بسم الله الرحمن الرحيم
THE RECTUM
by Dr. Mohammedsalih A. Ali
Embryology and Anatomy
GIT develops at 4th week of gestation- it derived from the endoderm and divided into three segments: foregut, midgut, and hindgut.
-Both midgut and hindgut contribute to the colon, rectum, and anus
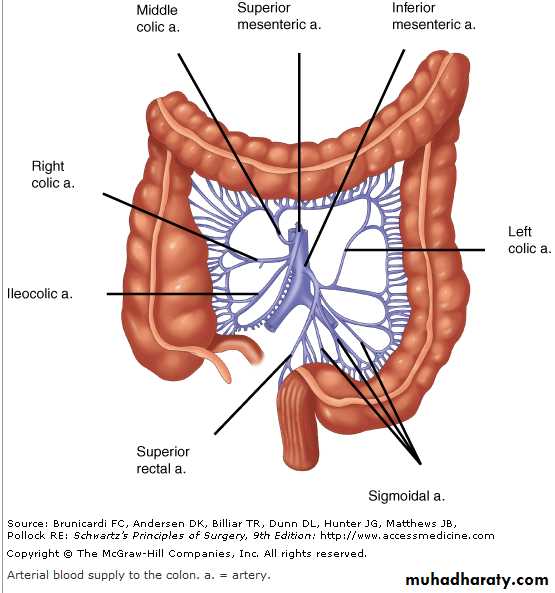
-The midgut develops into the small intestine, ascending colon, and proximal transverse colon, and receives blood supply from the superior mesenteric artery
.
The hindgut develops into
1- the distal transverse colon2- descending colon
3- rectum
4- proximal anus
all of which receive their blood supply from the inferior mesenteric artery
Anatomy
-The large intestine extends from the ileocecal valve to the anus.
- It is divided anatomically and functionally into the colon, rectum, and anal canal.
- The wall of the colon and rectum consist of 4-layers:
1- mucosa
2- submucosa
3- muscular layer
- inner circular
- outer longitudinal muscle, the outer longitudinal muscle is separated into three teniae coli except at rectum and appendix is circumferential
4-serosa.
The intraperitoneal colon and proximal one third of the rectum are covered by serosa;
- the middle and lower rectum lack serosa.
Colon and rectum Lymphatic Drainage
- The lymphatic drainage of the colon originates in the muscularis mucosa.- Lymphatic vessels and lymph nodes follow the regional arteries. it divided to 4 group
1- epicolic Lymph nodes are found on the bowel wall
2- paracolic along the inner margin of the bowel adjacent to the arterial arcades
3-intermediate around the named mesenteric vessels
4- main at the origin of the superior and inferior mesenteric arteries , superior or inferior mesenteric lymph node
Colon Nerve Supply
The colon is innervated by both sympathetic (inhibitory) and parasympathetic (stimulatory) nerves, which parallel to the course of the arteries.
- Sympathetic nerves arise from T6-T12 and L1-L3.
- The parasympathetic innervations to the right and transverse colon is from the vagus nerve
- the parasympathetic nerves to the left colon arise from sacral nerves S2-S4 to form the nervi erigentes.
The rectum
- Rectum start at rectosigmoid junction , which is at the level of the sacral promontory and at this point the three teniae coli of the colon coalesce to form the outer longitudinal smooth muscle of rectum-The rectum is approximately 12 to 15 cm in length.
-Three distinct submucosal folds, the Houston`s valves extend into the rectal lumen , the upper and lower convex to right and middle convex to left
- the rectum is divided to three part
1-upper third covered anteriorly and laterally by peritoneum
2- middle third covered only anteriorly by peritoneum
3- lower third is exteraperitoneal
The lower part of the rectum separated from surrounding organ by fascia
Posteriorly- At lower two sacrum and coccyx rectosacral fascia ( Waldeyer's fascia) is dense fascia is between the rectum and sacrum it separate the rectum from presacral venous plexus and pelvic nerves, and act as barrier for spread of tumor
anteriorly
Denonvilliers' fascia separates the rectum from the prostate and seminal vesicles in men and from the vagina in women
Laterally
- The lateral ligaments from rectum to lateral wall of pelvis , it support the lower rectum
Anorectal Vascular Supply
1-The superior rectal artery arises from the terminal branch of the inferior mesenteric artery and supplies the upper rectum.
