Baghdad College of Medicine / 4
th
grade
Student’s Name :
Dr. Mohammed Basil
Lec. 5
Urinary Tract Infection
Tues. 19 / 4 / 2016
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2015 – 2016
UTI Dr. Mohammed Basil
19-4-2016
2
©Ali Kareem 2015-2016
Urinary Tract Infection
What do we by UTI ?
o The inflammatory response of the urothelium to bacterial invasion.
Definitions
o Bacteriuria is the presence of bacteria in the urine .
o Pyuria is the presence of white blood cells (WBCs) in the urine.
o Sterile pyuria.
Classifications
o Uncomplicated UTI is one occurring in a patient with a structurally and
functionally normal urinary tract.
o Uncomplicated UTIs, and if there is an underlying anatomical or
structural abnormality.
o Isolated UTI has an interval of at least 6 months between infections.
o Recurrent UTI is >2 infections in 6 months, or 3 within 12 months.
o Unresolved infection is failure of the initial treatment course to eradicate
bacteria from the urine.
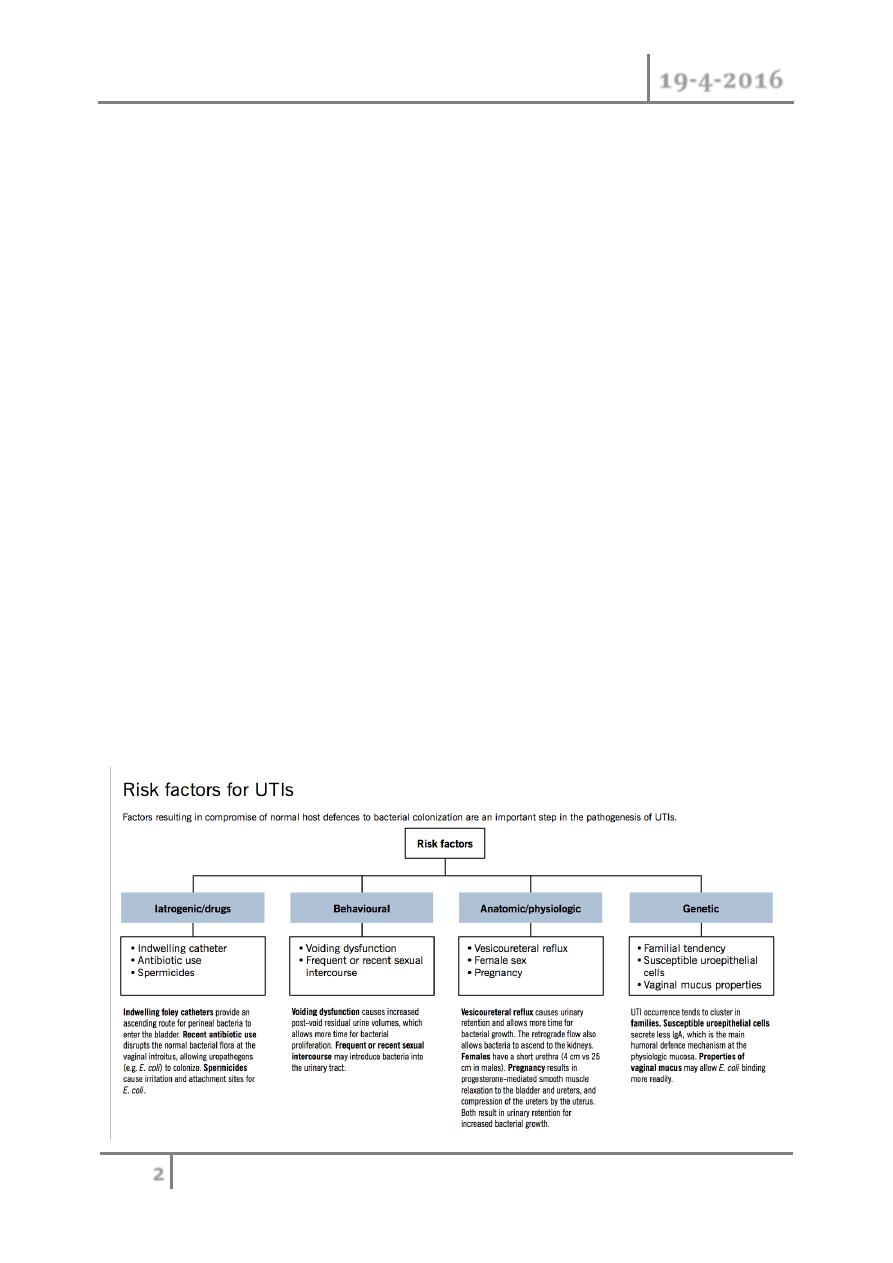
What are the risk factors for UTI ?

UTI Dr. Mohammed Basil
19-4-2016
3
©Ali Kareem 2015-2016
Incidence
o Age Female Male
o Infants (<1 year) 1% 3%
o School (<15 years old) 1–3% <1%
o Reproductive 4% <1%
o Elderly 20–30% 10%
Investigations
o Urine dipstick.
o Urine microscopy.
o Urine culture and collection.
Further workup is needed if the following occur :
o Symptoms and signs of upper tract infection (flank pain, malaise, fever)
o that suggest acute pyelonephritis, a pyonephrosis, or perinephric abscess
o Recurrent UTIs develop .
o The patient is pregnant.
o Unusual infecting organism (e.g., Proteus), suggesting the possibility of
an infection stone
Factors protecting against UTI are the following :
1. Mechanical flushing effect of urine .
2. A mucopolysaccharide coating of the bladder.
3. Low urine pH and high osmolarity reduce bacterial growth.
4. Urinary immunoglobulin (IgA) inhibits bacterial adherence.
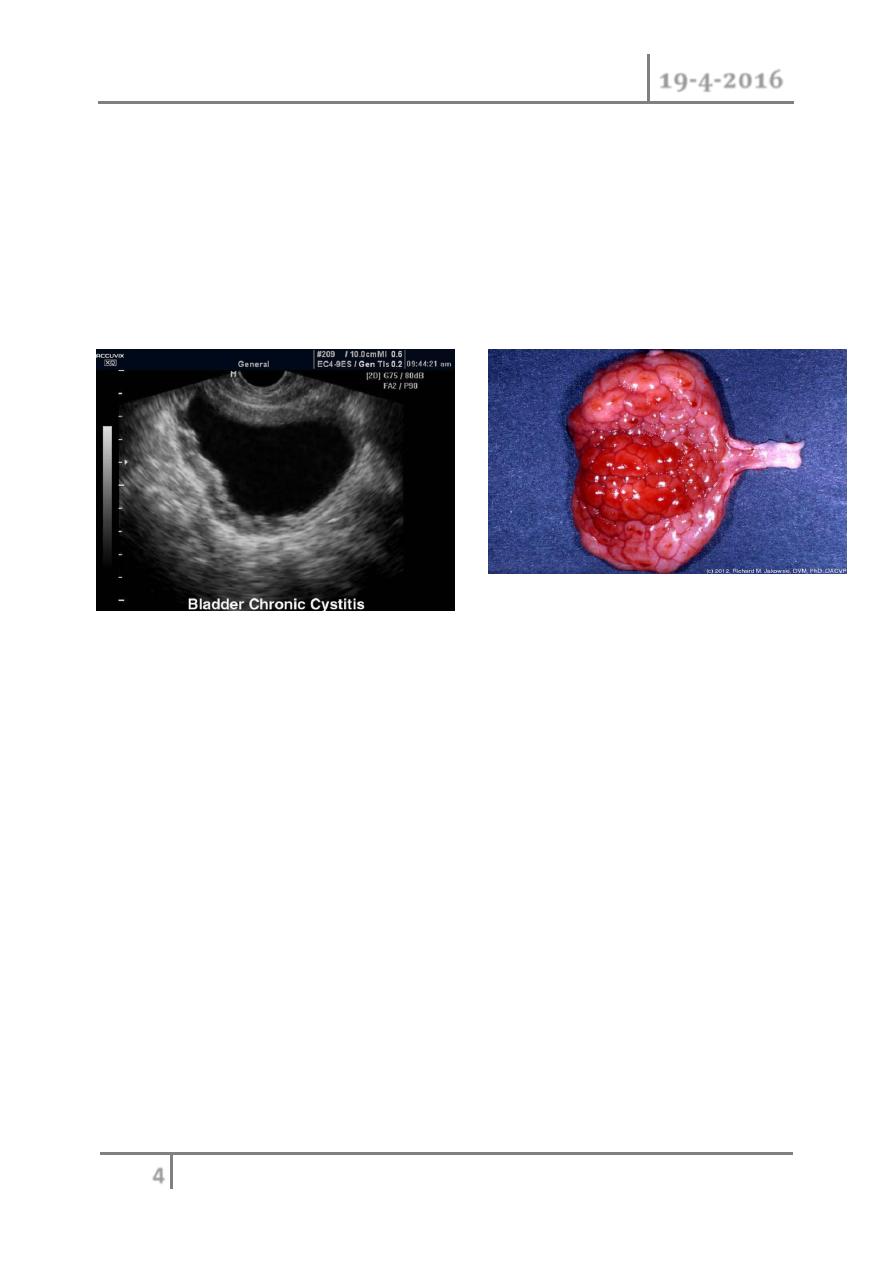
Lower urinary tract infection
o Cystitis is infection and/or infl ammation of the bladder.
