Dr. Manal
Lec. 6
DYSLIPIDEMIA
Tues. 12 / 4 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Dyslipidemia Dr. Manal
12-4-2016
1
Dyslipidemia
Objectives
At the end of this lecture, students should be able to:
Define different types of lipoprotein and recognize their functions.
State the pathophysiology of atherosclerosis.
Identify the primary and secondary causes of hyperlipidemia.
Classify hyperlipoproteinemia.
Determine when to check lipids and their goals.
Outline the treatment lines of hyperlipidemia.
List the main antihyperlipidemic agents.
Case scenario
A 24- year old male patient is found to have a cholesterol level of 290 mg/ dL. He
notes that his mother and grandmother had problems with high cholesterol. He is
thought to have familial hypercholesterolemia.
What will you do next?
Introduction
Dyslipidemia Dr. Manal
12-4-2016
2
Definitions
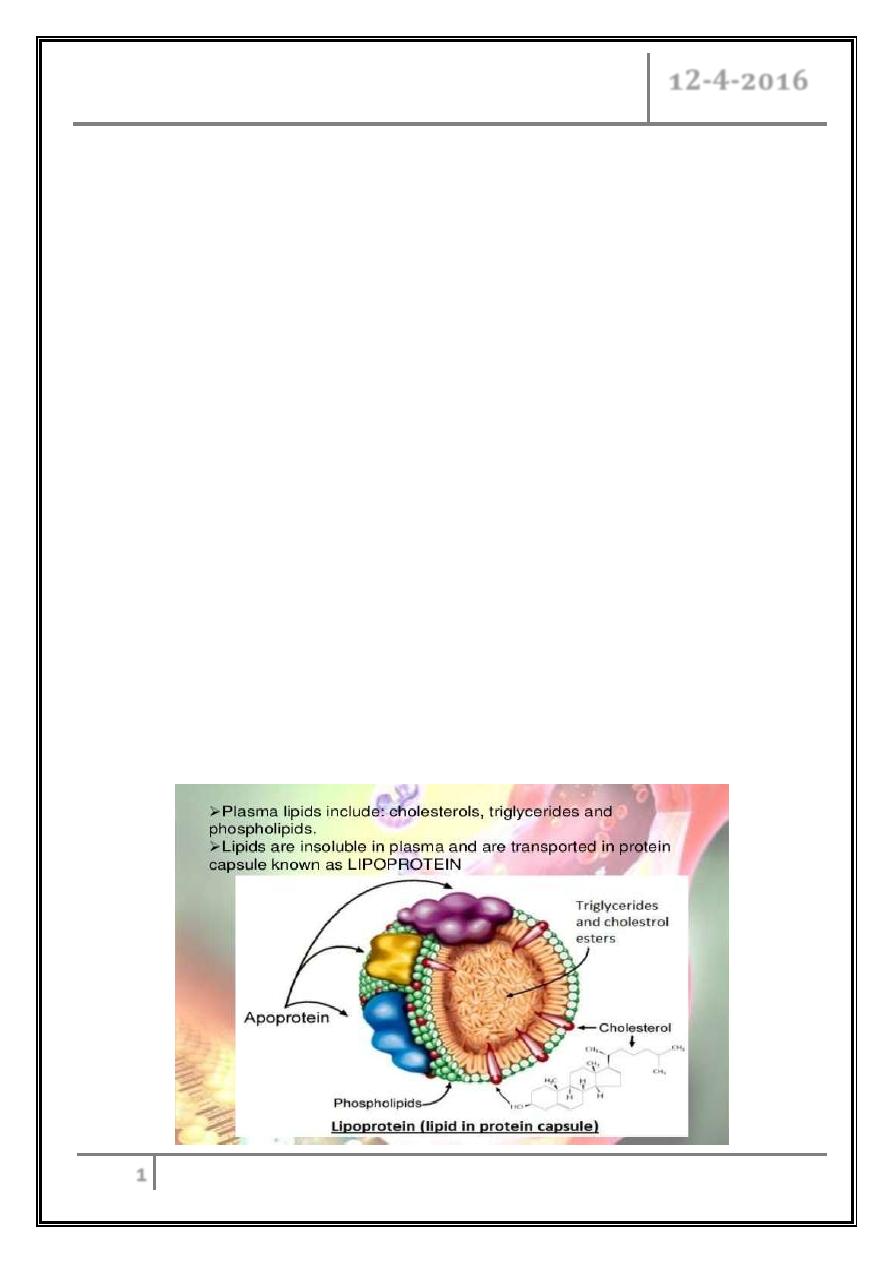
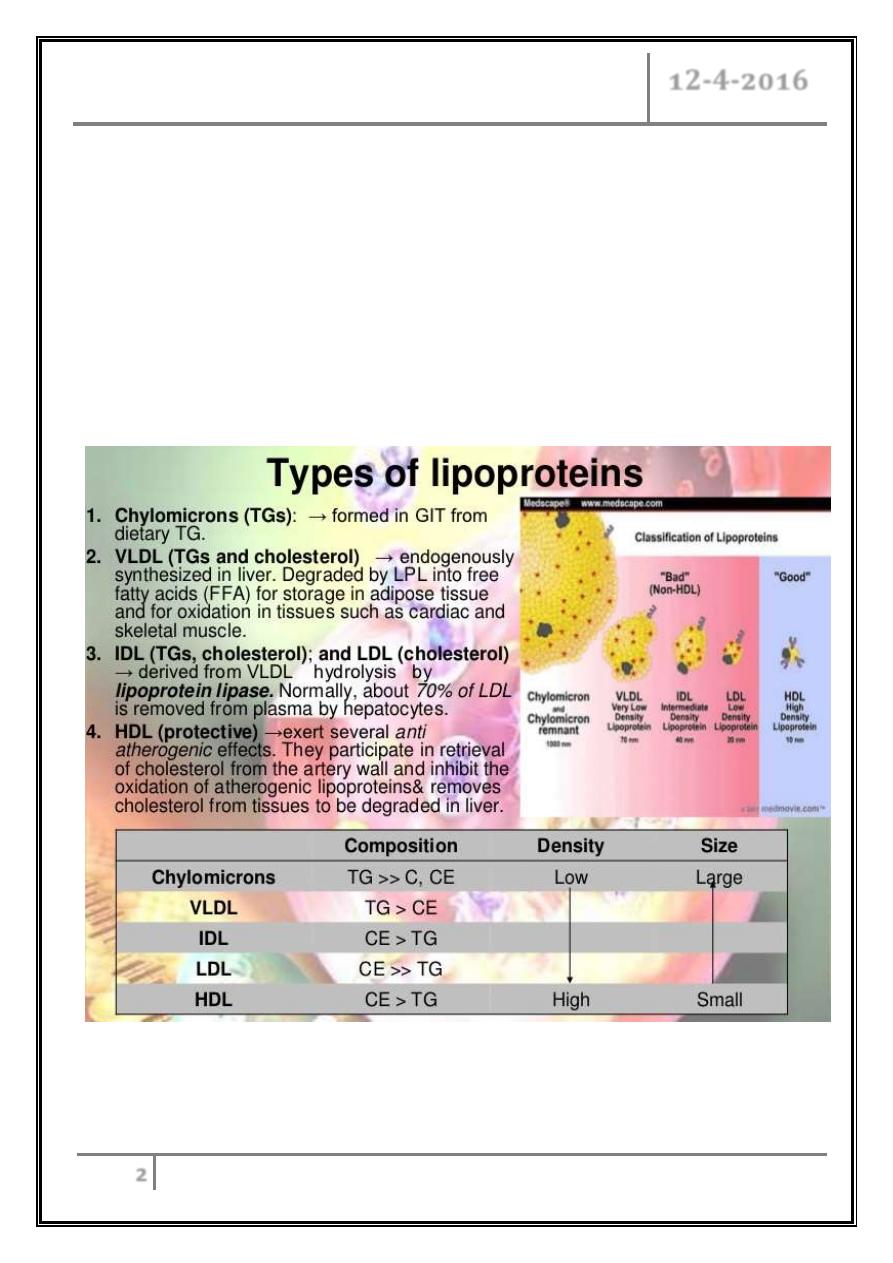
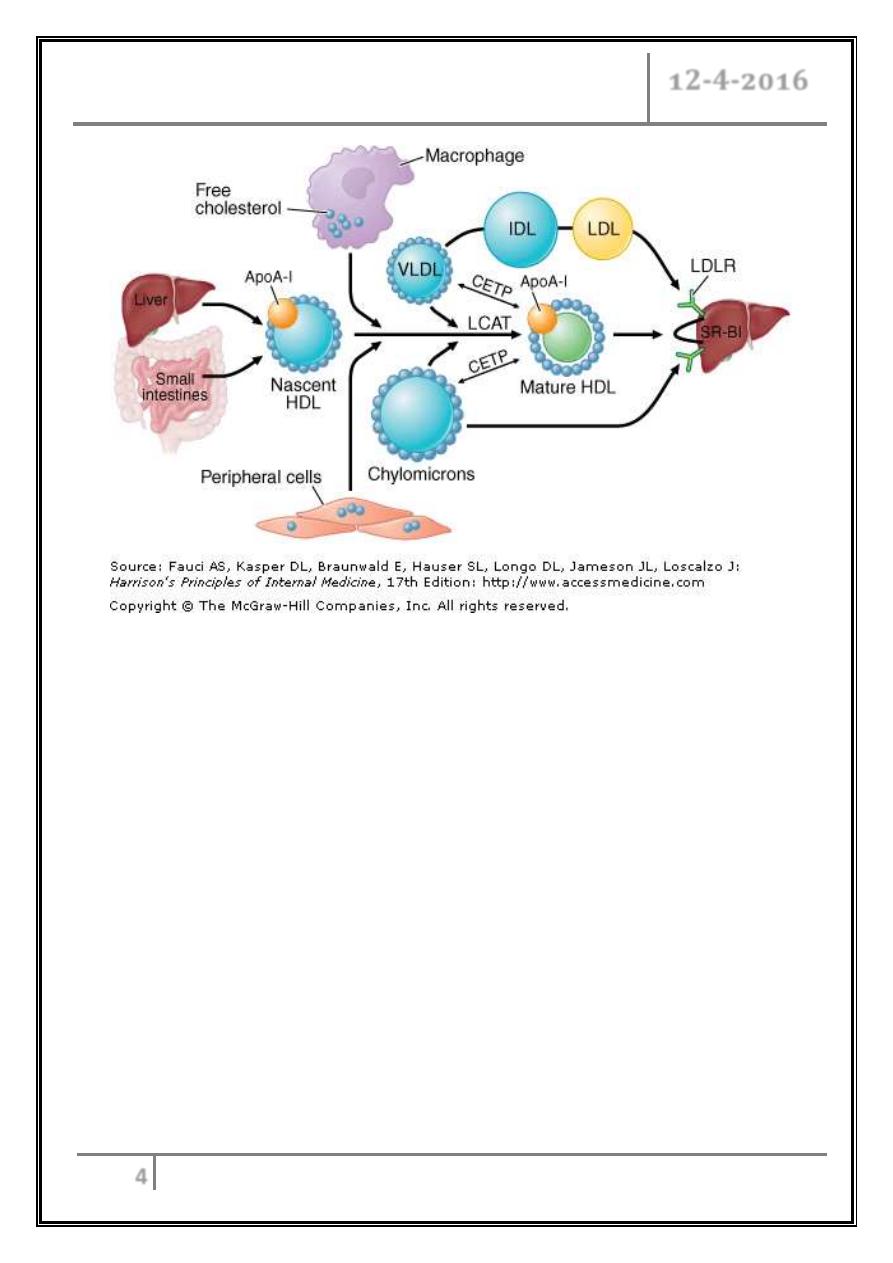
Lipids circulate in plasma as lipoproteins.