2-The middle rectal artery arises from the internal iliac artery
3-The inferior rectal artery arises from the internal pudendal artery, which is a branch of the internal iliac artery.
A rich network of collaterals between these arteries
The venous drainage of the rectum parallels the arterial supply.
1-The superior rectal vein drains into the portal system via the inferior mesenteric vein.2-The middle rectal vein drains into the internal iliac vein.
3-The inferior rectal vein drains into the internal pudendal vein, and subsequently into the internal iliac vein.
A submucosal plexus deep to Morgagni columns forms the hemorrhoidal plexus and Anorectum drains into all three veins
2/28/2013
13anal and rectal examination
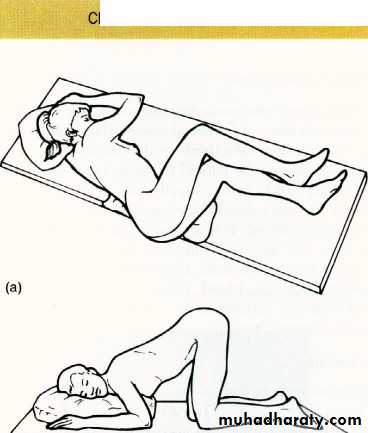
Position:- the left-lateral (Sims) position
- the knee-elbow position
- the lithotomy position:
a- left lateral position
b- elbow- knee positionInspection:-
- With the buttocks opened, the anus is inspected. Note is made of any lesions,e.g. inflammatory skin changes,
hemorrhoids,
fissure ('sentinel pile),
fistula
mass , tumor
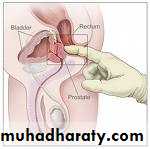
Digital examination
with the index finger, to palpate forIntraluminal-
- abnormal: polyp or carcinoma
- normal: sphincter muscles and anorectal angle
Intramural-
- abnormal: leiomyoma or carcinoma
- Extramural,
for prostate any abnormal mass at Douglas pouch
Digital examination
investigation
-Proctoscopy- regid sigmoidoscope
-Fexible sigmodoscope
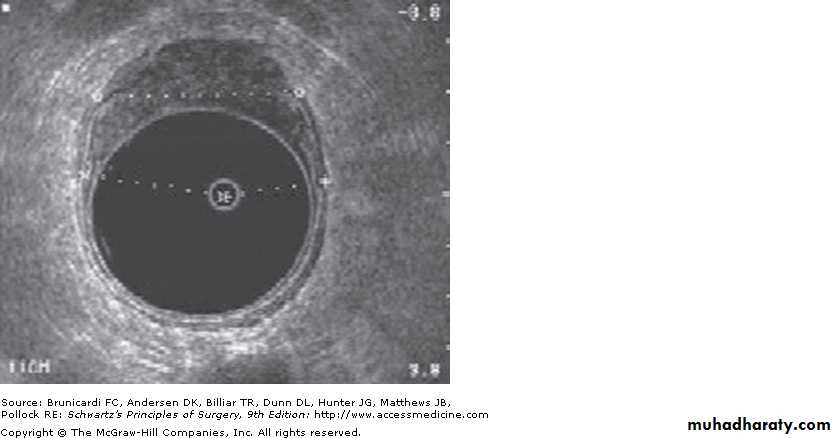
- endoscopic ultrasound
- ultra sound of pelvis
- Ct-scan, MRI
- anorectal manometry,
defecography -
Flexible sigmoidoscopy
rectum
Rectal valve
rectum
• Symptoms:
• 1-Bleeding: This demands at least digital examination at any age.• 2- Altered bowel habit: constipation ,or diarrhea
• Early morning stool frequency ('spurious diarrhea') is a symptom of rectal carcinoma, while blood-stained frequent loose stools characteristic of the inflammatory diseases.
• 3-Discharge: Mucus and pus are associated with rectal pathology.
• 4-Tenesmus: desire to pass stool but there is noting
• often described by the patient as '1 feel I want to go but nothing happens'; this is normally an ominous symptom of rectal cancer.
• .
• 5-Prolapse: protrusion of rectum through anal orifice This usually indicates either mucosal (partial) or full thickness (complete) rectal wall descent.
• 6-Pruritis: This may be secondary to a rectal discharge.
