1 |
P a g e
//
SURGERY
LEC.13
Dr. Muayad Abbas
Lec.1
LIVER SURGERY
Tues. 3 / 11 / 2015
DONE BY : Mustafa Naser
مكتب اشور لالستنساخ
2015 – 2016
2 |
P a g e
LIVER SURGERY
Anatomy:
The liver is the largest
organ in the body, weighing
5.1
kg
in the
average
07
-
kg man
.
The liver parenchyma is
entirely covered
by
a
thin capsule
and by
visceral peritoneum
on all but the posterior
surface of the
liver, termed the
‘
bare area
.’
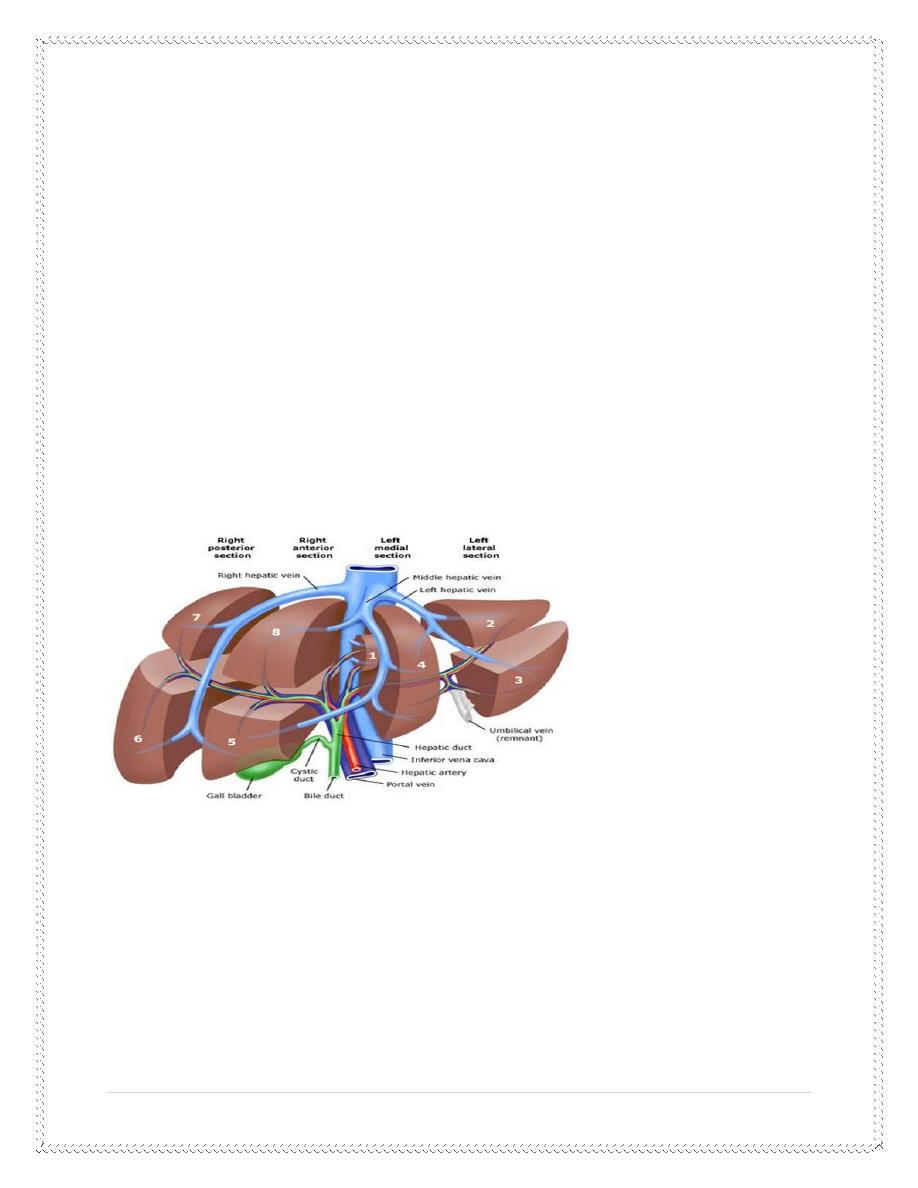
The liver is divided into a
large right lobe
,
which constitutes
three-quarters
of the
liver parenchyma, and a smaller
left lobe
.
