Operative intervention in obstetrics Dr. Raghad March 10, 2016
1
BY:TAHER ALI
Operative Intervention in Obstetrics
The best outcome of pregnancy is a healthy mother and baby, ideally
following a normal vaginal delivery with an intact perineum. Sadly, for
many women and babies, the hazards of childbirth are a serious risk.
Indeed, operative intervention to manage these hazards has come to be
regarded as a mainstay of safe motherhood.
Episiotomy:
Definition: Episiotomy is a surgical incision of the perineum made to
increase the diameter of the vulval outlet during childbirth.
It was thought that all primigravidae should receive an episiotomy to
protect the fetal head and the pelvic floor, but researches showed that
high rate of episiotomy was associated with high rate of complications,
which include unsatisfactory anatomical results, increased blood loss,
perineal pain and dyspareunia, so these studies concluded that routine use
of episiotomy should be abandoned.
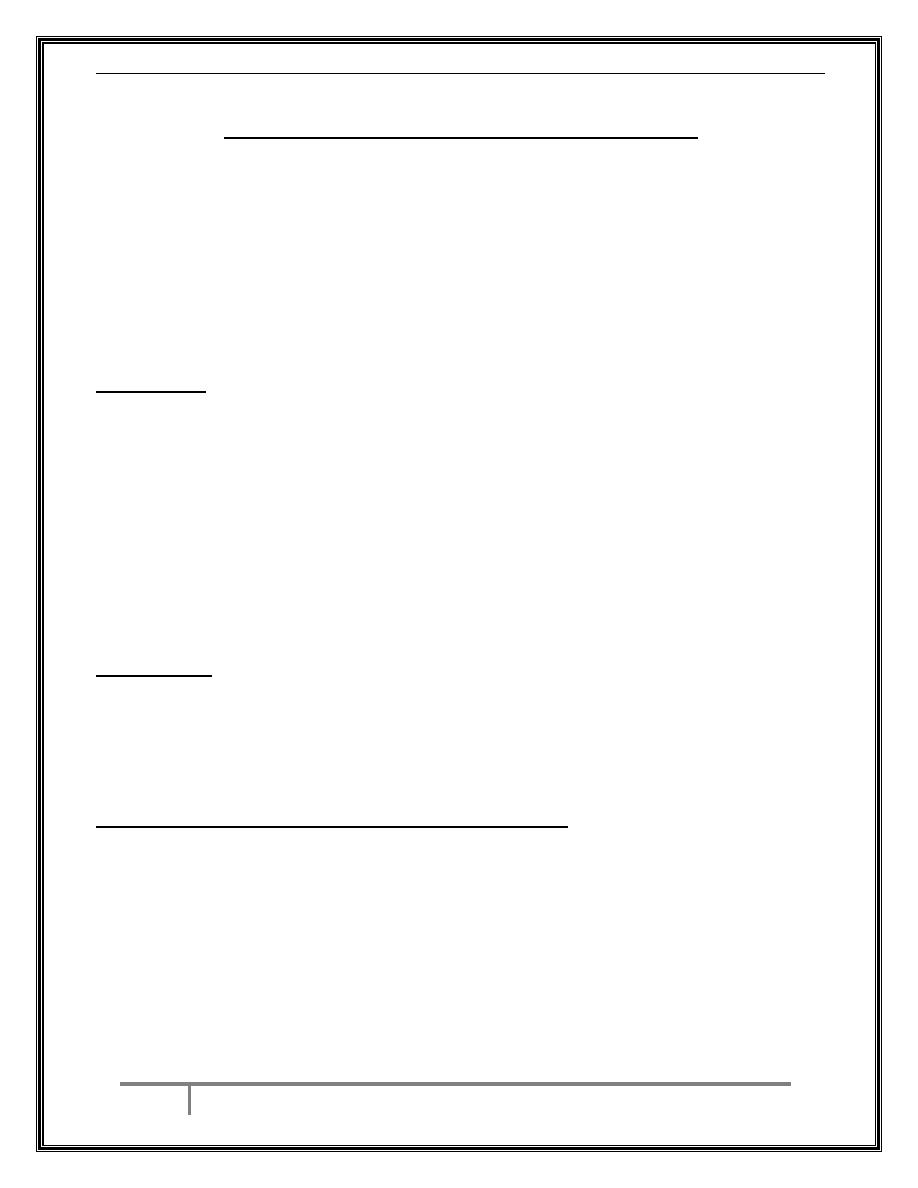
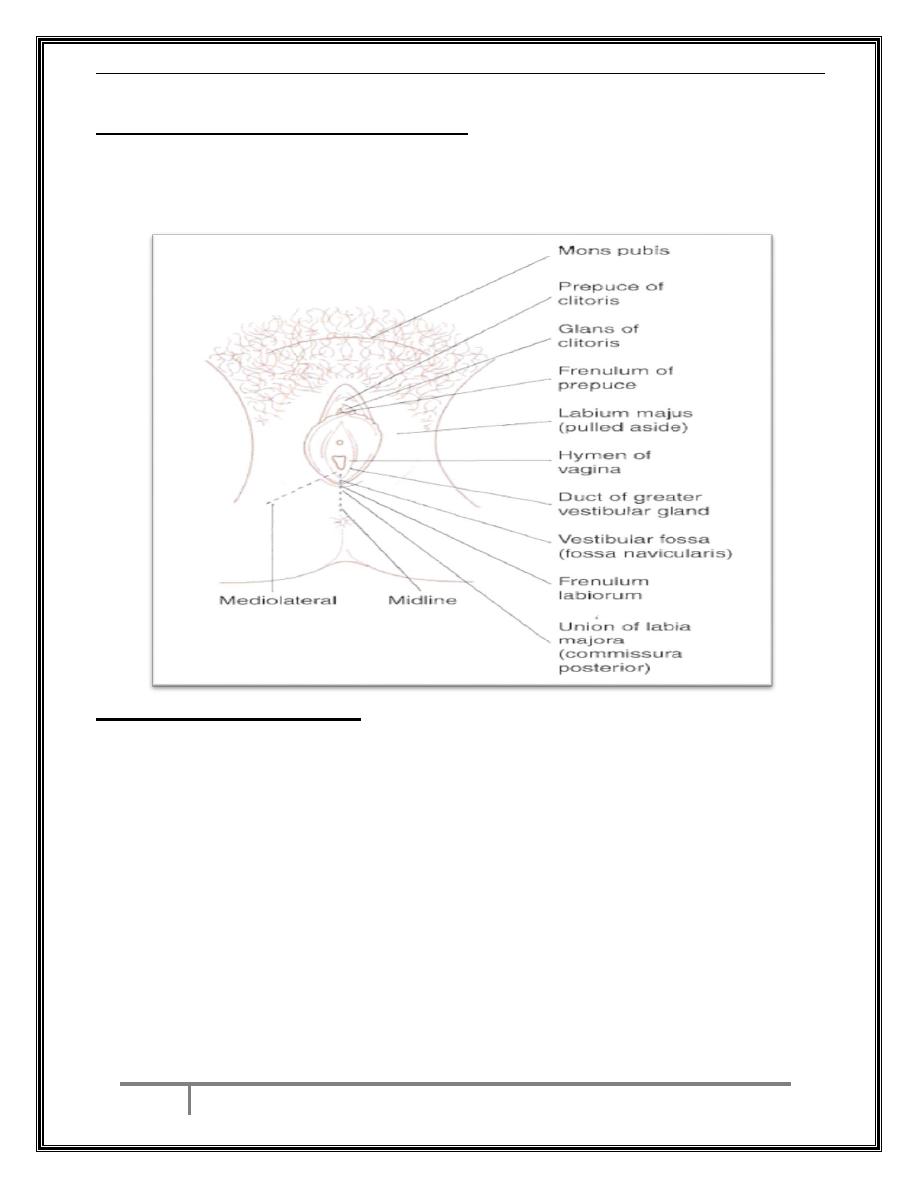
Technique: there are two different techniques that are widely used:
1. Midline: this cut vertically from the fourchette down towards the anus.
2. Medio-lateral: this starts at the fourchette but is then directed diagonally
outwards to avoid the anal sphincter.
The advantages of the midline episiotomy are:
Less blood loss,
It is easier to repair,
The wound heal quicker,
There is less pain in postpartum period,
The incidence of dyspareunia is reduced.
Operative intervention in obstetrics Dr. Raghad March 10, 2016
2
BY:TAHER ALI
Disadvantage of midline episiotomy:
The major disadvantage is that it carries a more than six-fold risk of it
extending to involve the anal sphincter (third/ or fourth-degree perineal
tear).