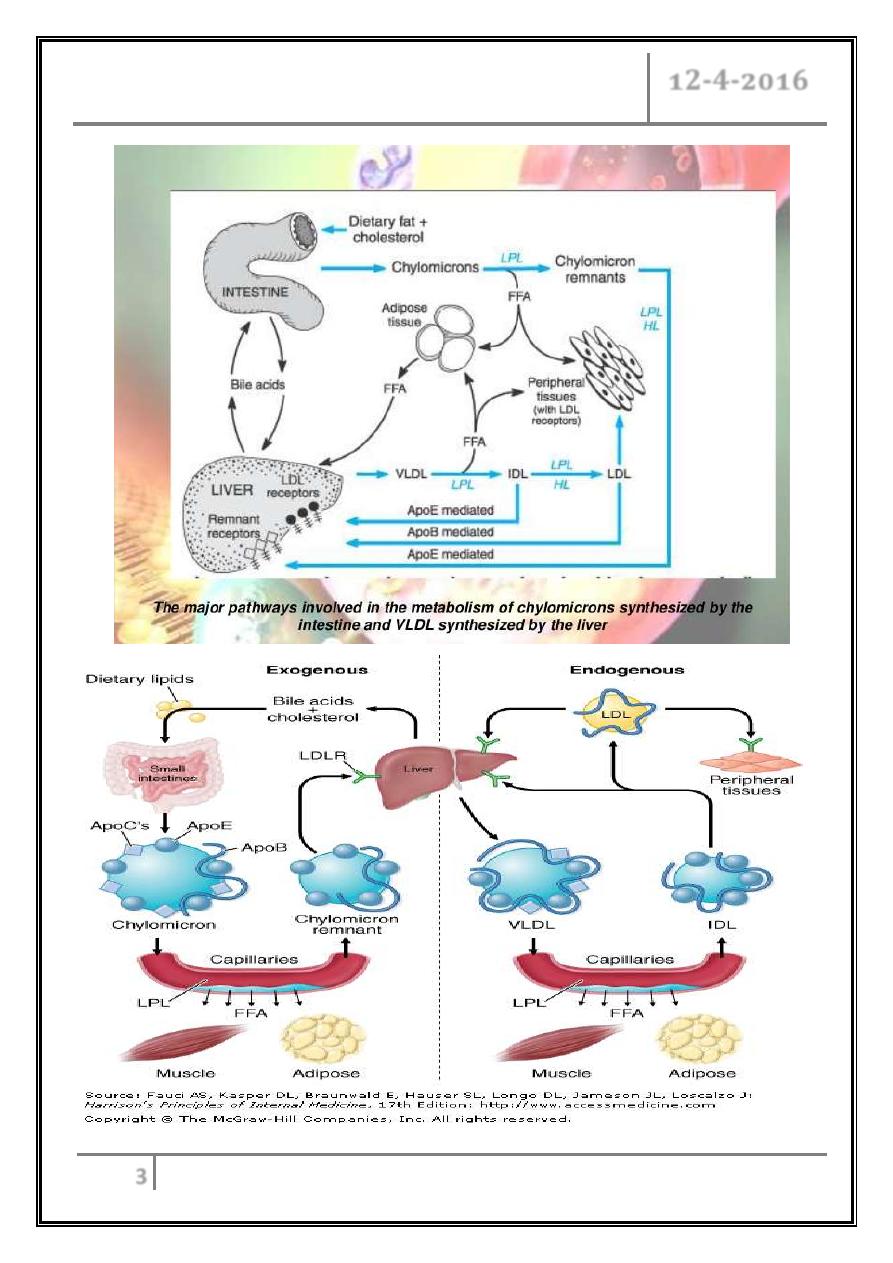
Chylomicrons transport fats from the intestinal mucosa to the liver.
In the liver, the chylomicrons release triglycerides and some cholesterol and
become low-density lipoproteins (LDL).
LDL then carries fat and cholesterol to the body’s cells.
High-density lipoproteins (HDL) carry fat and cholesterol back to the liver for
excretion.
Dyslipidemia Dr. Manal
12-4-2016
3
Dyslipidemia Dr. Manal
12-4-2016
4
HDL metabolism and reverse cholesterol transport
Dyslipidemia Dr. Manal
12-4-2016
5
Atherosclerosis
Pathophysiology of atherosclerosis
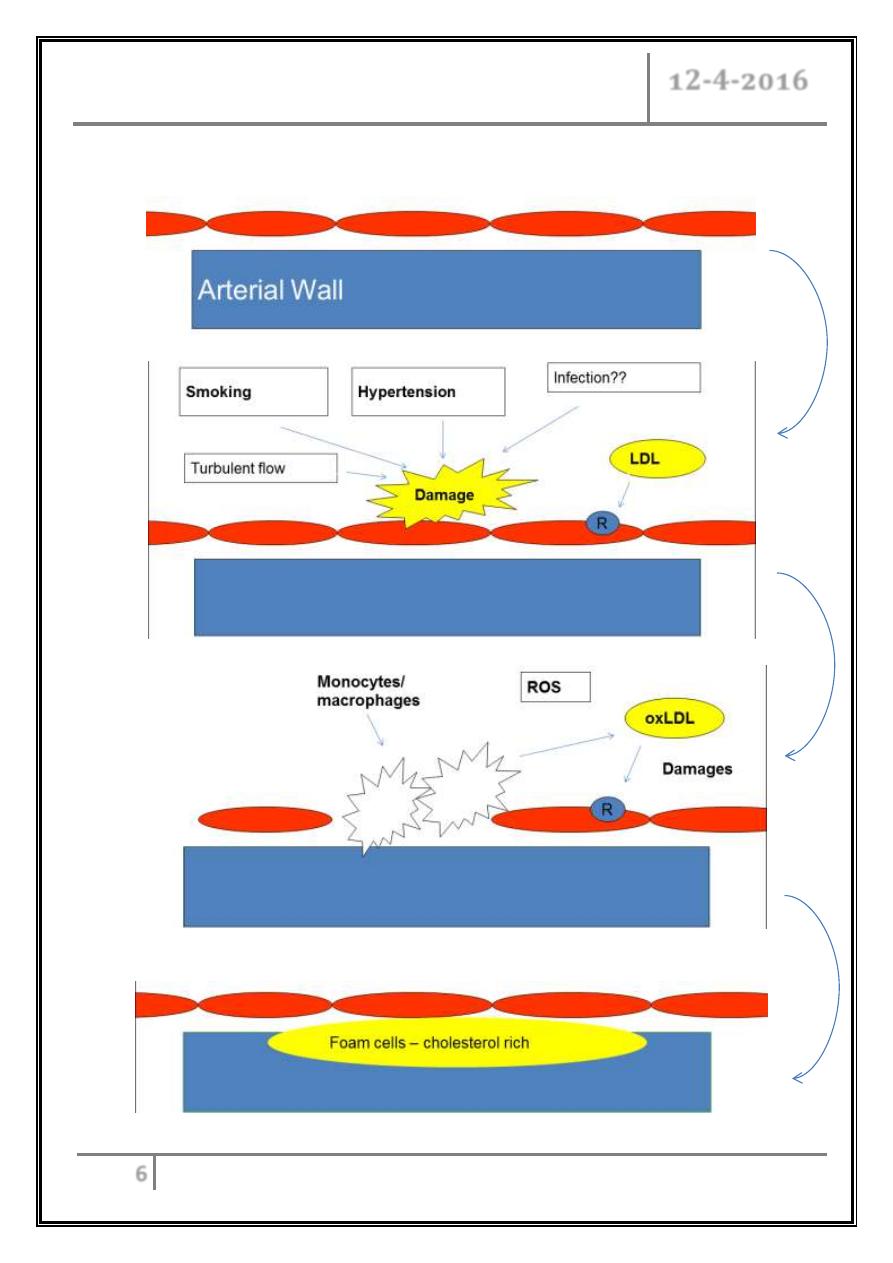
When oxidized LDL cholesterol gets high, it provokes inflammatory response, so
monocytes recruited & transformed into macrophages resulting in cholesterol
laden foam cell accumulation, which are beginnings of arterial fatty streaks,
then atheroma formation occurs, which causes atherosclerosis.
HDL cholesterol is able to go and remove cholesterol from the atheroma.
