Infertility and ED
Dr. Mohammed BassilDefinition of infertility
Failure of conception after at least 12 months of unprotected intercourse. The chance of a normal couple conceiving is estimated at 20%-25% per month, 75% by 6 months, and 90% at 1 year.Epidemiology
Up to 50% of infertility is due to male factors. Up to 25% of couples may be affected at some point in their reproductive years.
Pathophysiology
Failure of fertilization of the normal ovum due to defective sperm development, function, or inadequate numbers. There may be abnormalities of morphology (teratospermia), motility (asthenospermia), low sperm numbers (oligospermia), or absent sperm (azoospermia). Abnormal epididymal function may result in defective spermatozoa maturation or transport, or induce cell deathEtiology
•Idiopathic (25%)•Varicocele (present in 40%)
•Cryptorchidism (undescended testes)
•Functional sperm disorders: immunological infertility (sperm antibodies); head or tail defects; Kartagener's syndrome (immotile cilia); dyskinetic cilia syndrome
•Erectile or ejaculatory problems
•Testicular injury: orchitis (post-pubertal, bilateral mumps orchitis); testicular torsion; trauma; radiotherapy
Etiology
Endocrine disorders: Kallmann's syndrome (isolated gonadotrophin deficiency causing hypogonadism); Prader–Willi syndrome (hypogonadism, short stature, hyperphagia, obesity); pituitary gland adenoma, radiation, or infection.
Hormone excess: excess prolactin (pituitary tumour); excess androgen (adrenal tumour, congenital adrenal hyperplasia, anabolic steroids); excess oestrogens
Etiology
•Genetic disorders: Kleinfelter's syndrome (47XXY) involves azoospermia, ↑ FSH/LH and ↓ testosterone; XX male; XYY syndrome•Male genital tract obstruction: congenital absence of vas deferens; epididymal obstruction or infection; Mأullerian prostatic cysts; groin or scrotal surgery
•Systemic disease: renal failure; liver cirrhosis; cystic fibrosis
•Drugs: chemotherapy; alcohol; marijuana; sulphasalazine; smoking
•Environmental factors: pesticides; heavy metals; hot baths
History
•Sexual: duration of problem; frequency and timing of intercourse; previous successful conceptions; previous birth control; erectile or ejaculatory dysfunction.•Developmental: age at puberty; history of cryptorchidism; gynaecomastia.
•Medical and surgical: detailed assessment for risk factors—recent febrile illness; post-pubertal mumps orchitis; varicocele; testicular torsion, trauma, or tumour; sexually transmitted diseases; genitourinary surgery; radiotherapy; respiratory diseases associated with ciliary dysfunction; diabetes.
History
•Drugs and environmental: previous chemotherapy; exposure to substances which impair spermatogenesis or erectile function; alcohol consumption; smoking habits; hot baths.•Family: hypogonadism; cryptorchidism.
