Dr. Rabah
Lec. 5
INFLAMMATORY BOWEL DISEASES
–
PART 1
Thur. 31 / 3 / 2016
Done By: Ibraheem Kais
2015 – 2016
ﻣﻜﺘﺐ ﺁ
ﺷﻮﺭ ﻟﻼﺳﺘﻨﺴﺎﺥ
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
1
Inflammatory bowel diseases – Part 1
Ulcerative colitis and Crohn's disease are immune-mediated chronic
inflammatory bowel diseases with relapsing and remitting courses.
Ulcerative colitis only involves the colon.
Crohn's disease can involve any part of the gastrointestinal tract from mouth to
anus.
Epidemiology
In developing world
- Crohn's disease appears to be rare.
- Ulcerative colitis, more common.
In the west
- Ulcerative colitis prevalence of 100-200 per 100 000.
- Crohn's disease prevalence of 50-100 per 100 000.
Young adults (between 15 and 30 years) , second smaller incidence peak in the
seventh decade (between 60 and 80 years).
The male to female ratio for UC is 1:1 and for CD is 1.1–1.8.
UC and CD have two- to fourfold increased frequency in Jewish.
Etiology
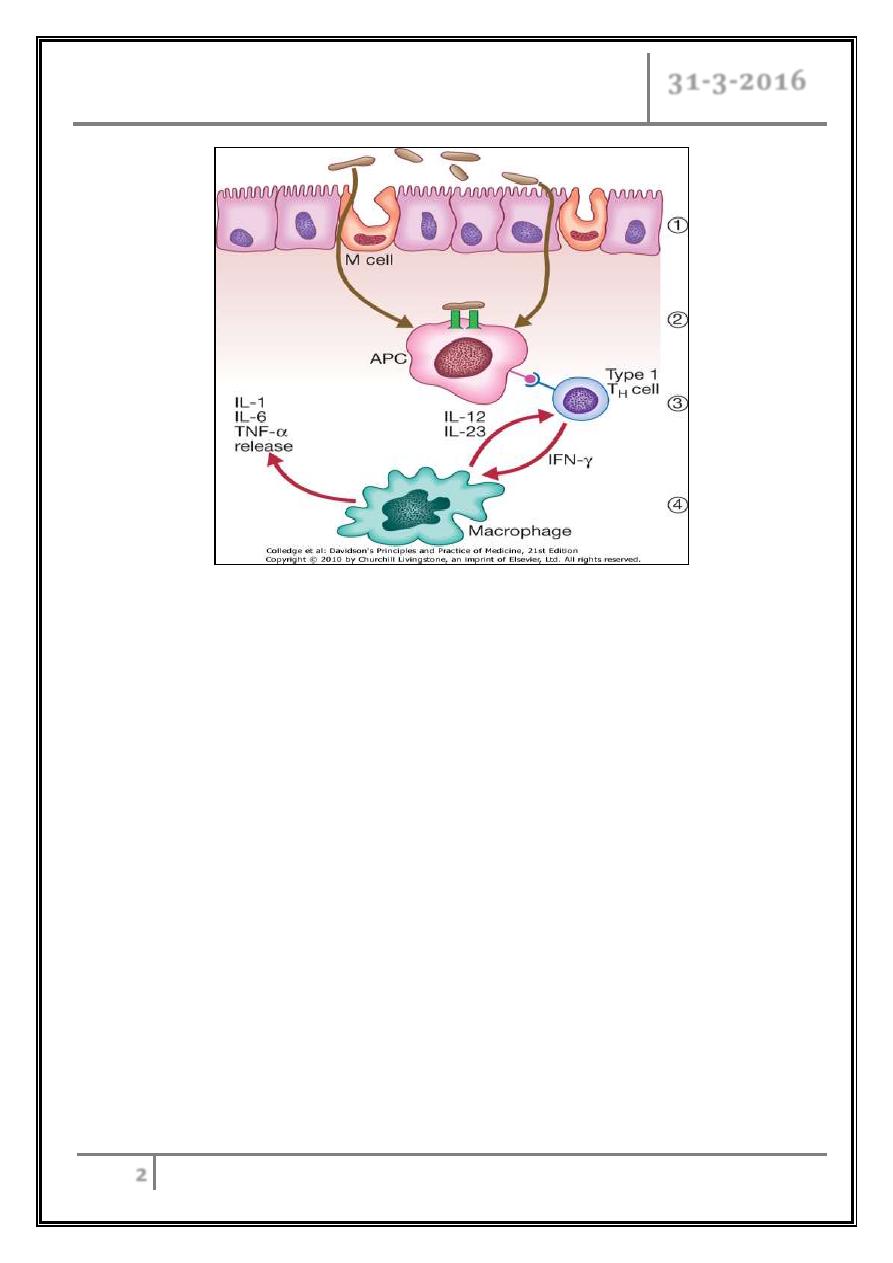
Abnormal host response to an environmental trigger in genetically susceptible
individuals.
