Pneumonia
Dr.Abdulla Al-farttoosi

OBJECTIVES
•
To define pneumonia .
•
To determine methods of its classification
•
To describe its epidemiology.
•
To describe Community Acquired Pneumonia (CAP) and its causes and
types.
•
To identify factors that predispose to pneumonia.
•
To recognize Clinical features of CAP.
•
To revise characteristic features of the common causes of CAP.
•
To asses and investigate a case of CAP.
•
To evaluate lines of management of CAP.
•
To recognize complications of CAP.
•
Pneumonia is defined as an acute
respiratory illness associated with recently
developed
radiological
pulmonary
shadowing which may be segmental, lobar
or multilobar.
•
Pneumonia
is
an
infection
of
the
pulmonary parenchyma.
•
Not a single disease, but a group of
specific infection, each having different
epidemiology,
pathogenesis,
clinical
manifestations and clinical course.
CLASSIFICATION:
•
Aetiology.
•
Morphological class. - Bronchopneumonia
vs. lobar pneumonia(
'
Lobar
:homogeneous
consolidation of one or more lung lobes, often with associated
pleural inflammation;
bronchopneumonia
:more patchy alveolar
consolidation associated with bronchial and bronchiolar
inflammation often affecting both lower lobes)
•
Community acquired vs hospital acquired
(nosocomial) infection.
•
The patient's immune status.

•
Community-acquired pneumonia (CAP):
Outside of
hospital or extended-care facility.
•
Hospital-acquired pneumonia (HAP)
:
≥ 48 h from
admission.
•
Ventilator-associated pneumonia (VAP)
:
≥ 48 h
from endotracheal intubation.
•
Health care-associated pneumonia (HCAP):
onset of
pneumonia as outpatients in patients infected with the
multidrug-resistant (MDR) pathogens usually associated
with HAP.

Epidemiology
•
Leading cause of death from an infectious
disease
•
6th leading cause of death in the US
•
Mortality ranges 2-30% in hospitalized
patients and averages 14%
•
Mortality if admitted to ICU nearly 50%
•
Community-acquired pneumonia (CAP)
remains a leading cause of death
worldwide despite improvement in patient
management.
•
Early recognition of lung infection and
prompt
initiation
of
adequate
antibiotherapy are crucial elements to
ensuring favourable outcomes.

•
Nonetheless, in a number of cases, death
occurs despite both these targets being
met. In these patients, possible excessive
inflammatory responses, as in sepsis and
septic shock, are believed to contribute to
unfavourable outcome.

PATHOPHYSIOLOGY
•
Pneumonia results from the proliferation of microbial
pathogens at the alveolar level and the host' s response to those
pathogens.
•
Microorganisms gain access to the lower respiratory tract in
several ways. The most common is by aspiration from the
oropharynx .Small-volume aspiration occurs frequently during
sleep (especiallyin the elderly) and in patients with decreased
levels of consciousness.
•
Many pathogens are inhaled as contaminated droplets.
•
Rarely pneumonia occurs via hematogenous spread
Host defense mechanisms
•
The hairs and turbinates of the nares capture larger
inhaled particles
•
The branching architecture of the tracheobronchial
tree .
•
Mucociliary clearance
•
The gag reflex and the cough mechanism.
•
The normal flora adhering to mucosal cells of the
oropharynx.
•
When these barriers are overcome or when
microorganisms are small enough to be inhaled to the
alveolar level, resident alveolar macrophages are
extremely efficient at clearing and killing pathogens.
•
Only when the capacity of the alveolar
macrophages to ingest or kill the
microorganisms is exceeded does clinical
pneumonia become manifest.
•
In that situation, the alveolar macrophages
initiate the inflammatory response to bolster
lower respiratory tract defenses.
•
The host inflammatory response, rather than
proliferation of microorganisms, triggers the
clinical syndrome of pneumonia.
Community Acquired
Pneumonia
•
Community Acquired Pneumonia (CAP) is
an acute infection of lung tissue that
develops outside of the hospital setting.
The most common bacterial cause of CAP
is Streptococcus pneumoniae .