Indications of episiotomy:
Fetal distress.
Short or inelastic perineum.
Shoulder dystocia.
Fetal malposition, e.g. occipito-posterior.
An instrumental or breech delivery.
Previous pelvic floor surgery.
Operative intervention in obstetrics Dr. Raghad March 10, 2016
3
BY:TAHER ALI
Performing the episiotomy:
Local infiltration with anesthesia (xylocain) is required before
episiotomy.
Large, sharp, straight scissors are the instrument of choice.
It must be performed in one single cut, if it is enlarged by several small
cuts, a zigzag incision line will be produced which is difficult to repair.
It should begin in the midline at the fourchette.
It should not extend too laterally because of risk of damage to Bartholin's
gland without increasing the vulval outlet, and should not be too small
which as it will be insufficient, and may be a weak point from which a
tear may extend.
Prophylactic antibiotic may be indicated.
Complications of episiotomy:
Cuts that begin more laterally are likely to be more painful and more
complicated to suture.
Any episiotomy may extend to cause third-degree tear to anal sphincter.
Heavy bleeding.
Infection.
Dyspareunia.
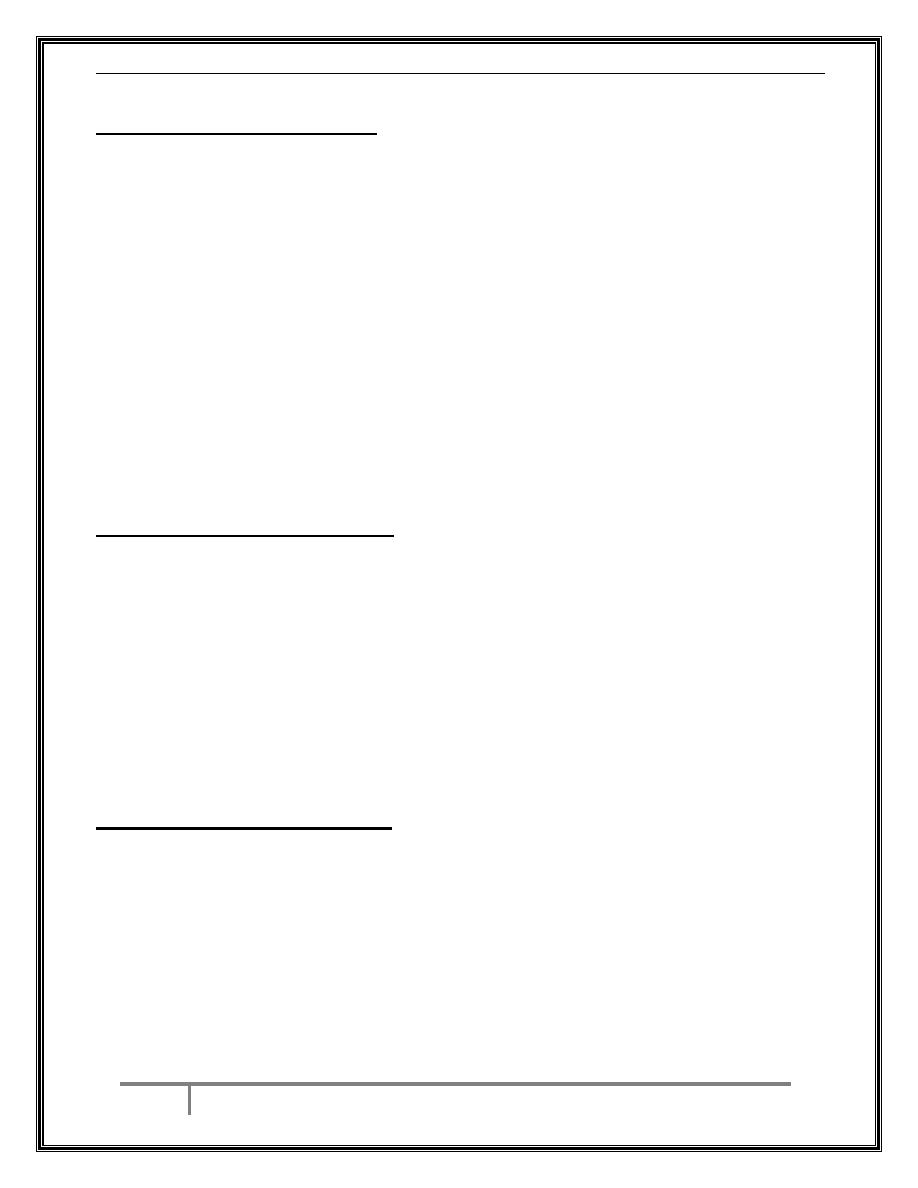
Perineal Tear:
Definition of perineal injury:
First degree: involves skin only.
