Baghdad College of Medicine / 4
th
grade
Student’s Name :
Dr. Basim Rassam
Lec. 2
Portal Hypertension
Tues. 17 / 11 / 2015
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2015 – 2016
Portal Hypertension Dr. Basim Rassam
17-11-2015
2
©Ali Kareem 2015-2016
Portal Hypertension
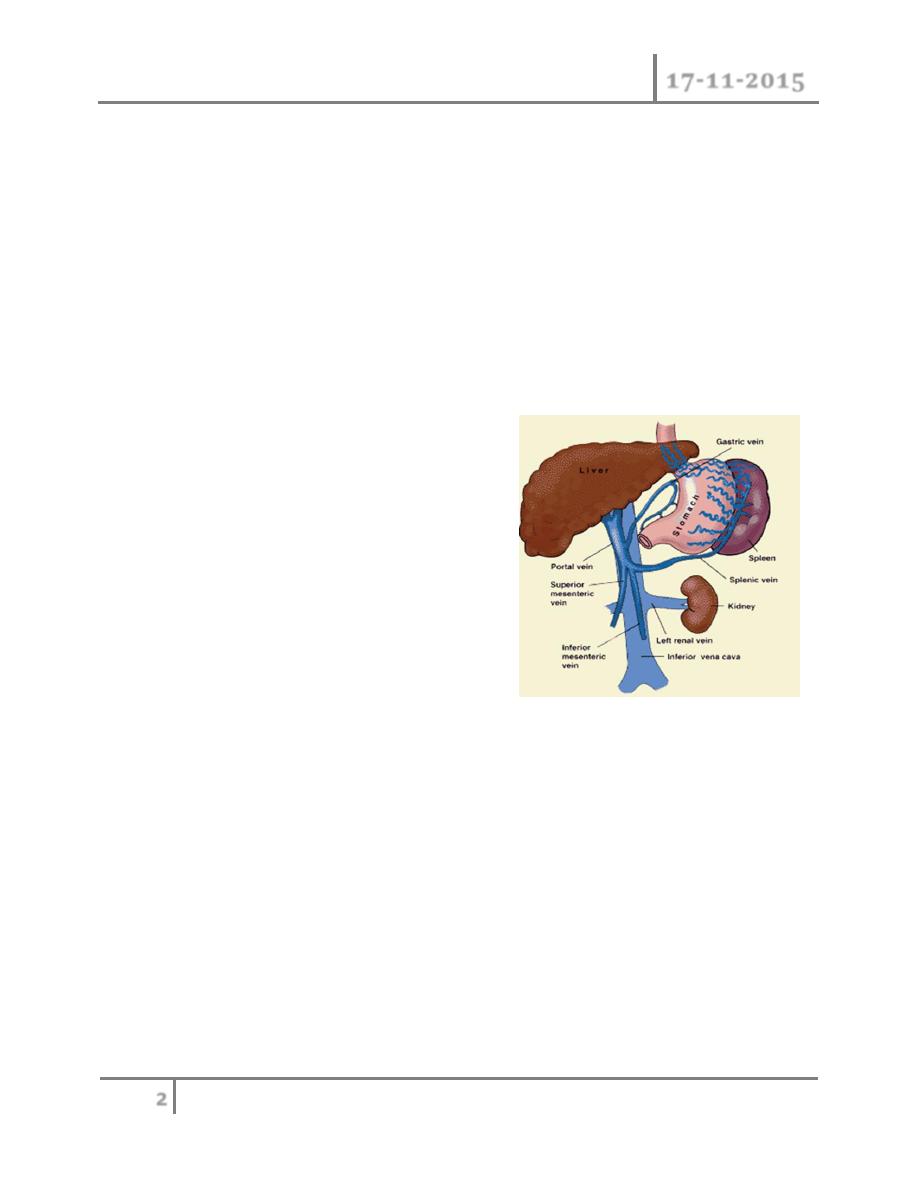
Normal portal venous pressure is 80 -120 mm H2O and depends on splanchnic
blood flow, resistance to outflow from the liver and pressure in the Inferior vena
cava. In portal hypertension it reaches 400 mm H2O or more.
Bleeding from oesophageal varices starts when portal pressure exceeds
250 – 300 mm H2O. The portal vein is formed of two main vessels- the
Superior mesentieric and splenic veins.