o frequency, dysuria, urgency, offensive Urine, suprapubic
pain,hematuria,fever(uncommon), and incontinence.
o Investigation
o Dipstick and microscopy of midstream specimen of urine (MSU).
o Noninfective hemorrhagic cystitis.
UTI Dr. Mohammed Basil
19-4-2016
4
©Ali Kareem 2015-2016
o (radiation cystitis—bladder capacity is reduced and multiple areas of
mucosal telangiectasia are seen cystoscopically and drug-induced
cystitis(e.g., cyclophosphamide )
o Urethritis is inflammation of the urethra. Urethritis in men is a sexually
transmitted disease, which presents with dysuria and urethral discharge.
o Gonococcal urethritis (GU)
o Nongonococcal urethritis (NGU)
Upper urinary tract infection
Acute pyelonephritis
o A clinical diagnosis is based on the presence of fever, flank pain, and
tenderness often with an elevated white count. Nausea and vomiting are
common.
o Differential diagnosis includes cholecystitis, pancreatitis, diverticulitis,
and appendicitis.
o Risk factors of acute pyelonephritis
o These include vesicoureteric reflux (VUR), urinary tract obstruction,
calculi,
o spinal cord injury (neuropathic bladder), diabetes mellitus, congenital
malformation, pregnancy, and indwelling catheters.
Pathogenesis and microbiology of acute pyelonephritis
o Initially, there is patchy infi ltration of neutrophils and bacteria in the
parenchyma. Later changes include the formation of infl ammatory bands
extending from renal papilla to cortex, and small cortical abscesses.
UTI Dr. Mohammed Basil
19-4-2016
5
©Ali Kareem 2015-2016
o 80%of infections are secondary to E. coli (possessing P pili virulence
factors).
o Other infecting organisms include enterococci (Streptococcus
faecalis),Klebsiella, Proteus, and Pseudomonas.
Investigation and treatment of acute pyelonephritis
o For those patients who have a fever but are not systemically ill,
outpatient management is reasonable. Culture the urine and start oral
antibiotics.
o oral agents include the following:
o Fluoroquinolones (ciprofl oxacin 500 mg PO bid, or levofl oxacin 750
mg PO qd) empiric treatment.
o Trimethoprim-sulfamethoxazole (TMP-SMZ) as alternative.
o Therapy should be continued for 10–14 days and milder cases may be
treated for 7 days.
o If the patient is systemically ill, obtain culture urine and blood and start
IV fl uids and IV antibiotics.
o Treat patient until afebrile for 24 hours, then switch to oral agents based
on sensitivities as above for a total of 14 days of antibiotic therapy.
o Empiric choices include the following:
Ampicillin (2 g IV q6h) and gentamicin (1.5 mg/kg IV q8h or 3
mg/kg daily dosing)
Ceftriaxone (1 g IV qd)
Intravenous fluoroquinolones (e.g., ciprofloxin 200–400 mg IV
q12h).
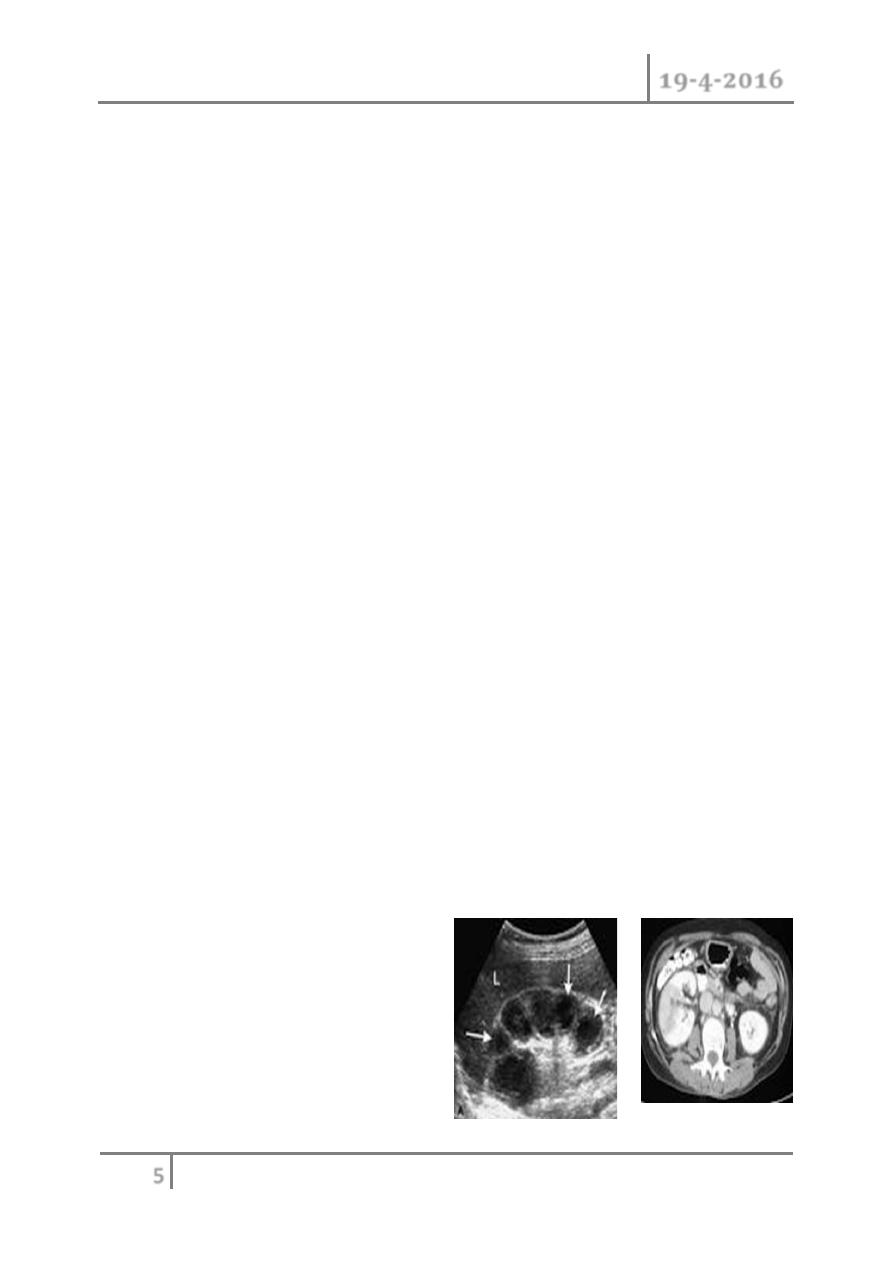
o Arrange a KUB radiograph and renal ultrasound to see if there is an
underlying upper tract abnormality, unexplained hydronephrosis, or
(rarely) gas surrounding the kidney (suggesting emphysematous
pyelonephritis).
o Some centers will use a CT
urogram as the first screening
tool. However, if the patient
does not respond within 3 days
to this regimen of IV antibiotics
a CT urogram is essential.
