Dr. Rabah
Lec. 4
MALABSORPTION & PROTEIN
LOSING ENTEROPATHY – PART 2
Wed. 30 / 3 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Malabsorption & protein losing Dr. Rabah
enteropathy – Part 2
30-3-2016
1
Malabsorption & protein losing enteropathy – Part 2
Malabsorption
Tropical sprue
Chronic malabsorption in a patient from the tropics, associated with
abnormalities of small intestinal structure and function.
5-10% of tropical areas’ population is affected.
Etiology
Pathogenesis of tropical sprue is uncertain.
Infective agent:
- Often begins after an acute diarrhoeal illness.
- Isolation of Escherichia coli, Enterobacter and Klebsiella.
- Response to Abs.
Folic acid deficiency.
Clinical features
o Chronic diarrhea.
o Abdominal distension.
o Anorexia, fatigue.
o Weight loss.
o Features of malabsorption:
- Megaloblastic anaemia (folic acid malabsorption).
- Other deficiencies.
The course of the disease
Remissions and relapses may occur.
The differential diagnosis
Infective cause of diarrhea.
- Giardiasis.
Malabsorption & protein losing Dr. Rabah
enteropathy – Part 2
30-3-2016
2
Diagnosis
Chronic diarrhea plus malabsorption.
Patient in tropics.
Small-intestinal mucosal biopsy partial villous atrophy.
No response to GFD.
Management
Tetracycline 250 mg 6-hourly with folic acid (5 mg daily) for 28 days is the
treatment of choice.
Small bowel bacterial overgrowth (blind loop
syndrome)
A group of disorders with diarrhea, steatorrhea, and macrocytic anemia due to
the proliferation of colonic-type bacteria within the small intestine
The normal duodenum and jejunum contain less than 104 * 10
3
organisms/ ml.
Pathophysiology
Disorders which impair the normal physiological mechanisms controlling
bacterial proliferation in the intestine causing:
Deconjugation of bile acids.
Bacterial utilisation of vitamin B12.
Malabsorption & protein losing Dr. Rabah
enteropathy – Part 2
30-3-2016
3
Etiology
Hypo- or achlorhydria
- Pernicious anaemia.
- Partial gastrectomy.
- Long-term PPI therapy.
Impaired intestinal motility
- Scleroderma.
- Diabetic autonomic neuropathy.
- Chronic intestinal pseudo-obstruction.
Structural abnormalities
- Gastric surgery (blind loop after Billroth II operation).
- Jejunal diverticulosis.
- Enterocolic fistulas (e.g. Crohn's disease).
- Strictures (e.g. Crohn's disease).
Impaired immune function
- Hypogammaglobulinaemia.
Clinical features
Watery diarrhoea and/or steatorrhoea.
Anemia due to B12 deficiency.
Symptoms from the underlying intestinal cause.
Investigations
Barium follow-through may reveal blind loops or fistulas.
Endoscopic duodenal biopsies exclude mucosal disease such as coeliac
disease.
Jejunal contents for bacteriological examination can be aspirated at
endoscopy.
Schilling test abnormal.
Serum vitamin B12 concentration is low.
Malabsorption & protein losing Dr. Rabah
enteropathy – Part 2
30-3-2016
4
Management