Bacteria commonly enter the respiratory tract,
but do not normally cause pneumonia. When
pneumonia does occur, it is the result of:
1.A very virulent microbe
2.A large “dose” of bacteria
3.An impaired host defense mechanism
Factors that predispose to pneumonia
•
Cigarette smoking
•
Upper respiratory tract infections
•
Alcohol
•
Corticosteroid therapy
•
Old age
•
Recent influenza infection
•
Pre-existing lung disease
•
HIV
•
Indoor air pollution
•
•
Causative organism established in 60% CAP in
research setting, 20% in clinical setting
•
“Typical”:
– S. pneumoniae, Haemophilus influenzae,
Staphylococcus aureus, Group A streptococci,
Moraxella catarrhalis, anaerobes, and aerobic
gram-negative bacteria
•
“
Atypical”
- 20-28% CAP worldwide Legionella
spp, Mycoplasma pneumoniae, Chlamydophila
pneumoniae, and C. psittaci
– Mainly distinguished from typical by not being
detectable on Gram stain or cultivable on
standard media
Clinical features
•
fever, rigors, shivering, headache and vomiting .
•
Dyspnea , cough with
mucopurulentsputum(occasional
haemoptysis)and Pleuritic chest pain
•
Upper abdominal pain
•
Less typical presentations may be seen at the
extremes of age.
•
signs:Crackles & bronchial breathing and
whispering pectoriloquy

Common clinical features of community-
acquired pneumonia
•
Streptococcus pneumoniae
•
Most common cause. Affects all age
groups, particularly young to middle-aged.
•
Sudden onset of fever, rigors, dyspnea,
bloody sputum production, chest pain,
tachycardia, tachypnea and abnormal
findings on lung exam
•
may be accompanied by herpes labialis

Staph aureus
•
Associated with debilitating illness and
often preceded by influenza.
•
Radiographic features include multilobar
shadowing, cavitation, pneumatocoeles
and abscesses.
•
Dissemination to other organs may cause
osteomyelitis, endocarditis or brain
abscesses. Mortality up to 30%

Klebsiella pneumoniae
•
More
common
in
men,
alcoholics,
diabetics, elderly, hospitalised patients,
and those with poor dental hygiene.
Predilection
for
upper
lobes
and
particularly liable to suppurate and form
abscesses. May progress to pulmonary
gangrene.

•
Haemophilus influenzae
:
More common
in old age and those with underlying lung
disease (COPD, bronchiectasis).
•
Pseudomonas
: not a typical cause of
CAP and usually associated in patients
who have prolonged hospitalization, have
been on broad-spectrum antibiotics, high-
dose steroids, structural lung disease

Mycoplasma pneumonia
•
Gram neg bacteria with no true cell wall
•
Frequent cause of CAP in adults + children
•
May be asymptomatic
•
Gradual onset
•
Objective abnormalities on physical exam are
minimal in contrast to the patients reported symptoms
•
Epidemics occur every 3-4 years, usually in autumn.
Rare complications include haemolytic anaemia,
Stevens-Johnson syndrome, erythema nodosum,
myocarditis, pericarditis, meningoencephalitis,
Guillain-Barré syndrome
Legionella pneumophila
•
Middle to old age.
•
Local epidemics around contaminated source,
e.g. cooling systems in hotels, hospitals. Person-
to-person spread unusual.
•
Some features more common, e.g. headache,
confusion, malaise, myalgia, high fever and
vomiting and diarrhoea.
•
Tends to be the most severe of the atypical
pneumonias
•
Laboratory abnormalities include
hyponatraemia, elevated liver enzymes,
hypoalbuminaemia and elevated creatine
kinase.