UTI Dr. Mohammed Basil
19-4-2016
6
©Ali Kareem 2015-2016
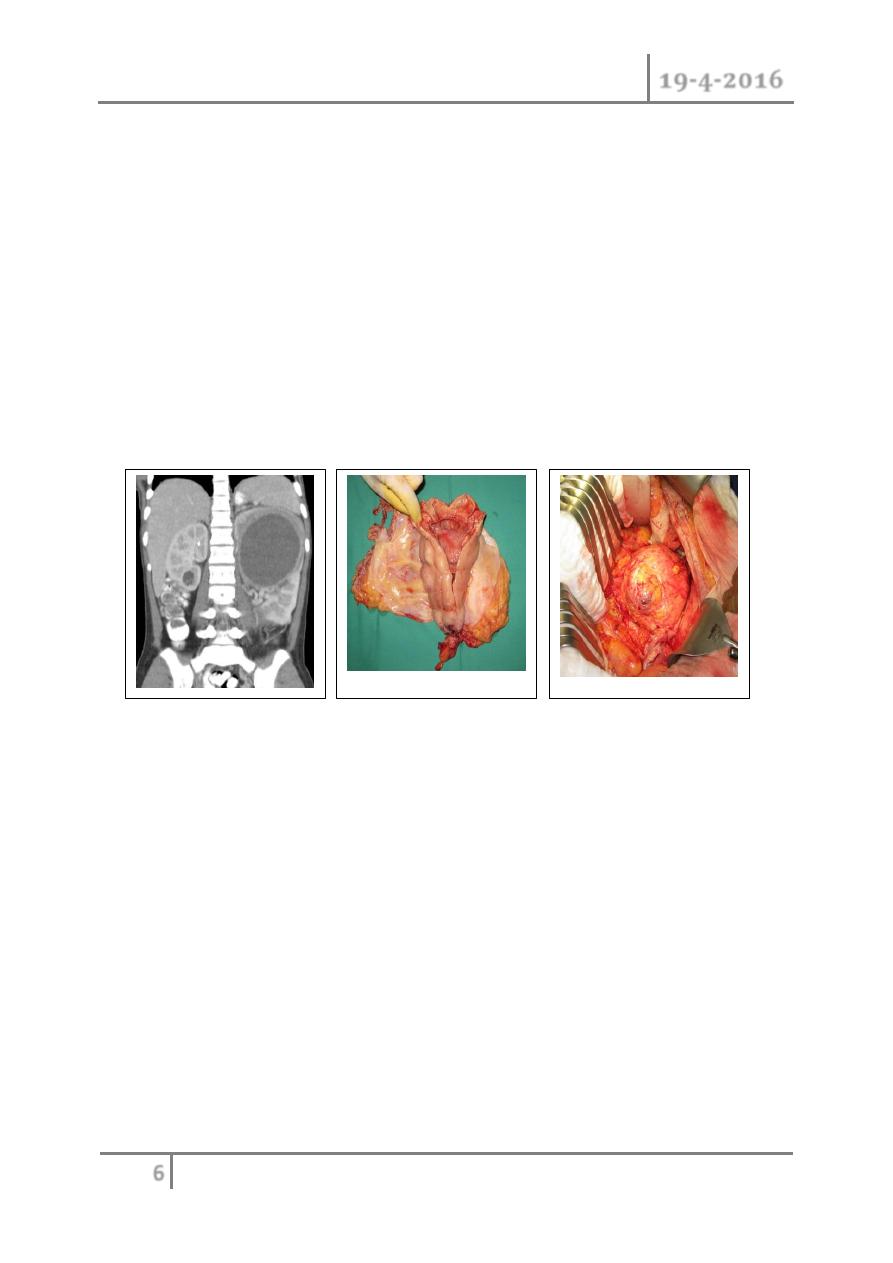
Pyonephrosis and perinephric abscess
o Pyonephrosis is an infected hydronephrosis. Pus accumulates within the
renal pelvis and calyces.
o The causes are essentially those of hydronephrosis, where infection has
supervened.
o Patients with pyonephrosis are usually very ill, with a high fever, flank
pain, and tenderness.
o will usually be investigated urgently by a renal ultrasound or CT
urogram.
o Treatment consists of IV antibiotics , IV fl uids,and percutaneous
nephrostomy insertion for drainage.
o Perinephric abscess develops as a consequence of extension of infection
outside the parenchyma of the kidney in acute pyelonephritis or, more
rarely today, from hematogenous spread of infection.
o The abscess develops within Gerota (perinephric) fascia. These patients
are often diabetic, and associated conditions such as an obstructing
ureteric calculus may be the precipitating event.
o Imaging studies will establish the diagnosis and allow radiographically
controlled percutaneous drainage of the abscess. If the pus collection is
large, formal open surgical drainage under general anesthetic will
provide more effective drainage.
UTI Dr. Mohammed Basil
19-4-2016
7
©Ali Kareem 2015-2016
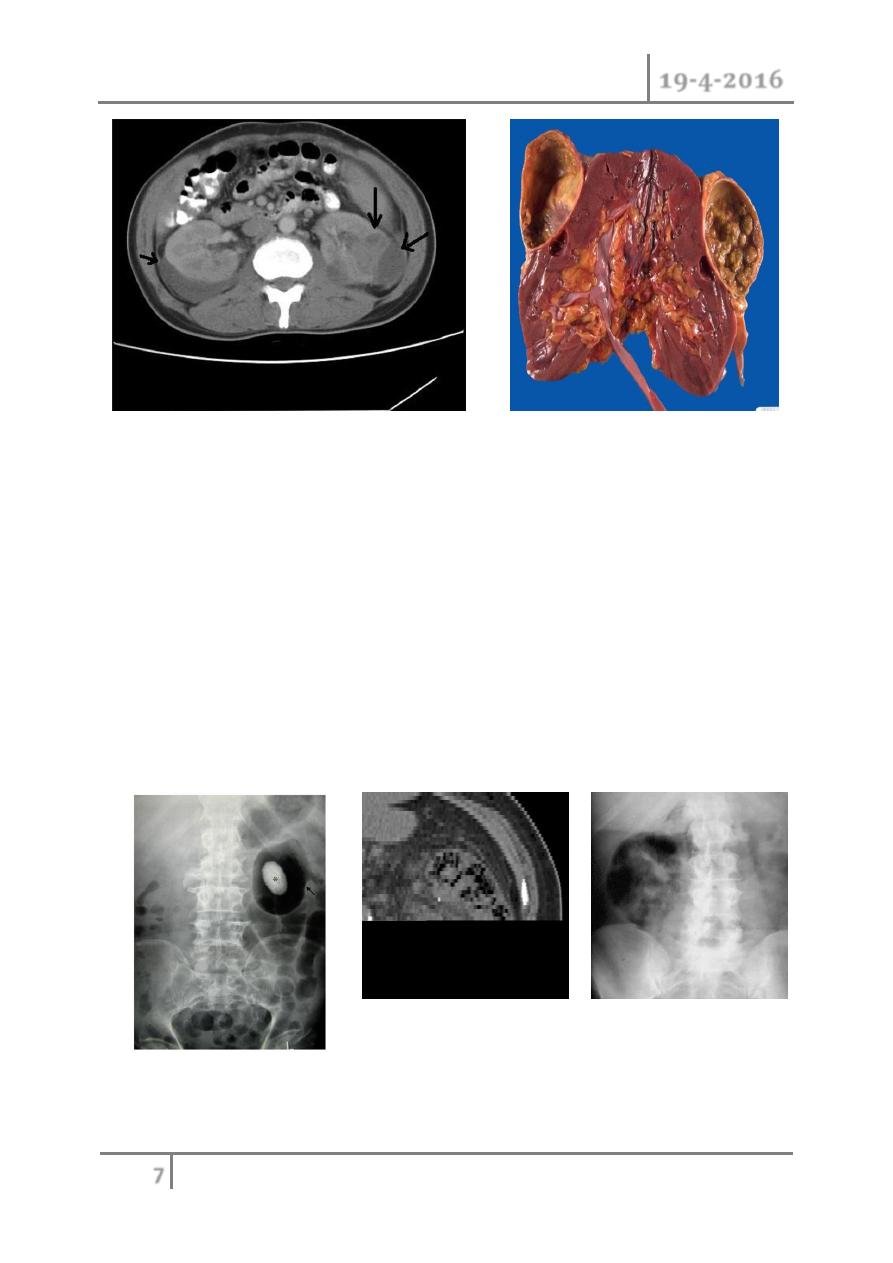
Emphysematous pyelonephritis
o This is a rare, severe form of acute pyelonephritis caused by gas-forming
organisms. It is characterized by high fever and abdominal pain, with
radiographic evidence of gas within and around the kidney.