Atherogenic cholesterol → LDL, VLDL, IDL.
VLDL= TG/ 5.
Dyslipidemia Dr. Manal
12-4-2016
6
Atherogenesis: an inflammatory response to injury
ROS: reactive oxygen species
Dyslipidemia Dr. Manal
12-4-2016
7
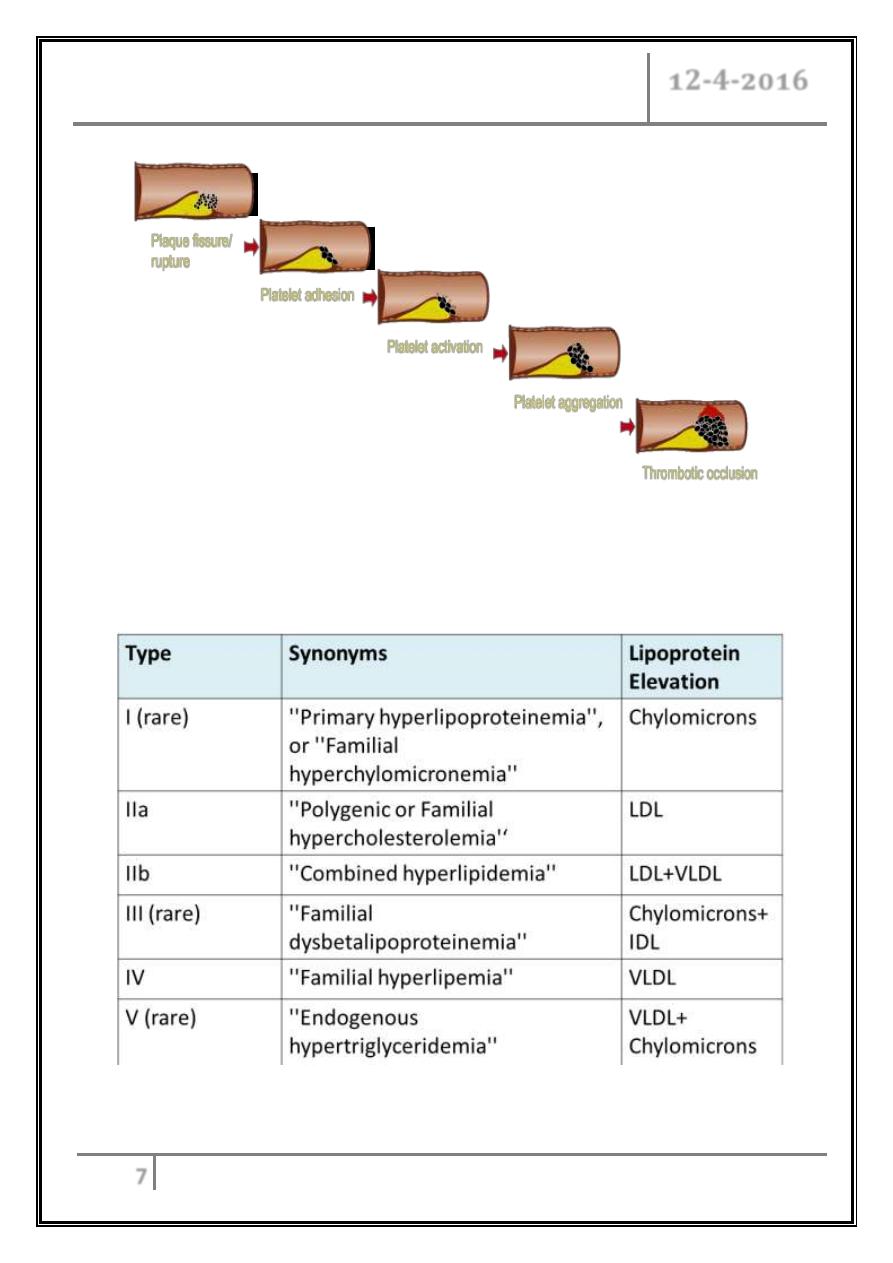
Hyperlipidemia hyperlipoproteinemia: abnormally increased plasma
lipoproteins - one of the risk factor for atherosclerosis.
Hyperlipemia: increased level of TG.
Hyperlipoproteinemia
Fredrickson classification
Dyslipidemia Dr. Manal
12-4-2016
8
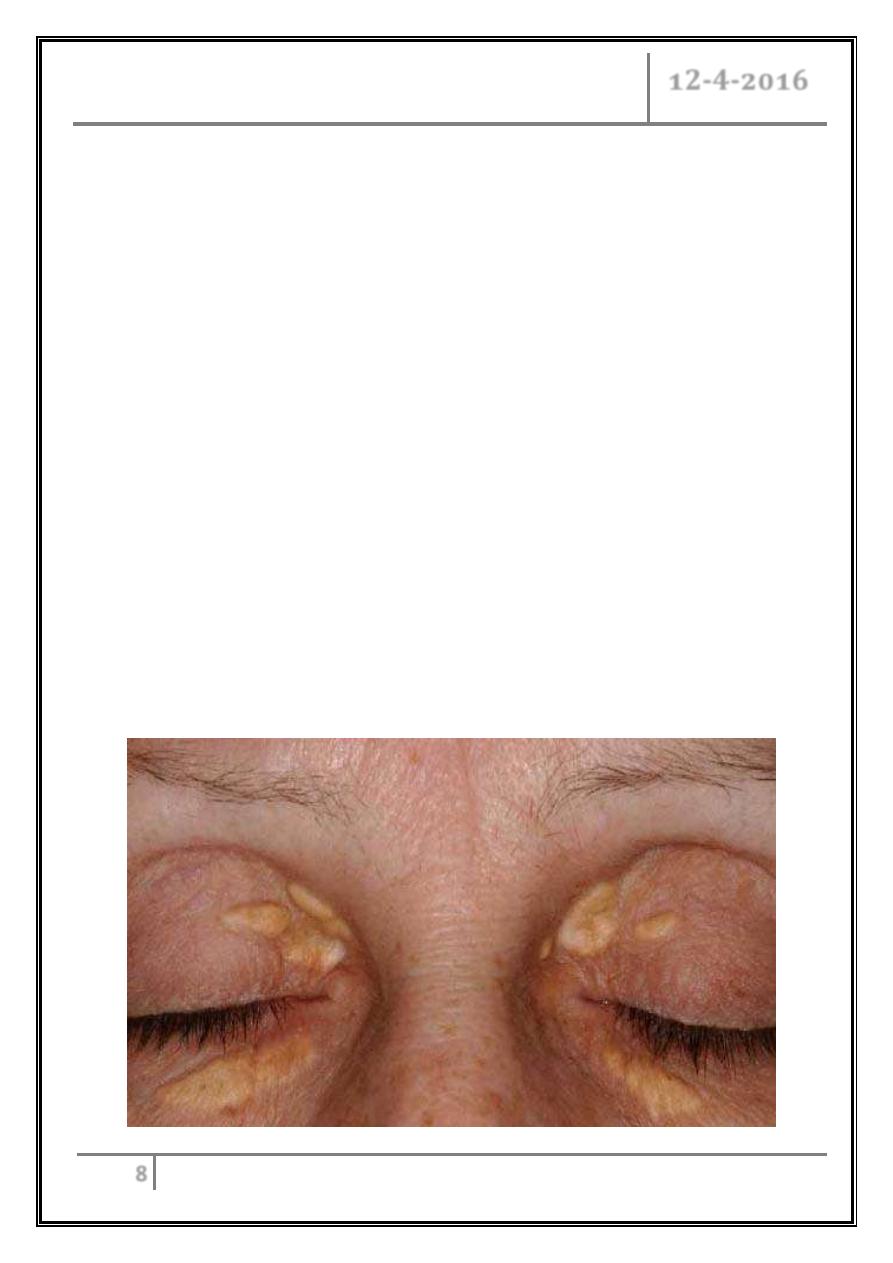
Hereditary causes of hyperlipidemia caused by known single gene mutations
Familial Hypercholesterolemia:
- Occurs in 1 in 500 individuals/ AD.