• 7-Loss of weight: This usually indicates serious or advanced disease, e.g. metastases
Rectal injury
Causes:.
1- falling in a sitting posture on to a spiked or blunt pointed object it also cause anal injury.
2-due to complication of labor. the fetal head during childbirth, especially forceps-assisted cause perineal tear which extend to the rectum
3-During the administration of an enema by a syringe.
4- by rigid sigmoidoscopy, usually when examining a patient suffering from ulcerative proctocolitis or amoebic dysentery.
- perforation is usually anteriorly through the rectosigmoid junctional zone.
5- Split perineum’. A lacerated wound of the perineum, involving the anal canal, is an occasional pillion-riding accident,
6-Compressed-air rupture (as a result of joke).
7-Insertion of a foreign body
Foreign bodies in the rectum
Treatment
- good clinical examination.- investigation such as proctoscope, sigmoidoscope if possible ,ultra-sound and ct-scan
A-If there is intraperitorteal rupture of the rectum
1- laparotomy
2- perforation is closed with sutures
3- defunctioning colostomy is constructed in the left iliac fossa.
4- antibiotic
B- If the rectal injury is below the pelvic floor, extraperitoneal
1- do wide drainage from below (pre-sacral drainage)2- protective colostomy is advisable some time.
3-Care must be taken to preserve sphincter function during the debridement of the perineal wounds.
4-antibiotic cover
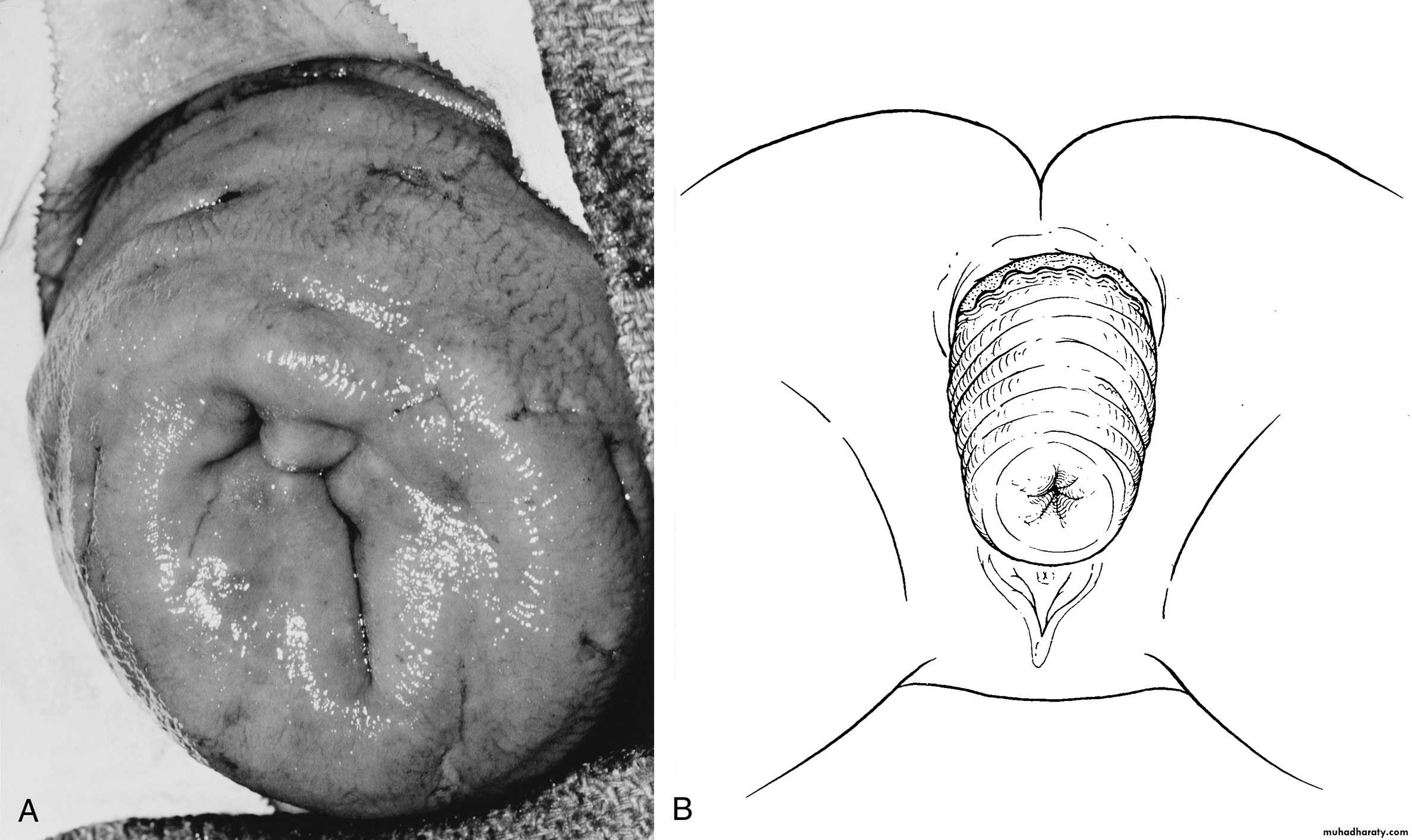
Rectal Prolapse
Rectal prolapse: protrusion of the rectum outside the anus.Types:
Partial prolapse: The mucous membrane and submucosa of the rectum protrude outside the anus for approximately 1-4 cm.