o It usually occurs in diabetics and,in many cases, is precipitated by
urinary obstruction.
o It is commonly caused by E. coli, less frequently by Klebsiella and
Proteus.
o On KUB radiograph, crescent- or kidney-shaped distribution of gas may
been seen around the kidney.
UTI Dr. Mohammed Basil
19-4-2016
8
©Ali Kareem 2015-2016
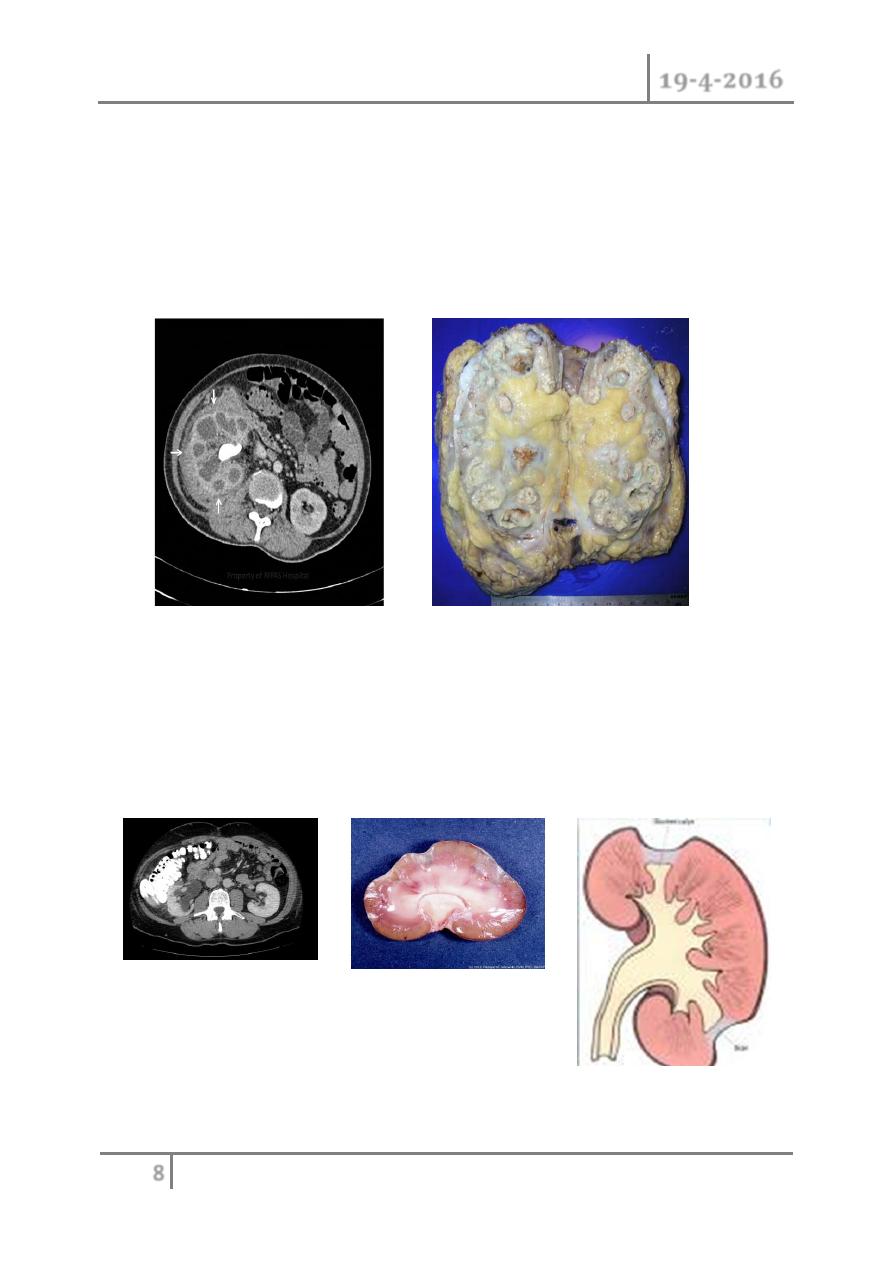
Xanthogranulomatous pyelonephritis
o This is a severe renal infection usually, although not always, occurring in
association with underlying renal calculi and renal obstruction.
o The severe infection results in destruction of renal tissue, leading to a
non-functioning kidney.
o E. coli and Proteus are common causative organisms.
Chronic pyelonephritis
o It is not a specifically clinically based diagnosis.
o The appearance, either pathologically or radiologically, is one of renal
scarring.
