Dr. Adnan M. Al- Jubouri
Lec. 3
ARDS
Tues. 22 / 12 / 2015
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
ARDS Dr. Adnan M. Al- Jubouri
22-12-2015
1
Acute respiratory distress syndrome (ARDS)
Definition
It is a syndrome in which there is pulmonary oedema without increment in the
pulmonary capillary venous pressure or non-cardiac pulmonary oedema.
It is also called “shock lung”.
Unlike the Lt. sided heart failure, in which there is pulmonary oedema due to
increment in the Lt. atrial pressure which causes increment in the pulmonary
venous pressure → oozing of fluids to the lung tissue → cardiac pulmonary
oedema, while in ARDS, the pulmonary oedema is due to oozing of fluids
through the capillaries without increment in pulmonary venous pressure which
means that the defect in the respiratory membrane.
How to understand ARDS & acute lung injury (ALI)
Acute lung injury (ALI):
It is any form of lung damage and less severe form of the condition is called
ALI. It could progress to ARDS.
This syndrome is caused by a variety of causes that are either directly or
indirectly cause damage to the lung tissue.
- Directly: bullet injury, blast, embolus, infections, etc.
- Indirectly: haemolytic anaemia, multiple fractures, head injury, etc.
ARDS Dr. Adnan M. Al- Jubouri
22-12-2015
2
Causes
There are many processes that precipitate ARDS. The following are well known
causes:
1) Pulmonary infection:
a. Viral, e.g. H1N1 influenza, SARS, etc.
b. Mycoplasma.
c. Bacterial.
d. Tuberculosis
2) Injuries:
a. Lung injury: either directly by a bullet or blast, etc., or indirectly by
fractures or haemolytic anaemia, etc.
b. Fractures.
c. Head injury.
d. Surgery – if prolonged- causes ARDS.
3) Septicemia & septic shock, in fact all shock states can cause ARDS, that is why
ARDS is called "shock lung".
4) Acute pancreatitis
5) Burn
6) Embolization: either fatty embolus, pulmonary thrombo-embolus, air embolus,
& amniotic fluid embolus.
** Usually, embolization is due to a small embolus that blocks small tributary of
pulmonary artery; but the patient may develop ARDS (unknown cause) or by big
embolus → massive pulmonary embolization → ARDS.
7) Direct damage to the lung by acids (due to vomiting or regurgitation) → ARDS.
8) Drowning: water is detrimental to the lung & can initiate ARDS.
9) Hanging: either suicidal or execution, if the patient - for example- survive after
hanging himself → develop ARDS.
ARDS Dr. Adnan M. Al- Jubouri
22-12-2015
3