Second degree: involves perineal muscule and therefore include
episiotomy.
Third degree: second-degree tear with disruption of the anal sphincter,
further subdivided into:
3a: less than 50% of external sphincter thickness torn.
3b: more than 50% of external sphincter thickness torn.
Operative intervention in obstetrics Dr. Raghad March 10, 2016
4
BY:TAHER ALI
3c: internal anal sphincter also torn.
Fourth degree: third-degree tear with torn anal epithelium.
Repair of perineal tears:
* Some first-degree tears will not requiring repair, and others will simply
require one or two interrupted sutures.
* Second degree tears or episiotomy is sutured in layers by opposing the
vaginal epithelium, perineal muscles and skin.
*In third/fourth degree tears disruption of anal sphincter will result in
retraction of the muscle ends, therefore adequate muscle relaxation with
regional or general anesthesia is essential, then repair is done either by
end-to-end technique by approximating the two muscle ends or by
overlap technique. Both techniques have the same outcome. Antibiotic
and laxative agents are prescribed to prevent secondary infection and
constipation.
Complications of perineal tears:
Missing of the apex of a tear or an episiotomy may lead to continued
bleeding or development of paravaginal hematoma.
Deep sutures involving rectal mucosa could lead to fistula formation.
Tight sutures can lead to significant later discomfort.
Operative intervention in obstetrics Dr. Raghad March 10, 2016
5
BY:TAHER ALI
Mal-aligned repair can lead to distortions in the healing and increased
scarring or dyspareunia.
Up to half of women who sustained a third/fourth degree tears develop
bowel symptoms (including fecal incontenance).
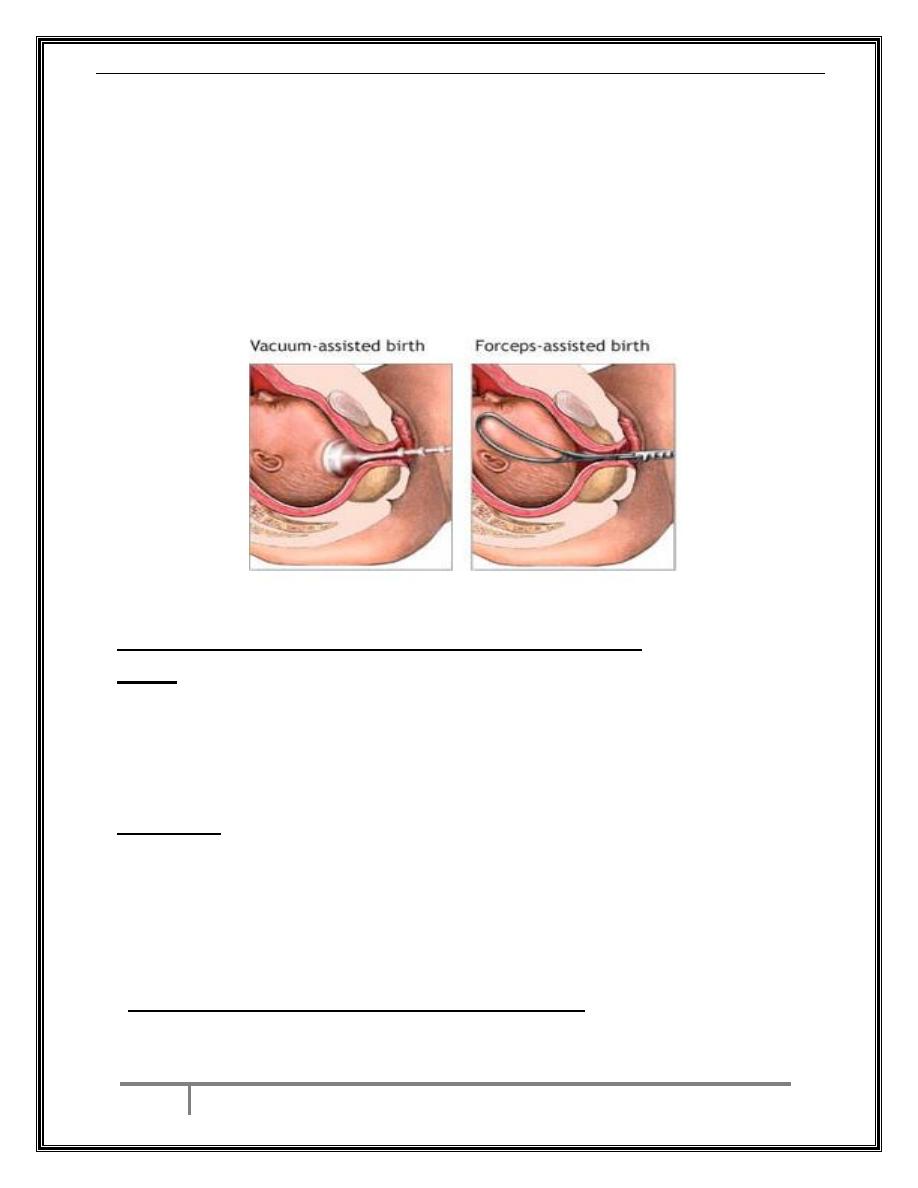
Instrumental Vaginal Delivery:
Definition: Delivery of a baby vaginally using an instrument for
