Dr. Khalid A. Al- Khazraji
Lec. 9
ALCOHOLIC LIVER DISEASE
Wed. 9 / 3 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Alcoholic liver disease Dr. Khalid A. Al- Khazraji
9-3-2016
1
Alcoholic Liver Disease
Introduction
Chronic and excessive alcohol ingestion is one of the major causes of liver
disease.
The pathology of alcoholic liver disease consists of three major lesions:
- Fatty liver.
- Alcoholic hepatitis.
- Cirrhosis.
The prognosis of severe alcoholic liver disease is bad; the mortality of patients
with alcoholic hepatitis concurrent with cirrhosis is nearly 60% at 4 years.
Although alcohol is considered a direct hepatotoxin, only between 10 and 20%
of alcoholics will develop alcoholic hepatitis.
Global considerations: alcohol is the world’s third largest risk factor for
disease burden.
Pathogenesis
Quantity and duration of alcohol intake are the most important risk factors
involved in the development of alcoholic liver disease.
Progress of the hepatic injury beyond the fatty liver stage seems to require
additional risk factors that remain incompletely defined.
Gender is a strong determinant for alcoholic liver disease.
Obesity, high fat-diet and the protective effect of coffee, has been postulated to
play a part in the development of the pathogenic process.
Chronic infection with hepatitis C (HCV) is an important comorbidity in the
progression of alcoholic liver disease to cirrhosis in chronic and excessive
drinkers.
Alcoholic liver disease Dr. Khalid A. Al- Khazraji
9-3-2016
2
Pathology
Fatty liver is the initial and most common histologic response to hepatotoxic
stimuli, including excessive alcohol ingestion.
The accumulation of fat within the perivenular hepatocytes coincides with the
location of alcohol dehydrogenase.
Then continuing alcohol ingestion results in fat accumulation throughout in the
entire hepatic lobule.
Despite extensive fatty changes and distortion of the hepatocytes with
macrovesicular fat, stopping alcohol reverses the changes.
The appearance of steatohepatitis and certain pathologic features such as giant
mitochondria, perivenular fibrosis, and macrovesicular fat may be associated
with progressive liver injury.
The hallmark of alcoholic hepatitis is hepatocyte injury characterized by
ballooning degeneration, spotty necrosis, polymorphonuclear infiltrate, and
fibrosis in the perivenular and perisinusoidal space of Disse. Mallory bodies are
often present in florid cases.
Cirrhosis is present in up to 50% of patients with biopsy-proven alcoholic
hepatitis.
Alcoholic liver disease Dr. Khalid A. Al- Khazraji
9-3-2016
3
Clinical Features
Patients with fatty liver will present with right upper quadrant discomfort,
nausea, and, rarely jaundice.
Alcoholic hepatitis is associated with a wide range of clinical features; fever,
spider nevi, jaundice, and abdominal pain simulating an acute abdomen.
Portal hypertension, ascites, or variceal bleeding can occur in the absence of
cirrhosis.
It is important to recognize that patients with alcoholic cirrhosis often exhibit
clinical features identical to other causes of cirrhosis.
Laboratory Features
o The typical laboratory abnormalities seen in fatty liver are nonspecific and
include modest elevations of the aspartate aminotransferase (AST), alanine
aminotransferase (ALT), and γ-glutamyl transpeptidase (GGT), accompanied
by hypertriglyceridemia, hypercholesterolemia, and occasionally,
hyperbilirubinemia.
o In alcoholic hepatitis and in contrast to other causes of fatty liver, the AST and
ALT are usually elevated two- to seven-folds.
o Hyperbilirubinemia is common and is accompanied by modest increases in the
alkaline phosphatase level.
o Hypoalbuminemia and coagulopathy are common in advanced liver injury.
o Ultrasonography is useful in detecting fatty infiltration of the liver and
determining liver size.
Alcoholic liver disease Dr. Khalid A. Al- Khazraji
9-3-2016
4
Prognosis
Severe alcoholic hepatitis is heralded by coagulopathy (prothrombin time
increased > 5 s), anemia, serum albumin concentrations <25 g/L (2.5 mg/ dL), serum
bilirubin levels >137 µmol/ L (8 mg/ dL), renal failure, and ascites. A discriminant
function (DF) is calculated as 4.6 X [the prolongation of the prothrombin time above
control (seconds)] + serum bilirubin (mg/dL) can identify patients with a poor
prognosis.
