Dr. Omar Al- Azzawy
Lec. 7
THE THYROID GLAND –
PART 2
Thur. 25 / 2 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
1
The thyroid gland
Thyroid crisis (thyroid storm)
Thyroid storm is an acute form of hyperthyroidism that results from either
unrecognized untreated or inadequately treated severe hyperthyroidism. It is a
rare medical emergency, which has a mortality of 10% despite early recognition
and treatment.
Precipitated by infection, trauma, surgery, or any other stressful condition.
Presents with florid symptoms of hyperthyroidism with one or more of the
following: fever, agitation confusion, psychosis, coma, tachycardia or atrial
fibrillation, cardiovascular collapse, and shock.
Treatment of thyroid storm
Patients should be rehydrated.
Give propranolol, either orally (80 mg 4 times daily) or intravenously (1–5
mg 4 times daily). It helps in controlling adrenergic symptoms and also
reduces the peripheral conversion of T4 to T3 (propranolol only in high
doses).
Sodium ipodate (500 mg per day orally) will restore serum T3 levels to
normal in 48–72 hours (inhibits the release of thyroid hormones, and
reduces the peripheral conversion of T4 to T3.
Dexamethasone (2 mg 4 times daily) also reduces the peripheral conversion
of T4 to T3.
Oral carbimazole 40–60 mg daily should be given to inhibit the synthesis of
new thyroid hormone.
If the patient is unconscious or uncooperative, carbimazole can be
administered rectally with good effect.
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