assistance. Instruments include ventouse, and forceps.
Indications for instrumental vaginal delivery:
Fetal:
Fetal head malpositions (occipito-lateral and occipito-posterior).
Fetal distress.
Forceps can be used in delivering the after coming head in vaginal
breech delivery.
Maternal:
Maternal distress, exhaustion or prolongation of the second stage of
labour.
Medically significant conditions like aortic valve disease with
significant
outflow
obstruction;
myasthenia
gravis;
severe
hypertensive disease.
Pre-requisites for any instrumental delivery:
o Confirmed rupture of the membranes.
Operative intervention in obstetrics Dr. Raghad March 10, 2016
6
BY:TAHER ALI
o The cervix must be fully dilated (except in second twin and cord
prolapsed with 9 cm cervical dilatation.
o Vertex presentation with identification of the position.
o Engaged head and the station of the presenting part should be at
+1 and more below the ischial spine.
o Adequate analgesia/anesthesia.
o Empty bladder/ no obstruction below the fetal head (pelvic kidney,
ovarian cyst...)
o Experienced operator.
o An adequately informed and consented patient.
o For forceps in addition the blades of the forceps should be checked
before application for matching and should lock with ease.
Ventouse (vacuum extractor) delivery:
Types of ventouse cup: the metal cups most widely used are the "bird
modification" one. These have a central traction chain and a separate
vacuum pipe. Different sizes present (4, 5, and 6 cm sizes) with size of 5
may be suitable for most infants. Recently, a silicone-rubber cup have
been developed which is associated with less fetal complication as
compared with rigid cups and can be used in straight forward occipito-
anterior position, while rigid cup is used for malposition and complicated
occipito-anterior positions.
