Dr. Khalid A. Al- Khazraji
Lec. 11
CIRRHOSIS & ITS SEQUELAE –
PART 1
Mon. 4 / 4/ 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Cirrhosis & its sequelae Dr. Khalid A. Al- Khazraji
Part 1
4-4-2016
1
Cirrhosis & its sequelae – Part 1
Definition
It’s the final stage of any chronic liver disease, is a diffuse process
characterized by fibrosis and conversion of normal architecture to structurally
abnormal nodules. These “regenerative” nodules lack normal lobular
organization and are surrounded by fibrous tissue.
Cirrhosis can be classified by its status as compensated or decompensated.
Decompensated cirrhosis is defined by the presence of ascites, variceal
bleeding, encephalopathy, or jaundice.
Epidemiology
The prevalence of chronic liver disease or cirrhosis worldwide is estimated to
be 100 (range, 25 to 400) per 100,000 subjects.
According to the WHO, about 800,000 people die of cirrhosis annually.
The 12th leading cause of death overall.
Chronic liver disease and cirrhosis are the seventh leading cause of death in the
United States in individuals between 25 and 64 years of age.
PATHOLOGY
Liver fibrosis/ cirrhosis
In response to injury, hepatic stellate cells become activated, secrete
extracellular matrix they become contractile hepatic myofibroblasts.
Collagen deposition in the space of Disse leads to defenestration of the
sinusoidal endothelial cells (“capillarization” of the sinusoids), decreased
sinusoidal diameter.
Cirrhosis & its sequelae Dr. Khalid A. Al- Khazraji
Part 1
4-4-2016
2
Clinical manifestations
The clinical manifestations of cirrhosis range widely from an asymptomatic
patient with no signs of chronic liver disease to a patient who is confused and
jaundiced and has severe muscle wasting and ascites.
The natural history of cirrhosis is characterized by an initial phase, termed
compensated cirrhosis, followed by a rapidly progressive phase marked by the
development of complications of portal hypertension or liver dysfunction (or
both), termed decompensated cirrhosis.
In the compensated phase, identified for the development of varices or ascites.
As the disease progresses, portal pressure increases, portal hypertensive
gastrointestinal (GI) bleeding, encephalopathy, and jaundice.
Transition from a compensated to a decompensated stage occurs at a rate of
approximately 5 to 7% per year.
Compensated cirrhosis
o Cirrhosis is mostly asymptomatic, Nonspecific fatigue, decreased libido, or
sleep disturbances.
o About 40% of patients with compensated cirrhosis have esophageal varices
but no bleeding.
Decompensated cirrhosis
Ascites, variceal hemorrhage, jaundice, hepatic encephalopathy, or any
combination of these findings.
Ascites, which is the most frequent sign of decompensation, is present in 80%
of patients with decompensated cirrhosis.
Cirrhosis & its sequelae Dr. Khalid A. Al- Khazraji
Part 1
4-4-2016
3
Variceal hemorrhage
Present in approximately 50% of patients with newly diagnosed cirrhosis.
The prevalence of varices correlates with the severity of liver disease and
ranges from 40% in Child A
*
cirrhotic patients to 85% in Child C
*
cirrhotic
patients.
(
*
Child-Pugh score -
consists of five clinical features and is used to assess the
prognosis of chronic liver disease and cirrhosis).
The incidence of a first variceal hemorrhage in patients with small varices is
about 5% per year, whereas medium and large varices bleed at a rate of
approximately 15% per year.
Ascites
Occurs at a rate of 7 to 10% per year.
The most frequent symptoms associated with ascites are increased abdominal
girth.
Hepatorenal syndrome - Acute---Chronic
Hepatic encephalopathy
Occurs at a rate of approximately 2 to 3% per year.
Gradual onset and rarely fatal.
Clinically, it is characterized by alterations in consciousness and behavior
ranging from inversion of the sleep-wake pattern and forgetfulness; to
confusion, bizarre behavior, to lethargy to coma.
On physical examination, a distal tremor, asterixis. Additionally, sweet-
smelling breath, a characteristic termed fetor hepaticus.