Examination
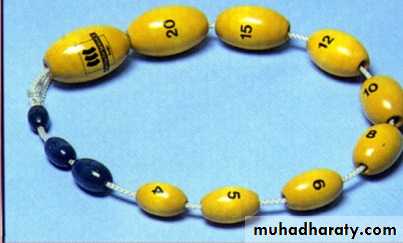
Perform a full assessment of all systems, with attention to general appearance (evidence of secondary sexual development; signs of hypogonadism; gynaecomastia). Urogenital examination should include assessment of the penis (Peyronie's plaque, phimosis, hypospadias); measurement of testicular consistency, tenderness, and volume with a Prader orchidometer (normal >20ml; varies with race); palpate epididymis (tenderness, swelling) and spermatic cord (vas deferens present or absent, varicocele); digital rectal examination of prostate.Investigation of male infertility
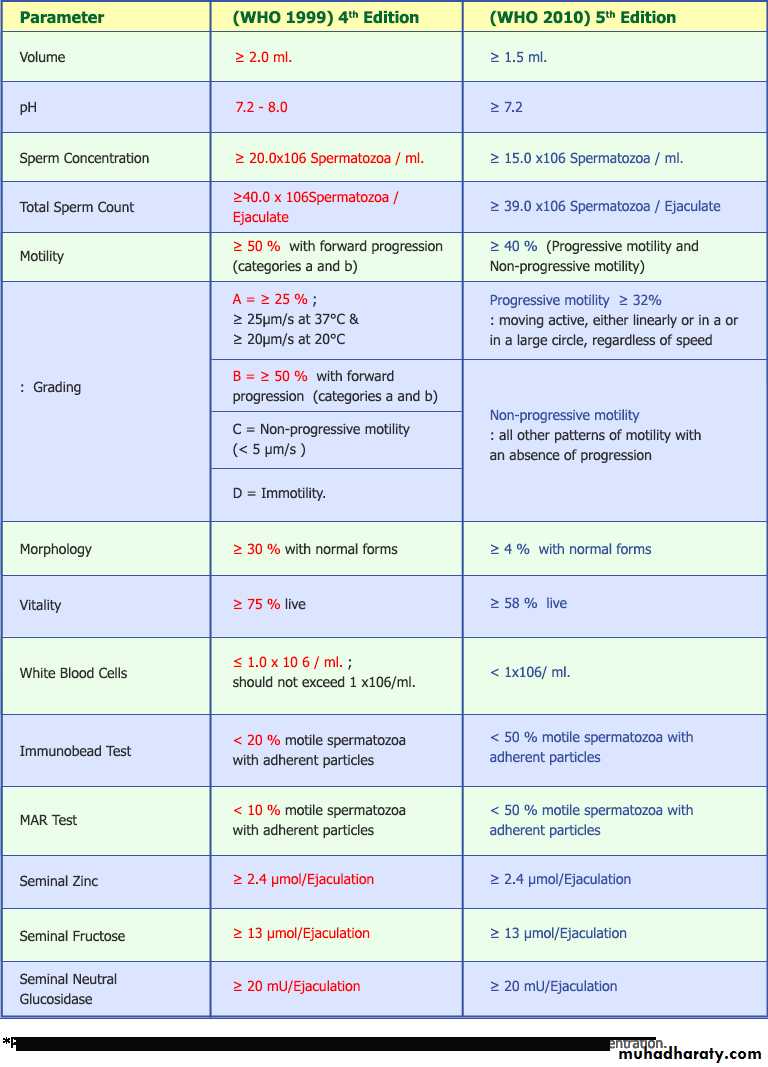
Basic investigationsSemen analysis 2 or 3 specimens over several weeks, collected after 3-7 days of sexual abstinence. Deliver specimens to the laboratory within 1h. Ejaculate volume, liquefaction time, and pH are noted . Microscopy techniques measure sperm concentration, total numbers, morphology, and motility. The mixed agglutination reaction (MAR test) is used to detect antisperm antibodies. The presence of leucocytes (>1 أ— 106/ml of semen) suggests infection, and cultures should be requested.
Hormone measurement Serum FSH, LH, and testosterone. In cases of isolated low testosterone level, it is recommended to test morning and free testosterone levels. Raised prolactin is associated with sexual dysfunction, and may indicate pituitary disease.
Investigation of male infertility
Special investigationsChromosome analysis
Indicated for clinical suspicion of an abnormality (azoospermia or oligospermia, small atrophic testes with ↑ FSH).
Testicular biopsy
Performed for azoospermic patients, to differentiate between idiopathic and obstructive causes. May also be used for sperm retrieval.
Investigation of male infertility
Sperm function tests•Post coital test: cervical mucus is taken just before ovulation, and within 8 hours of intercourse, and microscopy performed. Normal results shows >10 sperm per high-powered field, the majority demonstrating progressive motility. Abnormal results indicate inappropriate timing of the test; cervical mucus antisperm antibodies; abnormal semen; inappropriately performed coitus.
•Sperm penetration test: a sample of semen is placed directly onto pre-ovulatory cervical mucus on a slide and the penetrative ability of spermatozoa observed.
