
can be repeated every 15 minutes for a total dose of 2 mg. Carboprost
has been proven to control hemorrhage in up to 87 percent of
patients. In cases where it is not effective, chorioamnionitis or other
risk factors for hemorrhage often are present. Hypersensitivity is the
only absolute contraindication, but carboprost should be used with
caution in patients with asthma or hypertension. Side effects include
nausea, vomiting, diarrhea, hypertension, headache, flushing, and
pyrexia.
¡ Misoprostol is another prostaglandin that increases uterine tone and
decreases postpartum bleeding. Misoprostol is effective in the
treatment of postpartum hemorrhage, but side effects may limit its
use. It can be administered sublingually, orally, vaginally, and rectally.
Doses range from 200 to 1,000 mcg; the dose recommended by FIGO
is 1,000 mcg administered rectally. Higher peak levels and larger
doses are associated with more side effects, including shivering,
pyrexia, and diarrhea. Although misoprostol is widely used in the
treatment of postpartum hemorrhage, it is not approved by the U.S.
Food and Drug Administration for this indication.
TRAUMA
¡ L acerations and hematomas resulting from birth trauma can cause
significant blood loss that can be lessened by hemostasis and timely
repair. Sutures should be placed if direct pressure does not stop the
bleeding. Episiotomy increases blood loss and the risk of anal
sphincter tears, and this procedure should be avoided unless urgent
delivery is necessary and the perineum is thought to be a limiting
factor.
¡ Hematomas can present as pain or as a change in vital signs
disproportionate to the amount of blood loss. Small hematomas can
be managed with close observation. Patients with persistent signs of
volume loss despite fluid replacement, as well as those with large or

11
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
enlarging hematomas,require incision and evacuation of the clot.
The involved area should be irrigated and the bleeding vessels
ligated.In
12
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
patients with diffuse oozing, a layered closure will help to
secure hemostasis and eliminate dead space.
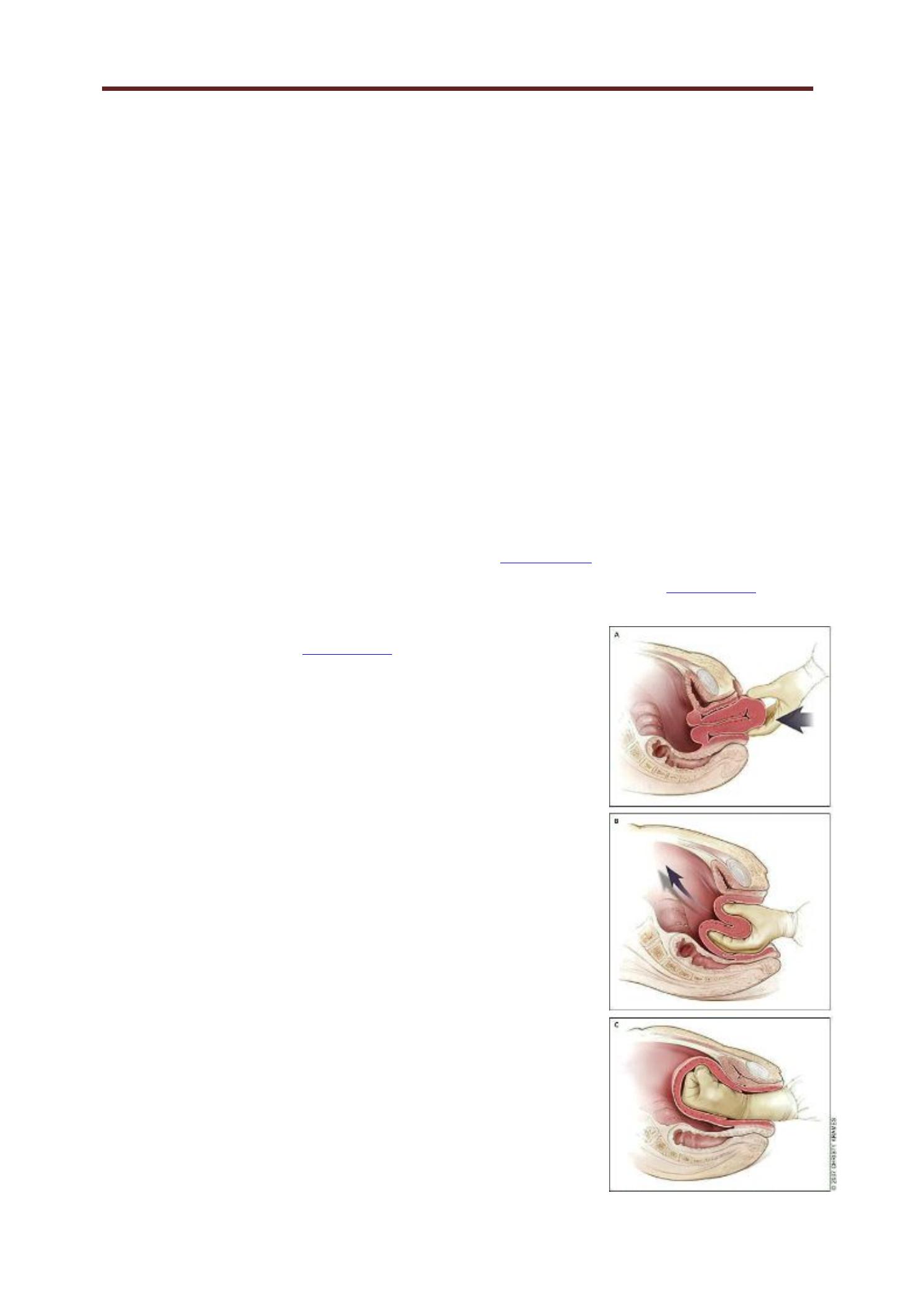
¡ Uterine I nversion
¡ Uterine inversion is rare, occurring in 0.05 percent of deliveries.
Active management of the third stage of labor may reduce the
incidence of uterine inversion. Fundal implantation of the placenta
may lead to inversion; the roles of fundal pressure and undue cord
traction are uncertain. The inverted uterus usually appears as a bluish-
gray mass protruding from the vagina. Vasovagal effects producing
vital sign changes disproportionate to the amount of bleeding may be