This causes inflammation of the intestine and release of inflammatory
mediators, such as TNF, IL-12 and IL-23, which cause tissue damage.
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
2
Factors associated with the development of IBD
Genetic
- More common in Ashkenazi Jews.
- 10% have a first-degree relative or at least one close relative with IBD.
- High concordance between identical twins.
- Some abnormal genes detected.
- Associated with autoimmune thyroiditis and SLE.
Environmental
- Ulcerative colitis is more common in non-smokers.
- Most Crohn's patients are smokers.
- Appendicectomy protects against ulcerative colitis.
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
3
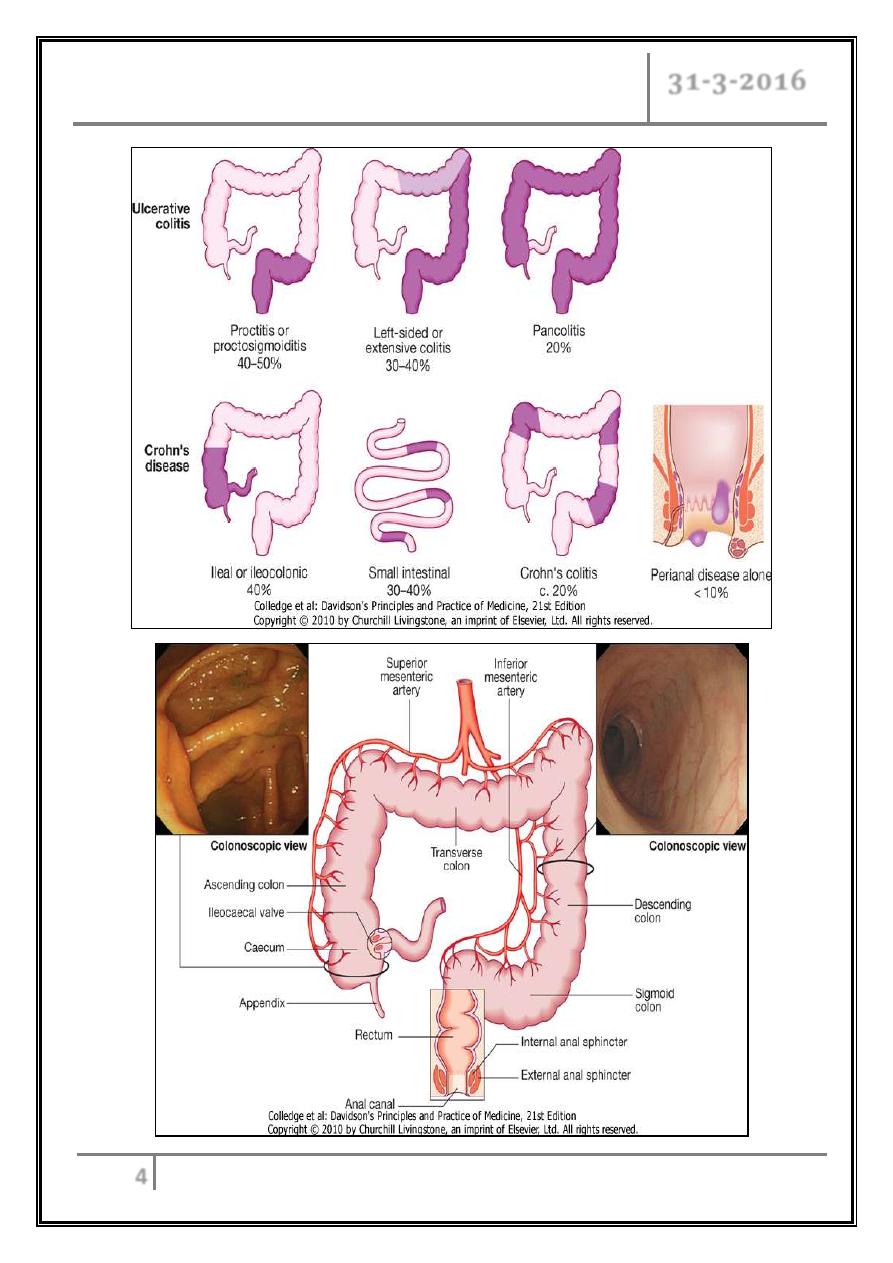
Pathology
Ulcerative Colitis
o
Macroscopic features
- Extends proximally to involve all or part of the colon.
- 40–50% of patients involve the rectum, rectosigmoid.
- 30–40% beyond the sigmoid.