- Mutation in LDL receptor, resulting in elevated levels of LDL at birth and
throughout life.
- High risk for atherosclerosis, tendon xanthomas.
- and xanthelasmas of eyes, CHD.
Familial Combined Hyperlipidemia:
- Autosomal dominant.
- Increased secretions of LDL& VLDLs.
- High risk for atherosclerosis, no xanthomas.
Dysbetalipoproteinemia:
- Affects 1 in 10,000.
- A binding-defective form of apoE (which usually plays important role in
catabolism of chylomicron and VLDL).
- Increased risk for atherosclerosis, palmar xanthomas, CHD, PVD.
Dyslipidemia Dr. Manal
12-4-2016
9
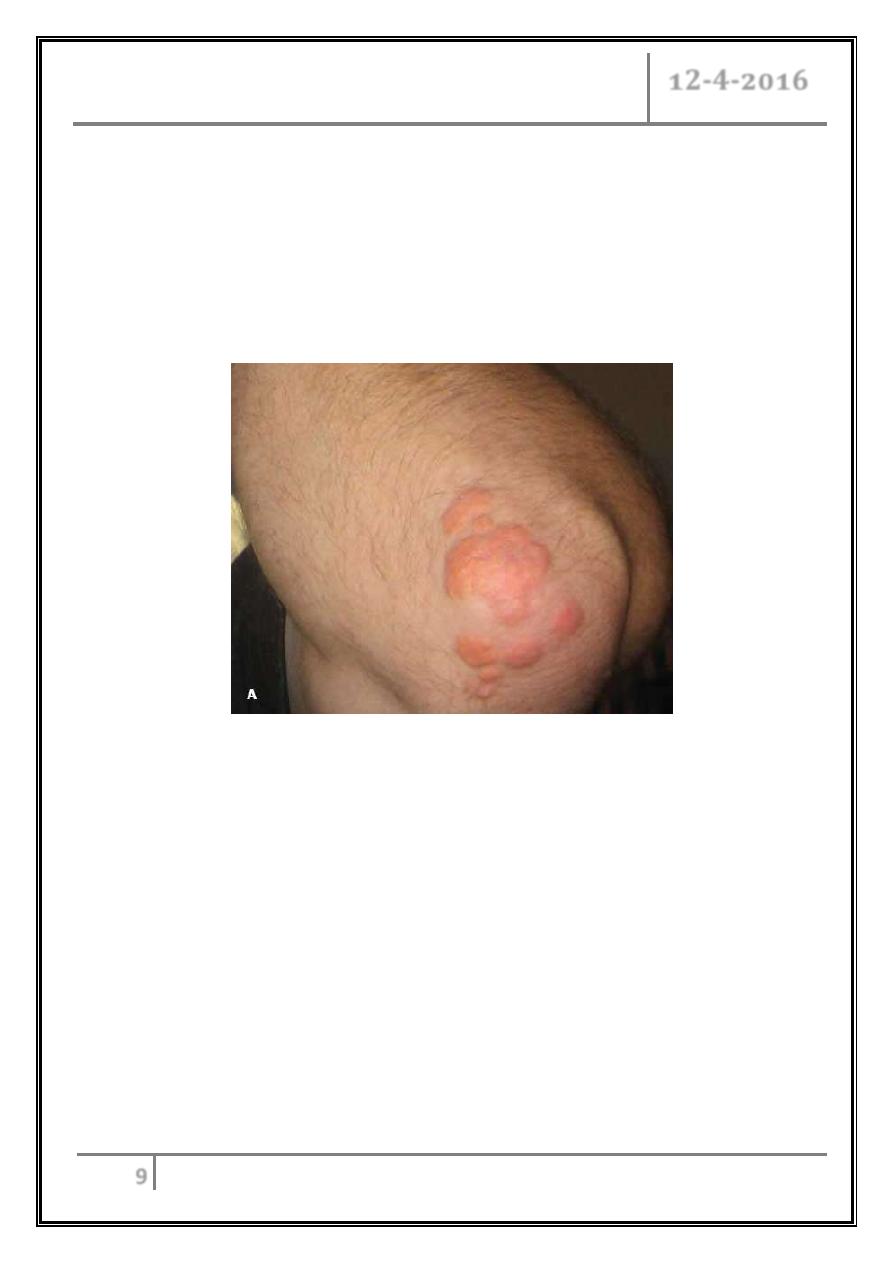
During a routine physical examination, flesh-colored papules were noted on
a 36-year-old man’s elbows, and knees. They had been present for a long
time, were nonpruritic, and had remained the same color and size. He had no
significant medical or surgical history and no medication allergy. He smoked
1 pack of cigarettes per day, drank alcohol socially. What is the name of his
lesion?
Secondary causes of lipoprotein abnormalities
o Hypercholesterolemia
- Hypothyroidism, cholestasis, nephrotic syndrome, drugs (progestogen,
cyclosporine, thiazides, steroids).
o Hypertriglyceridemia
- Obesity, DM, pregnancy, CRF, alcohol, stress, sepsis, acute hepatitis,
SLE, drugs (estrogen, β- blockers, steroids, interferon, thiazides), MM,
lymphoma, acromegaly.
o Low HDL
- Type-2 DM, rheumatoid arthritis, malnutrition, obesity, cigarette
smoking, beta blockers.
Dyslipidemia Dr. Manal
12-4-2016
10
What is the low density lipoprotein goal for a patient
with ischemic heart disease?