•Sperm-cervical mucus test: a specimen of semen (control), and one mixed with cervical mucus are placed separately on a slide, and observed for 30 minutes. More than 25% exhibiting jerking movements in the mixed sample (but not the control) is a positive test for antisperm antibodies.
Treatment options for male factor infertility
General
Modification of life style factors (reduce alcohol consumption; avoid hot baths).
Medical treatment
Correct any reversible causative factors.Treatment options for male factor infertility
Hormonal•Secondary hypogonadism (pituitary intact) may respond to human chorionic gonadotrophin (hCG) 2000IU subcutaneously 3 times a week, which stimulates an increase in testosterone and testicular size. If the patient remains azoospermic after 6 months of treatment, FSH is added (human recombinant FSH or human menopausal gonadotrophin). Alternatively, pulsatile LHRH can be administered subcutaneously via a minipump.
Treatment options for male factor infertility
• Testosterone deficiency requires testosterone replacement therapy.• Hyperprolactinaemia is treated with dopamine agonists.
• Anti-oestrogens (clomiphene citrate 25mg OD) are often used empirically to increase LHRH, which stimulates endogenous gonadotrophin secretion.
Treatment options for male factor infertility
Erectile and ejaculatory dysfunctionErectile dysfunction may be treated conventionally (oral, intraurethral, intracavernosal drugs; vacuum devices or prostheses). Ejaculatory failure may respond to sympathomimetic drugs (desipramine) or electroejaculation (used in spinal cord injury), where an electrical stimulus is delivered via a rectal probe to the postganglionic sympathetic nerves that innervate the prostate and seminal vesicles.
Antisperm antibodies
Corticosteroids have been used, but assisted conception methods are usually required.
Treatment options for male factor infertility
Surgical treatment
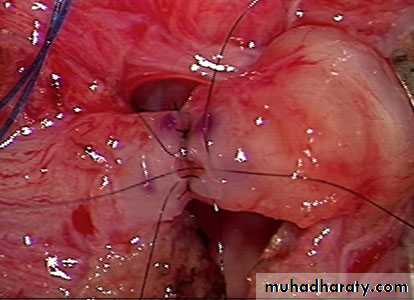
Genital tract obstruction
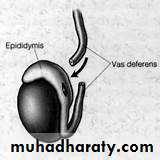
•Epididymal obstruction can be overcome by microsurgical anastomosis between the epididymal tubule and vas (epididymovasovasostomy).
•Vas deferen obstruction is treated by microsurgical reanastomosis of ends of the vas, and is used for vasectomy reversal.
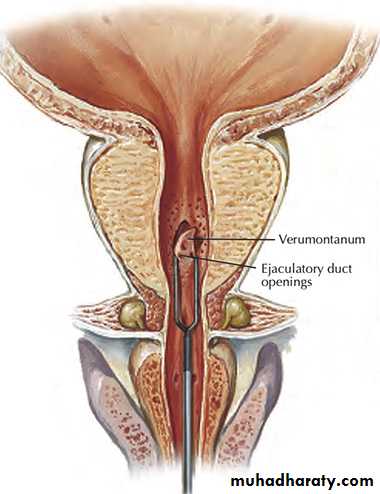
•Ejaculatory duct obstruction requires transurethral resection of the ducts.
Varicocele
Repaired by embolization or open/laparoscopic surgical ligation.