- 20% have a total colitis.
- Inflammation is diffused
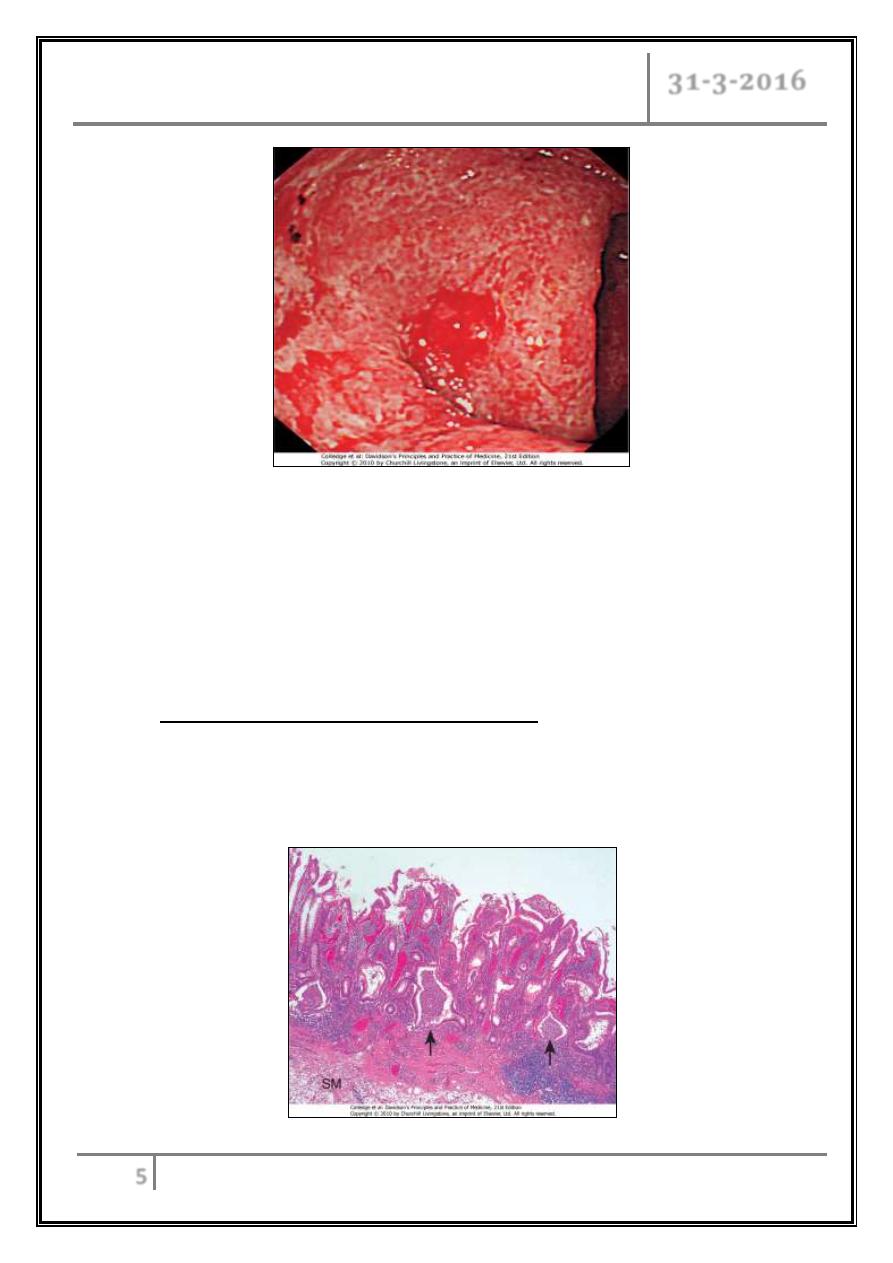
Mild
The mucosa is erythematous and fine granular surface
More severe
The mucosa is hemorrhagic, edematous, and ulcerated (superficial
diffused)
Fulminant
Disease can develop a toxic megacolon where the bowel wall thins
and the mucosa is severely ulcerated; this may lead to perforation.
In long-standing disease
Inflammatory polyps (pseudopolyps) may be present as a result of
epithelial regeneration.
Many years of disease it appears atrophic and featureless and the
entire colon becomes narrowed and shortened.
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
4
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
5
o
Microscopic features
- Mucosal vascular congestion, edema and focal hemorrhage.
- Inflammatory cell infiltrate of neutrophils, lymphocytes, plasma cells, and
macrophages may be present.