o Scars can be seen radiologically on a renal ultrasound, an IVU, renal
isotope scan, or a CT
UTI Dr. Mohammed Basil
19-4-2016
9
©Ali Kareem 2015-2016
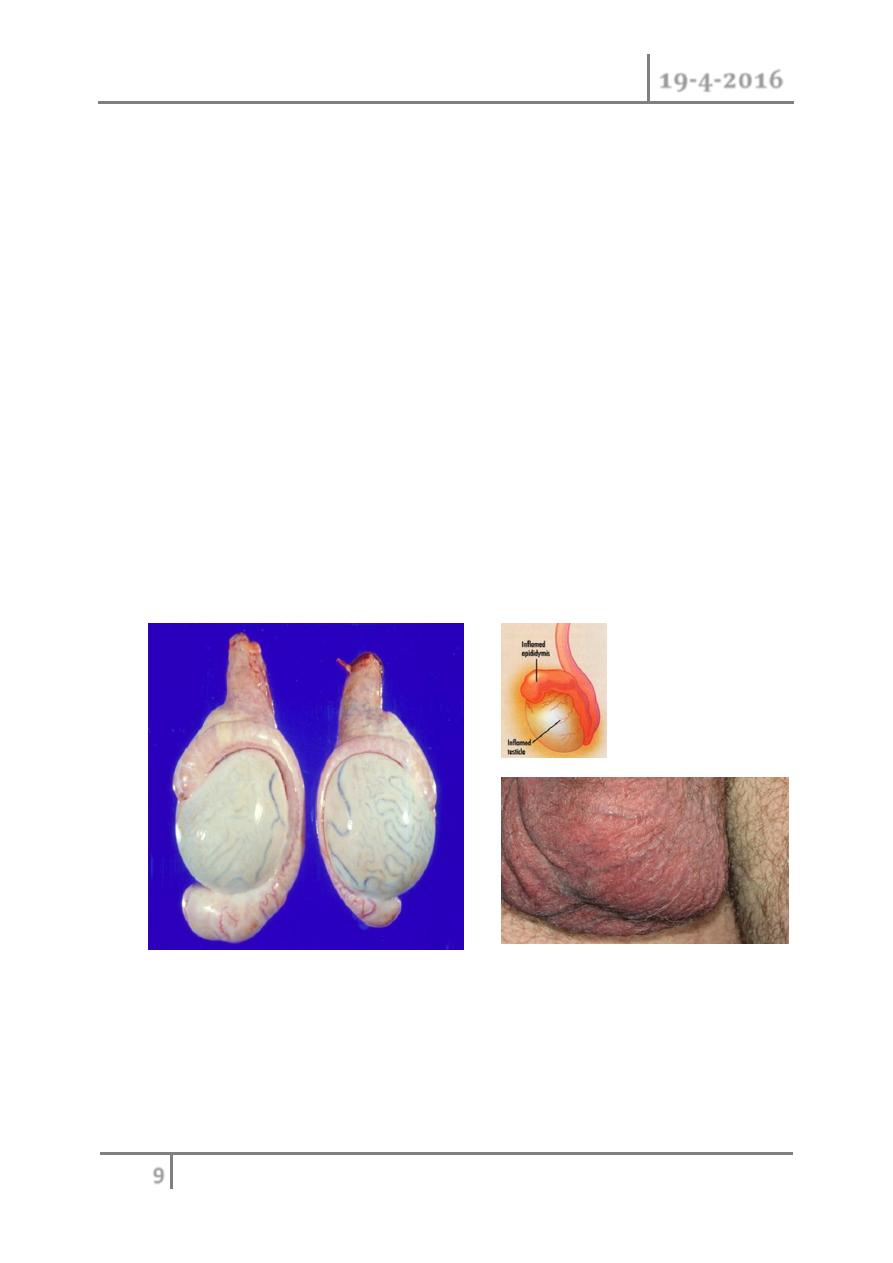
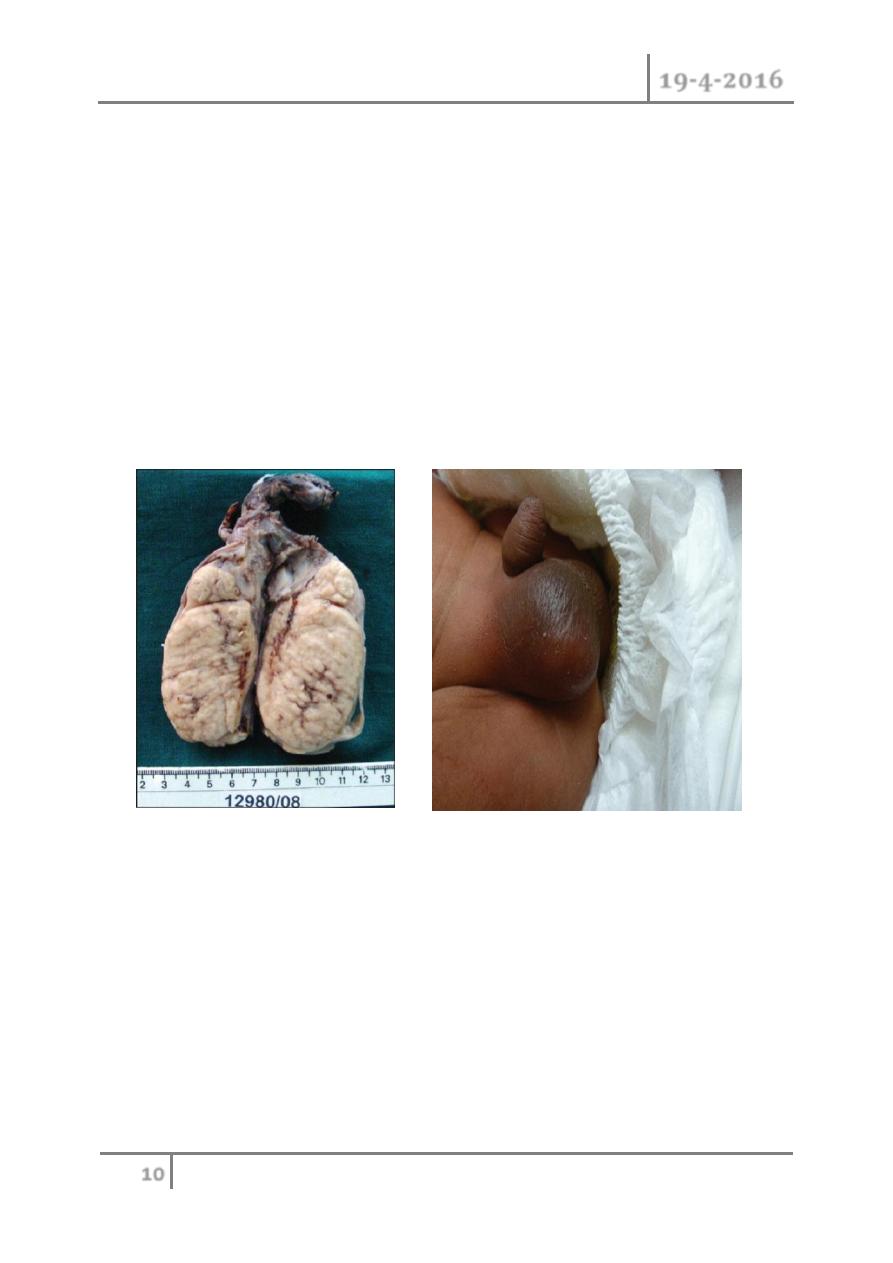
Epididymitis
o is an infl ammatory condition of the epididymis, and caused usually
caused by bacterial infection. It has an acute onset and a clinical course
lasting <6 weeks. It presents with pain, swelling, and tenderness of the
epididymis.
o It should be distinguished from chronic epididymitis, where there is
longstanding pain in the epididymis but usually no swelling. Untreated,
bacterial epididymitis can extend to the testicle, resulting in epididmo-
orchitis.
o Infection ascends from the urethra or bladder. In men aged <35 years,the
infective organism is usually N. gonorrhoeae, C. trachomatis, or coliform
bacteria (causing a urethritis that then ascends to infect the epididymis).
o In children and older men, the infective organisms are usually coliforms
(such as E coli, Pseudomonas, Proteus, and Klebsiella species).
Occasionally, Ureaplasma urealyticum, Corynebacterium, or
Mycoplasma is the cause. Mycobacterium tuberculosis (TB) is a rarer
cause—the epididymis feels like a beaded cord.
Treatment of epididymitis
o Culture urine, any urethral discharge, and blood (if the patient appears
systemically ill). Urine cultures are often sterile. Management consists of
o bed rest, analgesia, anti-infl ammatories, ice packs and antibiotics. Any
form of urethral instrumentation should be avoided.
UTI Dr. Mohammed Basil
19-4-2016
10
©Ali Kareem 2015-2016
Orchitis
o Orchitis is infl ammation of the testis, although it often occurs with
epididymitis (epididymo-orchitis). Causes include mumps; M.
tuberculosis; syphilis;autoimmune processes (granulomatous orchitis).