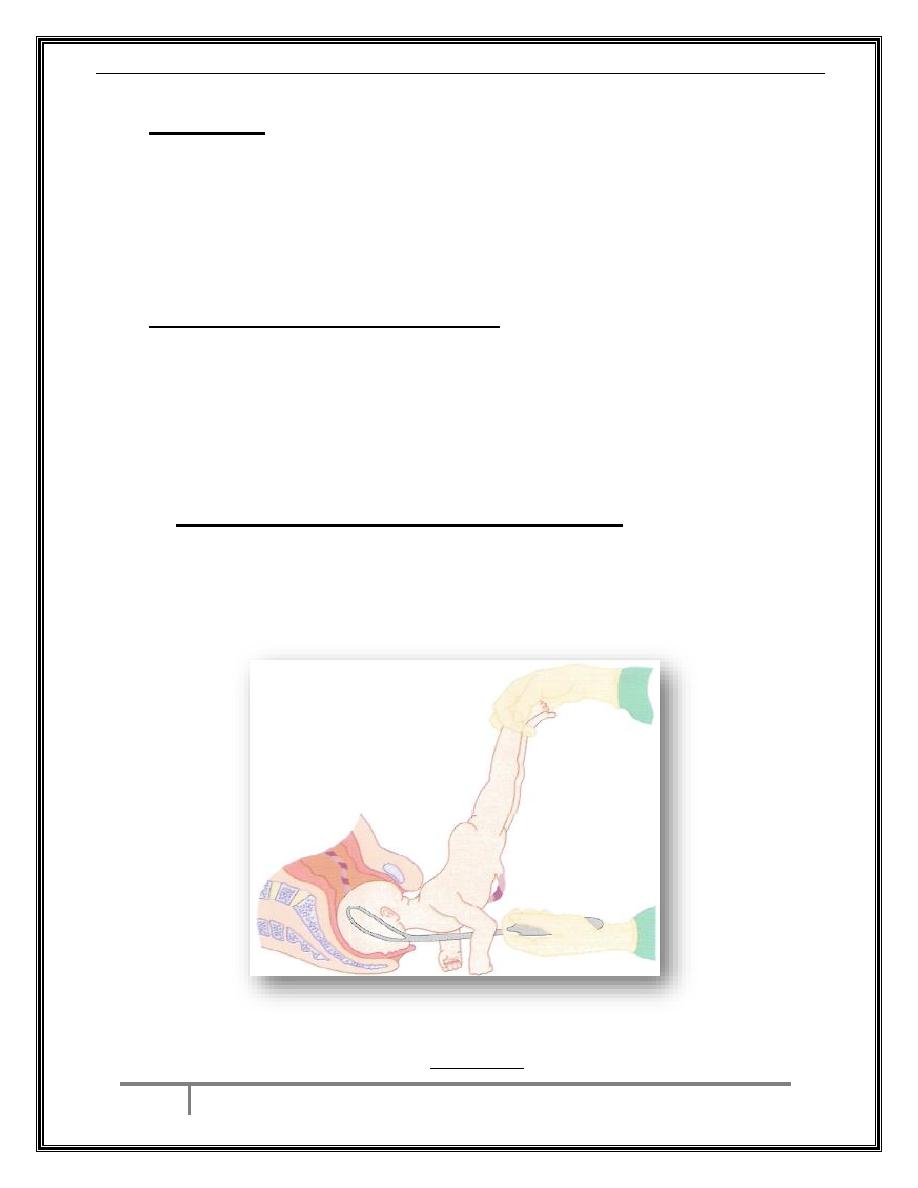
Technique:
In lithotomy position, full dilation of cervix, full engagement of head, ,
good uterine contraction, co-operation of the patient with adequate
infiltration of perineum by xylocain if an episiotomy is planned, the
appropriate cup should be chosen and connected to pump, the cup is
gently inserted and applied on the saggital suture of the fetal head 3cm
anterior to the posterior fontanelle (flexion point) by one hand with other
hand parts the labia, then increase suction to 0.2 kg/cm
2
then recheck that
no maternal tissue is caught under the cup edge. When this is confirmed
Operative intervention in obstetrics Dr. Raghad March 10, 2016
7
BY:TAHER ALI
the suction then can be increased to (0.6-0.8)kg/cm
2
. Traction should be
applied along the pelvic axis (downwards at 45
ₒ
) for the duration of
contraction.
The delivery should be completed within 15 minutes of application.
The head, not just the scalp, should descend with each pull.
The cup should be reapplied no more than twice.
Forceps should not be triad if failure of delivery by ventouse has
occurred.
Avoid rotating the head as it results in severe scalp lacerations.