Surgical resection of these
lobes would
be termed a
right or
left lobectomy
.
Ligaments and peritoneal reflections:
left triangular ligament
The right triangular ligament
falciform ligament
(
remnant of the umbilical
3 |
P a g e
vein), which runs from the umbilicus to the
liver between them right and left
lobes, passing into the interlobar fissure
.
Liver blood supply:
The blood supply to the liver
is unique
,
07
%
being derived from the
portal
vein
and
07
%
from the
hepatic artery
.
The arterial blood supply in
most individuals is derived from the
coeliac
trunk
of the aorta, where the
hepatic artery
arises along with the
splenic
artery
.
After supplying the
gastroduodenal artery
,
it branches at a very
variable level to produce the
right and left hepatic arteries
.
The blood supply to the right
lobe of the liver may be partly or completely
supplied by a right hepatic
artery arising from the
superior
mesenteric
artery
Similarly, the arterial blood
supply to the left lobe of the liver may be
derived from the coeliac trunk via
its
left
gastric branch
.
The hepatic artery, portal
vein and bile duct are present within the free edge
of the lesser omentum or
the
‘
hepatoduodenal
ligament
.’
The usual anatomical
relationship of these structures is for the bile duct to
be within the free
edge, the hepatic artery to be above and medial, and the
portal vein to lie
posteriorly
.
Within this ligament, the
common hepatic duct is joined by the cystic duct at
a varying level to form the
common bile duct
.
The
common hepatic artery
branches at a variable level
within the ligament
to form two, or often three, main arterial branches to the
liver
.
The right
hepatic artery
often crosses the bile duct
either anteriorly or posteriorly
before giving rise to the
cystic artery
.
Multiple small hepatic arterial
branches
provide blood to the
bile duct
,
principally from the
right hepatic artery
.
The
portal vein
arises from the confluence of
the
splenic
vein
and the
superior mesenteric vein
behind the neck of
thepancreas. It has some
4 |
P a g e
important tributaries, including the left gastric vein
which joins just above
the pancreas
.
Venous drainage of the liver:
The
venous drainage
of the liver is via the
hepatic veins into the IVC
.
The
inferior hepatic veins
are short vessels that pass
directly between the
liver parenchyma and the anterior wall of the IVC
.
The
major venous drainage
is through
three large veins that join the
IVC
immediately below the diaphragm
. .
The
right hepatic
vein can be exposed fully
outside the liver
,
but the
middle and left veins
usually join within the liver
parenchyma
.
Main functions of the liver:
■
Maintaining
core body temperature
■
pH balance
andcorrection
of lactic acidosis
■
Synthesis of
clotting factors
■
Glucose
metabolism, glycolysis and gluconeogenesis
■
Urea
formation from protein catabolism
■
Bilirubin
formation from haemoglobin degradation
■
Drug and
hormone metabolism
■
Removal of
gut endotoxins and foreign antigens
Liver function test :
USED TO
Detect presence of liver
disease
Distinguish among different
types of liver diseases
5 |
P a g e
Gauge the extent of known
liver damage
Follow the response of
treatment
Tests based on detoxification
&
excretory
functions:
Serum bilirubin
Urine bilirubin
Blood ammonia
Serum enzymes : AST, ALT
,
GGT, 5’Nucleotidase,ALP
Tests that measure Biosynthetic function of
liver:
Serum Albumin
Serum Globulins
PT ,INR
Liver function test:
Bilirubin
is synthesised in the liver
and excreted in the bile. Increased levels
may be associated with: 1
-
increased haemoglobin breakdown
0
-
hepatocellular dysfunction
resulting in impaired
bilirubin transport and
excretion, or
3
-
biliary obstruction
.