an additional clue. The placenta often is still attached, and it should be
left in place until after reduction. Every attempt should be made to
replace the uterus quickly. The Johnson method of reduction begins
with grasping the protruding fundus
Figure 2A
) with the palm of the
hand and fingers directed toward the posterior fornix (
Figure 2B
). The
uterus is returned to position by lifting it up through the pelvis and into
the abdomen (
Figure 2C
). Once the uterus is
reverted, uterotonic agents should be given to
promote uterine tone and to prevent
recurrence. If initial attempts to replace the
uterus fail or a cervical contraction ring
develop, administration of magnesium sulfate,
terbutaline (Brethine), nitroglycerin, or general
anesthesia may allow sufficient uterine
relaxation for manipulation. If these methods
fail, the uterus will need to be replaced
surgically.
Fig ure 2.
¡ Reduction of uterine inversion (Johnson
method). (A) The protruding fundus is
grasped with fingers directed toward the
posterior fornix. (B, C) The uterus is returned
to position

13
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
by pushing it through the pelvis and into the abdomen with
steady pressure towards the umbilicus.
¡ Redrawn with permission from Anderson J, Etches D, Smith D.
Postpartum hemorrhage. In: Baxley E. Advanced Life Support in
Obstetrics course syllabus. 4th ed. Leawood, K an.: American
Academy of Family Physicians,2001.
¡ Uterine Rupture
¡ Although rare in an unscarred uterus, clinically significant uterine
rupture occurs in 0.6 to 0.7 percent of vaginal births after cesarean
delivery in women with a low transverse or unknown uterine scar. The
risk increases significantly with previous classical incisions or uterine
surgeries, and to a lesser extent with shorter intervals between
pregnancies or a history of multiple cesarean deliveries, particularly in
women with no previous vaginal deliveries. Compared with
spontaneous labor, induction or augmentation increases the rate of
uterine rupture, more so if prostaglandins and oxytocin are used
sequentially. However, the incidence of rupture is still low (i.e., 1to 2.4
percent). Misoprostol should not be used for cervical ripening or
induction when attempting vaginal birth after previous cesarean
delivery.
¡ Before delivery, the primary sign of uterine rupture is fetal
bradycardia. Tachycardia or late decelerations can also herald a
uterine rupture, as can vaginal bleeding, abdominal tenderness,
maternal tachycardia, circulatory collapse, or increasing abdominal
girth. Symptomatic uterine rupture requires surgical repair of the
defect or hysterectomy. When detected in the postpartum period, a
small asymptomatic lower uterine segment defect or bloodless
dehiscence can be followed expectantly.