The testis is swollen and tense, with edema of connective tissues and infl
ammatory cell infi ltration.
o Treat the underlying cause.
o Mumps orchitis occurs in 30% of infected post-pubertal males. It
manifests 3–4 days after the onset of parotitis, and can result in tubular
atrophy.
o 10–30% of cases are bilateral and are associated with infertility.
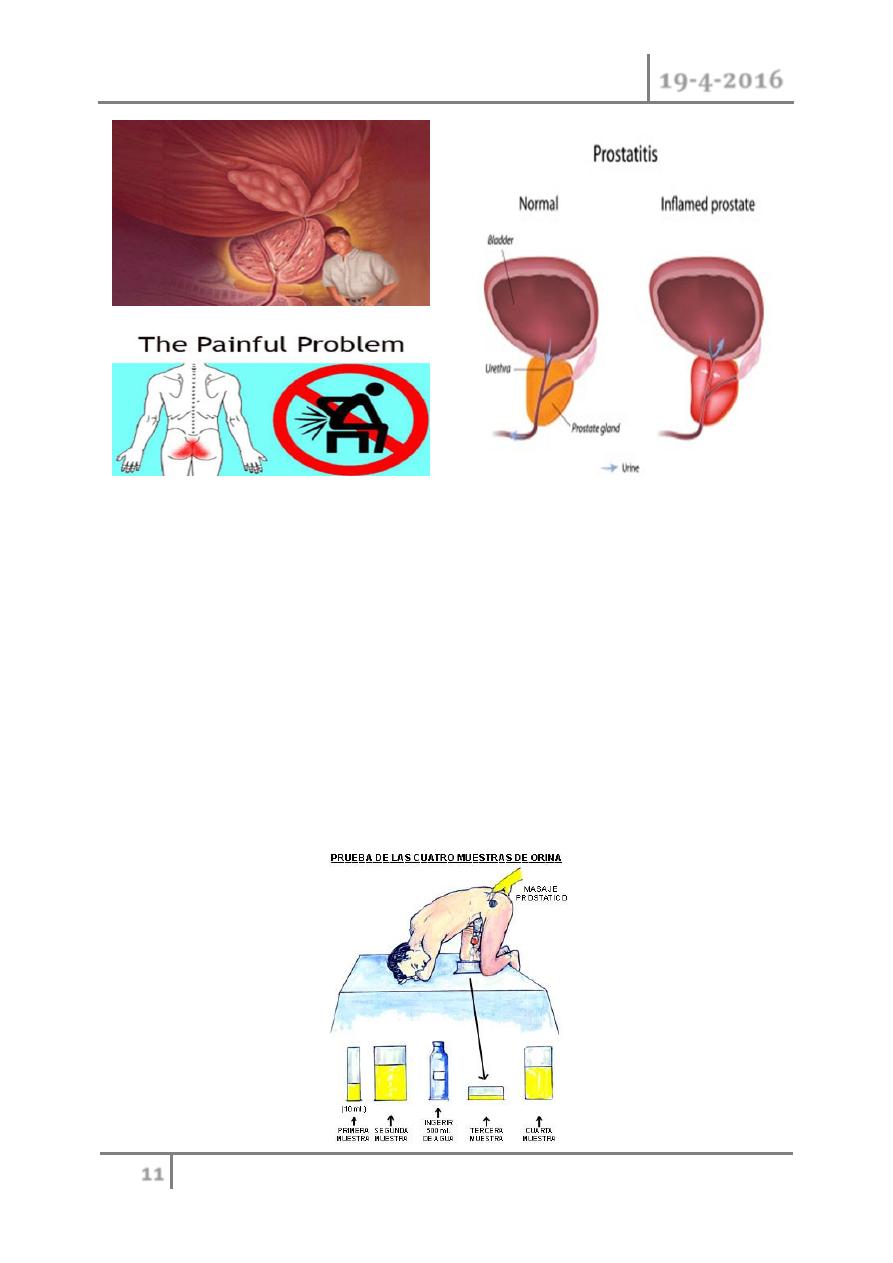
Prostatitis
Classification of prostatitis
o I Acute bacterial prostatitis (ABP)
o II Chronic bacterial prostatitis (CBP)
o III Chronic pelvic pain syndrome (CPPS)
o IIIA Infl ammatory CPPS (chronic nonbacterial prostatitis): WBC in
expressed prostatic secretions (EPS), VB3, or semen
o IIIB Noninfl ammatory CPPS (prostatodynia): no WBC in EPS, VB3 or
semen
o IV Asymptomatic infl ammatory prostatitis (histological prostatitis)
UTI Dr. Mohammed Basil
19-4-2016
11
©Ali Kareem 2015-2016
Epidemiology
o The most common type of prostatitis is NIH III chronic pelvic pain
syndrome, accounting for 90–95% of cases of prostatitis. Acute and
chronic bacterial prostatitis (NIH I and II) each makes up another 2–5%
of cases.
Risk factors
o These include UTI; acute epididymitis; urethral catheters; transurethral
surgery; intraprostatic ductal reflux; phimosis; prostatic stones
(corporaamylacea that can provide a nidus of infection for chronic
prostatitis).
UTI Dr. Mohammed Basil
19-4-2016
12
©Ali Kareem 2015-2016
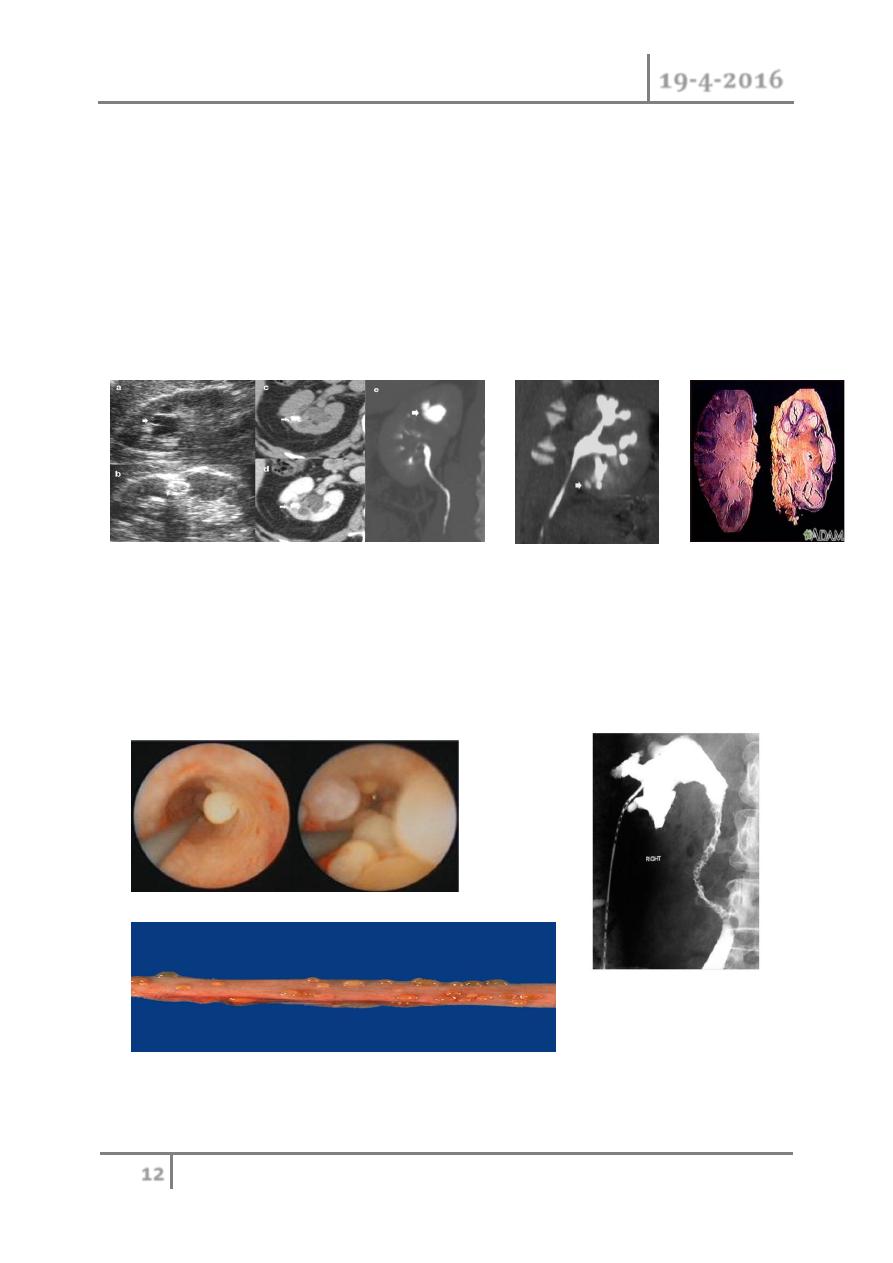
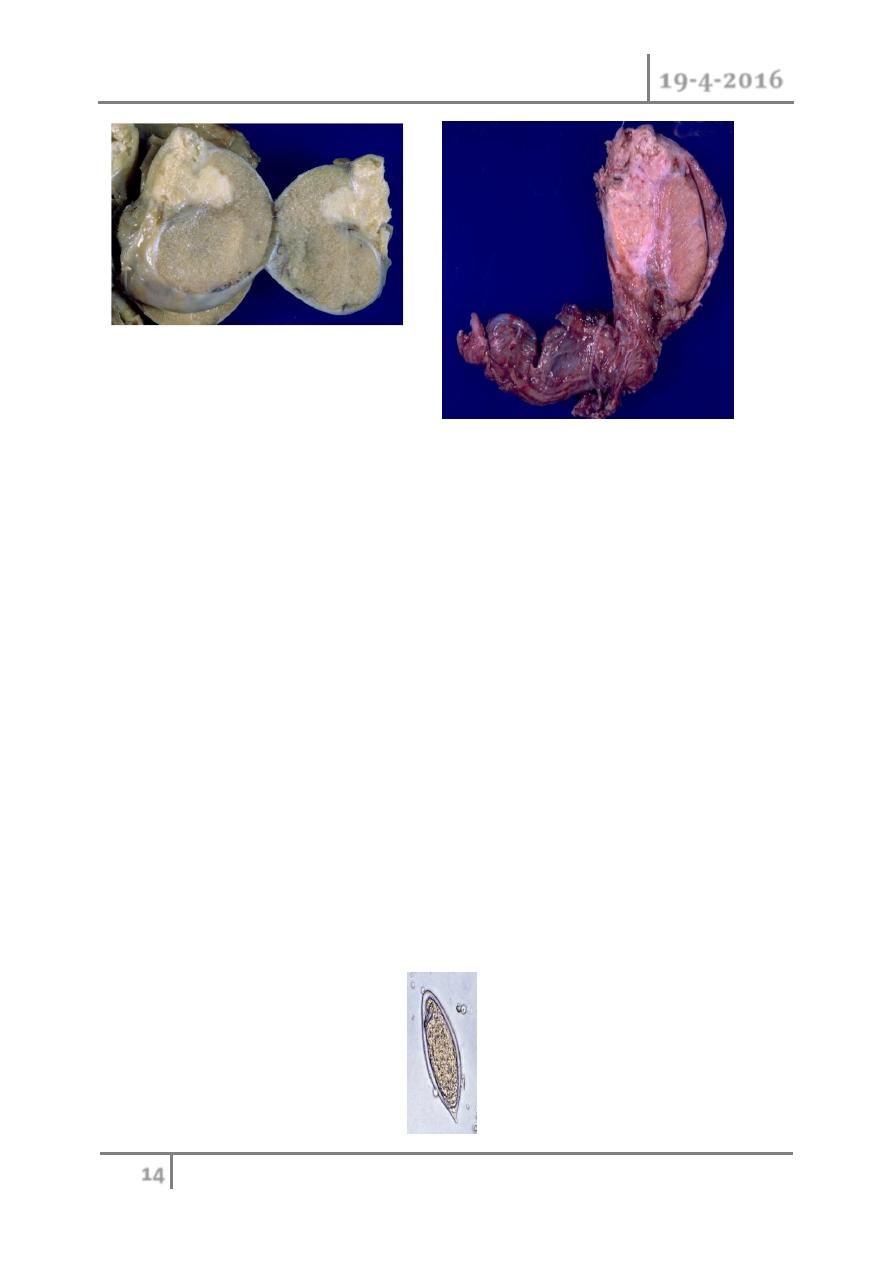
Tuberculosis (TB) of the genitourinary (GU) tract
Kidney
o Hematogenous spread causes granuloma formation in the renal cortex,
associated with caseous necrosis of the renal papillae and deformity of