Chlamydia pneumoniae
•
Young to middle-aged.
•
Large-scale epidemics or sporadic; often
mild, self-limiting disease. Headaches and
a longer duration of symptoms before
hospital admission.
•
Usually diagnosed on serology
Differential diagnosis of
pneumonia
•
Pulmonary infarction
•
Pulmonary/pleural TB
•
Pulmonary oedema (can be unilateral)
•
Pulmonary eosinophilia (p. 713)
•
Malignancy: bronchoalveolar cell
carcinoma
•
Rare disorders: cryptogenic organising
pneumonia/
•
bronchiolitis obliterans organising
pneumonia (COP/BOOP)

Investigations
•
To exclude other conditions that mimic
pneumonia , assess the severity, and
identify the development of complications.
•
A
chest
X-ray
usually
provides
confirmation of the diagnosis.

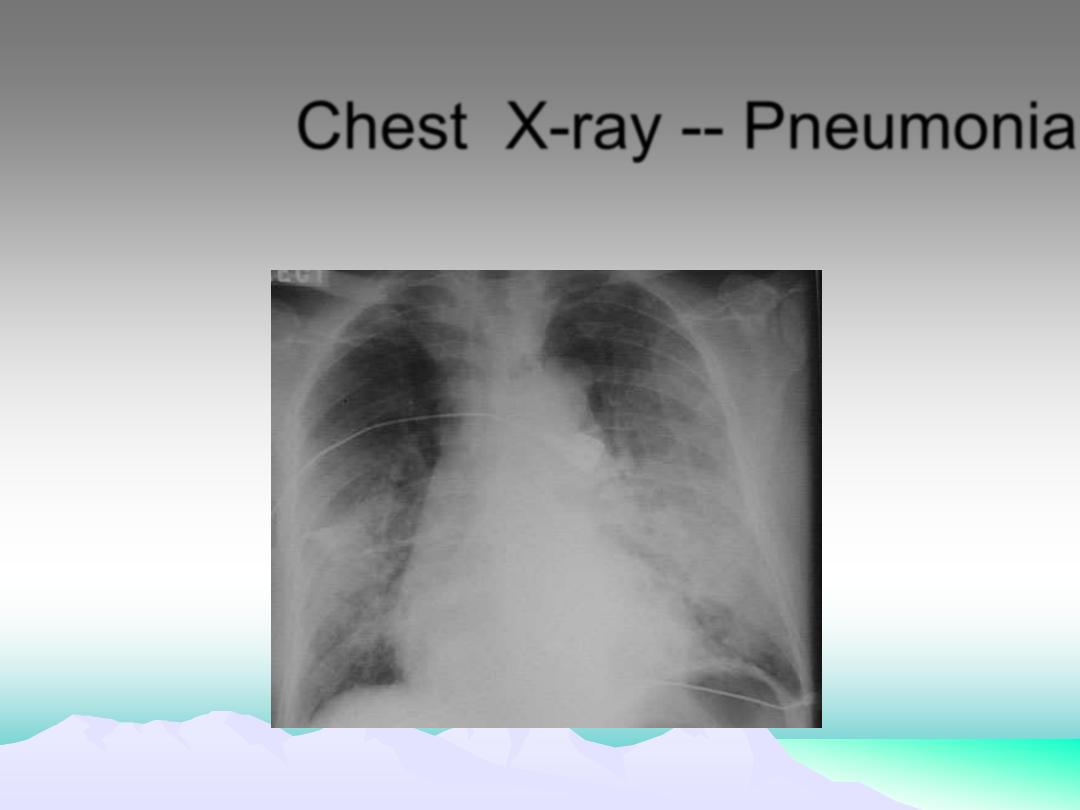
Chest X-ray -- Pneumonia

Microbiological investigations
•
Severe disease
•
Notification(Legionella pneumophila)
•
In patients who do not respond to initial
therapy
•
provides useful epidemiological
information