2
Atrial fibrillation in thyrotoxicosis
Occurs in about 10% of patients with thyrotoxicosis. The incidence increases
with age, so that almost half of all males with thyrotoxicosis over the age of 60
are affected.
Characteristically and specifically, the ventricular rate is little influenced by
digoxin, but responds to the addition of a β-blocker.
Thromboembolic complications are common in thyrotoxic atrial fibrillation so
anticoagulation with warfarin is required, unless contraindicated.
Subclinical thyrotoxicosis
Serum TSH is undetectable or very low, and serum T3 and T4 are at the upper
end of the normal range.
This is most often found in older patients with multinodular goitre.
These patients are at increased risk of atrial fibrillation and osteoporosis, and
hence the consensus view is that they have mild thyrotoxicosis and require
therapy, usually with
131
I.
Otherwise, annual review is essential, as the conversion rate to overt
thyrotoxicosis is about 5% each year.
Hypothyrodism
o Hypothyroidism is a state of thyroid hormone deficiency.
o Occurs at any age but is particularly common among the elderly, 10% of
women and 6% of men > 65 are affected.
o In all age group women are 6 times more frequently affected than men.
o High calcitonin concentration can be an indicator of medullary thyroid
carcinoma.
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
3
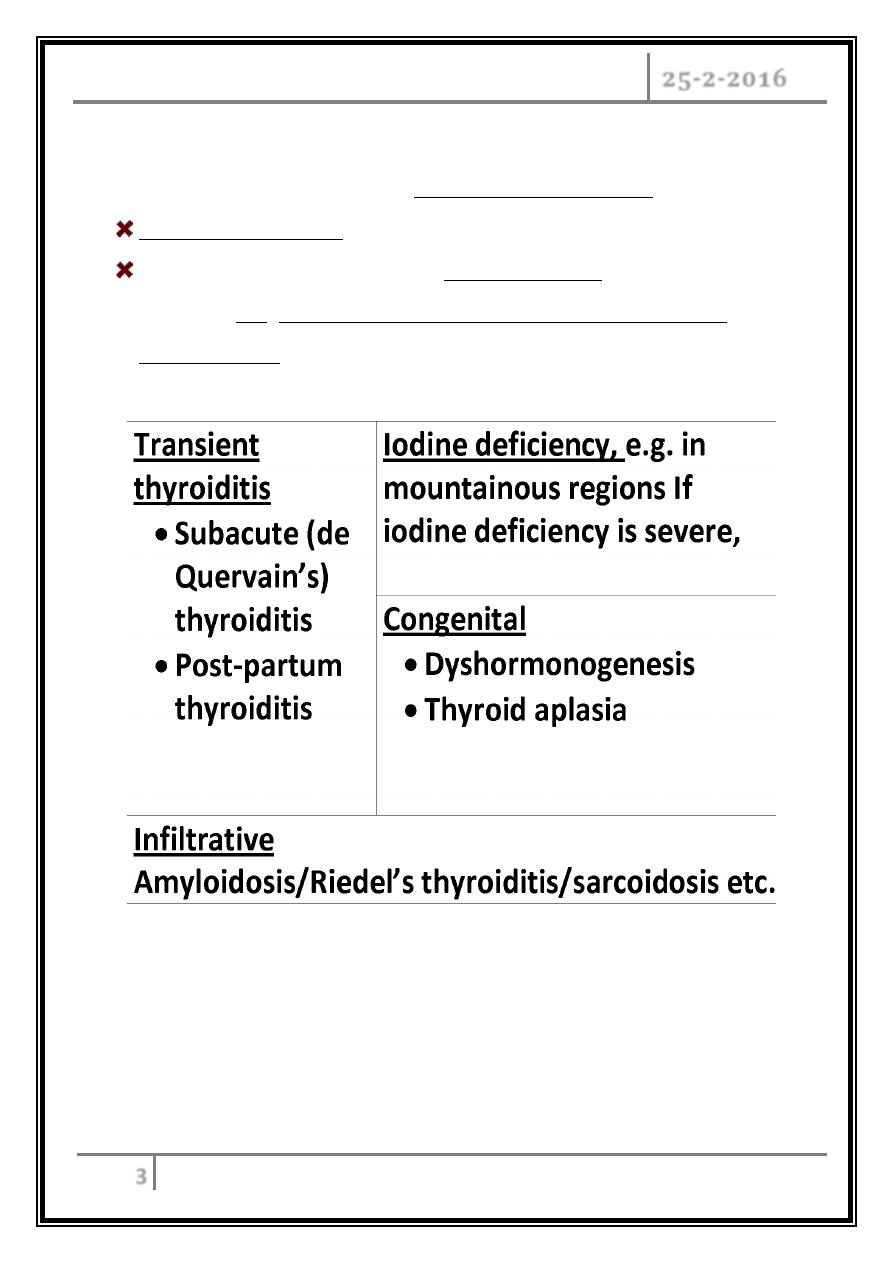
Causes
The most common cause of primary hypothyroidism is