Complete prolapse: full thickness of the rectum protrudes outside the anus.
Aetiology
Partial prolapse
The condition occurs most often at the extremes of life.
A--In children it is common between 1 and 3 years of age and is probably result of combination of factors
1-undeveloped sacral curve ,the anus and rectum forming vertical tube.
2-straining
- at defecation due to prolonged diarrhea
- at severe cough in case of whooping cough
3- loss of weight.
which result in loss of supporting pararectal and ischiorectal fat
.
B-In elderly people it due to
1-usually associated with third-degree haemorrhoids2-in the male, straining in case of urethral stricture
3- atony of sphincter mechanism
4- due to injury of anal sphincter in case of operation for fistula in ano or perineal tear in labor
clinical feature
Symptom1- protrusion of the mucosa of the rectum on straining
it reduce spontaneously or digitally
In partial prolapse the protrusion is less than 5-cm but in complete is more
2- mucous discharge
3- fecal incontinence
4- feature of complication of irreducibility such as ulceration, gangrene
By the examination of partial prolapse between the thumb and finger ,you feel no more than two layers of the mucosa.
but in case of complete prolapse you feel much more thicker tissue which is two layers of the rectal wall
Differential diagnosis
- prolapsed hemorrhoid- prolapsed polyp
- prolapsed intussusceptions
Treatment of partial collapse
In children
1-avoidence of constipation and straining
2-improve nutritional status
3-manual reduction of prolapse and strapping the buttock
4-sub mucosal injection of 5% phenol in almond oil for resistance cases
5- surgery rarely indicated (Thiersch`s operation)
In adults:
-sub mucosal injection of 5% phenol in almond- Excision of the prolapsed mucosa (Goodsall's ligature)
Complete prolapse (syn. procidentia)
- More common in the elderly.
- Women are six times more often affected than men.
- Is less common than the partial variety.
- The protrusion consists of all layers of the rectal wall.
- It is more than 4 cm and commonly as much as 10-15 cm in length.
- On palpation between the finger and the thumb, the prolapse feels much thicker than a partial prolapse, and obviously consists of a double thickness of the entire wall of the rectum.
- The prolapsed mucous membrane is often arranged in a series of circular folds.
- The anal sphincter is characteristically patulous.
the real pathophsiology is not well known but there is multiple theory
1-failure of rectal support by elevators and pelvic fascia due to defective collagen maturation in the pelvic floor2- rectal prolapse may be represent a sliding hernia
3-abnormal mobility of the mesorectum leading to lack of fixation of rectum to the sacrum
4-pelvic floor denervation due to repeated birth
Complete prolapse (syn. procidentia)
Treatment of complete prolapse
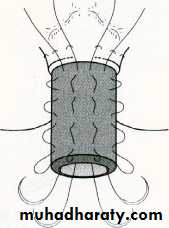
usually need surgery ,there are multiple surgery1- rectopexy (Well`s operation)
through abdominal approach, the rectum mobilized and pulled upward, polypropylene mesh or ivalon sponge is attached to presacral fascia then wrapped and sutured around the back and side of the rectum, this form fibrosis and fix the rectum to the sacrum
2- delorme`s operation
through perineal approacha) The mucosa has been removed from the prolapsed rectum
b) interrupted sutures have been placed in the underlying muscle so that, when tied, the muscle is plicated
3- excision of redundant rectum either through perineal or abdominanal approach
4- thiersch`operation for older and tired patientit is narrowing of the anus by the non-absorbable suture is tunneled subcutaneously around the anal canal so narrowed anus prevent the rectum from prolapse
Solitary Rectal Ulcer Syndrome
Solitary rectal ulcer syndrome is commonly associated with internal intussusception.- Patients may complain of pain, bleeding, mucus discharge,.