Serum Bilirubin:
A break down product of
porphyrin ring of heme – containing proteins
,
found in blood in 2 fractions
–
conj/unconj
Conjugated
:
water soluble , so excreted
by kidneys
Unconjugated
:
insoluble in water , bound
to albumin in blood
About
377
mg of bilirubin
is formed per day
6 |
P a g e
Normal total serum bilirubin
:
7.3
–
5.3
mg/dl
Direct/conjugated bilirubin
:
7.5
–
7.0
mg/dl
Indirect/unconjugated
bilirubin: 0.2 – 0.9mg/dl
Urine Bilirubin:
Unconj bilirubin – binds to
albumin in serum
&
not filtered by kidneys
Any bilirubin in urine is
conj.bilirubin, the presence of bilirubinuria – liver
ds
.
In acute viral hepatitis
–
bilirubin appears in urine before urobilinogen and
jaundice
.
Undiagnosed febrile illness
with
bilirubinuria - hepatitis
Blood Ammonia:
Produced by
normal protein metabolism
by intestinal bacteria in colon
Liver – detoxification
–
converting into urea which is excreted by kidneys
.
Pts with advanced liver
diseases contributes to hyperammonemia
.
The serum
alkaline phosphatase
is particularly elevated with
cholestatic
liver
disease
or
biliary
obstruction
.
The
transaminase levels [aspartate
transaminase (AST
)
and
alanine
transaminase (ALT
])
reflect acute
hepatocellular damage, as does the
gamma-glutamyl transpeptidase
(
GGT) level, which may be
used to detect
the
liver
injury associated with acute alcohol ingestion
.
The synthetic functions of
the liver are reflected in the ability to synthesise
proteins (albumin level
)
and clotting factors (prothrombin time
.)
The
standard method
of monitoring
liver function in patients with
chronic
liver disease is serial measurement of bilirubin, albumin and
prothrombin
time
.
7 |
P a g e
Alanine transaminase(SGPT)
Normal : 7 – 41 U/L
ALT found primarily in liver
.
Aspartate transaminase (SGOT
(:
Normal
–
23
–
43
U/L
AST – liver , cardiac
muscles, skeletal muscle, kidneys, brain, pancreas,
lungs, leucocytes, RBC in
decreasing order
.
Serum Enzymes – that reflect cholestasis:
3
enzymes
Alkaline Phosphatase
6
’
Nucleotidase
Alkaline Phosphatase:
<
4
fold rise can be seen
in many types of liver ds ( infective, alcoholic
hepatitis, HCC
)
<
5
times – cholestatic
liver ds, infiltrative liver ds, bone ds with rapid bone
turnover
.
In absence of
jaundice/elevated aminotransferases – elevated ALP of liver
– often early
cholestasis and less often infiltrative hepatic ds
.
Isolated rise of ALP
–
hodgkins lymphoma
,
diabetes
hyperthyroidism
CHF
amyloidosis
inf.bowel
ds
8 |
P a g e
▪ Not helpful in diff b/w
intrahep
&
extrahep cholestasis
6
’
Nucleotidase:
Normal :2 – 10 U/L
Moderate elevated – hepatitis
Highly elevated – biliary obs
Unlike ALP , the level is
unrelated with osteoblastic activity ie.. Unaffected
by bone ds
.
Test Normal
range
Bilirubin 5–17 μmol l–1
Alkaline phosphatase (ALP
)
46
–
241
IU l–1
Aspartate transaminase (AST
)
6
–
51
IU l–1
Alanine transaminase (ALT
)
6
–
51
IU l–1
Gamma-glutamyl transpeptidase
(
GGT) 10–48 IU l–1
Albumin 35–50 g l–1
Prothrombin time (PT) 12–16 s
Imaging of the liver:
Ultrasound:
This is the
first-line test
owing to its
safety
and
availability
.
It is entirely
operator dependent
.
It is useful for determining
bile duct dilatation
,
the
presence of gallstones
and the
presence of liver tumours
.