Autoimmune disease that usually results from Hashimoto's thyroiditis.
The 2nd most common cause is post-therapeutic hypothyroidism,
following
131
I, surgical treatment of thyrotoxicosis and goiter or
overtreatment with antithyroid drugs. Both accounts for over 90% of
causes, others are:
Secondary hypothyroidism
Occurs when the hypothalamus produces insufficient thyrotropin-releasing
hormone (TRH) or the pituitary produces insufficient TSH.
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
4
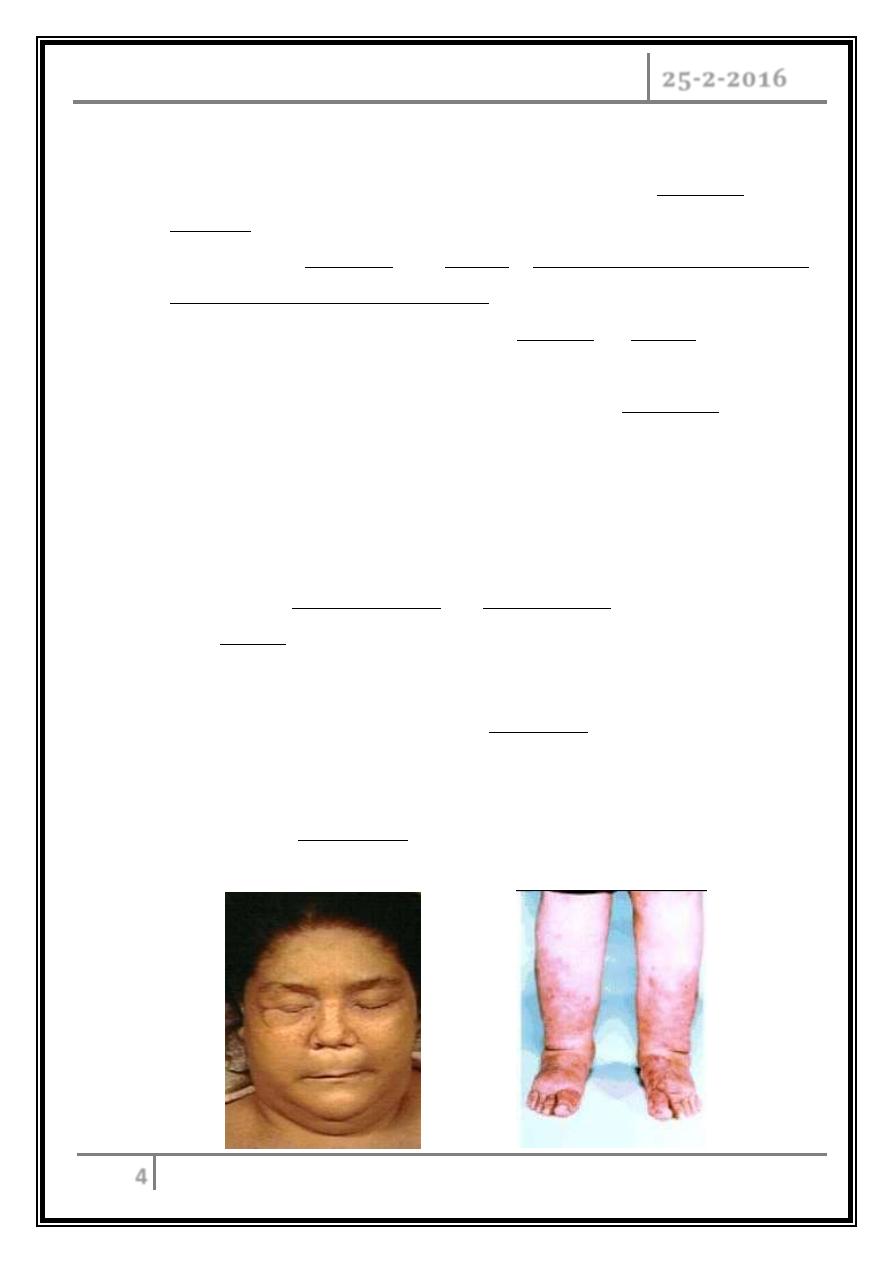
Clinical features of hypothyroidism
Symptoms and signs of primary hypothyroidism are often subtle and
insidious.
It may manifest atypically in the elderly as confusion, anorexia, weight loss,
incontinence, and decreased mobility.
The clinical presentation depends on the duration and severity of the
disease.
A prolonged duration of hypothyroidism, leads to the infiltration of many
body tissues by:
- Mucopolysaccharides,
- Hyaluronic acid, and
- Chondroitin sulphate,
resulting in a low-pitched voice and slurred speech due to a large tongue,
poor hearing, and compression of the median nerve at the wrist (carpal
tunnel syndeome with paresthesias of the hands).
Infiltration of the dermis gives rise to non-pitting oedema (myxedema),
which is most marked in the skin of the hands, feet, face, and eyelids,
resulting in periorbital and facial puffiness with dull facial expression
combined with facial pallor due to vasoconstriction, anemia, or a lemon-
yellow tint of the skin caused by carotenaemia.
