Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
1
Diseases Of Urinary System In
Pregnancy
Urinary tract infection :
UTI is defined as the presence of at least 100,000 organisms per
milliliter of urine in an asymptomatic patient, or as more than 100
organisms/mL of urine with accompanying pyuria (> 7 white blood
cells [WBCs]/mL) in asymptomatic patient. A diagnosis of UTI
should be supported by a positive culture for a uropathogen,
particularly in patients with vague symptoms
Pathophysiology :
Infections result from ascending colonization of the urinary tract,
primarily by existing vaginal, perineal, and fecal flora. Various
maternal physiologic and anatomic factors predispose to
ascending infection. Such factors include urinary retention caused
by the weight of the enlarging uterus and urinary stasis due to
progesterone-induced ureteral smooth muscle relaxation. Blood-
volume expansion is accompanied by increases in the glomerular
filtration rate and urinary output.
Loss of ureteral tone combined with increased urinary tract
volume results in urinary stasis, which can lead to dilatation of the
ureters, renal pelvis, and calyces. Urinary stasis and the presence
of vesicoureteral reflux predispose some women to upper urinary
tract infections (UTIs) and
Calyceal and ureteral dilatation are more common on the right
side; in 86% of cases, the dilatation is localized to the right. The
degree of calyceal dilatation is also more pronounced on the right
than the left (average 15 mm vs 5 mm). This dilatation appears to
begin by about 10 weeks’ gestation and worsens throughout
pregnancy.
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
2
Glycosuria and an increase in levels of urinary amino acids
(aminoaciduria) during pregnancy are additional factors that lead
to UTI.
Etiology :
E coli is the most common cause of urinary tract infection (UTI),
accounting for approximately 80-90% of cases. It originates from
fecal flora colonizing the periurethral area, causing an ascending
infection. Other pathogens include the following:
Klebsiella pneumoniae (5%)
Proteus mirabilis (5%)
Enterobacter species (3%)
Staphylococcus saprophyticus (2%)
Group B beta-hemolytic Streptococcus (GBS; 1%)
Proteus species (2%)
Classification of UTI’s
Clinical:
Asymptomatic (8%)
Symptomatic (1-2%)
Anatomical:
Lower tract dis: asymptomatic bacteriuria and acute cystitis
Upper tract dis: acute pyelonephritis
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
3
Asymptomatic bacteriuria :
IT is commonly defined as the presence of more than 100,000
organisms/mL in 2 consecutive urine samples in the
absence of declared symptoms. Untreated asymptomatic
bacteriuria is a risk factor for acute cystitis (40%) and
pyelonephritis (25-30%) in pregnancy.
Acute cystitis :
Acute cystitis involves only the lower urinary tract; it is
characterized by inflammation of the bladder as a result of
bacterial or nonbacterial causes (eg, radiation or viral infection).
Acute cystitis develops in approximately 1% of pregnant patients,
of whom 60% have a negative result on initial screening. Signs and
symptoms include hematuria, dysuria, suprapubic discomfort,
frequency, urgency, and nocturia. These symptoms are often
difficult to distinguish from those due to pregnancy itself.
Acute pyelonephritis :
Pyelonephritis is the most common urinary tract complication in
pregnant women, occurring in approximately 2% of all
pregnancies. Acute pyelonephritis is characterized by fever, flank
pain, and tenderness in addition to significant bacteriuria. Other
symptoms may include nausea, vomiting, frequency, urgency, and
dysuria. Furthermore, women with additional risk factors (eg,
immunosuppression, diabetes,
, recurrent or persistent UTIs before pregnancy) are at an
increased risk for a complicated UTI.
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
4
Complications :
The primary complication of bacteriuria during pregnancy is
cystitis,. Other complications may include the following:
• Perinephric cellulitis and abscess
•
• Renal dysfunction (usually transient, but as many as 25% of
pregnant women with pyelonephritis have a decreased
glomerular filtration rate)
• Hematologic dysfunction
• Hypoxic fetal events due to maternal complications of
infection that lead to hypoperfusion of the placenta
• Premature delivery leading to increased infant morbidity and
mortality
•
acute respiratory distress syndrome
Diagnosis(history , examination and laboratory)
• Laboratory studies can include blood studies and urine
studies, including culture, urinalysis, dipstick testing.
• Imaging tests can include ultrasonography and intravenous
pyelography.