It has no valves .As a result of portal
hypertension, extrahepatic portasystemic
anastomotic channels become engorged and
dilated ( i.e. oesphageal varices with
profuse painless heamatmesis, caput medusa
around umbilicus and haemorrhoids)
Hypersplenisim with pancytopaenia, stasis in
the portal circulation with portal vein thrombosis and infarction of the intestine,
as well as ascites , also results.
Causes of Portal Hypertension
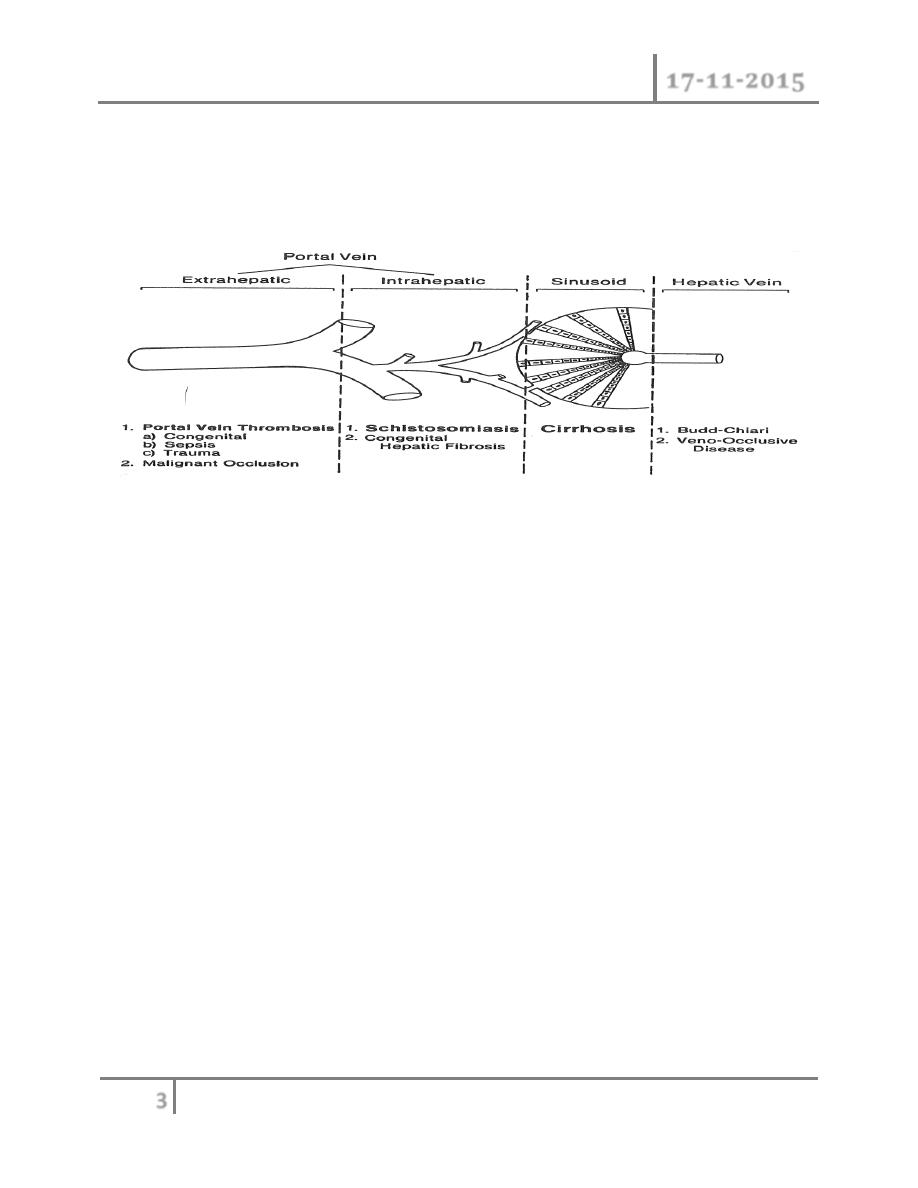
o Prehepatic presinusoidal (liver is normal) include umbilical sepsis
(neonatal), clotting diathesis (polycythaemia), malignant portal vein
obstruction and idiopathic causes.
o Intrahepatic presinusoidal (liver is diseased) include schistosomiasis,
congenital hepatic fibrosis, sarcoidosis and liver intoxication.
o Intrahepatic postsinusoidal group includes cirrhosis.