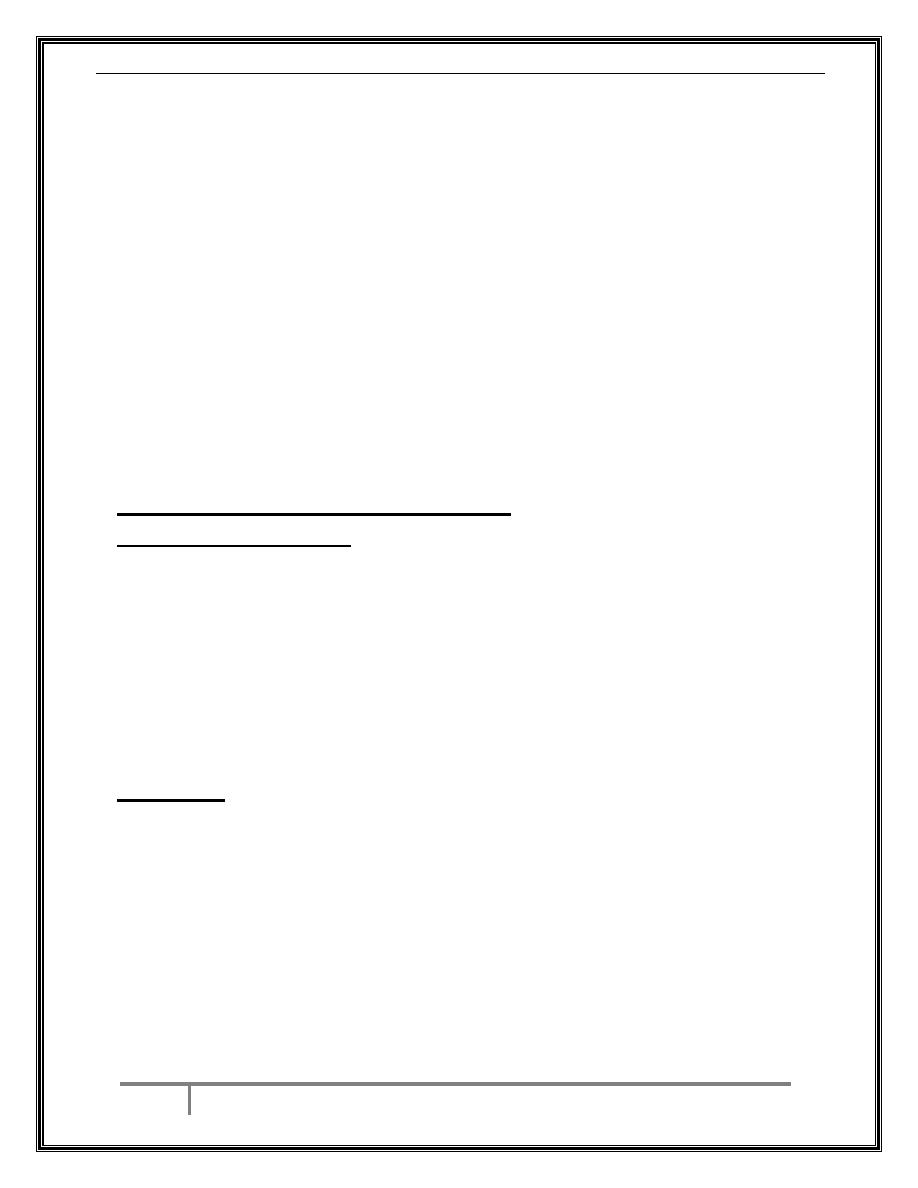
Traction down the pelvic axis
Contraindications of ventouse:
Face presentation.
Marked active bleeding from a fetal blood sampling site.
Breech presentation.
Gestation less than 34 weeks.
Operative intervention in obstetrics Dr. Raghad March 10, 2016
8
BY:TAHER ALI
Complications of ventouse delivery:
Trauma to genital tract (laceration to vagina and cervix) leading to
severe hemorrhage.
Caput succidanium (edematous skin bump).
Cephalhematoma (sub-periosteal bleed).
Serious intracranial injuries and cerebral palsy may occur if
multiple attempts at delivery are made with a variety of
instruments.