• Complete blood count (CBC)
• Serum electrolytes
• Blood urea nitrogen (BUN)
• Serum creatinine
Treatment of asymptomatic bacteruria & acute
cystitis
:
Antibiotic therapy
• Oral antibiotics are the treatment of choice for
asymptomatic bacteriuria and cystitis. Appropriate oral
regimens include the following:
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
5
• Cephalexin 500 mg 4 times daily
• Ampicillin 500 mg 4 times daily
• Nitrofurantoin 100 mg twice daily
• Sulfisoxazole 1 g 4 times daily
•
10-14 days of treatment is usually recommended to
eradicate the offending bacteria.
Treatment of pyelonephritis
Hospital admission and intravenous (IV) administration of
cephalosporins or penicillins. IV fluids must be administered with
caution. Patients with pyelonephritis can become dehydrated
because of nausea and vomiting and need IV hydration. However,
they are at high risk for the development of pulmonary edema
and acute respiratory distress syndrome (ARDS).
Fever should be managed with antipyretics (preferably,
acetaminophen) and nausea and vomiting with antiemetics.
Chronic Renal disease
Women with chronic kidney disease are less able to make the
renal adaptations necessary for a healthy pregnancy and
pregnancy in women with renal disease therefore requires
increased maternal and fetal surveillance.
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
6
Pre-pregnancy counseling :
• Pre-pregnancy counselling is recommended in all women
with chronic kidney disease and they should be made aware
of the risks to the fetus and to their long-term renal function
before conception.
• Pre-pregnancy counselling discussion should include:
Safe contraception until pregnancy advised
Fertility issues if indicated
Genetic counselling if inherited disorder
Risks to mother and fetus during pregnancy
Avoid known teratogens and contraindicated drugs
Management of antihypertensives :
Low-dose aspirin for most pregnancies
Need for anticoagulation once pregnant in some conditions
Need for compliance with strict surveillance
Likelihood of prolonged admission or early delivery
Possibility of accelerated decline in maternal renal function
Need for postpartum follow up.
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
7
Chronic kidney disease :
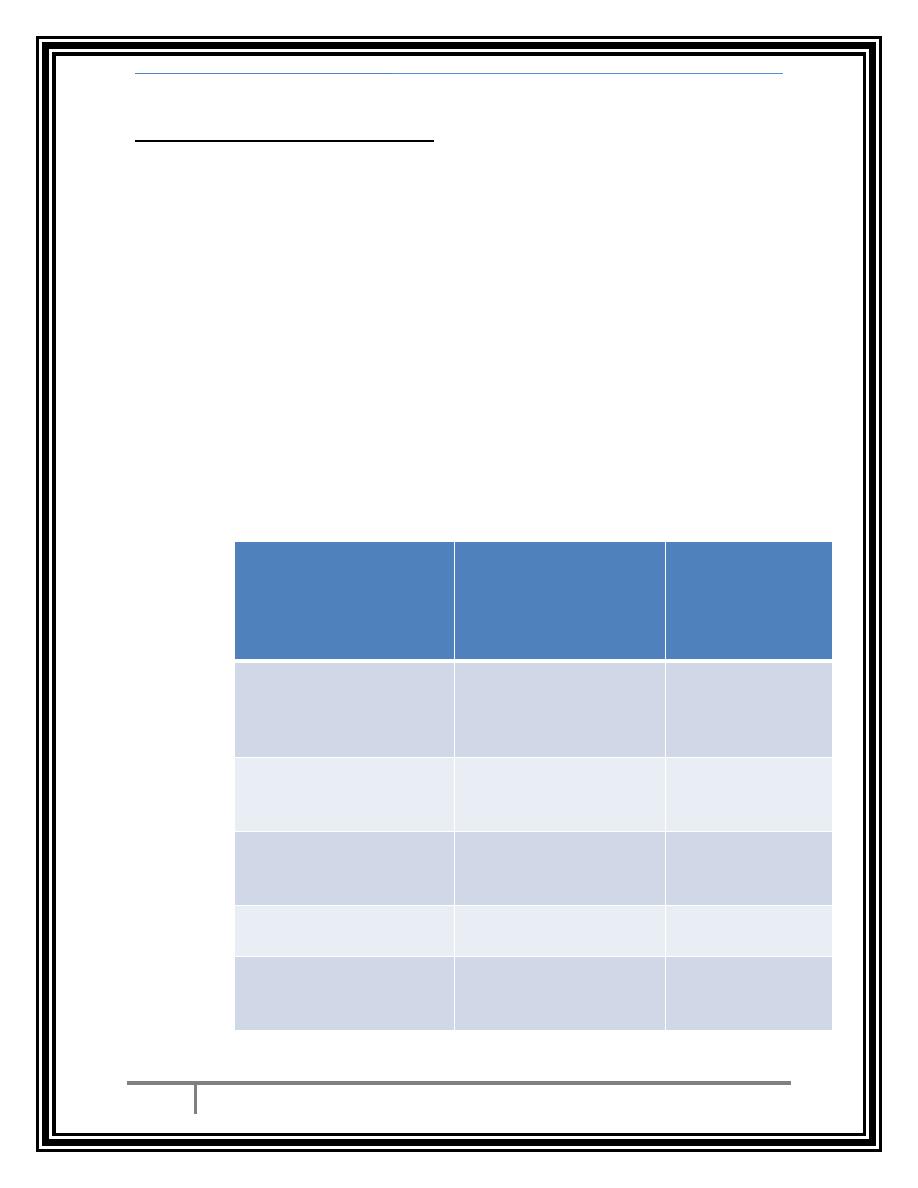
• Chronic kidney disease (CKD) is classified into five stages
based on the level of renal function. Stages 1 and 2 affect
around 3 per cent of women of childbearing age (20–39),
and while stages 3–5 affect 1 in 150 women in this age
group, pregnancy in these women is less common. Some
women are found to have CKD for the first time in their
pregnancy, and pregnancy can unmask previously
unrecognized renal disease.