10) Inhalation of chemicals & toxic materials: as in the wars, which cause ARDS
& serious respiratory problems to the soldiers, or it can happen to the workers
(who works in water refinery system)
where chlorine is used for water cleaning,
but chlorine is very irritant to the lung & cause damage to the lung tissue, it
also happens in housewives who use detergent in large conc.
11) In cardio-pulmonary bypass in cardiac surgery.
12) Multiple blood transfusions.
13) Gastric aspiration.
14) Toxic gases that cause this syndrome one of which is O
2
. Though O
2
is used in
the treatment of this syndrome, it is an irritant gas if given in high conc., so it is
mandated not to give high conc. for more than 24 hours, & this could happen in
mechanical ventilators, if you breath into close circuit & getting pure O
2
(100%
conc.), so if you need O
2
, you should not use pure O
2
over 24hs because it may
lead to this syndrome.
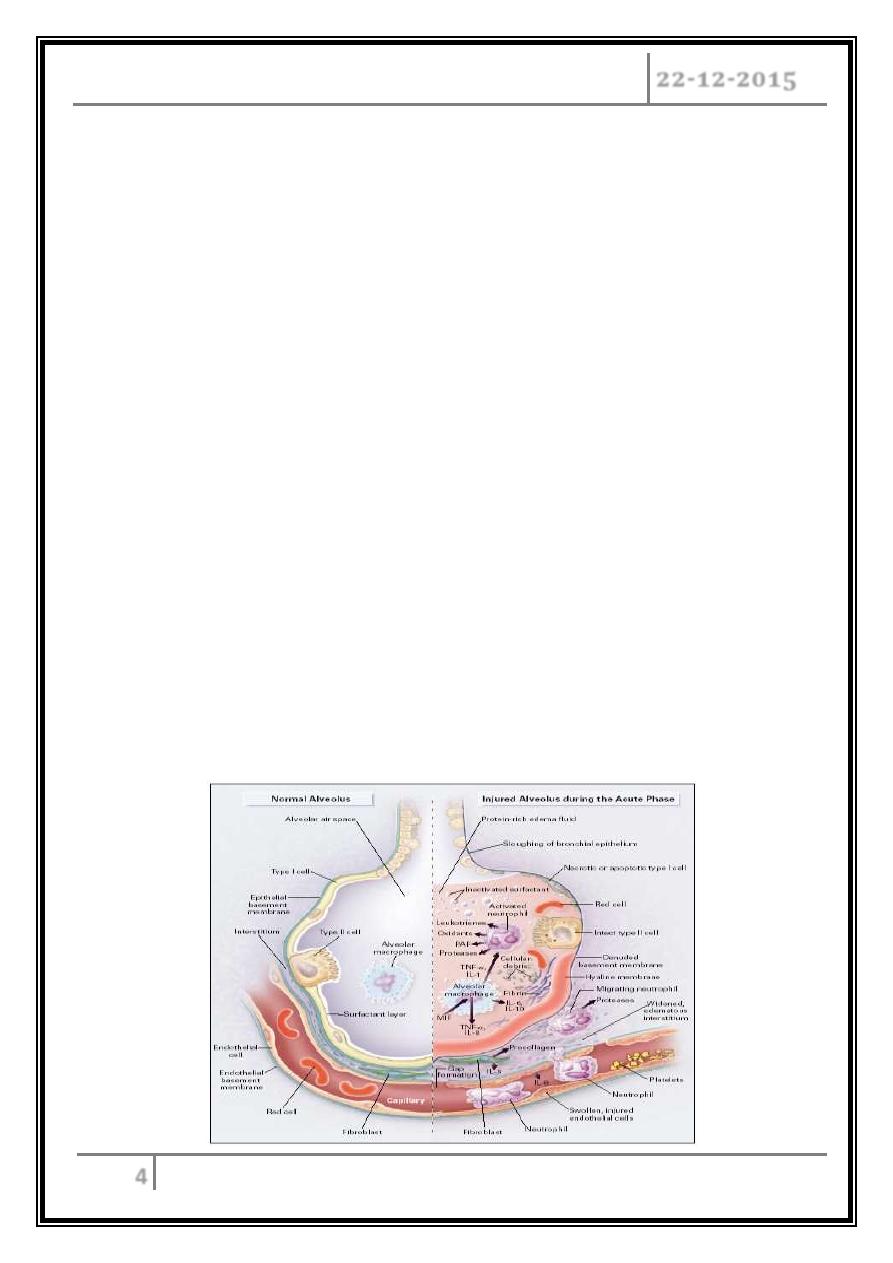
Pathophysiology
Regardless of the cause of ARDS, it will lead to destruction of the lung tissue &
this tissue contains endothelium of the blood vessels & the epithelium in the alveoli
which constitute the respiratory membrane. Hence, the process will lead to damage to
both epithelium & the endothelium or to any one of them, & once the capillaries get
damaged it will lead to oozing of oedema fluid to the alveolar spaces, this is actually a
pulmonary oedema, (such thing can occur in left sided heart failure) & there will be
oozing of fluid from the capillaries to the air-spaces of the lung tissue. Hence, damage
to the epithelial & endothelial layers due to inflammatory process of ARDS will lead to
stiffness of the lung.
ARDS Dr. Adnan M. Al- Jubouri
22-12-2015
4
Acute Phase:
Pulmonary oedema with normal vascular pedicle.
Associated with no cardiomegaly or upper lobe blood diversion.
When pulmonary vessels can be distinguished they are often constricted.
Septal lines usually absent because capillary leak occurs directly into
alveolar spaces (cardiogenic pulmonary oedema).
Progressive lung destruction and transition from alveolar to interstitial
opacities.
Chronic phase
Fibrosis.
Focal emphysema.
Inflammatory Alveolar Injury
Activation of inflammatory mediators and cellular components resulting in
damage to capillary endothelial and alveolar epithelial cells.
Increased permeability of alveolar capillary membrane.
Influx of protein rich edema fluid and inflammatory cells into air spaces.
Dysfunction of surfactant.