Doppler ultrasound
allows flow in the hepatic
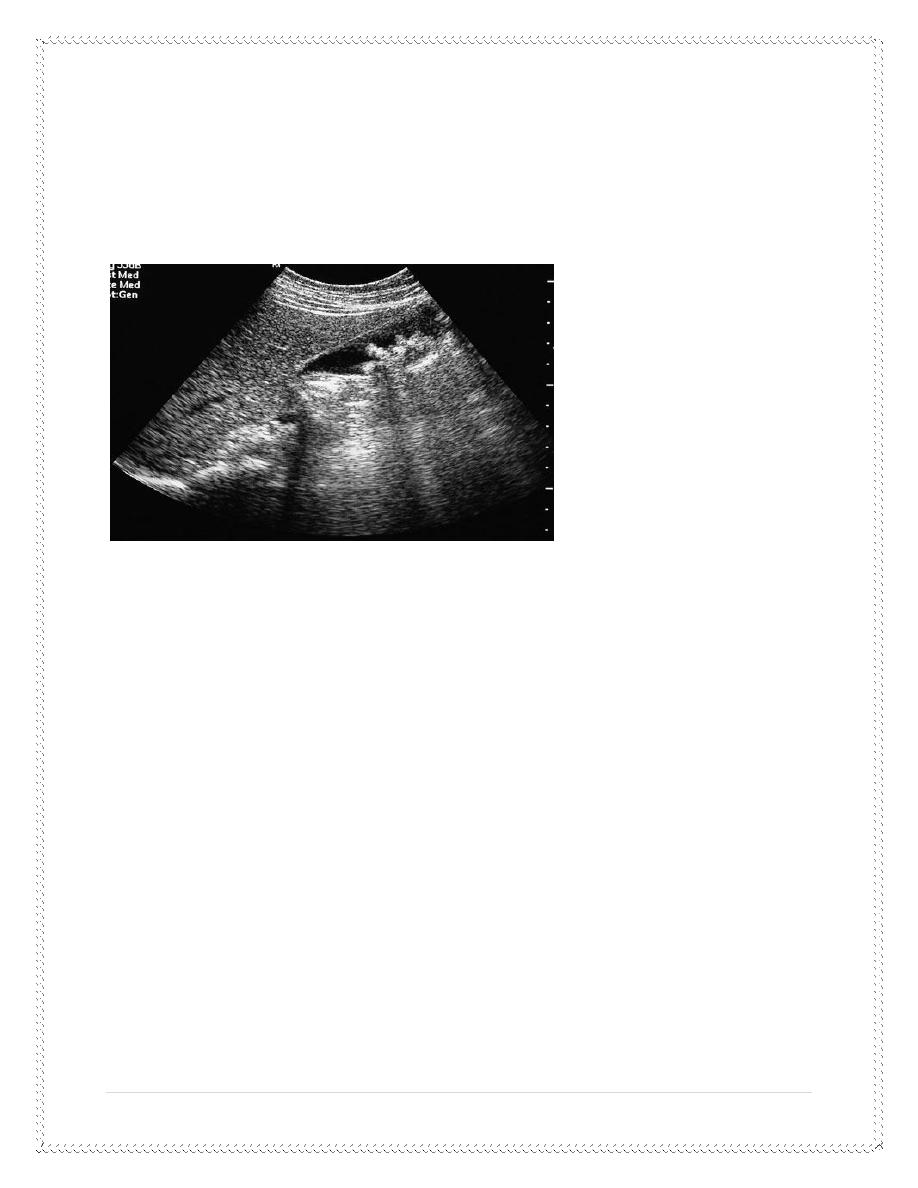
9 |
P a g e
artery, portal vein and hepatic veins to be
assessed
.
In some countries, it is used as a
screening test
for the development of
primary liver cancers in a high-risk population
.
Ultrasound
is useful in guiding the
percutaneous biopsy of a liver
lesion
Computerised tomography:
The current
‘
gold standard
’
for liver imaging is
triple-phase, multislice,
spiral computerised tomography (CT
.)
This provides fine detail of
liver lesions down to
less
than 1 cm
in diameter
and gives
information on their nature
.