47
14
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
¡TISSUE :
¡C lassic signs of placental separation include a small gush of blood
with lengthening of the umbilical cord and a slight rise of the uterus
in the pelvis. Placental delivery can be achieved by use of the Brandt-
Andrews maneuver, which involves applying firm traction on the
umbilical cord with one hand while the other applies suprapubic
counterpressure (
Figure 4
29
).
49
The mean time from delivery until
placental expulsion is eight to nine minutes.
4
Longer intervals are
associated with an increased risk of postpartum hemorrhage, with
rates doubling after 10 minutes.
4
Retained placenta (i.e., failure of the
placenta to deliver within 30 minutes after birth) occurs in less than 3
percent of vaginal deliveries.
50
One management option is to inject
the umbilical vein with 20 mL of a solution of 0.9 percent saline and
20 units of oxytocin. This significantly reduces the need for manual
removal of the placenta compared with injecting saline alone.
51
Alternatively, physicians may proceed directly to manual removal of
the placenta, using appropriate analgesia. If the tissue plane between
the uterine wall and placenta cannot be developed through blunt
dissection with the edge of the gloved hand, invasive placenta should
be considered.
15
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
Fig ure 3.
¡ Brandt-Andrews maneuver
for cord traction. Firm
traction is applied to the
umbilical cord with one
hand while the other applies
suprapubic counter
pressure.
¡ Redrawn with permission
from Anderson J, Etches D,
Smith D. Postpartum
hemorrhage. In: Baxley E.
Advanced Life Support in
Obstetrics course syllabus.
4th ed. Leawood, K an.:
American Academy of
Family Physicians, 200
¡ Invasive placenta can be life threatening. The incidence has increased
from 0.003 percent to 0.04 percent of deliveries since 1950s; this
increase is likely a result of the increase in cesarean section rates.
Classification is based on the depth of invasion and can be easily
remembered through alliteration: placenta accrete adheres to the
myometrium, placenta increta invades the myometrium, and placenta
percreta penetrates the myometrium to or beyond the serosa. Risk
factors include advanced maternal age, high parity, previous invasive
placenta or cesarean delivery, and placenta previa (especially in
combination with previous cesarean delivery, increasing to 67 percent
with four or more). The most common treatment for invasive placenta
is hysterectomy. However, conservative management (i.e., leaving the
placenta in place or giving weekly oral methotrexate until human
chorionic gonadotropin levels are 0) is sometimes successful. Women
treated for a retained placenta must be observed for late sequelae,
including infection and late postpartum bleeding.

16
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
THROMBI N
¡ Coagulation disorders, a rare cause of post-partum hemorrhage, are
unlikely to respond to the measures described above. Most
coagulopathies are identified before delivery, allowing for advance
planning to prevent postpartum hemorrhage. These disorders include
idiopathic thrombocytopenic purpura, thrombotic thrombocytopenic
purpura, von Willebrand's disease, and hemophilia. Patients also can
develop HEL LP (hemolysis, elevated liver enz yme levels, and low
platelet levels) syndrome or disseminated intravascular coagulation.
Risk factors for disseminated intravascular coagulation include severe
pre-eclampsia, amniotic fluid embolism, sepsis, placental abruption,
and prolonged retention of fetal demise. Abruption is associated with
cocaine use and hypertensive disorders. Excessive bleeding can
deplete coagulation factors and lead to consumptive coagulation,
which promotes further bleeding. Coagulation defects should be
suspected in patients who have not responded to the usual measures
to treat post-partum hemorrhage, and in those who are not forming
blood clots or are oozing from puncture sites
¡ Evaluation should include a platelet count and measurement of
prothrombin time, partial thromboplastin time, fibrinogen level, and
fibrin split products (i.e., d-dimer). Management consists of treating
the underlying disease process, supporting intravascular volume,
serially evaluating coagulation status, and replacing appropriate
blood components. Administration of recombinant factor VIIa or clot-
promoting medications (e.g., tranexamic acid [ Cyklokapron]) may be
considered.

17
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
Clinical Approach
¡ Significant blood loss from any cause requires standard maternal
resuscitation measures. Blood loss of more than 1,000 mL requires
quick action and an interdisciplinary team approach. Hysterectomy is
the
18
A b normalities of the third stage of labor
29/ 11/ 2015
DR .Maad
definitive treatment in women with severe, intractable hemorrhage.
In patients who desire future fertility, uterus-conserving treatments
include uterine packing or tamponade procedures, B-lynch uterine
compression sutures, artery ligation, and uterine artery embolization.
The End
BY :
Taher Ali Taher