the calyces, leading to release of bacilli into the urine. This is followed by
healing fibrosis and calcification, which causes destruction of renal
architecture and autonephrectomy.
Ureters
o Spread is directly from the kidney and can result in stricture
formation(vesicoureteric junction, pelviureteric junction, and mid-
ureteric) and ureteritis cystica.
UTI Dr. Mohammed Basil
19-4-2016
13
©Ali Kareem 2015-2016
Bladder
o Infection is usually secondary to renal infection, although iatrogenic TB
can be caused by intravesical BCG treatment for carcinoma in situ. The
bladder wall becomes edematous, red, and inflamed, with ulceration .
o Disease progression causes fibrosis and contraction (resulting in a small
capacity ‗thimble‘ bladder), obstruction, and calcification.
Prostate and seminal vesicles
o Hematogenous spread causes cavitation and calcification, with palpable,
hard-feeling structures. Fistulae may form to the rectum or perineum.
Epididymis
o
Hematogenous spread results in a ―beaded‖ cord. Infection may spread
to the testis.
UTI Dr. Mohammed Basil
19-4-2016
14
©Ali Kareem 2015-2016
Presentation
o Early symptoms include fever, lethargy, weight loss, night sweats, and
UTI not responding to treatment. Later manifestations include LUTS,
hematuria, and flank pain.
Investigations
o Urine: At least 3 early morning urines are required.
o CXR and sputum
o Tuberculin skin test
o IVP or CT urogram: Findings include renal calcifi cation
o
(nephrocalcinosis), irregular calyces (―moth-eaten kidney‖),
infundibular stenosis, cavitation, pelviureteric and vesicoureteric
obstruction, and a contracted, calcified bladder.