- In solitary rectal ulcer syndrome, one or more ulcers are present in the distal rectum, usually on the anterior wall.
- Evaluation should include anorectal manometry,
defecography, and either colonoscopy or barium enema to exclude other diagnoses.
- Biopsy of an ulcer or mass is mandatory to exclude malignancy
Treatment
- non-operative therapy is effective in the majority of patients1- high-fiber diet
2- defecation training to avoid straining
3- and laxatives or enemas.
-Surgery
- either abdominal or perineal repair of prolapse as described above.
- is reserved for highly symptomatic patients and not respond to conservative treatment
Benign rectal tumor
Rectal polyp1- juvenile polyp
-It is bright red glistening pedunculated sphere
-It occur in infant and children , occasionally persist to adult life
-It has no tendency to malignancy
- patient has bleeding per rectum
- some time prolapsed during defecation , and obstructed and cause pain
Treatment is excision
2- Inflammatory polyp
It is edematous bosses of the mucous membrane and usually associated with colitis3- Metaplastic polyp
Small, pinkish, sessile, 2-4mm in diameter, multiple , not cause symptom and not malignant
4- Villous adenoma
- it has frond like appearance, large in size , might fill the rectum
- It has tendency to malignant change
- some time it cause profuse mucous discharge containing high potassium which lead to fluid and electrolyte disturbence , hypokalaemai
Treatment excision and biopsy
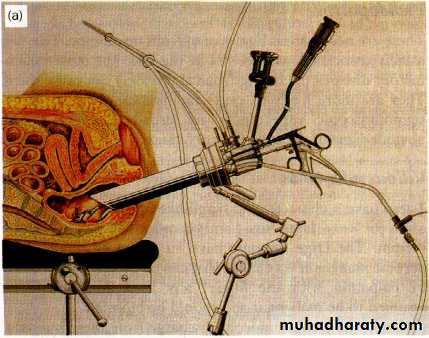
- recently anew technique to remove the polyps by transanal endoscopic microsurgery TEM.
- All neoplastic polyp can be snared through colonoscope
Villous adenoma
Rectal polyps
Transanal endoscopic microsurgery technique.
5-Familial adenomatous polyposis- it is inhereditory disease, autosomal dominant, the gene of it is isolated on chromosome 5.
- it is either tubular,or tubulovillous, or villous histologically
- It is premalignant, all of them changed to malignancy
Clinical features
- present at age 10-15 years
- patient has diarrhea, bleeding and abdominal pain
Diagnosis;
barium enema, colonoscopy and biopsy
Treatment
- totalproctocolectomy is indicated , either with permanent ileostomy,
or totat proctocolectomy with pouch-anal anastomosis
Carcinoma of the rectum
- incidence ca of colorectum is the second ca.as general.- in male it is 2nd most common after ca of bronchus it comes
- in female is 4th most common
the rectum is most frequent site involved
- in 5% of cases there is more than one carcinoma present in the rectum or colon (synchronous tumor)
most of carcinoma started as adenoma and it pass to dysplasia then to carcinoma in situ then invasive carcinoma
adenma-carcimnoma siequence
adenom → dysplasia → carcinoma insitu → invasive carcinoma
frond
Risk Factors
1-Aging the incidence rising steadily after age 50 years. More than 90% of cases older than age 50 years2-Hereditary 80%is sporadic, but20% of patients has family history of colorectal cancer, defects in the APC gene and in mismatch repair genes
3-Environmental and Dietary
- saturated or polyunsaturated fats (animal fat) increases risk of colorectal cancer
- while a diet high in oleic acid (olive oil, coconut oil, fish oil) does not increase risk
- a diet high in vegetable fiber appears to be protective
- obesity and sedentary lifestyle dramatically increase cancer-related mortality
4-Inflammatory Bowel Disease depend on extend and duration of disease
- In ulcerative pancolitis, the risk of carcinoma is approximately 2% after 10 years, 8% after 20 years, and 18% after 30 years.- Patients with Crohn's pancolitis have similar risk
- screening colonoscopy with multiple random mucosal biopsies has been recommended annually for
a- after 8 years of disease for patients with pancolitis
b- after 12 to 15 years of disease for patients with left-sided colitis
5- smoking , more than 35 years
6- ureterosigmoidostomy
7- Acromegaly
8- Pelvic irradiation
Pathology
A- it is adenocarcinoma arising from the mucosa of the rectum
By cross section it occur as
- an ulcerative
- papilliferous
- infiltrating type