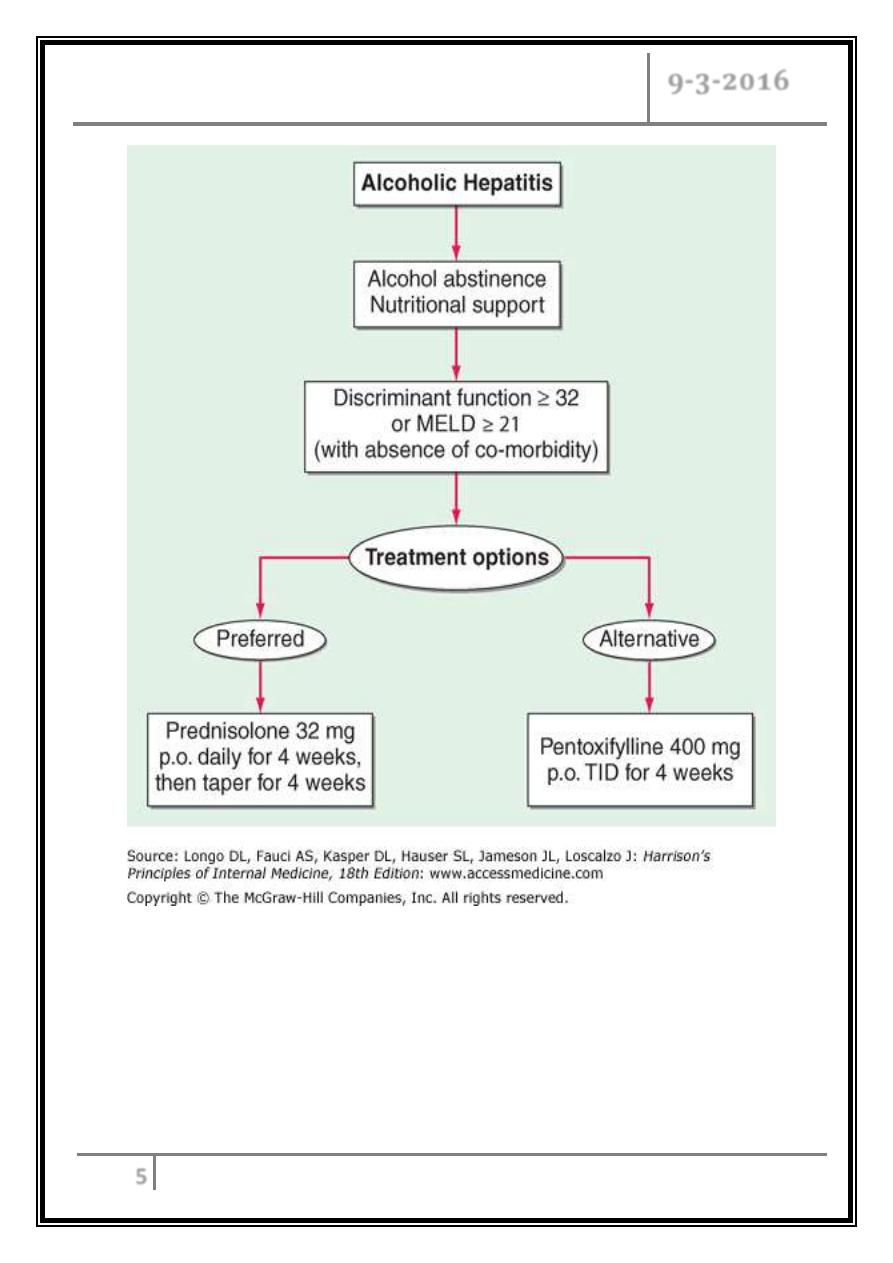
Treatment
Complete abstinence from alcohol is the cornerstone in the treatment of
alcoholic liver disease. Improved survival and the potential for reversal of
histologic injury.
Attention should be directed to the nutritional and psychosocial states during
the evaluation and treatment periods.
Glucocorticoids have been extensively evaluated in the treatment of alcoholic
hepatitis.
Patients with severe alcoholic hepatitis, defined as a discriminant function >32
or MELD >20, should be given prednisone (40 mg/ d), or prednisolone (32
mg/d), for 4 weeks, followed by a steroid tapering.
Exclusion criteria include active gastrointestinal bleeding, renal failure, or
pancreatitis.
The role of TNF-α expression and receptor activity in alcoholic liver injury has
led to an examination of TNF inhibition as an alternative to glucocorticoids for
severe alcoholic hepatitis. The nonspecific TNF inhibitor, pentoxifylline,
demonstrated improved survival in the therapy of severe alcoholic hepatitis.
Liver transplantation indicated in end-stage cirrhosis.
Alcoholic liver disease Dr. Khalid A. Al- Khazraji
9-3-2016
5
Treatment algorithm for alcoholic hepatitis
… End …