Checking lipids
Non
-
fasting lipid panel
- Measures HDL and total cholesterol.
Fasting lipid panel
- Measures HDL, total cholesterol and TG.
- LDL cholesterol is calculated:
LDL = total cholesterol – (HDL + TG/5)
When to check lipid panel?
Women aged 45 years and older, and men ages 35 years and older undergo
screening with a total and HDL cholesterol every 5 years.
If total cholesterol > 200 or HDL <40, then a fasting panel should be
obtained.
Cholesterol screening should begin at 20 years in patients with a history of
multiple CV risk factors, DM, or family history of either elevated cholesterol
levels or premature CVD.
Goals for lipids
LDL
-
< 100 →
Optimal
- 100-129 → Near optimal
- 130-159 → Borderline
- 160-189→ High
-
≥ 190 → Very High
Total Cholesterol
-
< 200 → Desirable
- 200-239 → Borderline
-
≥240 → High
Dyslipidemia Dr. Manal
12-4-2016
11
HDL
-
< 40 → Low
-
≥ 60 → High
Serum TG
-
< 150 → normal
- 150-199 → Borderline
- 200-499 → High
-
≥ 500 → Very High
Determining cholesterol goal (LDL!)
Cigarette smoking.
Hypertension (BP ≥140/90 or on treatment).
Low HDL cholesterol (< 40 mg/ dL).
Family History of premature coronary heart disease (CHD).
(CHD in first-degree male relative <55 or CHD in first-degree female
relative < 65).
Age (men ≥ 45, women ≥ 55).
LDL Goals
0 – 1 Risk factors:
- LDL goal is 160.
-
If LDL ≥ 160: Initiate TLC (therapeutic lifestyle changes).
-
If LDL ≥ 190: Initiate pharmaceutical treatment.
2 + Risk factors:
- LDL goal is 130.
-
If LDL ≥ 130: Initiate TLC.
-
If LDL ≥ 160: Initiate pharmaceutical treatment.
CHD or CHD risk equivalent:
- LDL goal is 100 (or 70).
-
If LDL ≥ 100: Initiate TLC and pharmaceutical treatment.
Dyslipidemia Dr. Manal
12-4-2016
12
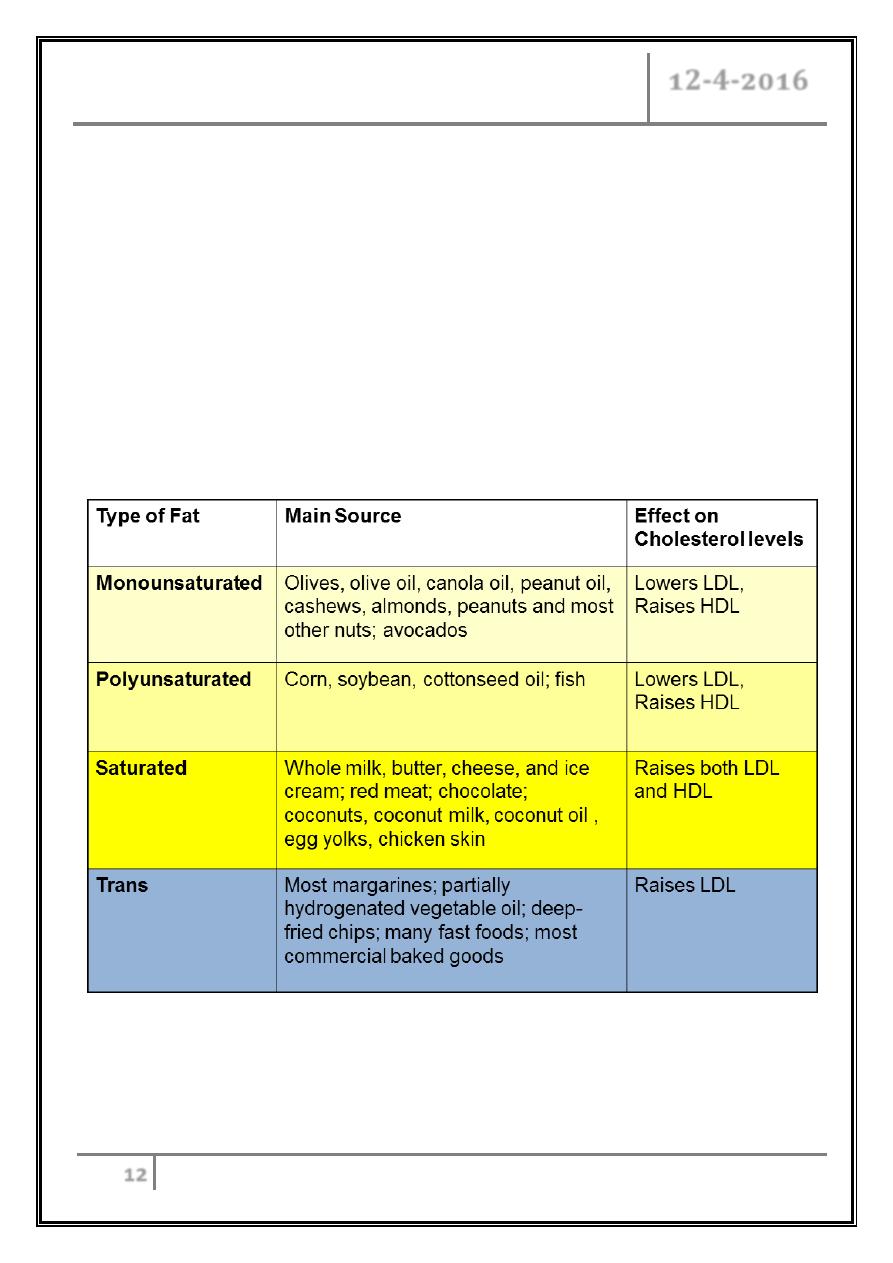
Treatment of hyperlipidemia
Therapeutic Lifestyle Changes (TLC):
Restricted total fat, saturated fats, cholesterol intake.
Moderate increase in polyunsaturated fat.
Increase soluble fiber intake.
Exercise: moderate intensity 30min/ day most days.
Weight reduction (initial goal of 10%) if needed.
Smoking cessation.
Treat HTN.