•
Sputum:
direct smear by Gram and Ziehl-
Neelsen stains. Culture and antimicrobial
sensitivity testing
•
Blood culture
: frequently positive in
pneumococcal pneumonia
•
Serology
: acute and convalescent titres for
Mycoplasma, Chlamydia, Legionella,
and
viral infections. Pneumococcal antigen
detection in serum or urine
•
PCR
:
Mycoplasma
can be detected from
swab of oropharynx
•
Pulse oximetry
and arterial blood gas
•
The white cell count
: A very high (> 20
×
109/l) or low (< 4
× 109/l) white cell count
may be seen in severe pneumonia.
•
Urea
and electrolytes and liver function
tests
•
C-reactive protein

CURB-65
To assess severity and Determining Site of Care
• C
onfusion (
disorientation to person, place or time)
• U
rea (
BUN > 7 mmol/L)
• R
espiratory Rate (
RR > 30 breaths/minute)
• B
lood Pressure
(systolic< 90 mmHg-diastolic< 60 mm Hg)
• 65
(years of age or greater)
One point for each prognostic variable
0-1 treat as outpatient, 2 general inpatient admission,
3-5 intensive care admission
Management
•
Oxygen
•
Fluid balance
•
Antibiotic therapy.
•
Nutritional support
•
Treatment of pleural pain
•
Physiotherapy

Oxygen
•
All patients with tachypnoea, hypoxaemia,
hypotension or acidosis with the aim of
maintaining the PaO2
≥ 8 kPa (60 mmHg)
or SaO2
≥ 92%.
•
High concentrations (EXCEPT in COPD)
•
Assisted ventilation should be considered
at an early stage in those who remain
hypoxaemic despite adequate oxygen
therapy.
Antibiotic treatment for CAP
•
Uncomplicated CAP
•
Amoxicillin 500 mg 8-hourly orally
•
If patient is allergic to penicillin Clarithromycin
500 mg 12-hourly orally or
•
Erythromycin 500 mg 6-hourly orally
•
If Staphylococcus is cultured or suspected
Flucloxacillin 1-2 g 6-hourly i.v. plus
•
Clarithromycin 500 mg 12-hourly i.v.
•
If Mycoplasma or Legionella is suspected
Clarithromycin 500 mg 12-hourly orally or
i.v. or Erythromycin 500 mg 6-hourly orally
or i.v. plus
•
Rifampicin 600 mg 12-hourly i.v. in severe
cases
•
•
•
Severe CAP
•
Clarithromycin 500 mg 12-hourly i.v. or
•
Erythromycin 500 mg 6-hourly i.v.
plus
•
Co-amoxiclav 1.2 g 8-hourly i.v. or
•
Ceftriaxone 1-2 g daily i.v. or
•
Cefuroxime 1.5 g 8-hourly i.v. or
•
Amoxicillin 1 g 6-hourly i.v. plus
flucloxacillin 2 g 6-hourly i.v.
•
•

•
Patients with severe CAP should not
receive corticosteroids, unless shock that
requires vasopressor infusion is present.
•
In addition, corticosteroids should not be
given
in
case
of
influenza-related
respiratory distress.
•
patients exposed to NSAIDs during the
early stage of CAP had a worse
presentation
of
CAP,
more
pleuropulmonary
complications
and
required noninvasive ventilatory support
more often, such as high-flow oxygen
therapy
•
59- A patient was treated for right sided lobar pneumonia, he started to
improve but 5 days latter fever recurred with chills, night sweats and
chest pain in deep breathing, O/E dull chest percussion note on the right
side, chest X- ray showing D-shaped opacity. Which one of the followings
is the most likely cause?
•
A- Chylothorax
•
B- Empyema
•
C- Hemothorax
•
D- TB
•
E- Lung abscess
Complications of pneumonia
•
Para-pneumonic effusion-common
•
Empyema
•
Retention of sputum causing lobar collapse
•
DVT and pulmonary embolism
•
Pneumothorax, particularly with Staph. aureus
•
Suppurative pneumonia/lung abscess
•
ARDS, renal failure, multi-organ failure
•
Ectopic abscess formation (Staph. aureus)
•
Hepatitis, pericarditis, myocarditis,
meningoencephalitis
•
Pyrexia due to drug hypersensitivity
•