Portal Hypertension Dr. Basim Rassam
17-11-2015
3
©Ali Kareem 2015-2016
o Posthepatic postsinusoidal include hepatic vein obstruction (Budd-Chiari
syndrome) and constrictive pericarditis.
o Schistosomiasis and cirrhosis are the commonest causes of portal
hypertension worl-wide.
There are four main areas of portosystemic anastomosis that become developed
in portal obstruction. These are:
o Between the left vein and the oesophageal veins: forming oesophageal
varices
o Between the supperior and inferior rectal veins: forming haemorrhoids
o Along the obliterated umblical vein to the superior and inferior epigastric
veins: forming a caput medusae
o Retroperitoneal and diaphragmatic anastomoses: which may cause
intraoperative hazards
o Oesophageal varices and resulting gastrointestinal haemorrhage are the
most serious complication of portal hypertension.
o Splenomegaly occurs because of:
o Portal congestion
o Leucopenia and thromobocytopenia causing hypertrophy of the splenic
substance itself
o Ascites is due to a combination of:
o Raised portal pressure (not enough to cause ascites on its own)
o Low serum albumin
o
↑ Aldosterone activity with sodium retention
o
↑ Lymphatic pressure in the cirrhotic liver resulting in lymph transudation.

Portal Hypertension Dr. Basim Rassam
17-11-2015
4
©Ali Kareem 2015-2016
Clinical features of portal hypertension
o Because of its range of effects, portal hypertension can present in many
ways:
o Haemorrhage from bleeding oesphageal varices or haemorrhoids
o With signs hepatic failure: jaundice; CNS effects; stigmata of liver disease
o A cause of splenomegaly
o A cause of hepatomegaly
o Because of its catastrophic effect, haemorrhage from bleeding oesphageal
varices is the most significant surgical presentation of portal hypertension.
Haemorrhage from oesophageal varices
o Oesophageal varices account from 50% of deaths from upper
gastrointestinal bleeding, although they cause only 10% of cases. Whilst the
patient is being resuscitated, certain investigations should take place- others
should be delayed until the patient’s condition stabilizes (see the shaded box
below).
Diagnosis and assessment of portal hypertension
Liver function tests; chest X-ray; barium swallow (soap-bubble appearance of
varices); barium meal; i.v. urography to evaluate left renal function (for lienorenal
shunt); splenoportography and ultrasound (may show patent or obstructed portal
vein); transhepatic venography and endoscopy especially in emergency bleeding to
confirm the site of bleeding from chronic peptic ulcer or erosive gastritis which
may account for %40 of misdiagnosed bleeding varices. Peptic ulcer is more
common in cirrhotics and the presence of varices does not necessarily mean that
they are source of upper gastrointestinal tract bleeding. The severity of liver
disease is graded according to Child’s classification into A, B and C and modified
into a flexible system using points.

Portal Hypertension Dr. Basim Rassam
17-11-2015
5
©Ali Kareem 2015-2016
Serum bilirubin
o (mg/100ml) < 2 (1), 2-3 (2), > 3 (3)
o (μmol/1) < 34 (1), 34-51 (2), >51 (3)
Serum albumin
o (g/100ml) > 3.5 (1), 3-3.5 (2), <3 (3)
Prothrombin time
o (seconds prolonged) <2 (1), 3-5 (2), >5 (3)
Ascites None (1), Mild/moderate (2),
Gross (3)
Encephalopathy None (1), Minimal (2),
Moderate/severe (3)
The added points are classified as follows:
A= 5-7 points
B= 8-9 points
C= 10-15 points
A liver biopsy is essential and liver scan may be required to exclude hepatomas.
The ideal patient for a shunt operation should be under 45 years of age, category
A or B, with inactive liver disease and should look and feel well.
The four important effects of portal hypertension are:
Development of a collateral portosystemic circulation
Splenomegaly
Ascites
Hepatic failure and its sequelae.

Portal Hypertension Dr. Basim Rassam
17-11-2015
6
©Ali Kareem 2015-2016
The management should be carried out in high-dependency units with specialized
teams. The principles are:
Control the acute bleeding
Prevent recurrent bleeding
Treat underlying
Control of variceal haemorrahge
Immediate resuscitation takes priority. The airway should be protected. Central
venous access is often indicated. Blood, fresh frozen plasma and platelets are
usually needed. Catheterization to monitor urine output. Over-expansion of the
circulation may cause a dangerous increase in portal venous pressure. Prevention
od complication or the early recognition and treatment of these is important.