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
5
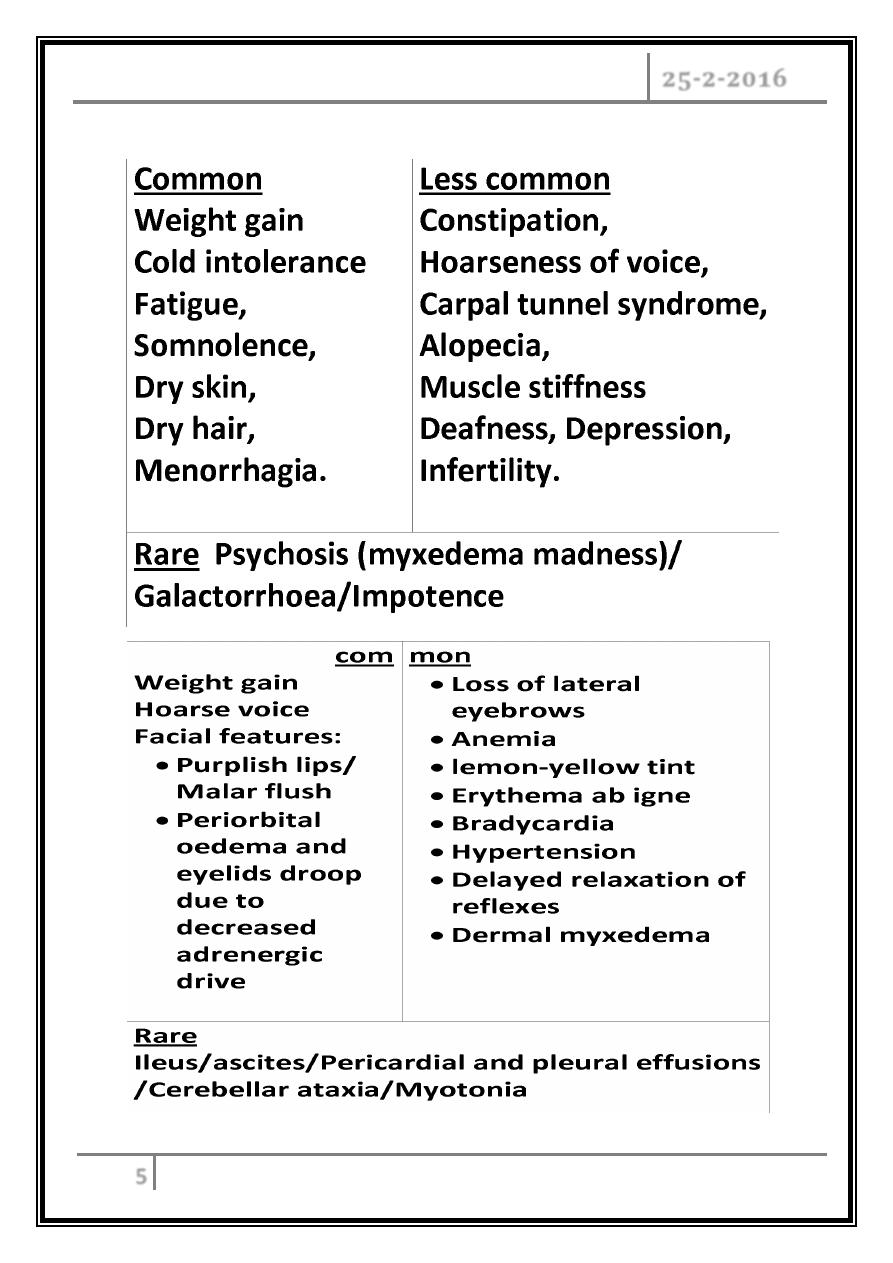
Other symptoms are
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
6
Investigations
In primary hypothyroidism, the serum T4 is low and TSH is elevated, usually in
excess of 20 mU/L.
Measurements of serum T3 are unhelpful since they do not discriminate reliably
between euthyroidism and hypothyroidism.
Measurement of thyroid peroxidase antibodies, although +ve in many different
etiologies, is sometimes helpful.
Other non-specific abnormalities are:
Raised serum enzymes: creatine kinase, aspartate aminotransferase, lactate
dehydrogenase (LDH).
Hypercholesterolemia.
Anemia: normochromic normocytic or macrocytic.
Hyponatremia.
ECG classically demonstrates sinus bradycardia with low-voltage complexes
and ST segment and T-wave changes.
Treatment
It’s with levothyroxine (T) replacement.
In patients with known ischemic heart disease and elderly, thyroid hormone
replacement should be introduced at a low dose of 25 μg per day, and increased
very slowly, to finally reach a maintenance dose of 100–150 μg per day.
In younger patients, it is safe to initiate levothyroxine at a higher dose 100 μg
per day.
Aim to maintain serum TSH within the reference range, to achieve this, serum
T4 should be in the upper part of the normal range.
Levothyroxine has a half-life of 7 days so it should always be taken as a single
daily dose, absorption is maximal when the dose is taken before bed and may be
further optimized by taking vitamin C supplement.