- The neutrophils invade the epithelium, usually in the crypts, giving rise to
cryptitis and, to crypt abscesses.
o
Histological features of chronicity
- First, the crypt architecture of the colon is distorted.
- Second, some patients have basal plasma cells and multiple basal
lymphoid aggregates.
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
6
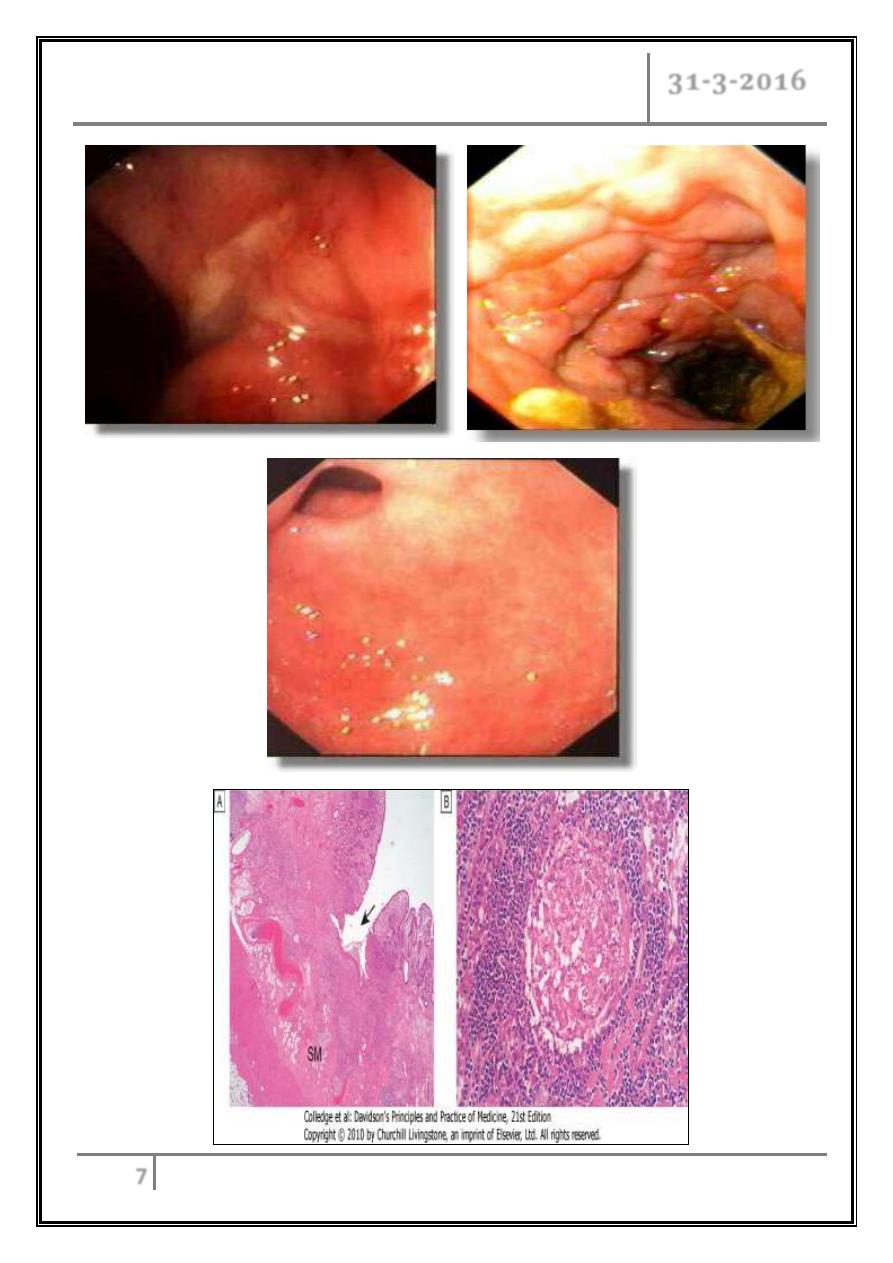
Crohn's disease:
o
Macroscopic features
- 30–40% of patients have small-bowel alone.
- 40–55% have disease involving the ileum and the Rt colon.
- 15–25% have colitis alone.
- 30 % have anal involvement.
- The rectum is often spared in CD.
- Segmental inflammation (skip areas of inflammation).
- Aphthous ulcerations.
- Stellate ulcerations fuse longitudinally and transversely to demarcate
islands of mucosa that frequently are histologically normal "cobblestone"
appearance.
- Ulcers may penetrate bowel wall to initiate abscesses or fistulas:
The bowel.
Bladder.
Uterus.
Vagina.
Skin of the perineum.
- Bowel narrowed and fibrotic, with chronic, recurrent bowel obstructions.
- Mesenteric lymph nodes are enlarged and the mesentery is thickened.
o
Microscopic features
- Transmural inflammation.
- Fissures penetrate deeply into the bowel wall.
- Bowel wall thickened.
- Chronic inflammatory infiltrate all layers.
- Focal crypt abscesses.
- Non-caseating granulomas.
- Microscopic skip areas.
- Other histologic features submucosal or subserosal lymphoid aggregates.
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
7
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
8
Clinical features
Ulcerative colitis
Bloody diarrhoea relapses and remissions.
Emotional stress.
Intercurrent infection.
Gastroenteritis.
Antibiotics.
NSAID therapy may all provoke a relapse.
Proctitis
- Rectal bleeding.
- Mucus discharge.
- Tenesmus.
- Frequent, small-volume fluid stools.
Proctosigmoiditis
- Bloody diarrhoea with mucus.