o Cystoscopy and biopsy
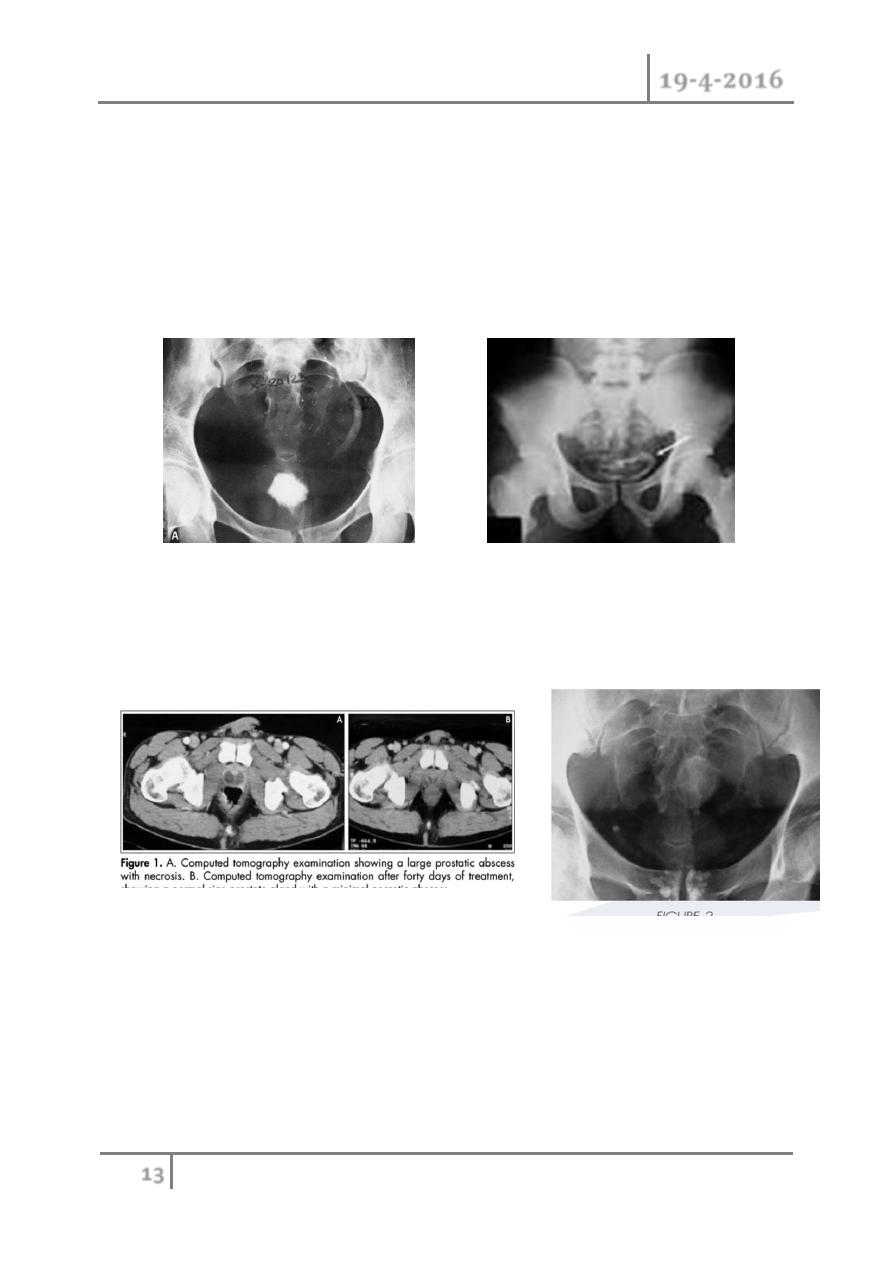
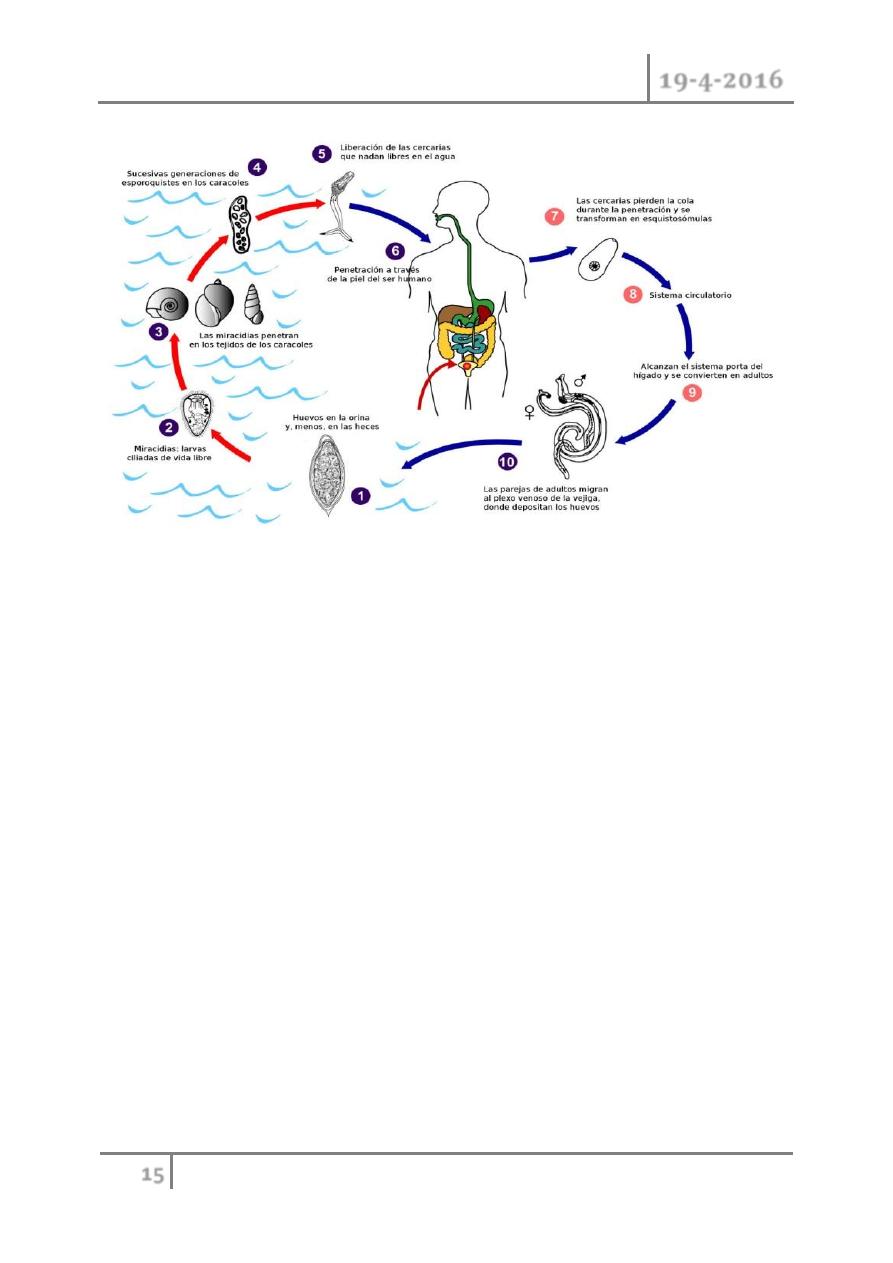
Schistosomiasis (bilharziasis)
o Urinary schistosomiasis is caused by the trematode (or fluke) Schistoma
haematobium.
UTI Dr. Mohammed Basil
19-4-2016
15
©Ali Kareem 2015-2016
Presentation
o
The first clinical sign is ―swimmer‘s itch‖—a local infl ammatory
response.Other early manifestations include Katayama fever, a
generalized allergic reaction, which includes fever, urticaria,
lymphadenopathy, hepatosplenomegaly, and eosinophilia. Active infl
ammation results in hematuria, frequency, and terminal dysuria. The
development of squamous cell carcinoma of the bladder is result of the
chronic inflammation.
Investigation
o Midday urine specimen; bladder and rectal biopsies may contain eggs
(distinguished by having a terminal spine).
o Serology tests (ELISA).
o
Cystoscopy identifies eggs in the trigone (―sandy patches‖).
o IVP or CT urogram may show a calcified, contracted bladder, and
obstructive uropathy.

UTI Dr. Mohammed Basil
19-4-2016
16
©Ali Kareem 2015-2016
Treatment
o Give praziquantel 40 mg/kg in 2 divided doses 4–6 hours apart.
Alternative medications include metrifonate or niridazole.
Complications
o Chronic infection can lead to obstructive uropathy, ureteric stenosis,
renal failure, and bladder contraction, or ulceration. The most signifi
cant and concerning complication is the development of squamous cell
carcinoma of the bladder that often presents at an advanced stage.
END OF THIS LECTURE …