ARDS Dr. Adnan M. Al- Jubouri
22-12-2015
5
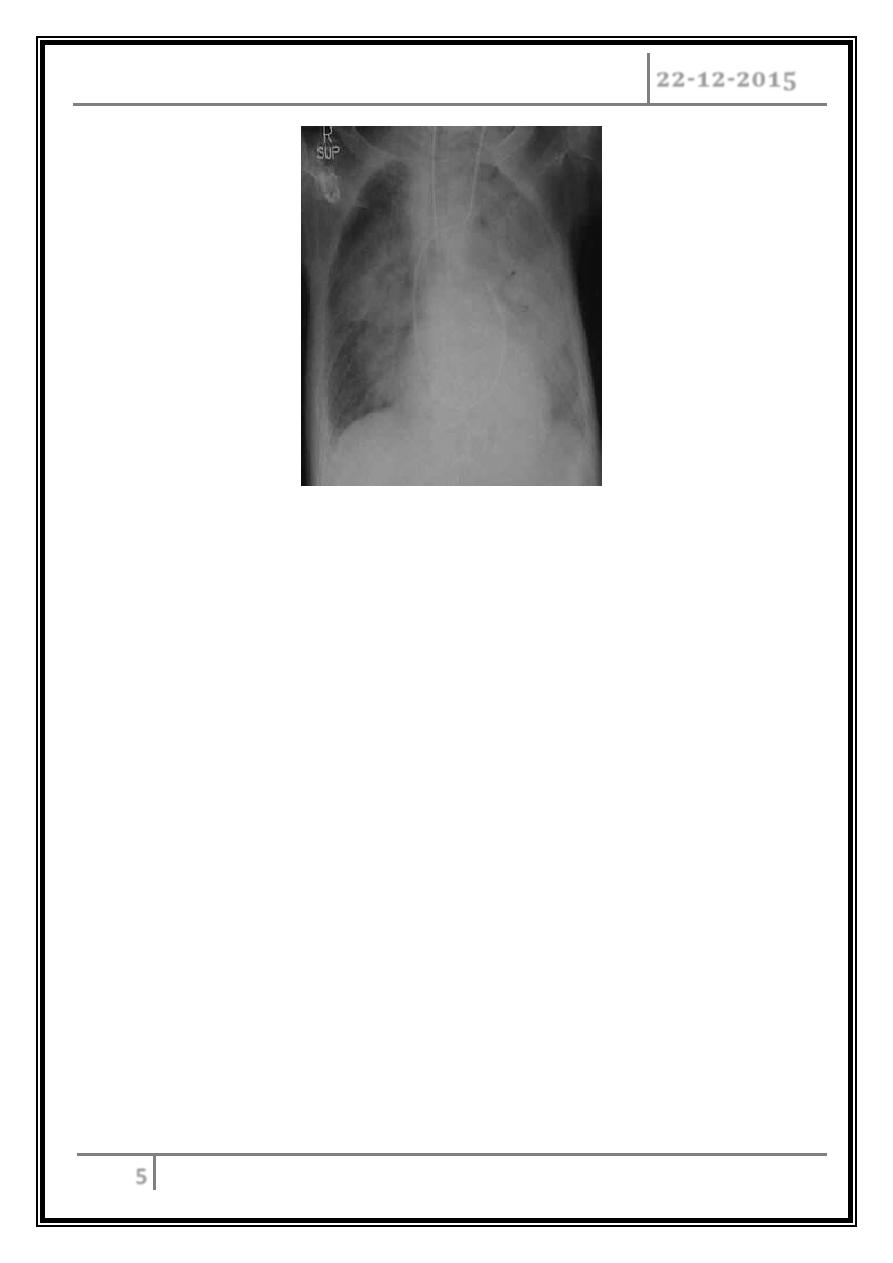
Severe ALI: Bilateral radiographic infiltrates PaO2/FiO2 <200 (N=201-300mmHg)
+ No
L Atrial P; PCWP <18mmHg
Clinical features
o Any patient having severe medical or surgical problem & the patient developed
severe RF within the first 1 or 2 days, you should think about ARDS.
o Again you find the features of the cause of the ARDS.
Complications
• Bacterial super infection, because oedema fluid is a good medium for infection
by many M.O.
• Multiple organ failure, because there will be septicemia which can leads to
liver, kidney, heart, or brain failure that is why the mortality rate is high even in
the best centers. Mortality rate in the best centers is about 50%, here in our
country the mortality rate is about 90%!! because of lack of sophisticated
equipment, the average mortality rate is about 70%.
• If the patient survives the acute phase then the patient will end up into
pulmonary fibrosis.
ARDS Dr. Adnan M. Al- Jubouri
22-12-2015
6
Summary of finding
1) Progressive SOB (1-2 days) following any medical or surgical problem.
2) Central cyanosis (resistant to treatment).
3) Hypoxia & hypocapnoea.
4) Wide-spread shadowing (bilateral) on chest X-ray.
5) On right sided cardiac catheterization to check the pulmonary venous pressure,
it will be normal (i.e. there is normal pulmonary wedge pressure, yet there is
pulmonary oedema.
6) Pulmonary fibrosis is the sequela of those who survive.
7) Fine crepitation, due to pulmonary edema O/E.
Treatment
The patient should be cared for in an "Intensive Care Unit" ICU, with facility for
mechanical ventilator & Rx is directed toward:
Cause (medical or surgical).
General measures.
General Measures
1) O2
therapy: liberal therapy should be offered for all patient regardless of the
cause; but not pure O
2
(high conc.) for more than 24h because it is irritant to
the lung tissue.
2) Mechanical ventilation: in ARDS, there is a damage to type II pneumatocyte →
decrease amount of surfactant, so you need always a +ve pressure to keep the
lung inflated & push the fluids away from the airspaces.
There are 2 types of assisted ventilation to keep this +ve pressure:
- IPPV “intermittent positive pressure ventilation".
- PEEP "positive end expiratory pressure".
ARDS Dr. Adnan M. Al- Jubouri
22-12-2015
7
3) Other general measures that include:
- Dealing with infection.
- Feeding & IV nutrition may be needed in ICU.
- Cleanliness.
- Prevent bed sore.
- Electrolyte balance must be carefully controlled.
- Use of steroids.
… END …