Extensive colitis
- Bloody diarrhea.
- Passage of mucus.
- Severe cramping.
- Abdominal pain can occur with severe attacks of the disease.
- Constitutional symptoms do not occur only in moderate to severe disease.
Severe colitis
- Bleeding.
- Severe diarrhea.
- Severe pain.
- Fever.
- Tachycardia.
- Abdominal tenderness.
- Edema.
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
9
Mild
- <4 stool/day no or small blood amount.
- No fever.
- No tachycardia.
- Mild anemia.
- ESR < 30.
Moderate
- Intermediate between mild and severe.
Severe
- 6 stool /day with blood.
- Fever > 37.5c.
- Heart rate > 90.
- Anemia < 75% of the normal.
- ESR > 30.
Crohn's disease
The major symptoms are
Pain is often associated with diarrhea.
Diarrhoea, usually watery not contain blood or mucus.
Weight loss.
Malabsorption.
Intestinal obstruction subacute or even acute.
Crohn's colitis
- As ulcerative colitis.
- Rectal sparing.
- Stricturing can occur in the colon
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
10
Perianal disease
- Affects about one-third.
- Large hemorrhoidal tags.
- Anal strictures.
- Anorectal fistulae.
- Perirectal abscesses.
- Incontinence.
Ileocolitis
- Recurrent right lower
quadrant pain.
- Diarrhea.
- Palpable mass.
- Fever, leukocytosis.
- Weight loss is common.
- Fistula formation.
- Abscess cavity in the mesentery.
Small intestinal crohns
- Malabsorption and steatorrhea.
- Nutritional deficiencies.
- Vomiting from jejunal strictures or severe oral ulceration.
Differential diagnosis
Colitis
Infective
Bacterial
- Salmonella.
- Shigella.
- Campylobacter jejuni.
- E. coli.
- Gonococcal proctitis.
- Pseudomembranous colitis.
- Chlamydia proctitis.
Viral
- Herpes simplex proctitis.
- Cytomegalovirus.
Protozoal
- Amoebiasis.
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
11
Non-infective
Vascular
- Ischaemic colitis.
- Radiation proctitis.
Idiopathic
- Collagenous colitis.
- Behçet's disease.
Drugs
- NSAIDs.
Neoplastic
- Colonic carcinoma.
Other
- Diverticulitis.
Small bowel Crohn's disease
Right iliac fossa mass:
- Caecal carcinoma.
- Appendix abscess.
Infection:
- Tuberculosis.
- Yersinia.
- Actinomycosis.
Intestinal Lymphoma.
Mesenteric adenitis.
Complications
Toxic megacolon
Acute colonic dilatation due severe flare of the colitis.
More with extensive colitis.
5% incidence.
Precipitating factors as hypokalemia, antimotility, and colonoscopy.
Clinical features:
- Features of severe colitis
with,
- Diffused abdominal
distension.
- Diffused tenderness.
- Decease bowel sound.
- Lab sings of systemic inflammation.