Oral contrast
enhancement allows
visualisation of the stomach and
duodenum in relation to the liver hilum
.
The
early arterial phase
of the intravenous contrast
vascular enhancement
is particularly useful for detecting small liver cancers
,
owing to their
preferential arterial blood supply
.
The
venous phase
maps the branches of the
portal vein within the liver
and the drainage via the hepatic veins
.
10 |
P a g e
Inflammatory liver lesions
often exhibit
rim enhancement
with
intravenous contrast
,
whereas the common
haemangioma
characteristically shows late venous enhancement
.
The
density of any liver lesion
can be measured, which can be
useful in
establishing the presence of a
cystic lesion
.
Magnetic resonance imaging:
Magnetic resonance imaging
(
MRI
)
would appear to be as effective an
imaging modality as CT in the majority of patients with liver disease
.
It does, however, offer
several advantages
.
First
,
the use of
iodine-containing intravenous contrast agents is
precluded in many patients
because of a history of allergy.Those patients
should be offered MRI rather
than contrast CT
.
Second
,
magnetic resonance
cholangiopancreatography (MRCP) provides
excellent quality, non-invasive
imaging of the biliary tract
.
It is useful for diagnostic
questions when
ERCP has
failed or is impossible
due to previous surgery
.
Magnetic resonance angiography
(
MRA) similarly provides
high-quality
images of the hepatic artery and portal vein, without the need for
arterial
cannulation
.
It is used as an alternative
to selective hepatic angiography for diagnosis
.
It is particularly useful in
patients with
chronic
liver disease
and a
coagulopathy
in whom the
patency of the portal vein
and its branches is in
question
.
11 |
P a g e
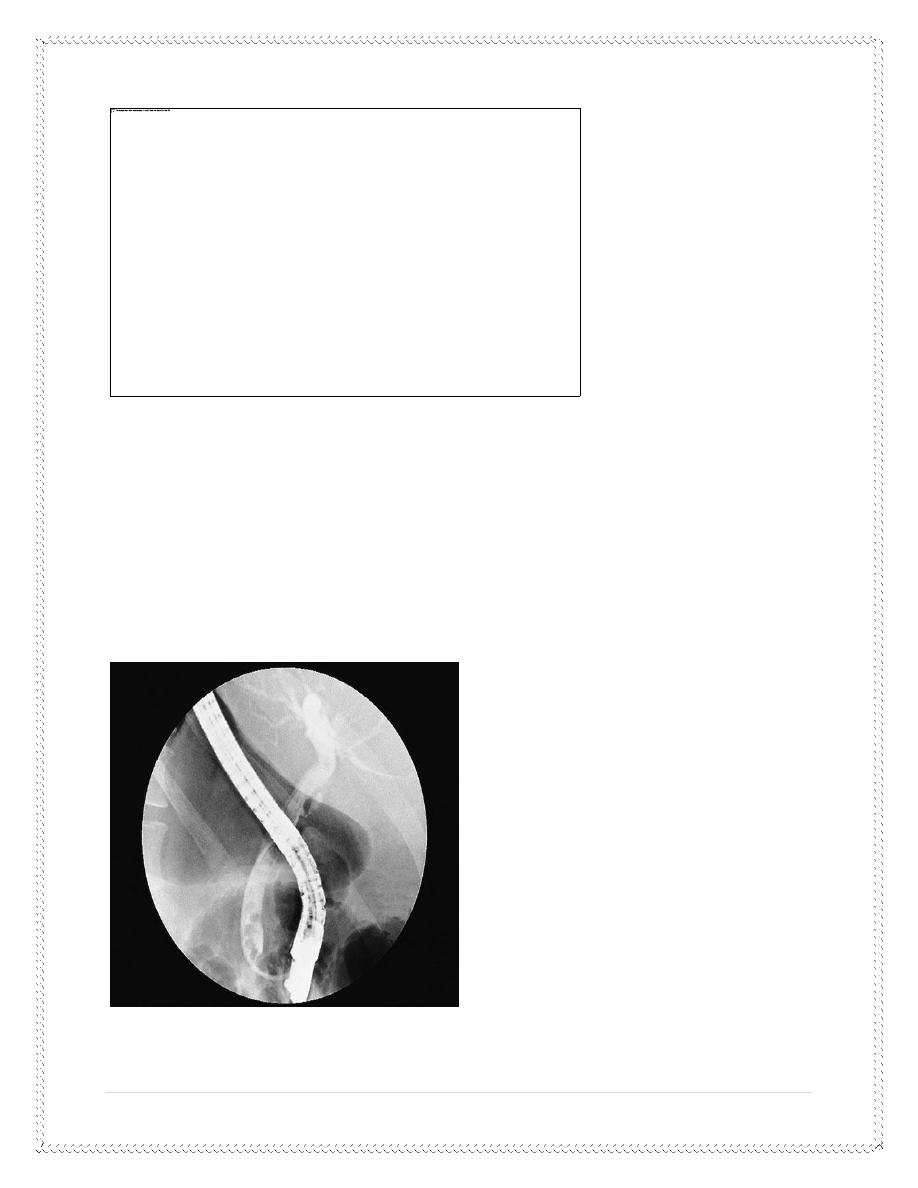
Endoscopic
retrograde
cholangiopancreatography:
ERCP is required in patients
with obstructive jaundice who cannot
undergo MRCP because of
claustrophobia
or where an
endoscopic intervention
is anticipated based on
previous
imaging [endoscopic removal of common bile duct (CBD) stones or
insertion of a palliative biliary tract
stent.
A preoperative check of
coagulation
is essential, along with
prophylactic
antibiotics
and an
explanation of the main
complications
,
which
include
12 |
P a g e
pancreatitis
,
cholangitis
and
bleeding or perforation