Dietary sources of cholesterol
Dyslipidemia Dr. Manal
12-4-2016
13
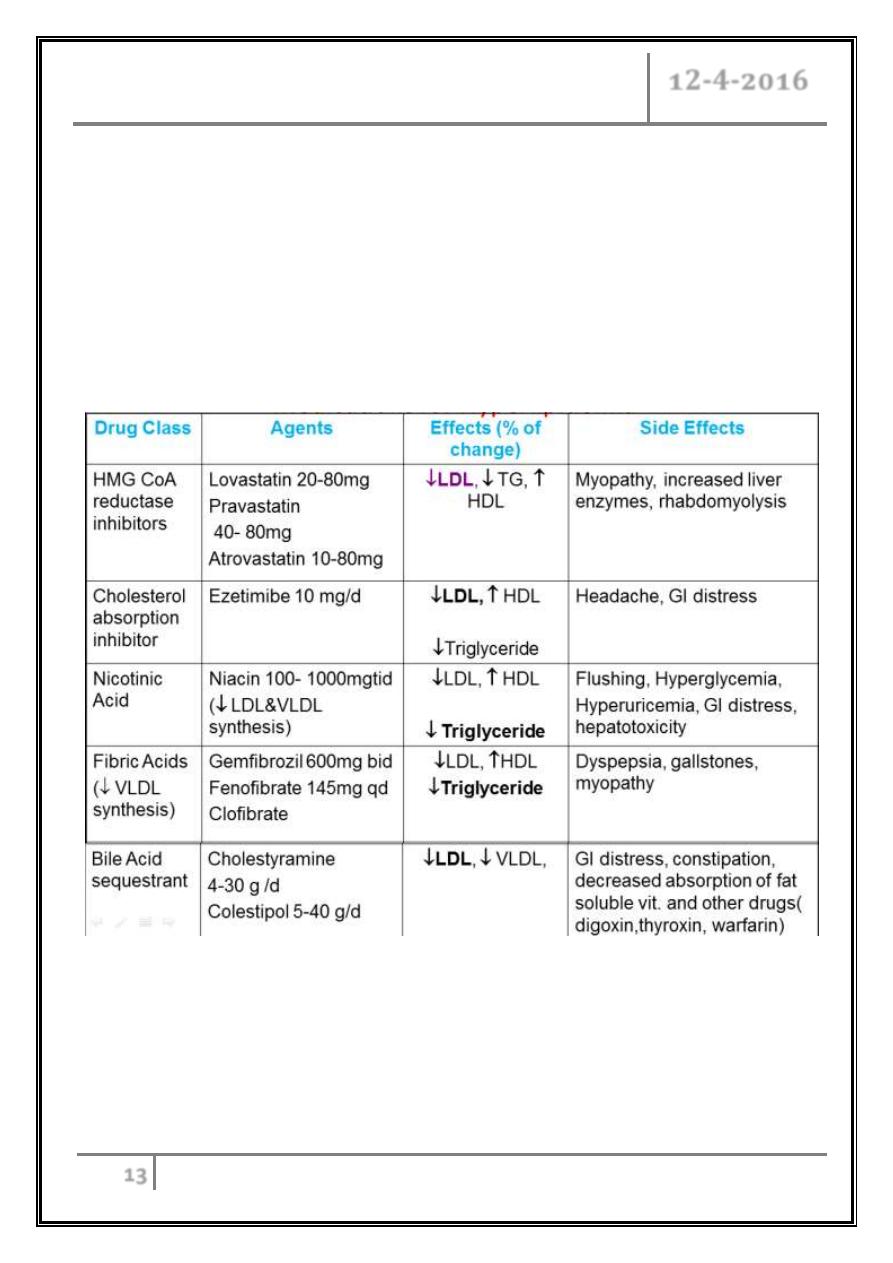
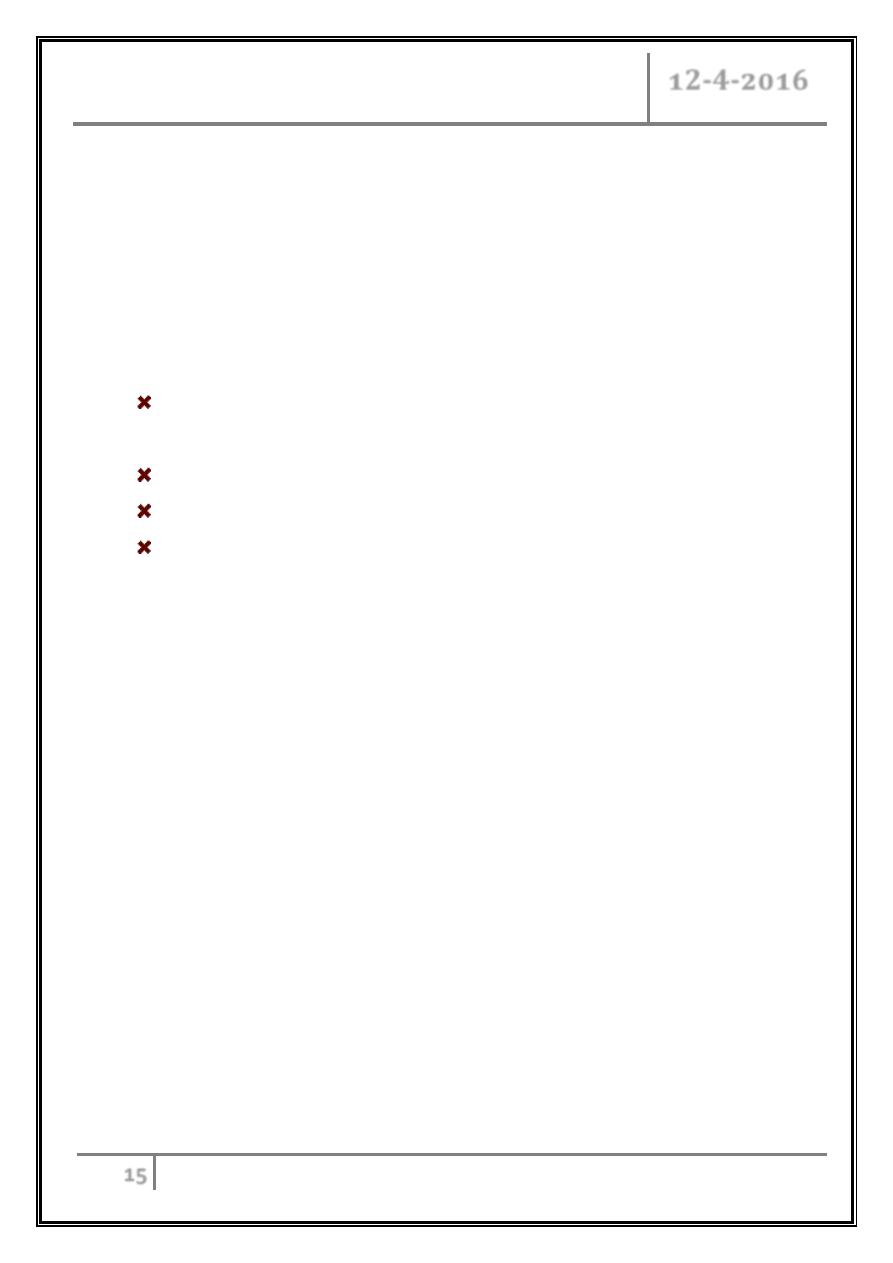
o Most patients should receive 3 m TLC trial before starting drugs unless very
high risk.