and by histological examination . There is glandular arrangement with sign of malignancy in the cell and it is graded accordingly to
- well- differentiated 11% good prognosis
- averagely differentiate 64% fair prognosis
- anplastic, highly undifferentiated 25% poor prognosis
Colloid carcinoma 12%
either primary or secondary- the secondary is most common and due to secondary mucoid degeneration of adenocarcinoma, hitologically glandular arrangement preserved and mucous fill the acini
- the primary mucoid , the mucous lies in the cell and displace the nucleus periphery like the the seal of signet ring the prognosis is bad
B- leomyosarcoma smooth muscle tumor (gastrointestinal stromal tumour GIST)
Rectal ca.
Rectal ca.
Colorectal ca
Type of spread of the rectal tumor
1- local spread-it spread circumferentially rather than longitudinally, it take two year to complete encirclement
- it invade the muscular coat and spread to surrounding mesorectum
- it invade surrounding organ, bladder, prostate, ovary, uterus and later on even sacrum although presacral fascia act as barrier
2- lymphatic spread
- the carcinoma of the rectum above the peritoneal reflection spread to the upward direction to lymph node at superior rectal artery then then to the nodes around inferior mesentric artery- below the reflection also spread to upward but to the pararectal lymph node and also for the lymph node at internal iliac node
- Downward extension might be occur to the groin could be occur but rare
3-Venous spread
- it is occur at late stage- anaplastic and rapidly growing tumor in younger patient is more liable to spread by this method
the organ which is the main site for this metastasis is
- liver 34%
- lung 22%
- adrenal 11%
4-Peritoneal dissemination
it occur after penetration of the peritoneal coat, involve peritoneal cavity ,ovary and other organ
staging
Duke staging1- stage A growth limited to the rectal wall 15% of cases, prognosis is excellent
2- stage B the growth is extend to extrarectal tissue , but not involving free peritoneal surface and no lymph node metastasis, 35% of cases, prognosis is reasonable
3- stage C there is secondary in the regional lymph node 50% of cases
C1 only pararectal lymph node affected
C2 the node accompanying supplying blood vessels are affected
4-Stage D for distal metastasis although not described by Duke
The three cardinal stages of progression of the neoplasm.
A B CTNM Staging
(T)DefinitionTx Cannot be assessed
T0 No evidence of cancer
Tis Carcinoma in situ
T1 Tumor invades submucosa
T2 Tumor invades muscularis propria
T3 Tumor invades through muscularis propria into subserosa or into nonperitonealized perirectal tissues
T4 Tumor directly invades other organs or tissues or perforates the visceral peritoneum of specimen
Nodal Stage (N)
NX Regional lymph nodes cannot be assessedN0 No lymph node metastasis
N1 Metastasis to one to three pericolic or perirectal lymph nodes
N2 Metastasis to four or more pericolic or perirectal lymph nodes
N3 Metastasis to any lymph node along a major named vascular trunk
Distant Metastasis (M)
MX Presence of distant metastasis cannot be assessed
M0 No distant metastasis
M1 Distant metastasis present
Clinical feature
1- bleeding it is earliest and most common symptom .often the bleeding is slight in amount and occur at end of defecation or it is noticed as stained cloth
2- alteration of bowel habit it is the most frequent symptom usually diarrhea , there is mucous and or blood with it ( early morning bloody diarrhea),
annular carcinoma cause constipation
3- tenismus and sense of incomplete defecation
4- pain is late stage , in case of intestinal obstruction and also in case of extend of tumor to surrounding organ such as prostate, bladder , sacrum
5- loss of weight in advanced and metastasis
Investagation
1-rectal examination 90% of rectal tumor felt digitally by PR examination2- abdominal examination
3- proctosigmoidoscopy and biopsy from tumor
4- colonoscopy to exclude the synchronous tumor which occur at5%
5- ultrasound of abdomen to sea metastasis
6- endoscopic ultrasound helpful in staging of tumor
7- ct-scan and MRI abdomen and pelvis
8- Chest x-ray to exclude metastasis
Differential diagnosis