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
7
At least 6 weeks should pass before repeating thyroid function tests and
adjusting the dose, usually by 25 μg/ day.
Measure thyroid function every 1–2 years once the dose of T4 is stabilized.
Patients feel better within 2–3 weeks. Reduction in weight and periorbital
puffiness occurs quickly, but the restoration of skin and hair texture and
resolution of any effusions may take 3–6 months.
Situations in which an adjustment of the dose of T4 is necessary are:
1- Pregnancy.
Increases concentration of serum thyroxine-binding globulin, require an
increase in the dose of levothyroxine of approximately 25–50 μg daily.
Inadequate maternal T4 therapy may be associated with impaired cognitive
development in an unborn child.
2- Malabsorption.
3- Drugs:
- Drugs that increase T4 clearance: phenobarbital, phenytoin,
carbamazepine, rifampicin, sertraline, chloroquine.
- Drugs that interfere with intestinal T4 absorption: colestyramine,
sucralfate, aluminium hydroxide, ferrous sulphate, dietary fibre
supplements, calcium carbonate.
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
8
Subclinical hypothyroidism
It’s an elevated serum TSH level in patients with absent or minimal symptoms of
hypothyroidism and normal serum levels of free T4.
It is relatively common; occurs in more than 15% of elderly women and 10% of
elderly men.
In patients with serum TSH > 10 mU/L, there is a high likelihood of progression
to overt hypothyroidism.
These patients are also more likely to have hypercholesterolemia and
atherosclerosis. They should be treated with T4, even if they are asymptomatic.
For patients with TSH levels between 4.5 and 10 mU/L, use of T4 is reasonable
if symptoms of early hypothyroidism (e.g. fatigue, depression) are present,
Therapy is also indicated in pregnant and women who plan to become pregnant
to avoid effects of hypothyroidism on the pregnancy and fetal development.
Patients should have annual measurement of serum TSH and free T4 to assess
progress of the condition if untreated or to adjust the T4 dosage.
Non-thyroidal illness (‘sick euthyroidism’)
This presents with a low serum TSH, raised T4 and normal or low T3, in a patient
with systemic illness who doesn't have clinical evidence of thyroid disease. These
abnormalities are due to:
Decreased peripheral conversion of T4 to T3,
Altered levels of binding proteins and their affinity for thyroid hormones,
Reduced secretion of TSH.
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
9
Myxedema coma
The condition usually occurs in patients with long-standing, undiagnosed
hypothyroidism and is usually precipitated by infection, cerebrovascular disease, heart
failure, trauma, or drug therapy.
It has a 50% mortality rate and needs urgent treatment.
Pathophysiology
Long-standing hypothyroidism is associated with reduced metabolic rate and
decreased oxygen consumption, which affects all body systems resulting in:
Hypothermia,
Cardiac contractility is impaired, leading to reduced stroke volume, low
cardiac output, bradycardia and hypotension and pericardial effusions.
Respiratory depression (central), hypoventilation with CO2 retention.
Brain function is affected by:
- Reduction in oxygen delivery.
- Decreased glucose utilization.
- Reduced cerebral blood flow.
Rapid diagnosis based on clinical judgment, history, and physical examination
is imperative, because death is likely without rapid treatment. So treatment must
begin before biochemical confirmation of the diagnosis.
The thyroid gland - Dr. Omar Al- Azzawy Part 2
25-2-2016
10
Treatment
Maintenance of adequate airway is crucial, since most patients have
depressed mental status with respiratory failure. Mechanical ventilation is
usually required during the first 36-48 hours.
Intravenous injection of 20 μg triiodothyronine, (T3)/ 3 times daily until
there is sustained clinical improvement.
Or an intravenous loading dose of 300-600 micrograms of levothyroxine
(T4) followed by a daily intravenous dose of 50-100 micrograms.
Corticosteroids are also given, because the possibility of central
hypothyroidism usually cannot be initially ruled out.
Treat hypothermia with passive rewarming using ordinary blankets and a
warm room. Active rewarming using external devices carries a risk of
vasodilatation and worsening hypotension and should be avoided.
The precipitating factor should be rapidly treated.
… END …