Indications for referral to ITU
•
CURB score of 4
–5,failing to respond
rapidly to initial management
•
Persisting hypoxia (
Pa
O
2
< 8 kPa (60
mmHg)), despite high concentrations of
oxygen
•
Progressive hypercapnia
•
Severe acidosis
•
Circulatory shock
•
Reduced conscious level

Hospital-acquired pneumonia
•
Refers to a new episode of pneumonia
occurring
at
least
2
days
after
admission to hospital. Older people are
particularly at risk, as are patients in
intensive care units, especially when
mechanically ventilated, in which case
the
term
ventilator-associated
pneumonia (VAP) is applied.

Health care-associated
pneumonia(HCAP
)
•
Refers to the development of
pneumonia in a person who has
spent at least 2 days in hospital
within the last 90 days, attended a
haemodialysis
unit,
received
intravenous antibiotics, or been
resident in a nursing home or other
long-term care facility.
Aetiology
•
When HAP occurs within 4-5 days of
admission (early-onset), the organisms
involved are similar to those involved in
CAP; however, late-onset HAP is more
often
attributable
to
Gram-negative
bacteria (e.g. Escherichia, Pseudomonas
and Klebsiella species), Staph. aureus
(including meticillin-resistant Staph. aureus
(MRSA)) and anaerobes.
Factors predisposing to hospital-acquired
pneumonia
•
Reduced host defences against
bacteria
•
Aspiration of nasopharyngeal or
gastric secretions
•
Bacteria introduced into lower
respiratory tract
•
Bacteraemia
Clinical features and investigations
•
HAP should be considered in any hospitalised or
ventilated patient who develops purulent sputum
,new radiological infiltrates, an otherwise
unexplained increase in oxygen requirement, a
core temperature > 38.3
°C, and a leucocytosis
or leucopenia. Appropriate investigations are
similar to those outlined for CAP, although
whenever possible, microbiological confirmation
should be sought. In mechanically ventilated
patients, bronchoscopy-directed protected brush
specimens or bronchoalveolar lavage (BAL) may
be performed.
Mangement
•
empirical antibiotic therapy :
•
Adequate Gram-negative cover by
•
a third-generation cephalosporin
+aminoglycoside
•
Or a monocyclic β-lactam (e.g. aztreonam) and
flucloxacillin.
•
or meropenem
•
MRSA is treated with intravenous vancomycin,

Suppurative pneumonia, aspiration
pneumonia and pulmonary abscess
•
These
conditions
are
considered
together, as their aetiology and clinical
features
overlap.
Suppurative
pneumonia
is
characterised
by
destruction of the lung parenchyma by
the inflammatory process
•
'pulmonary abscess' is usually
taken to refer to lesions in which
there is a large localised collection
of pus, or a cavity lined by chronic
inflammatory tissue, from which
pus has escaped by rupture into a
bronchus
.
risk factors
•
Inhalation of septic material during
operations or of vomitus during
anaesthesia or coma
•
Bulbar or vocal cord palsy
•
Stroke
•
Achalasia or oesophageal reflux
•
Alcoholism.
•
Local bronchial obstruction from a
neoplasm or foreign body.
•
Aspiration tends to localise to
dependent areas of the lung such
as the apical segment of the lower
lobe in a supine patient
•
Infections are usually due to a
mixture of anaerobes and aerobes
•
In a previously healthy lung, the
most likely infecting organisms are
Staph.
aureus
or
Klebsiella
pneumoniae
•
Injecting
drug-users
are
at
particular
risk
of
developing
haematogenous
lung
abscess,
often
in
association
with
endocarditis
affecting
the
pulmonary and tricuspid valves.
•
A non-infective form of aspiration
pneumonia-exogenous
lipid
pneumonia-may
follow
the
aspiration of animal, vegetable or
mineral oils.