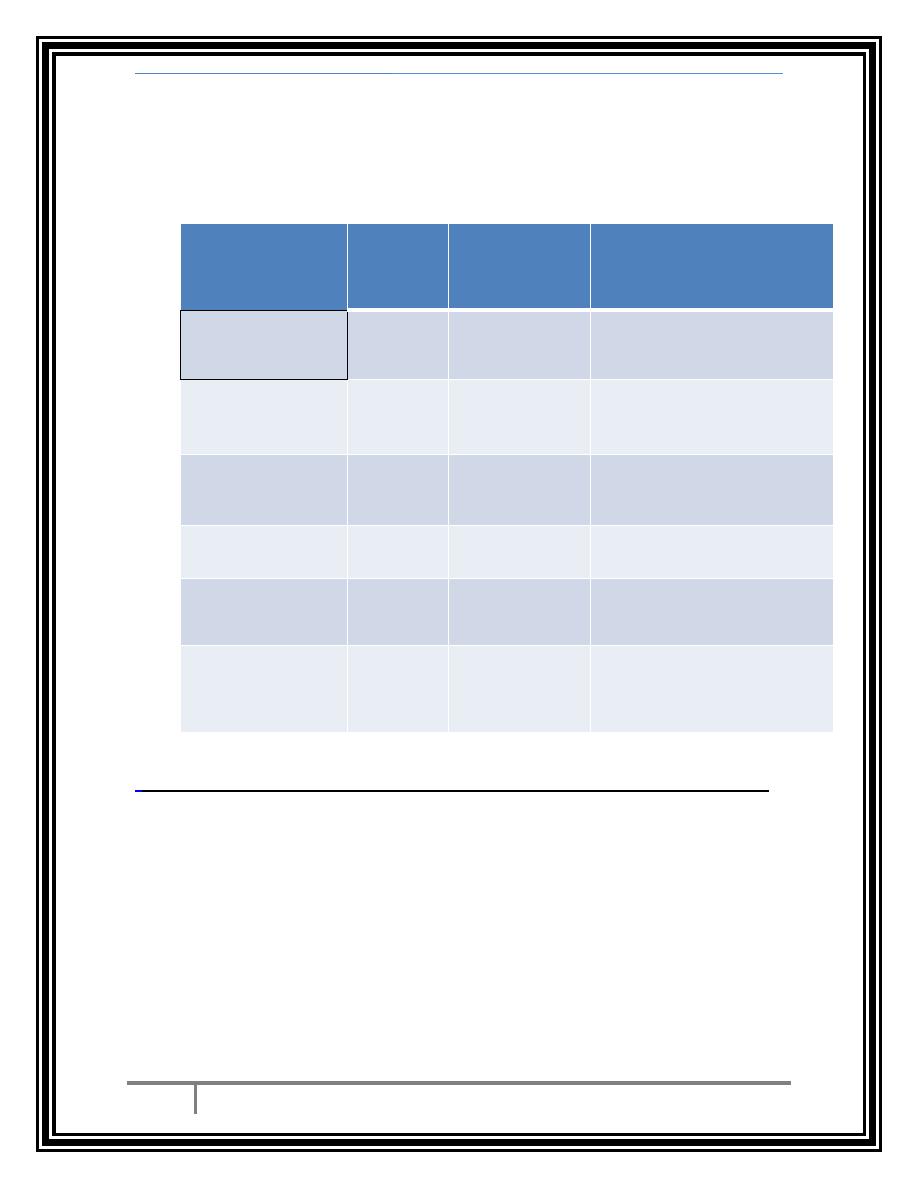
Stages of chronic kidney disease
stage
Description
Estimated GFR
(mL/min/1.73m2)
1
Kidney damage with
normal/raised GFR
>90
2
Kidney damage with mildly
low GFR
60-89
3
Moderately low GFR
30-59
4
Severely low GFR
15-29
5
Kidney failure
<15 or dialysis
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
8
Effect of pregnancy on CKD :
• Women with CKD stages 1–2 have mild renal dysfunction
and usually have an uneventful pregnancy and good renal
outcome. Pregnancy with a serum creatinine < 110 mmol/L,
minimal proteinuria (<1 g/24 hours), and absent or well-
controlled hypertension pre-pregnancy has been shown to
have little or no adverse effect on long-term maternal renal
function.