of the duodenum
related to
sphincterotomy
.
Percutaneous transhepatic cholangiography:
PTC is indicated where
endoscopic cholangiography has
failed
or
is
impossible
,
e.g. in patients with
previous pancreatoduodenectomy or Pólya
gastrectomy
.
It is often required in
patients with
hilar bile
duct tumours
to
guide
external
drainage
of the
bile ducts to
relieve
jaundice
and to
direct
stent
insertion
.
Angiography:
Selective visceral
angiography may be required for diagnostic purposes
but, with improving
cross-sectional imaging (CT and MR angiography), is
usually employed for
therapeutic intervention
.
Prior to liver resection
,
it may be used to visualise
the anatomy of the
hepatic artery to the right and left sides of the liver and
to confirm patency
or tumour involvement of the portal vein
.
It can also provide
additional information on the
nature of a liver nodule
,
as
primary liver tumours have a well developed arterial blood supply
.
Therapeutic interventions
include the
occlusion of arteriovenous
malformations
,
the
embolisation of bleeding sites
in the liver
and the
treatment of liver tumours
(
transarterial embolisation
,
TAE
.)
Nuclear medicine scanning:
Radioisotope scanning can
provide diagnostic information that cannot be
obtained by other imaging
modalities
.
Iodoida is a technetium-99m
(
99
mTc)-labelled radionuclide
that is
administered
intravenously, removed from the circulation
by the liver
,
13 |
P a g e
processed by hepatocytes and excreted in the
bile
.
Imaging under a gamma camera
allows its uptake and excretion to be
monitored in real time
.
These data are particularly
useful when a
bile leak
or biliary obstruction is
suspected and a non-invasive screening test is
required
.
A
sulphur colloid liver scan
allows Kupffer cell activity
in the liver to be
determined
.
This may be particularly
useful to confirm the nature of a liver lesion
;
adenomas and haemangiomas lack
Kupffer cells and hence show no
uptake of sulphur colloid
.
Laparoscopy and laparoscopic ultrasound:
Laparoscopy is useful for the
staging of
hepatopancreatobiliary cancers
.
Lesions overlooked by
conventional imaging are mainly peritoneal
metastases and superficial liver
tumours
.
Laparoscopic ultrasound
provides additional information for liver
tumours on their proximity to the major vessels and bile duct branches
.