Investigations
•
Radiological features :
•
lobar or segmental consolidation
or collapse.
•
abscesses are characterised by
cavitation and fluid level.
•
Sputum and blood culture.
Clinical features of
suppurative pneumonia
•
Cough productive of large
amounts of sputum which is
sometimes fetid and blood-stained
•
Pleural pain common
•
Sudden expectoration of copious
amounts of foul sputum occurs if
abscess ruptures into a bronchus

Clinical Signs
•
High remittent pyrexia
•
Profound systemic upset
•
Digital clubbing may develop quickly
(10-14 days)
•
Chest examination usually reveals
signs of consolidation; signs of
cavitation rarely found
•
Pleural rub common
•
marked weight loss
Mangement
•
Oral treatment with amoxicillin 500
mg 6-hourly is effective in many
patients. Aspiration pneumonia
can be treated with co-amoxiclav
1.2 g 8-hourly. If an anaerobic
bacterial infection is suspected
(e.g. from fetor of the sputum), oral
metronidazole 400 mg 8-hourly
should be given.
•
Parenteral
therapy
with
vancomycin or daptomycin can
also be considered.
•
Prolonged treatment for 4-6 weeks
may be required in some patients
with lung abscess
•
Physiotherapy
is
of
great
value,
especially when suppuration is present
in the lower lobes or when a large
abscess cavity has formed. In most
patients, there is a good response to
treatment,
and
although
residual
fibrosis
and
bronchiectasis
are
common sequelae, these seldom give
rise to serious morbidity. Surgery
should
be
contemplated
if
no
improvement occurs despite optimal
medical therapy.

Pneumonia
in the
immunocompromised patient
•
Patients immunocompromised by drugs
or disease are at high risk of pulmonary
infection. The majority of infections are
caused by the same pathogens that
cause
pneumonia
in
non-
immunocompromised individuals, but in
patients
with
more
profound
immunosuppression,unusual organisms,
or those normally considered to be of
low virulence or non-pathogenic, may
become 'opportunistic' pathogens

•
In addition to the more common
agents,
the
possibility
of
Gram-
negative
bacteria,
especially
Pseudomonas aeruginosa, viral agents,
fungi, mycobacteria, and less common
organisms
such
as
Nocardia
asteroides,
must
be
considered.
Infection is often due to more than one
organism.

Clinical Features
•
These typically include fever,
cough and breathlessness, but are
less specific with more profound
degrees of immunosuppression. In
general, the onset of symptoms
tends to be less rapid when caused
by opportunistic organisms such
as
Pneumocystis jirovecii
and in
mycobacterial infections, than with
bacterial infections
•
In
P. jirovecii
pneumonia, symptoms of
cough and breathlessness can be present
several days or weeks before the onset of
systemic symptoms or the appearance of
radiographic abnormality
Diagnosis
•
As many patients are too ill to undergo
Invasive investigations safely, 'induced
sputum' may offer a relatively safe method
of obtaining microbiological samples.
•
HRCT is useful in differentiating the likely
cause.

Management
•
The causative agent is frequently
unknown
and
broad-spectrum
antibiotic therapy is required, such
as:
•
a third-generation cephalosporin,
or
a
quinolone,
plus
an
antistaphylococcal antibiotic, or
•
an antipseudomonal penicillin plus
an aminoglycoside.
•
Thereafter
treatment
may
be
tailored according to the results of
investigations and the clinical
response.
Depending
on
the
clinical context and response to
treatment, antifungal or antiviral
therapies may be added.