• Women with moderate to severe disease (stages 3–5) are at
highest risk of complications during pregnancy and of an
accelerated decline in their renal function. Pre-existing
hypertension and proteinuria greatly increase the risk. If
pre-eclampsia develops, maternal renal function often
deteriorates further, but any other additional complications,
such as postpartum haemorrhage or use of non-steroidal
anti-inflammatory drugs, can critically threaten maternal
renal function.
Effect of CKD on pregnancy outcome :
• Pregnancies in mothers with CKD have increased risks of
preterm delivery, delivery by Caesarean section (40 per
cent) and FGR (increased two-fold). Diastolic blood pressure
has been suggested as the greatest risk factor for fetal
death, but overall fetal survival is reported at around 95 per
cent. The risk of adverse pregnancy outcome correlates with
the degree of renal dysfunction.
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
9
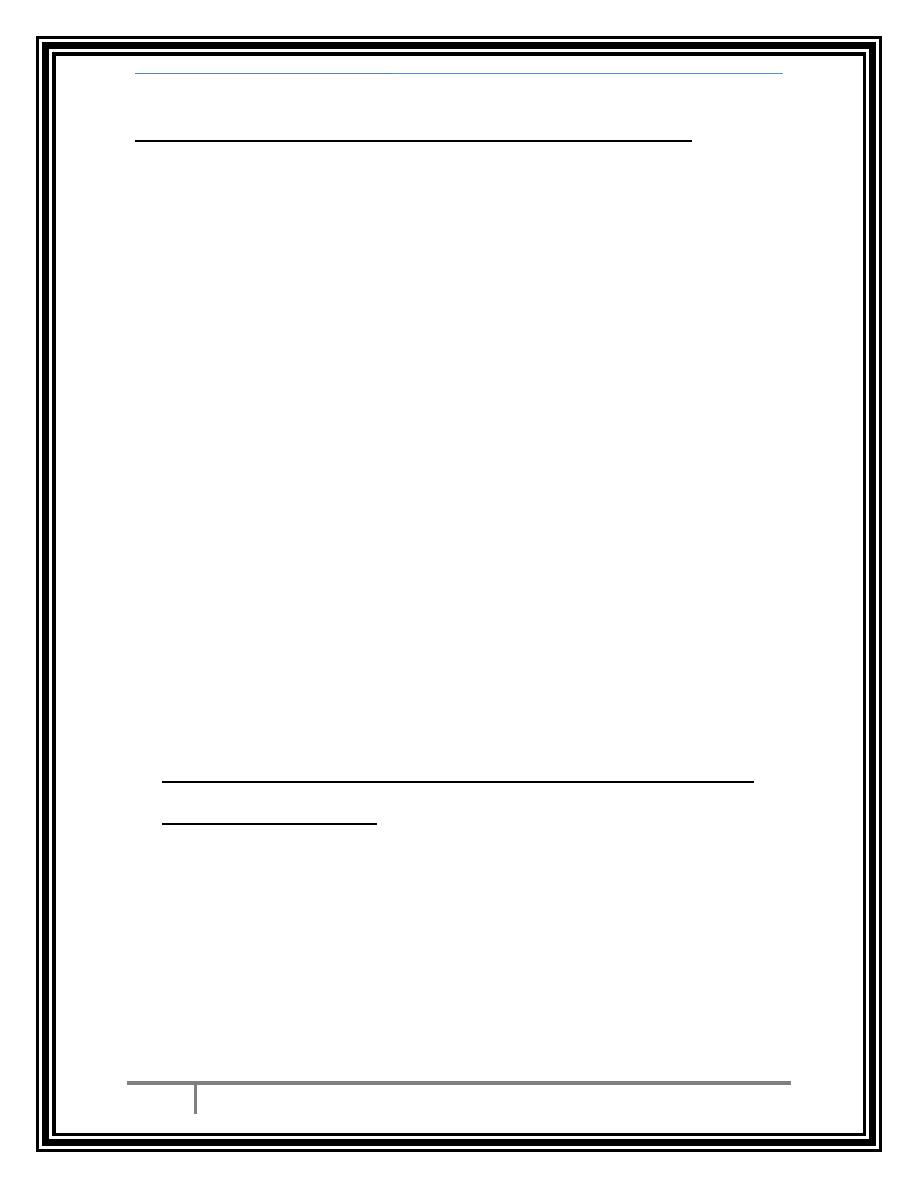
Estimated effects of renal function on pregnancy
outcome and maternal renal function
Mean pre-
pregnancy
value
serum
creatinine
<125
125–180
>180
Fetal growth
restriction (%)
25
40
65
Preterm delivery
(%)
30
60
>90
Pre-eclampsia (%)
22
40
60
Loss of <25% renal
function
0
20
50
End-stage renal
failure after 1 year
(%)
0
2
35
Monitoring of patients with CKD during pregnancy
• Blood pressure
• Renal function
• creatinine
• Urine
• infection
• proteinuria
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
10
• Full blood count
• haemoglobin
• ferritin
• Renal ultrasound
• Fetal ultrasound to asses :
Anatomy
uterine artery Doppler 20–24 weeks
growth.
Dialysis :
• The incidence of pregnancy on dialysis (stage 5 CKD) is
increasing. Dialysis must be adjusted to allow for the
physiological changes of pregnancy (plasma volume, fluid
retention, electrolytes), and haemodialysis is usually more
effective then peritoneal dialysis in achieving this.
Complication :
Complications include preterm delivery, polyhydramnios (30–60
per cent), pre-eclampsia (40–80 per cent) and Caesarean delivery
(50 per cent). If conceived on dialysis, 50 per cent of infants
survive, but pregnancy before dialysis has a better outcome.
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
11
Pregnancy in women with renal transplants :
-Women with end-stage kidney disease have hypothalamic-
gonadal dysfunction and infertility, so conception is rare.
Female fertility returns rapidly after renal transplantation and