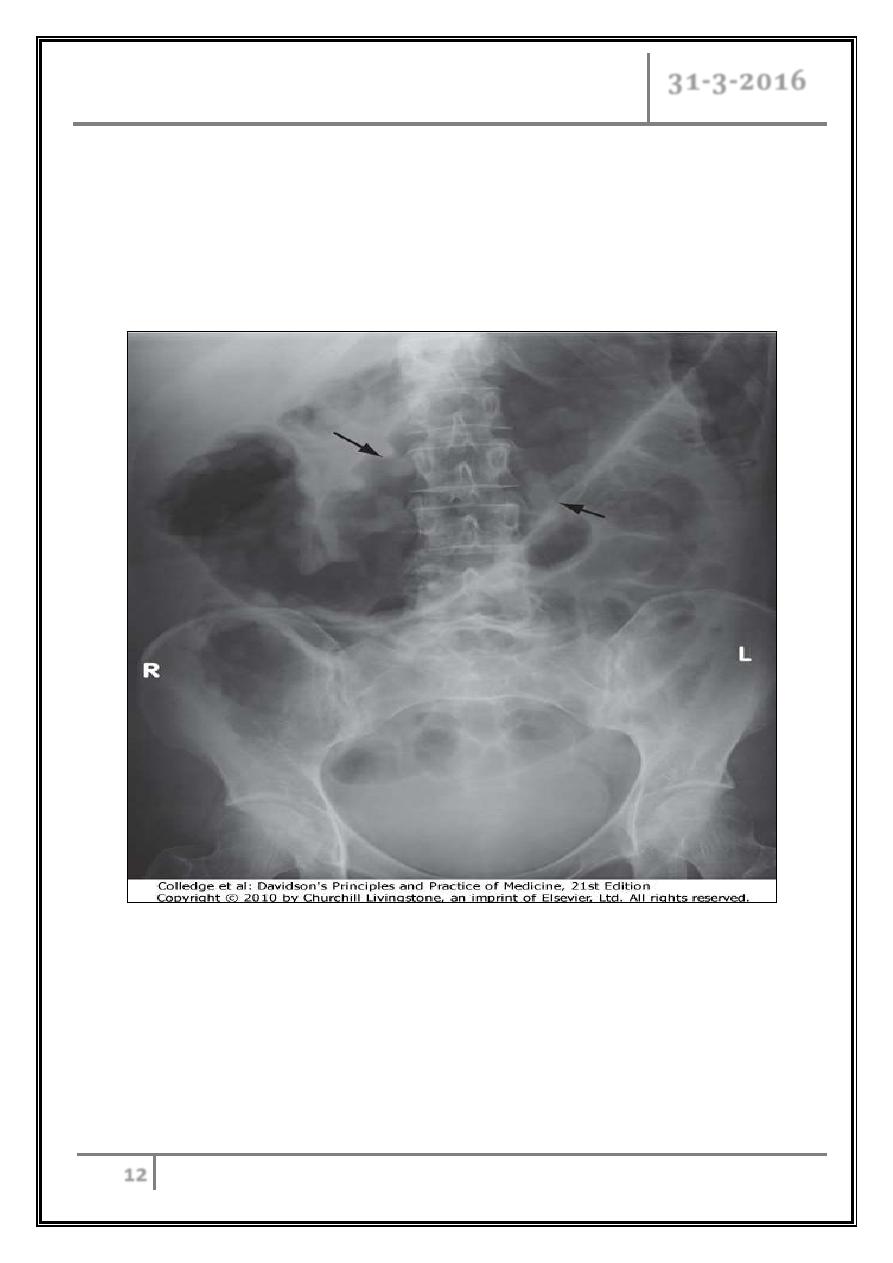
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
12
Treatment
- Conservative.
Indication for surgery:
- No response within 72 hr.
- Sings of peritonitis or perforation.
Toxic megacolon. Transverse colon diameter> 6 cm
Hemorrhage
Acute Haemorrhage (major artery) is rare.
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
13
Fistulas
Enteroenteric
- Diarrhoea.
- Malabsorption.
Enterovesical
- Recurrent UTI.
- Pneumaturia.
Enterovaginal
- A feculent.
- Vaginal discharge.
Bowel fistulation
- Perianal.
- Ischiorectal.
- Abscesses.
- Fissures.
Cancer
Active colitis of more than 10 years.
The cumulative risk 10%.
Lower for Crohn's colitis.
Tumors develop in areas of dysplasia.
Surveillance programmes beginning 10 years after diagnosis by colonoscopy
1-2-yearly.
Moderate-high-grade dysplasia panproctocolectomy.
Strictures
In Crohn's disease.