Complications of vericeal haemorrhage
Aspiration * Pneumonia
Hepatic encephalopathy * Hypoxia
Ascites * Renal failure
Infections from enteric organisms * Alcohol withdrawal
Drug treatment of oesophageal varices
Somatostation is a hormone that reduces splanchnic and hepatic flow. Octreotide
and lanreotide are longer-acting synthetic analogues of somatostatin. Vasopressin
causes generalized vasoconstriction but its use is controversial. It is given in
combination with glyceryltrinitrate under close cardiac monitoring. Terlipressin is
an analogue of vasopressin which has a longer action and fewer systemic effects.
Ballon tamonade
Insertion of a double-ballooned Sengstaken-Blakemore or Minnisota tube into the
oesophagus controls variceal bleeding temporarily by direct compression at the
bleeding site. Use of balloon tamponade is recommended in:
Massive bleeding preventing endoscopy

Portal Hypertension Dr. Basim Rassam
17-11-2015
7
©Ali Kareem 2015-2016
Stabilizing patients awaiting definitive therapy
Patients being transferred to a specialist unit.
It should not be used in patients with a large hiatus hernia.
Sclerotherapy of varices
Injecting sclerosant, such as ethanolamine, into bleeding varices is usually
undertaken at the initial emergency endoscopy to control acute bleeding.
Successful in 70-90% of cases, and may be repeated the following week to prevent
re-bleeding. If two attempts of sclerotherapy fail, a more major intervention is
indicated. Complications include:
Fever
Retrosternal discomfort
Dysphagia
Ulceration
Stricture
Local perforation
Variceal banding
Banding produces better control of bleeding than sclerotherapy with lower
morbidity and reduced re-bleeding. Not as suitable for the acutely bleeding
patient, due to technical limitations. Banding is therefore recommended for second
or subsequent endoscopy sessions to eradicate varices initially treated by
sclerotherapy.
Intrahepatic shunt
Trans-jagular intrahepatic porto-systemic shunt (TIPSS) is a radiological
technique for creating a porto-systemic shunt via the trans-jagular route.

Portal Hypertension Dr. Basim Rassam
17-11-2015
8
©Ali Kareem 2015-2016
Indications for TIPSS
Uncontrolled acute varical bleeding
Recurrent varical bleeding
Failed endoscopic therapy
Patient intolerant of endoscopic therapy
Surgery contraindicated by poor hepatic function or general condition
Patients awaiting liver transplants.
Under local or general anaesthetic, the right hepatic-hepatic vein is
cannulated by a percutaneous jagular route and the liver punctured to gain
access to the portal vein
The track is then dilated with a balloon catheter and a stent of 8-12mm
diameter is placed to maintain patency
The principle is to reduce the portal pressure gradient by short circuiting the liver.
TIPSS is contraindicated in:
Right-sided heart failure with an elevated central venous pressure
Polycystic liver disease
Severe acute progressive hepatic failure.
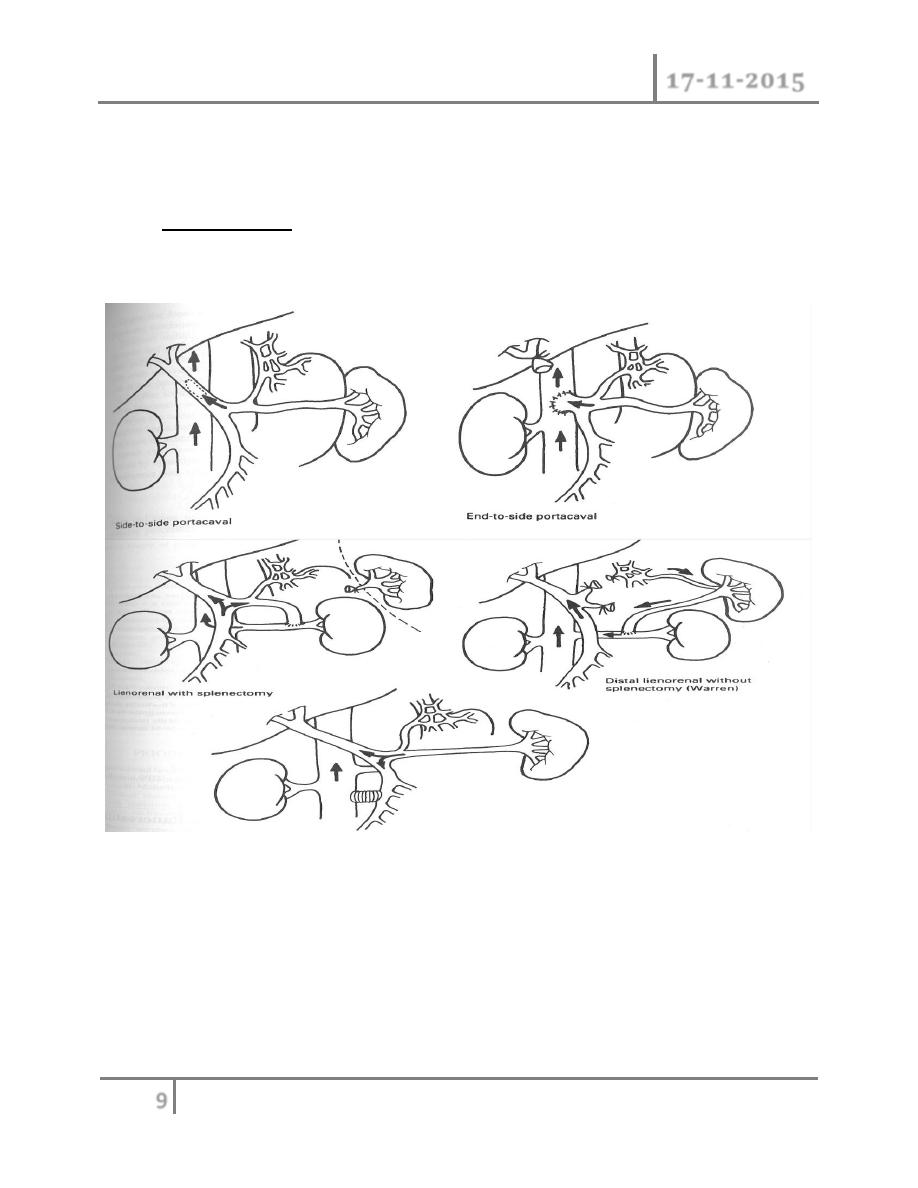
Extrahepatic shunt
In long-term elective treatment, extrahepatic shunt or oesophageal transection are
the alternatives to repeated sclerotherapy. The aim of extrahepatic shunt is to
decompress the whole or part of the portal venous circulation. These shunts
require a surgical procedure and are indicated in patients with failed endoscopic
treatment. The three main extrahepatic shunts are:
o Total shunt (portocaval): the whole of the portal venous circulation is fully
decompressed. In total shunts, there is no portal vein flow into the liver. The
incidence of encephalopathy is high.
o Partial shunt (narrow diameter portocaval): the whole of the portal venous
circulation is partly decompressed with a narrow (8-10mm) non-expansile
graft. Some portal flow continues so post-operative encephalopathy is
Portal Hypertension Dr. Basim Rassam
17-11-2015
9
©Ali Kareem 2015-2016
reduced. This procedure can be done without extensive dissection and so is
preferable to a total shunt for both uncontrolled acute and recurrent
bleeding.
o Selective shunt (distal splenorenal): an isolated part of the portal
circulation is fully decompressed. This is not advocated in an acute situation
because of its technical complexity.
Oesophageal transection
The aim of oesophageal transection is to interrupt the gastric oesophageal porto-
systemic anastomosis. Early oesophageal transection has compared favourably
with injection sclerotherapy, but it requires a laparotomy and disseration in the
Mesocaval graft interpostion

Portal Hypertension Dr. Basim Rassam
17-11-2015
10
©Ali Kareem 2015-2016
presence of established portal hypertension and opening of the stomach, all of
which may be hazardous in the acutely bleeding patient.
Anterior gastrotomy
Stabling gun passed up into the oesophagus
Vagus nerve identified and excluded
Lower oesophageal wall tied into stapling line
Gun fired to transect and re-anastomose the oesphagus simultaneously
Problems include:
Bleeding gastric varices require further devascularization
May be more hazardous than simple partial shunt
Chances od sepsis are increased by opening stomach
Recurrent bleeding is more likely than with shunts
Indication for elective surgery in portal hypertension
Bleeding oesophageal varices (once they have bled they will bleed again) is an
absolute indication. Hypersplenism and ascites are relative indications.
Liver transplantation
Liver transplantation may be the preferable option for intractable portal
hypertension. It is not suitable in cases of pre-hepatic obstruction with good liver
function or in cases with a persisting underlying cause.
END…