Treatment options for male factor infertility
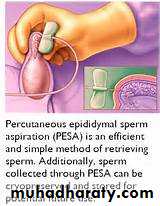
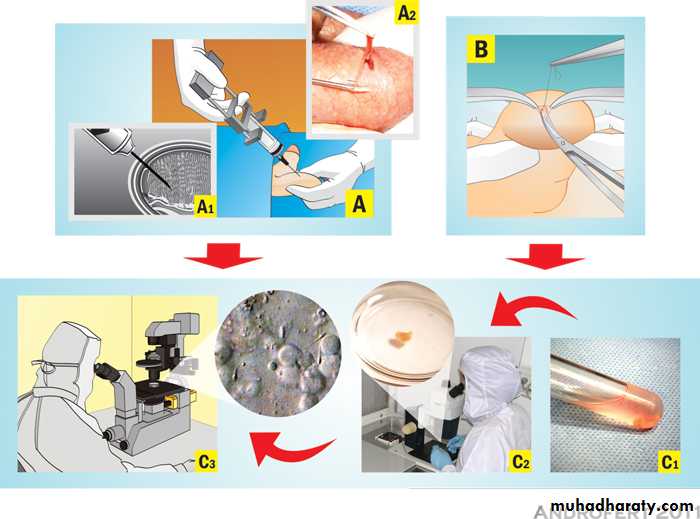
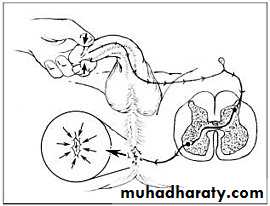
Assisted reproductive techniques (ART)Sperm extraction
Used for obstructive azoospermia. Sperm are removed directly from the epididymis by microsurgical epididymal sperm aspiration (MESA) or by percutaneous retrieval (PESA). If these methods fail, testicular sperm extraction (TESE) or aspiration (TESA) may be tried. Sperm undergo cryopreservation until required. Later, they are separated from seminal fluid by dilution and centrifuge methods, with further selection of motile sperm and normal forms using Percoll gradiant techniques.
Treatment options for male factor infertility
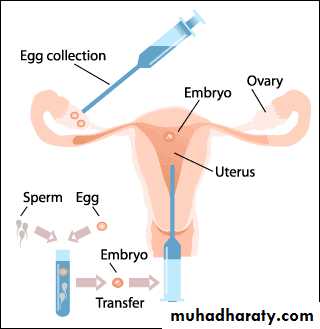
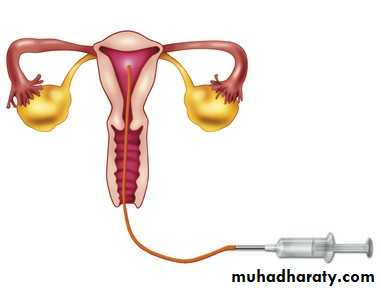
Assisted conception•Intrauterine insemination (IUI) Following ovarian stimulation, sperm are placed directly into the uterus.
•In vitro fertilization (IVF) Controlled ovarian stimulation produces oocytes which are then retrieved under transvaginal USS-guidance. Oocytes and sperm are placed in a Petri dish for fertilization to occur. Embryos are transferred to the uterine cavity. Pregnancy rates are 20–30% per cycle.
•Gamete intrafallopian transfer (GIFT) Oocytes and sperm are mixed and deposited into the fallopian tubes via laparoscopy. Variations include zygote intrafallopian transfer (ZIFT) and tubal embryo transfer (TET).
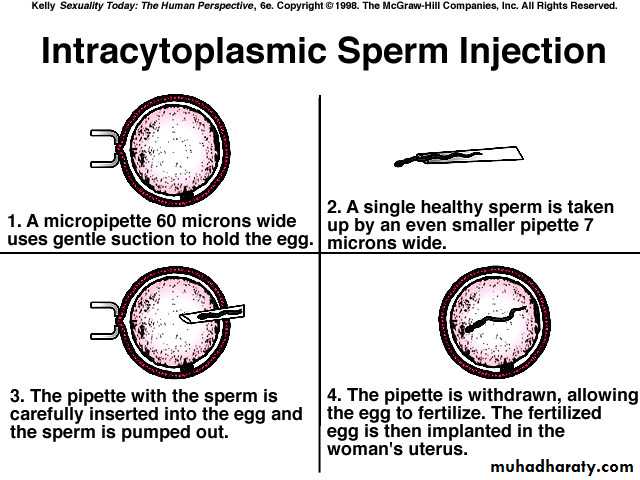
•Intracytoplasmic Sperm injection (ICSI) A single spermatozoon is injected directly into the oocyte cytoplasm (through the intact zona pellucida). Pregnancy rates are 15–22% per cycle.