Imaging modality Principal indication:
Ultrasound :Standard
first-line investigation
Spiral CT :Anatomical
planning for liver surgery
MRI :Alternative to spiral CT
MRCP: First-line
,
non-invasive cholangiography
ERCP :Imaging the biliary
tract when endoscopic
intervention
is anticipated (e.g. ductalstones
)
PTC :Biliary tract imaging
when ERCP impossible or failed
14 |
P a g e
Angiography :To detect
vascular involvement by tumour
Nuclear medicine :To quantify
biliary excretion and tumour
spread
Laparoscopy/Laparoscopic US
:
To detect peritoneal tumour spread and
superficial liver metastases
LIVER TRAUMA:
Liver trauma can be divided
into
blunt
and
penetrating
injuries
.
Blunt injury
produces
contusion
,
laceration
and
avulsion injuries
to the
liver, often in
association with
splenic
,
mesenteric or renal injury
.
Penetrating injuries, such as
stab
and
gunshot wounds
,
are often
associated
with chest or pericardial involvement
.
Diagnosis of liver injury:
Clinical diagnosis
suspicion of a possible liver
injury is essential
.
All lower chest and upper abdominal stab wounds
should be suspect,
especially
if considerable blood volume replacement has been required
.
Similarly
,
severe crushing injuries to the lower chest or upper
abdomen
often combine rib fractures, haemothorax and damage to the spleen
and/or liver
.
Patients with a penetrating
wound will require a laparotomy and/or
thoracotomy once active resuscitation is
under way
.
15 |
P a g e
Owing to the opportunity for
massive on-going blood loss and the rapid
development of a coagulopathy, the
patient should be directly transferred
to the operating theatre while blood
products are obtained and volume
replacement is taking place
.
Patients who are
haemodynamically stable should have an oral and
intravenous contrast-enhanced CT scan
of the chest and abdomen
.
This will demonstrate
evidence of parenchymal damage to the liver or
spleen as well as associated
traumatic injuries to their
feeding vessels
.
Free fluid can also be
clearly established and a
diagnostic
aspirate
performed
.
Additional investigations
that may be of value include
peritoneal lavage
,
which can confirm the presence of
haemoperitoneum, and
laparoscopy
,
which can demonstrate an
associated diaphragmatic rupture
.
Initial management of liver injuries
:
Penetrating
The initial management of a
patient with an upper abdominal penetrating
injury is the basis of
resuscitation
.
The initial survey assesses the patient’s
airway patency, breathing
pattern and circulation
.
Peripheral venous access is
gained with two large-bore cannulae and
blood sent for cross-match of 10 units
of blood
,
Full blood count, urea and
electrolytes, liver function tests, clotting
screen,
glucose and amylase
.
Initial volume replacement
should be with colloid or O-negative blood if
necessary
.
16 |
P a g e
Arterial blood gases should
be obtained and the patient intubated and
ventilated if the gas exchange is
inadequate
.
Intercostal chest drains
should be inserted if associated pneumothorax or
haemothorax is suspected
Once initial resuscitation
has commenced
,
the
patient should be
transferred to the operating theatre, with further
resuscitation performed
on the operating table
.
The necessity for
fresh frozen plasma
and
cryoprecipitate
should be
discussed with the
blood transfusion service immediately the patient
arrives, as these patients
rapidly develop
irreversible
coagulopathies
due to
a
lack of
fibrinogen and clotting factors
.
Blunt trauma
With severe blunt injuries
,
the plan for resuscitation and management is
as outlined above for penetrating
injuries
.
For the patient who is
haemodynamically stable, imaging by CT should be
performed to further evaluate
the nature of the injury
.
The basic surgical management
differs between penetrating and blunt
injuries thought to involve the liver
;
penetrating injuries should be
explored
,
whereas
blunt
injuries can be
treated conservatively
.
The indication for
discontinuing conservative treatment for blunt trauma
would be
evidence of on-going blood loss
despite correction of any
underlying coagulopathy
and the
development of signs of generalised
peritonitis
.