o Surgical treatment of the underlying cause.
o B12 supplementation is needed in chronic cases.
o Antibiotics (2-3 weeks):
- Tetracycline 250 mg 6-hourly,
- Metronidazole 400 mg 8-hourly, or
- Ciprofloxacin 250 mg 12-hourly.
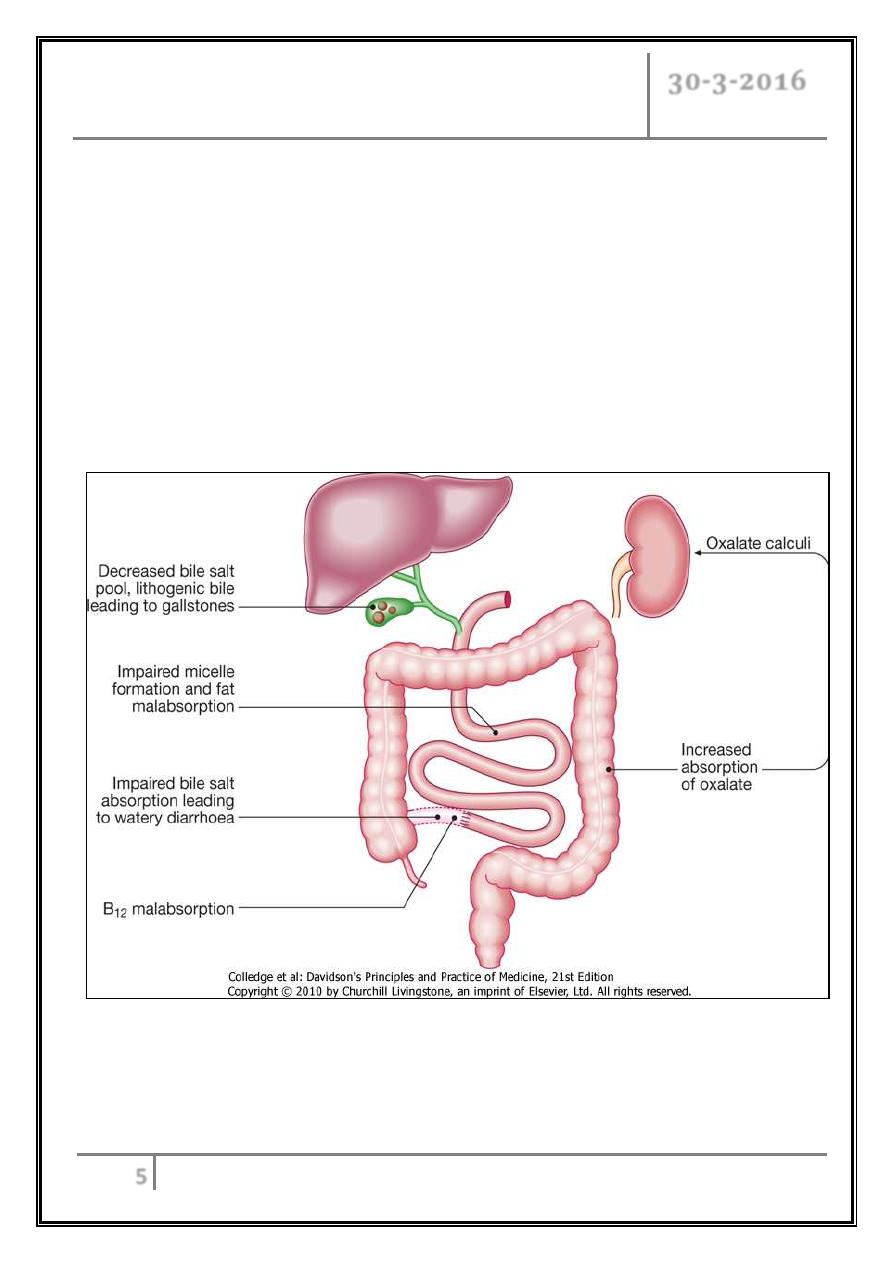
Short bowel syndrome
Short bowel syndrome is defined as malabsorption resulting from resection of
various length intestinal small.
Features depend on:
1) The segment resected (jejunum vs ileum).
2) The length of the resected segment.
3) The integrity of the ileocecal valve.
4) Whether any large intestine has also been removed.
5) Residual disease in the remaining small and/or large intestine (e.g., Crohn's
disease.
6) The degree of adaptation in the remaining intestine.
Etiology
Children
- Congenital anomalies (e.g. mid-gut volvulus, atresia).
- Necrotising enterocolitis.
Adults
- Mesenteric infarction.
- Crohn's disease.
- Radiation enteritis.
- Volvulus.
- Jejunoileal bypass for
obesity.
Malabsorption & protein losing Dr. Rabah
enteropathy – Part 2
30-3-2016
5
Clinical features
Diarrhea.
Steatorrhoea.
Dehydration and hypovolaemia.
Weight loss, malnutrition.
No intestinal symptoms:
- Renal calcium oxalate calculi.
- Cholesterol gallstones.
Malabsorption & protein losing Dr. Rabah
enteropathy – Part 2
30-3-2016
6
Treatment
Enteral feeding can be cautiously introduced after 1-2 weeks under careful
supervision.
PPI therapy is given to reduce gastric secretions.
Replacement therapy (VITAMINS).
Rx of the bacterial overgrowth.
TPN is needed less than 100 cm of jejunum remains.
Intestinal transplantation.
The principles of long-term management
Nutritional assessments at regular intervals.
Monitoring of fluid and electrolyte balance.
Fats are.medium-chain triglyceride.
Antidiarrhoeal agents, e.g. loperamide or codeine phosphate.
Low-fat and high-carbohydrate.
Protein-Losing Enteropathy
A group of gastrointestinal and nongastrointestinal disorders with
hypoproteinemia and edema in the absence of either proteinuria or defects in protein
synthesis in the liver, e.g., chronic liver disease.
Causes
With mucosal ulceration
- Crohn's disease.
- Ulcerative colitis.
- Radiation damage.
- Oesophageal, gastric or colonic cancer.
- Lymphoma.
Malabsorption & protein losing Dr. Rabah
enteropathy – Part 2
30-3-2016
7
Without mucosal ulceration
- Ménétrier's disease.
- Bacterial overgrowth.
- Coeliac disease.
- Tropical sprue.
- Eosinophilic gastroenteritis.
With lymphatic obstruction
- Intestinal lymphangiectasia.
- Constrictive pericarditis.
- Lymphoma.
- Whipple's disease.
Clinical features
o Peripheral edema.
o Low serum albumin and globulin levels.
o Lymphatic obstruction often has steatorrhea and diarrhea and lymphopenia.
Treatment
Treatment the underlying disease.
In intestinal lymphangiectasia, treatment of the hypoproteinemia is
accomplished by a low-fat diet and the administration of MCTs.
… END …