o If unable to reach goals with TLC alone choose lipid- lowering drugs based on
lipoprotein disorder.
o Combination therapy may be necessary.
o Medications for Hyperlipidemia
Drugs
Medications of hyperlipidemia
Dyslipidemia Dr. Manal
12-4-2016
14
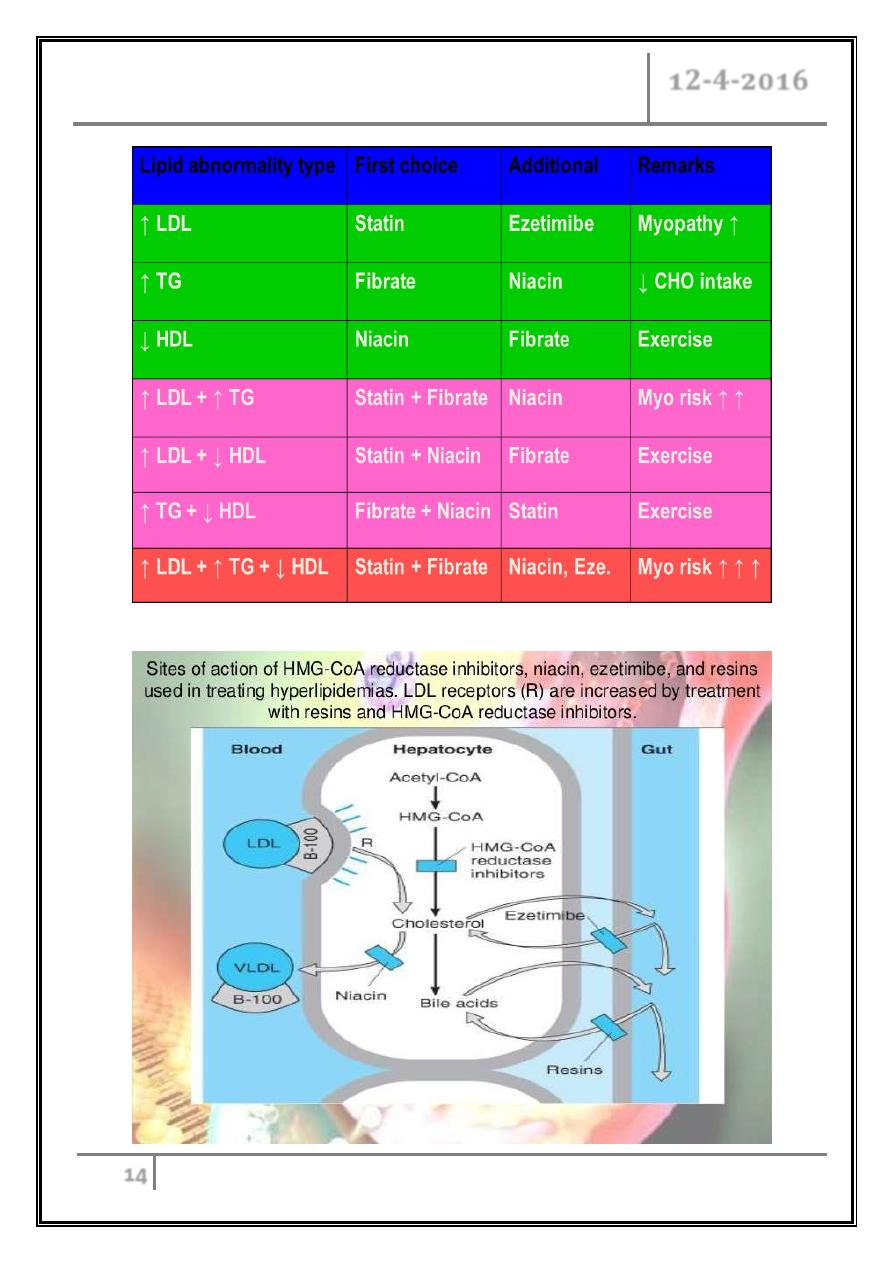
Summary of drug choice
Dyslipidemia Dr. Manal
12-4-2016
15
Back to the case of xanthomas
Total cholesterol level was 746 mg/ dL; triglyceride level, 1730 mg/ dL; and
HDL level, 38 mg/ dL. Low-density cholesterol was not calculable. The remainder
of the laboratory results was normal.
What is the treatment?
Omega 3 fatty acids
Diet rich in omega 3 FA (oil fish) decrease TC, TG, increase HDL &
decrease CV events.
FDA approved as dietary adjunct for very high TG levels ( > 500 mg/ dl).
< 3g daily is safe.
Adverse effects: thrombocytopenia, abnormal LFT, worsening glycemic
control, GI disturbance.
Hypertriglyceridemia
Associated with lipoprotein types I, III, IV, V.
Exclude primary disorders.
TLC:
- Achieve desirable body weight.
- Diet low in saturated fat, cholesterol.
- Regular exercise.
- Smoking cessation.
- Alcohol restriction.
Borderline- high TG+ CHD risk factors:
- FH of premature CHD.
- Concomitant LDL elevation or low HDL.
- Genetic forms associated with CHD (familial dysbetalipoproteinemia and
familial combined hyperlipidemia
- Consider initiation of niacin.
Dyslipidemia Dr. Manal
12-4-2016
16
Alternative therapies:
- Gemfibrozil, statins, fish oil, fibrates.
Very high TG (> 500 mg/ dL) associated with pancreatitis.
Genetic form often coexists with other causes like DM.
Medications:
- Gemfibrozil: preferred in diabetics.
- Niacin.
- Higher potency statins.
- Fenofibrate.
Low level of HDL cholesterol is a risk factor for coronary heart
disease, true or false?
Low HDL- C
Strong CHD risk predictor.
Causes:
- . DM type 2.
- Physical inactivity.
- Insulin resistance.
- Cigarette smoking.
- Very high carbohydrate intake
Treatment:
- TLC, drugs (fibric acid derivatives, niacin).
Dyslipidemia Dr. Manal
12-4-2016
17
Summery
Dyslipidemia is elevation of plasma cholesterol, TG, or both, or a low HDL
level that contributes to the development of atherosclerosis.
Causes may be primary (genetic) or secondary. Diagnosis is by measuring
plasma levels of total cholesterol, TG, and individual LP.
Treatment is dietary changes, exercise, and lipid lowering drugs.
References:
Davidson’s Principles& Practice of Medicine.
Harrison’s Principles of Internal Medicine.
… END …