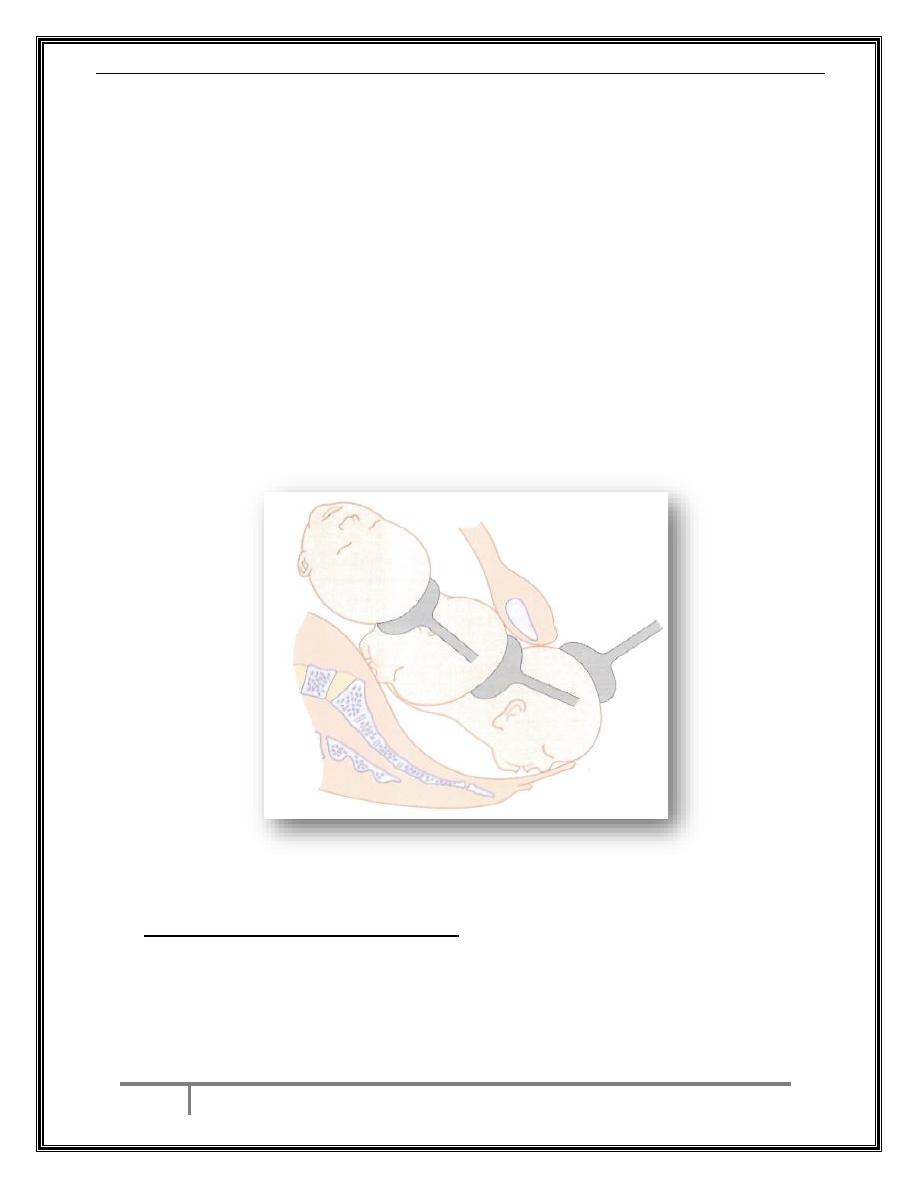
Forceps:
Types of forceps:
1. Classical forceps: e.g. Simpson forceps with longer cephalic curve
(used for molded head), and Wrigley forceps with shorter cephalic
curve (for unmolded head).
2. Special forceps: e.g. Piper forceps designed for after coming head
in breech delivery, and Kielland forceps which lack a pelvic curve for
rotational delivery at any station, also can be used for after coming
head of breech delivery.
The upper one is Simpson forceps the lower one is Kielland forceps
Operative intervention in obstetrics Dr. Raghad March 10, 2016
9
BY:TAHER ALI
Technique: the head should be fully engaged, cervix is fully dilated,
and position of the head is carefully noted, evacuation of bladder is
advised, episiotomy is required, the blades of the forceps should
matched, the left handed blade is inserted first (downwards then
inwards) guided by the right hand. The right handed blade is inserted
in the same procedure, and then the blade must lock easily and should
not be forced to close. The first pull is downwards and then upwards.
Complications of forceps delivery:
Traumatic vaginal and uterine injuries can result from undue
traction and rotatory forceps which may result in spiral vaginal
laceration or even bladder injury.
Third/fourth degree perineal tears with fecal incontinence.
Serious injuries to the baby can occur when excessive force is
used or when multiple attempts are made.
Indications for forceps instead of ventouse:
Face presentation.
Bleeding from fetal blood sampling site.
After-coming head of the breech.
Delivery before 34 weeks' gestation.
Forceps used for after coming head in breech vaginal delivery
THE END