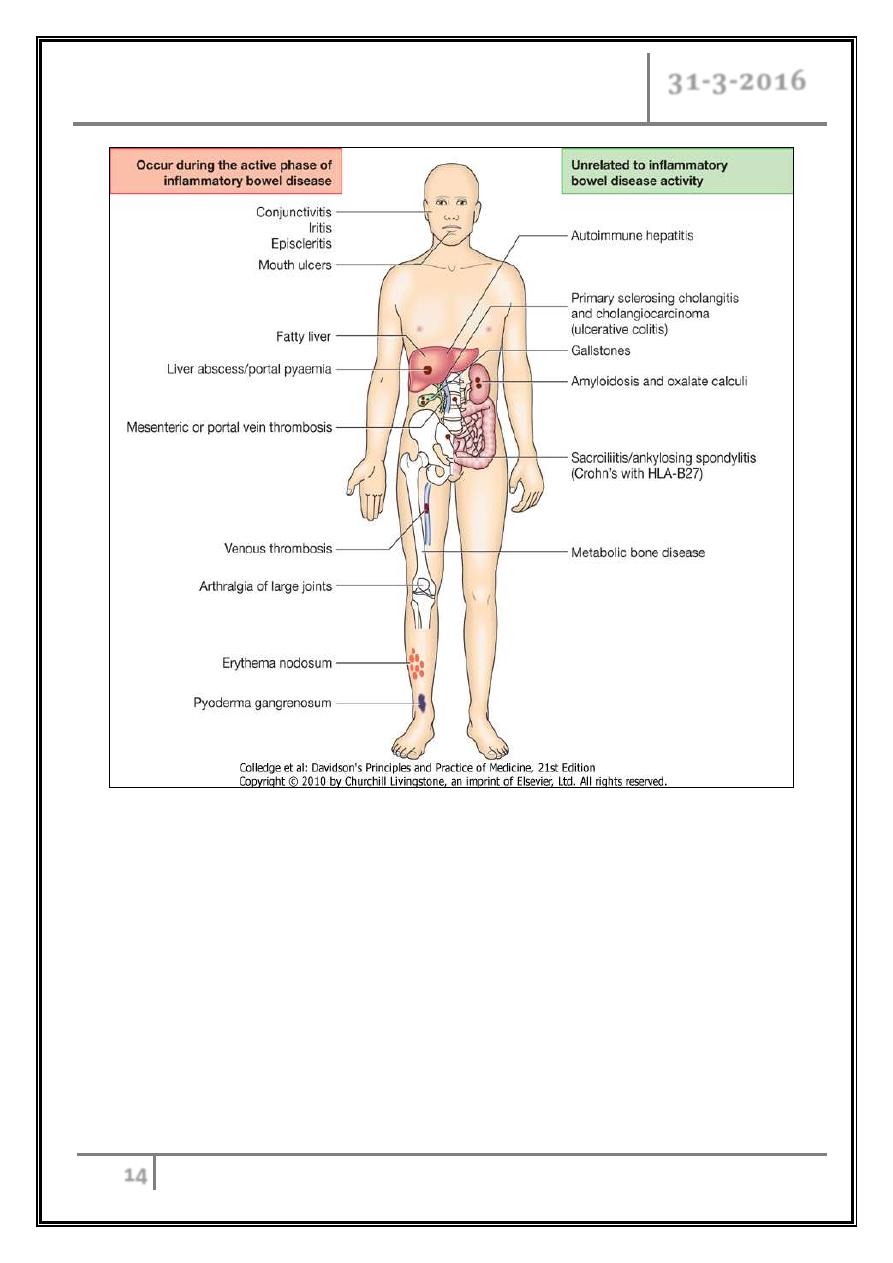
Extra intestinal complications
Common in IBD.
May dominate the clinical picture.
Some of these occur during relapse of intestinal disease.
Others unrelated to intestinal disease activity.
Include skin, joints, mouth, hematological, caogulopathy, eye and
hepatobiliary.
Inflammatory bowel diseases – Part 1 Dr. Rabah
31-3-2016
14
To be continued …