it is estimated that 2–10 per cent of female recipients conceive.
-if pregnancies progressing beyond the third trimester, the
vast majority (>90 per cent) result in a successful pregnancy
outcome. Most transplantation centres advise that
conception is safe after the second post-transplantation
year, provided the graft is functioning well and no rejection
episodes occur in the year before conception.
-All pregnancies in transplant recipients are high risk and
should be managed by a multidisciplinary team. Lower
immunosuppressive steroid dosage, longer time since
transplantation and better graft function with absence of
chronic rejection, are all associated with better maternal
outcomes.
-Complications of pregnancy in renal transplant
patients include :
high rates of pregnancy-induced hypertension (30–50 per
cent), preterm delivery (40–60 per cent), pre-eclampsia (10–40
per cent) and urinary tract infection (20–40 per cent).
Diagnosing pre-eclampsia can be difficult due to the normal
rise in blood pressure after 20 weeks and the presence of pre-
existing proteinuria.
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
12
-The risk of acute rejection in pregnancy is estimated at 2–10
per cent, and allograft dysfunction may also be difficult to
detect during pregnancy. Vaginal delivery is safe, with
Caesarean section considered for the usual obstetric
indications. From 5 to 15 per cent of women have worse graft
function after pregnancy.
Monitoring of renal transplant patients during
pregnancy :
• Renal function
• blood pressure
• creatinine
• proteinuria
• Drug levels
• Fetal growth
• If renal function declines, exclude:
a)Obstruction.
b)Infection.
c)Rejection.
Khafajy Renal disease
-
Dr Shaimaa Al
March 6, 2016
13
-Predictors of fetal outcome include :
a) pre-pregnancy maternal hypertension, diabetes mellitus and
maternal drug treatment. Many women have concerns about
the immunosuppressive drugs used post-transplantation,and
since immunosuppressive medications must be continued
throughout pregnancy, the fetus is inevitably exposed to
potential fetotoxic and teratogenic agents throughout
development.
b) The actual effects of medications on growth and
development are difficult to determine and may not be
obvious at birth.
c) It is also difficult to assess the relative effect of
immunosuppressive agents. Prednisolone, azathioprine,
cyclosporin and tacrolimus are considered safe.
…THE END…
BY :
TAHER ALI TAHER