1- adenoma2-Inflammtory bowel disease
3- amoebic granuloma
4- endometrioma of the rectum
5- carcinoid tumor
6- solitary rectal ulcer
Treatment
treatment is surgery and the aim is
1-is to excise the rectum
2- mesorectum and associated lymph node even in the presence of solitary liver metastasis and lymph node metastasis
In case of locally advanced , preoperative radiotherapy reduce the size and make it more enable for excision
Type of surgery
1- anterior resection- it is anal sphincter preserving mechanism
- indicated for tumor at upper two third of the rectum in which
- resection of the rectum at least 2cm. below the tumor
- removal of all mesorectum
- high proximal ligation of the inferior mesenteric lymphovascular pedicle
- restoration of continuity by direct end to end anastomosis manually or by stapler
Before the operation you should assess
- fitteen's of the patient for surgery- stage of tumor
- pre operative preparation of colon
1- bowel preparation by mechanical cleaning using combination of diet and purgative
2- prophylactic antibiotic covering both aerobic and anaerobic organism (cefuroxime and metronidazole) one hour before operation
-laparoscopic anterior resection
2- abdominoperineal resection
- for lower third tumor- anal sphincter cannot be preserved
- In which the rectum and anal canal removed as one part through abdominal and perineal approach
- end,permnant colostomy at left ilaic fossa area
laparoscopic abdominoperineal resection
3- Hartmann`procedure
- for old patient that can not tolerate long surgery as anterior resection or abdominperineal procedure,- through abdominal approach, excision of the rectum down to within2.5cm. of the anus was done
- and proximal stump was taken as colostomy at left iliac fossa
4-palliative colostomy in case of intestinal obstruction, and later on to do proper surgery if the tumor is resect able
5- more extensive surgery in case of local extension of tumor to bladder, uterus , it is to remove these structure with rectum
6- pelvic exenteration in case more locally extensive tumor , is to remove all pelvic organ with internal iliac and obturator lymph nodes
7-Liver resection
Excision of single or several liver metastasis can be done with low morbidity and mortality
8- local operation for small low grade tumor T1 with in 10 cm. from anal verge ,
recently this done by transanal endoscopic microscopic technique
Radiotherapy
1-adjuvant radiotherapy can reduce local recurrence but long term survival is not affected2- Pre operative radiation with chemotherapy or with out, reduce the size of tumor and make it `subsequent removal easy
3- palliative irradiation for not operable and recurrent tumor
chemotherapy
- 5-fluorouracil and folinic acid when combined with surgery has significant affect for survivalimmunotherapy, monoclonal antibody for disseminated tumor
Prognosis
depend on stage, grade, and centre in which patient treated
50% 5-year survival after surgery
Follow-Up and Surveillance
Patients who have been treated for one colorectal cancer are at risk for the development of recurrent disease (either locally or systemically) or metachronous disease (a second primary tumor).
1-a colonoscopy should be performed within 12 months.
2-CEA often is followed every 2–3 months for 2 years.
Local recurrence
- due to incomplete removal of tumor or implantation of malignant cell during surgery- only in minority of case recurrent can be removed
Guidelines for Screening
Current American Cancer Society guidelines advocate screening for the average-risk population (asymptomatic, no family history of colorectal carcinoma, no personal history of polyps or colorectal carcinoma, no familial syndrome) beginning at age 50 years.Recommended procedures include
1-yearly FOBT
2- flexible sigmoidoscopy every 5 years
3- FOBT and flexible sigmoidoscopy in combination
4- air-contrast barium enema every 5 years
5- or colonoscopy every 10 years
reference
1-Baily and Love SHORT PRACTICE OF SURGERY 24TH edition2- Schwartz`s PRINCIPLES OF SURGERY
3- KASR EL-AINI INTRODUCTION TO SURGERY third edition
4- APPLIED BASIC SCIENCE for BASIC SURGICAL TRINING
5- Some pictures from NET