Disorders of erectile function(impotence)
Impotence: evaluationDefinition
Impotence (also called erectile dysfunction or ED) describes the persistent inability to achieve or maintain a penile erection sufficent for sexual intercourse.
Epidemiology
Moderate to severe ED is found in ~10% of men aged 40-70 years. Prevalence increases with age.
Aetiology
ED is generally divided into psychogenic and organic causes , although it is often multifactorial.
Impotence: evaluation
HistorySexual: onset of ED (sudden or gradual); duration of problem; presence of erections (nocturnal, early morning, spontaneous); ability to maintain erections (early collapse, not fully rigid); loss of libido; relationship issues (frequency of intercourse and sexual desire, relationship problems).
Medical and surgical: hypertension; cardiac disease; peripheral vascular disease; diabetes mellitus; endocrine or neurological disorders; pelvic surgery, radiotherapy, or trauma (damaging innervation and blood supply to the pelvis and penis).
Drugs: enquire about current medications and ED treatments already tried (and outcome).
Social: smoking, alcohol consumption.
Impotence: evaluation
Examination
Full physical examination (CVS, abdomen, neurological); digital rectal examination to assess prostate; external genitalia assessment to document foreskin phimosis and penile lesions (Peyronie's plaques); confirm presence, size, and location of testicles. The bulbocavernosus reflex can be performed to test integrity of spinal segments S2–4 (squeezing the glans causes anal sphincter and bulbocavernosal muscle contraction).
Investigation
•Blood tests:fasting glucose; PSA; serum testosterone; sex hormone binding globulin; LH/FSH; prolactin; thyroid function test; fasting lipid profile.•Nocturnal penile tumescence testing: Rigiscan device contains 2 rings which are placed around base and distal penile shaft to measure tumescence and number, duration, and rigidity of nocturnal erections.
•Colour Doppler USS: measures arterial peak systolic and end diastolic velocities,1 pre and post intracavernosal injection of PGE1.
Causes of erectile dysfunction IMPOTENCE
Causes of erectile dysfunction IMPOTENCECauses of erectile dysfunction IMPOTENCE
Impotence: treatment
Psychosexual therapy
Aims to understand and address underlying psychological issues, and provides information and treatment in the form of sex education, instruction on improving partner communication skills, cognitive therapy, and behavioural therapy (programmed re-learning of couple's sexual relationship).
Oral medication
Phosphodiesterase type-5 (PDE5) inhibitors: sildenafil (Viagra); tadalafil (Cialis); vardenafil (Levitra). PDE5 inhibitors enhance cavernosal smooth muscle relaxation and erection by blocking the breakdown of cGMP. Sexual stimulus is still required to initiate events. Side-effects: headache; flushing; visual disturbance. Contraindications: patients taking nitrates; recent myocardial infarction; recent stroke; hypotension; unstable angina.
Impotence: treatment
Androgen replacement therapytestosterone replacement is indicated for hypogonadism. It is available in oral, intramuscular, pellet, patch, and gel forms. In older men, it is recommended that PSA is checked before and during treatment.
Intraurethral therapy
alprostadil (MUSE). Synthetic prostaglandin E1 (PGE1) pellet administered into the urethra via a specialized applicator. Once inserted, the penis is gently rolled to encourage the pellet to dissolve into the urethral mucosa, from where it enters the corpora. Side-effects: penile pain; priapism; local reactions.
Impotence: treatment
Intracavernosal therapyalprostadil/Caverjet (synthetic PGE1); papaverine (smooth muscle relaxant) ± phentolamine (a-adrenoceptor agonist).
Vacuum erection device
Penile prosthesis
semi-rigid, malleable, and inflatable penile prostheses are available for surgical implantation into the corpora to provide penile rigidity and sufficient erectile size for sexual intercourse. Side-effects: mechanical failure; erosions; infections.