Cirrhosis & its sequelae Dr. Khalid A. Al- Khazraji
Part 1
4-4-2016
4
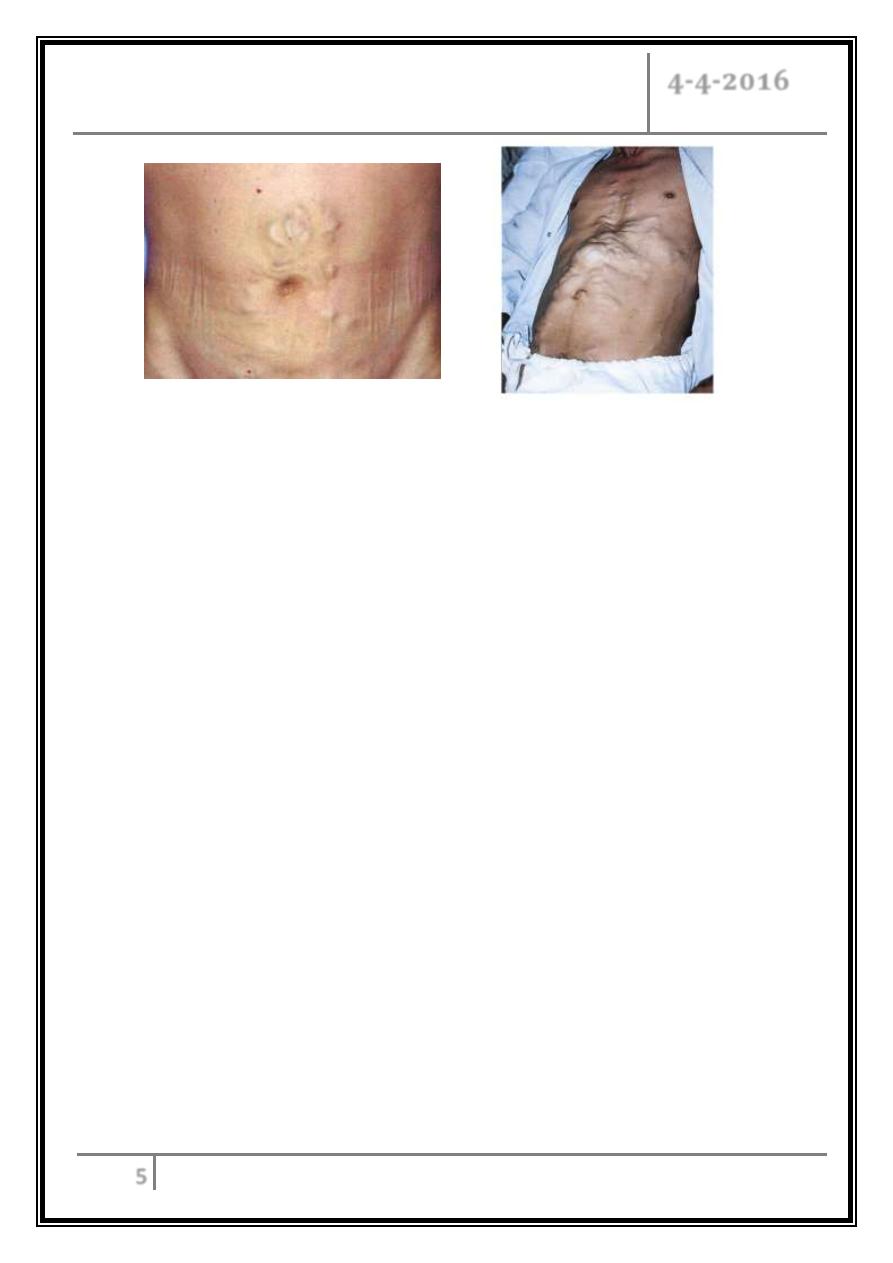
Palmar erythema
Dupuytren's contracture
Ascites
Cirrhosis & its sequelae Dr. Khalid A. Al- Khazraji
Part 1
4-4-2016
5
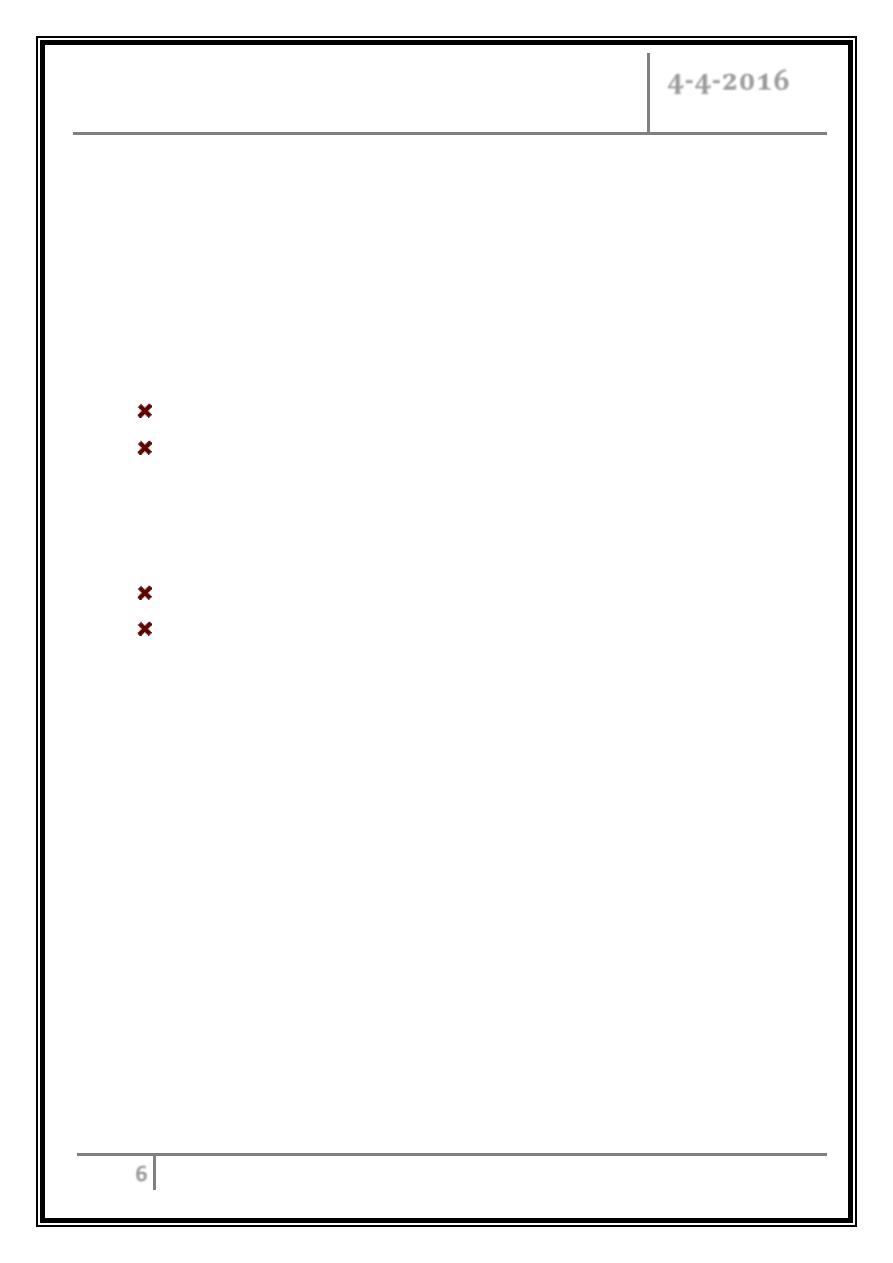
Caput medausae
DIAGNOSIS
The diagnosis of cirrhosis should be considered in any patient with chronic liver
disease.
In asymptomatic patients with compensated cirrhosis, diagnosis may often
require histologic confirmation by liver biopsy, which is the “gold standard” for
the diagnosis of cirrhosis.
In patients with symptoms or signs of chronic liver disease, confirmed
noninvasively by imaging studies without the need for liver biopsy.
Physical examination
Stigmata of cirrhosis consist of muscle atrophy, spider angiomas, and palmar
erythema. Males may have hair loss, gynecomastia, and testicular atrophy.
Petechiae and ecchymoses may be present as a result of thrombocytopenia or
a prolonged prothrombin time, Dupuytren’s contracture.
A pathognomonic feature of cirrhosis is small right liver lobe, with a span of
less than 7 cm on percussion, and a palpable left lobe that is nodular with
increased consistency. Splenomegaly may also be present and is indicative of
portal hypertension. Collateral circulation on the abdominal wall (caput
medusae).
Cirrhosis & its sequelae Dr. Khalid A. Al- Khazraji
Part 1
4-4-2016
6
Laboratory tests
o Subtle abnormalities in serum levels of albumin or bilirubin or elevation of
the international normalized ratio.
o Low platelet count, abnormal levels of aspartate aminotransferase, γ-
glutamyl transpeptidase.
Imaging studies
Computed tomography, ultrasound, and magnetic resonance imaging.
Findings consistent with cirrhosis include nodular contour of the liver, a
small liver with or without hypertrophy of the left or caudate lobe,
splenomegaly, and in particular, identification of intraabdominal collateral
vessels indicative of portal hypertension.
Transient elastography: measures liver stiffness.
In decompensated cirrhosis, detection of ascites, variceal bleeding, or
encephalopathy in the setting of chronic liver disease essentially establishes
the diagnosis of cirrhosis, so a liver biopsy is not necessary.
To be continued …