The surgical approach to liver trauma
A
rooftop incision
gives excellent visualisation
of the liver and spleen and,
if necessary, can be extended upwards for a median
sternotomy
.
17 |
P a g e
A stab incision in the liver
can be sutured with a fine absorbable
monofilament suture
.
If necessary, this may be
facilitated by producing vascular inflow
occlusion by placing an atraumatic
clamp across the foramen of Winslow
(the
Pringle manoeuvre
(
Lacerations to the hepatic
artery should be identified by placing an
atraumatic bulldog clamp on the
proximal vessel prior to repair with 5/0 or
6/0 Prolene suture
.
If unavoidable, the hepatic
artery may be ligated, although parenchymal
necrosis and abscess formation will
result in some individuals
.
Portal vein injuries should
be repaired with 5/0 Prolene, again with
exposure of the vessel being
facilitated by the placement of an atraumatic
vascular clamp
.
Diffuse parenchymal injuries
should be treated by
packing the liver to
produce
haemostasis
.
This is effective for the
majority of liver injuries if the liver is packed
against the
natural contour of the diaphragm by packing
from below
.
Large abdominal packs should be used to ease
their removal, and the
abdomen closed to facilitate compression
of the parenchyma
.
Necrotic tissue should be
removed, but poorly perfused, though viable,
liver left
in situ
.
If packing is necessary, the patient
should have the packs removed
after 48
hours, and usually no further surgical intervention is required
.
Antibiotic cover
is advisable, and full reversal of any coagulopathy is
essential
.
Other complications of liver trauma:
18 |
P a g e
A
subcapsular or intrahepatic
haematoma
requires
no specific
intervention and should be allowed to resolve spontaneously
.
Abscesses
may form as a result of
secondary infection of an area of
parenchymal ischaemia, especially after
penetrating trauma
.
Treatment
is with
systemic antibiotics
and
aspiration under ultrasound
guidance once the necrotic tissue has
liquefied
.
Bile collections
require aspiration under
ultrasound guidance or
percutaneous insertion of a pigtail drain
.
The site of origin of a
biliary fistula
should be determined by
endoscopic
or percutaneous
cholangiography, and biliary decompression
achieved by
nasobiliary or percutaneous transhepatic
drainage or stent insertion
.
Late vascular complications
include hepatic artery
aneurysm and
arteriovenous or arteriobiliary fistulae
.
These are best treated
nonsurgically by a specialist hepatobiliary
interventional radiologist
.
The feeding vessel can be embolised
transarterially
.
Hepatic failure
may occur following extensive
liver trauma
.
This will usually reverse
with conservative supportive treatment if the blood
supply and biliary drainage
of the liver are intact
Management of liver trauma:
■
Remember
associated injuries
■
At-risk
groups
Stabbing/gunshot
in lower chest or upper abdomen
Crush injury
with multiple rib fractures
19 |
P a g e
■
Resuscitate
Airway
Breathing
Circulation
■
Assessment
of injury
Spiral CT
with contrast
Laparotomy
if haemodynamically unstable
■
Treatment
Correct
coagulopathy
Suture
lacerations
Resect if
major vascular injury
Packing if
diffuse parenchymal injury
Other complications of liver trauma:
Other
complications of liver trauma
■
Intrahepatic
haematoma
■
Liver
abscess
■
Bile
collection
■
Biliary
fistula
■
Hepatic
artery aneurysm
■
Arteriovenous
fistula
■
Arteriobiliary
fistula
■
Liver
failure
20 |
P a g e
Pyogenic liver abscess:
The aetiology of a pyogenic
liver abscess is
unexplained
in the majority of
patients
.
It has an increased incidence
in the
elderly
,
diabetics
and the
immunosuppressed
,
who usually present with
anorexia
,
fevers
and
malaise
,
accompanied by
right upper quadrant
discomfort
.
The
diagnosis is suggested
by the finding of a
multiloculated cystic mass
on ultrasound or CT scan
.
And
is
confirmed by aspiration for culture and sensitivity
.
END of this lecture …
